Lung Cancer Risk from Occupational and Environmental Radon and Role of Smoking in Two Czech Nested Case-Control Studies
Abstract
:1. Introduction
2. Methods
2.1. Study Populations
2.2. Exposure Estimates
2.3. Method of Analyses




2.4. Lifetime Risk Calculation



3. Results
3.1. Relative Risks in Case-Control Studies
| Study | Cases | Controls | Mean exposure among cases | Mean exposure among controls |
|---|---|---|---|---|
| S study | 728 | 1,628 | 198 WLM | 145 WLM |
| N study | 212 | 739 | 9 WLM | 8 WLM |
| L study | 89 | 281 | 35 WLM | 32 WLM |
| Entire occupational study | 1,029 | 2,648 | 145 WLM | 95 WLM |
| Mid-Bohemia Pluton | 289 | 1,156 | 443 Bq·m−3 | 418 Bq·m−3 |
| Bulovka | 81 | 243 | 109 Bq·m−3 | 81 Bq·m−3 |
| Entire residential study | 370 | 1,399 | 370 Bq·m−3 | 359 Bq·m−3 |
| Occupational study | Residential study | |||
|---|---|---|---|---|
| cases | controls | cases | controls | |
| Never-smokers | 80 | 722 | 58 | 670 |
| Ex-smokers (>10 y) | 108 | 430 | 49 | 184 |
| Other smokers | 840 | 1,496 | 263 | 545 |
| Total | 1,029 | 2,648 | 370 | 1,399 |
| Cases | Controls | Crude OR | 90%CI | Adjusted OR | 90%CI | |
|---|---|---|---|---|---|---|
| Miners | ||||||
| Smoking | ||||||
| Never-smokers | 80 | 722 | 1.00 | 1.00 | ||
| Ex-smokers (>10 y) | 108 | 430 | 2.30 | 1.74–3.03 | 2.29 | 1.72–3.02 |
| Other | 840 | 1,496 | 5.98 | 4.78–7.49 | 5.79 | 4.61–7.27 |
| Radon exposure | ||||||
| <50 WLM | 329 | 1,239 | 1.00 | 1.00 | ||
| 50–99 WLM | 163 | 499 | 1.64 | 1.28–2.12 | 1.70 | 1.31–2.22 |
| 100–199 WLM | 249 | 539 | 2.47 | 1.90–3.21 | 2.46 | 1.87–3.23 |
| 200+ WLM | 288 | 371 | 4.06 | 3.10–5.32 | 3.74 | 2.82–4.96 |
| Residents | ||||||
| Smoking | ||||||
| Never-smokers | 58 | 670 | 1.00 | 1.00 | ||
| Ex-smokers (>10 y) | 49 | 184 | 3.96 | 2.65–5.93 | 4.00 | 2.68–5.99 |
| Other | 263 | 545 | 10.19 | 7.28–14.26 | 10.15 | 7.25–14.21 |
| Radon exposure* | ||||||
| <200 Bq/m3 | 85 | 311 | 1.00 | 1.00 | ||
| 200–399 Bq/m3 | 118 | 484 | 1.52 | 1.01–2.29 | 1.41 | 0.91–2.17 |
| 400+ Bq/m3 | 167 | 604 | 1.84 | 1.20–2.82 | 1.76 | 1.11–2.80 |
| Occupational study | Residential study | |||||
|---|---|---|---|---|---|---|
| Cases | ERR/WLM | 90%CI | Cases | ERR/100Bq·m−3 | 90%CI | |
| Never smokers | 80 | 0.049 | 0.010–0.179 | 58 | 0.73 | 0.02–1.9 |
| Ever smokers | 949 | 0.010 | 0.006–0.017 | 312 | 0.14 | 0.02–0.30 |
| Smoking adjusted | 0.014 | 0.009–0.023 | 0.14 | 0.03–0.39 | ||
| Smoking ignored | 0.013 | 0.007–0.019 | 0.12 | 0.02–0.32 | ||

3.2. Geometric Mixture Models
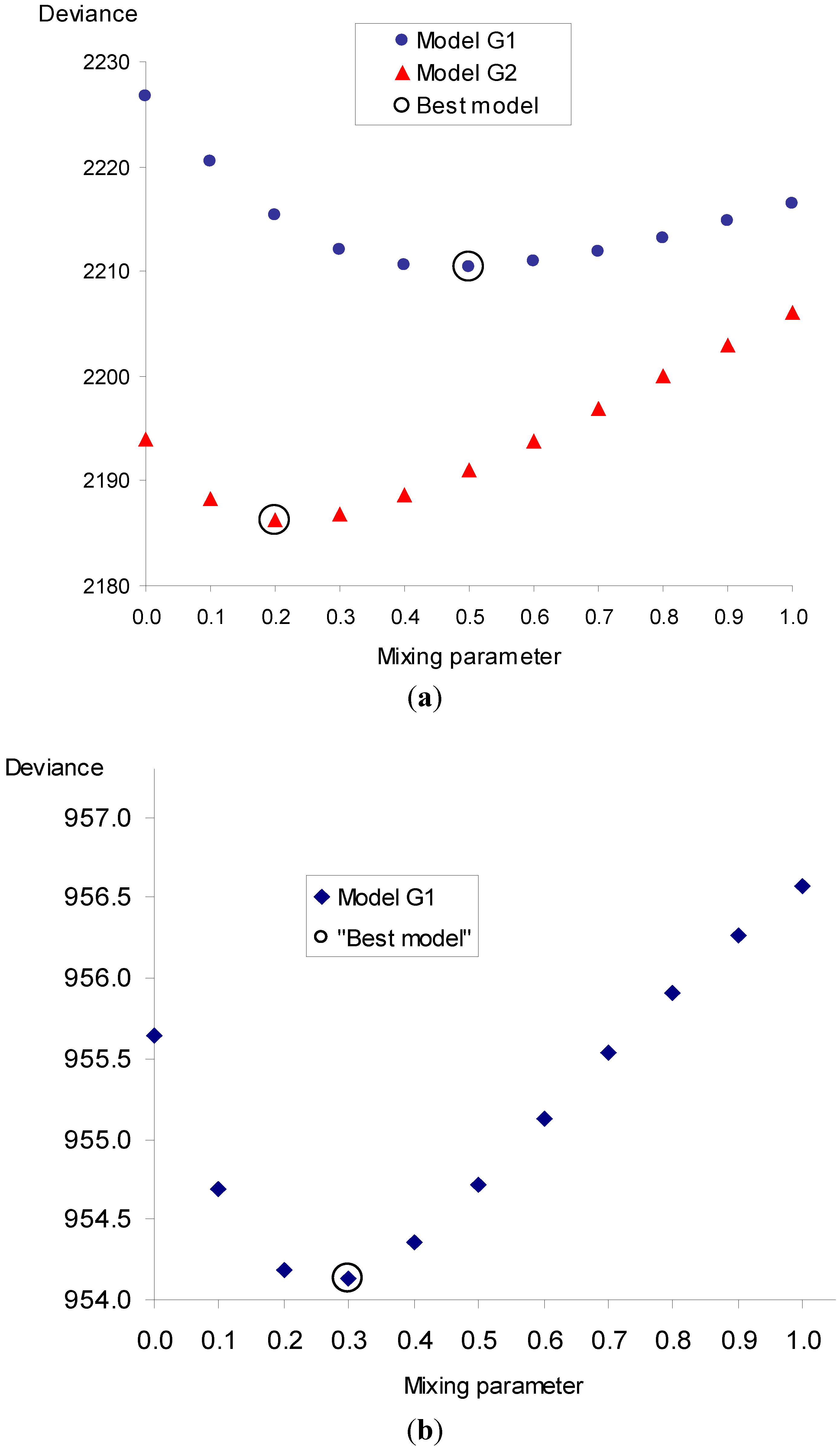
| Occupational study | |||||
| θ | Deviance | ERR/WLM | RR(S) * | 90%CI | |
| 0.0 | 2,193.98 | TSE 5–19 | 0.186 | 0.084–0.537 | |
| TSE 20+ | 0.018 | 0.005 0.064 | |||
| ex-smoker | 7.58 | 3.18–18.06 | |||
| smoker | 24.33 | 10.18–58.15 | |||
| 0.2 | 1,661.73 | TSE 5–19 | 0.149 | 0.074–0.338 | |
| TSE 20+ | 0.020 | 0.007–0.058 | |||
| ex-smoker | 5.98 | 3.27–10.95 | |||
| smoker | 18.75 | 10.37–33.88 | |||
| 1.0 | 1,678.54 | TSE 5–19 | 0.027 | 0.015–0.045 | |
| TSE 20+ | 0.007 | 0.003–0.013 | |||
| ex-smoker | 2.29 | 1.73–3.03 | |||
| smoker | 5.81 | 4.62–7.30 | |||
| Residential study | |||||
| θ | Deviance | ERR/100 Bq·m−3 | RR(S) * | 90%CI | |
| 0.0 | 955.64 | TSE 5–34 | 0.578 | 0.080–168.3 | |
| ex-smoker | 8.88 | 3.19–24.72 | |||
| smoker | 27.45 | 9.34–80.61 | |||
| 0.3 | 954.13 | TSE 5–34 | 0.637 | 0.108–10.5 | |
| ex-smoker | 7.33 | 3.44–15.61 | |||
| smoker | 21.38 | 9.93–46.03 | |||
| 1.0 | 956.58 | TSE 5–34 | 0.138 | 0.026–0.390 | |
| ex-smoker | 4.11 | 2.74–6.15 | |||
| smoker | 10.25 | 7.32–14.35 | |||
3.3. Estimation of Induced Lifetime Risk from Indoor Radon
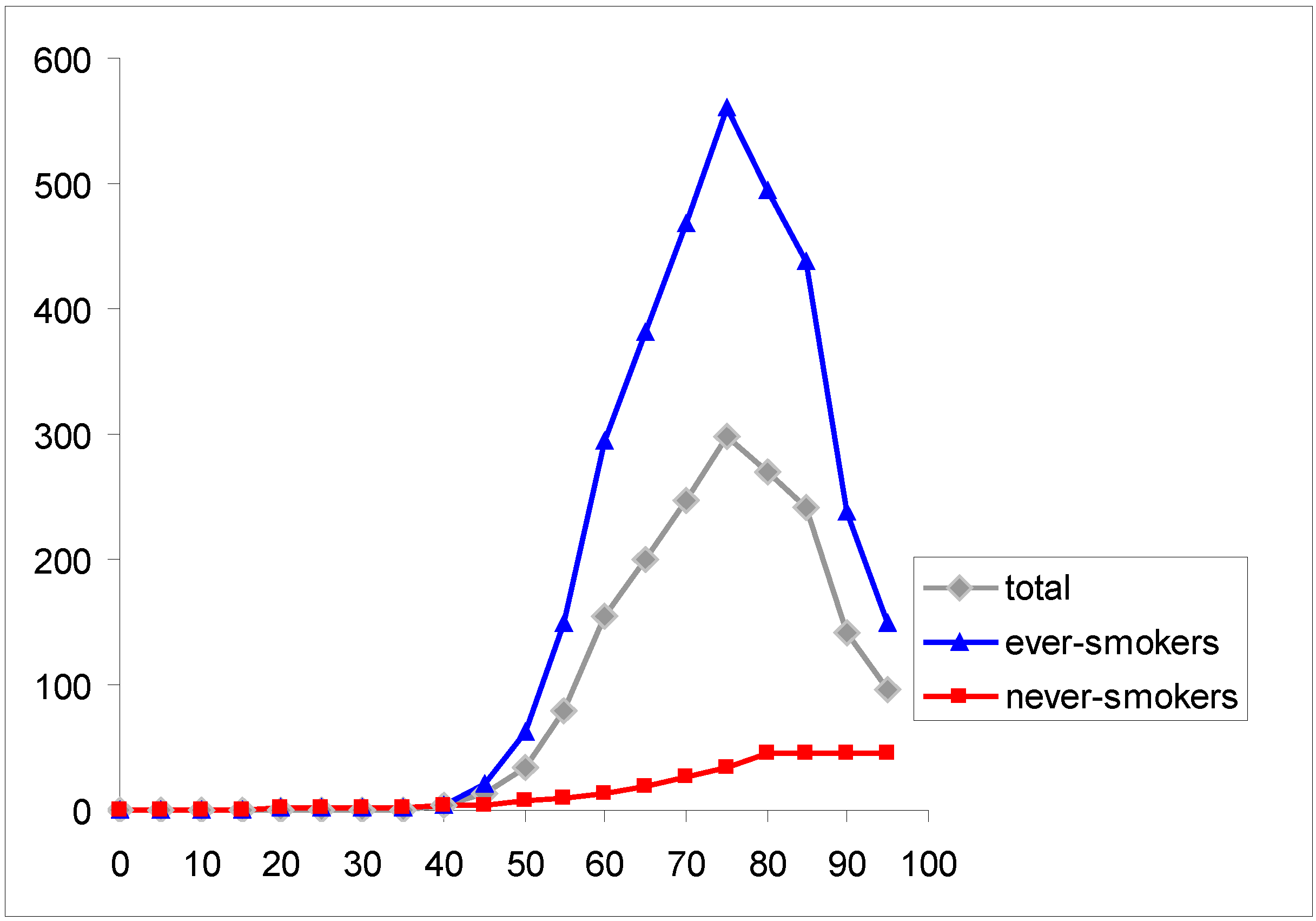

| Model | Non-smokers | Smokers | Total * | |
|---|---|---|---|---|
| “non-exposed” population | 666 | 9,165 | 4,915 | |
| exposed to 100 Bq·m−3 | multiplicative | 758 | 10,430 | 5,594 |
| geometric mixed (θ = 0.3) | 1,090 | 10,655 | 5,872 | |
| induced cases | multiplicative | 92 | 1,265 | 679 |
| at 100 Bq·m−3 | geometric mixed (θ = 0.3) | 424 | 1,490 | 957 |
4. Discussion
4.1. Data Collection
4.2. Strengths and Limitations
4.3. Comparison of Risk Coefficients in Relative Risk Models
4.4. Comparison to Other Studies
4.5. Lifetime Risk
5. Conclusions
Acknowledgements
References
- National Research Council, BEIR VI Health Risks of Exposure to Radon; National Academy Press: Washington, DC, USA, 1998.
- Sevc, J.; Placek, V.; Jerabek, J. Lung Cancer Risk in Relation to Long-Term Radiation Exposure in Uranium Mines. In Proceedings of the 4th Conference on Radiation Hygiene, Hradec Kralove, Czechoslovakia, 1971; pp. 315–326.
- Tomasek, L. Lung cancer mortality among Czech uranium miners—60 years since exposure. J. Radiol. Prot. 2012, 32, 301–314. [Google Scholar] [CrossRef]
- Tomasek, L.; Muller, T.; Kunz, E.; Heribanova, A.; Matzner, J.; Placek, V.; Burian, I.; Holecek, J. Study of lung cancer and residential radon in the Czech Republic. Cent. Eur. J. Publ. Health 2001, 9, 150–153. [Google Scholar]
- Tomasek, L. Lung cancer in a Czech cohort exposed to radon in dwellings—50 years of follow-up. Neoplasma 2012, 59, 559–565. [Google Scholar] [CrossRef]
- Placek, V.; Tomasek, L.; Kunz, E.; Heribanova, A. Lung cancer and exposure to radon under present mining conditions (in Czech). Pracov. Lek. 1997, 49, 14–20. [Google Scholar]
- Kubik, A.; Zatloukal, P.; Tomasek, L.; Dolezal, J.; Syllabova, L.; Kara, J.; Kopecky, P.; Plesko, I. A case-control study of lifestyle and lung cancer associations by histological types. Neoplasma 2008, 53, 192–199. [Google Scholar]
- Sevc, J.; Kunz, E.; Tomasek, L.; Placek, V.; Horacek, J. Cancer in man after exposure to Rn daughters. Health Phys. 1988, 54, 27–46. [Google Scholar] [CrossRef]
- Sevc, J.; Cech, J. Concentration of Rn-222 and its decay products in some Czechoslovak mines. (in Czech). Pracov. Lek. 1966, 18, 438–442. [Google Scholar]
- Tomasek, L. Interaction of radon and smoking among Czech uranium miners. Radiat. Prot. Dosim. 2011, 145, 238–242. [Google Scholar] [CrossRef]
- Preston, D.L.; Lubin, J.H.; Pierce, D.A.; McConney, M.E. Epicure Release 2.10, HiroSoft International Corporation: Seattle, WA, USA, 1998.
- Plummer, M. Improved estimates of floating absolute risk. Statist. Med. 2004, 23, 93–104. [Google Scholar] [CrossRef]
- Zdravotnicka Statistika; UZIS. CR: Praha, Czech Republic, 2011; pp. 44–46.
- Czech Statistical Office Life Tables for the Czech Republic, Areas and Regions. and http://www.czso.cz/csu/2011edicniplan.nsf/engt/93003E422D/$File/40021102.pdf (accessed on 31 May 2011).
- Peto, R.; Lopez, A.; Boreham, J.; Thun, M.; Heath, C. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet 1992, 339, 1269–1278. [Google Scholar]
- Darby, S.; Hill, D.; Deo, H.; Auvinen, A.; Barros-Dios, J.M.; Baysson, H.; Bochicchio, F.; Falk, R.; Farchi, S.; Figueiras, A.; et al. Residential radon and lung cancer—Detailed results of a collaborative analysis of individual data on 7,148 persons with lung cancer and 14,208 persons without lung cancer from 13 epidemiologic studies in Europe. Scand. J. Work Environ. Health 2006, 32, 1–80. [Google Scholar] [CrossRef]
- Simonato, L.; Agudo, A.; Ahrens, W.; Benhamou, E.; Benhamou, S.; Boffetta, P.; Brennan, P.; Darby, S.C.; Forastiere, F.; Fortes, C.; et al. Lung cancer and cigarette smoking in Europe: An update of risk estimates and an assessment of inter-country heterogeneity. Int. J. Cancer 2001, 91, 876–887. [Google Scholar] [CrossRef]
- Leuraud, K.; Schnelzer, M.; Tomasek, L.; Hunter, N.; Tirmarche, M.; Grosche, B.; Kreuzer, M.; Laurier, D. Radon, smoking and lung cancer risk: Results of a joint analysis of three European case-control studies among uranium miners. Radiat. Res. 2011, 176, 375–387. [Google Scholar]
- Lubin, J.H. Studies of radon and lung cancer in North America and China. Radiat. Prot. Dosim. 2003, 104, 315–319. [Google Scholar] [CrossRef]
- Barros-Dios, J.M.; Ruano-Ravina, A.; Perez-Ríos, M.; Castro-Bernardez, M.; Abal-Arca, J.; Tojo-Castro, M. Residential radon exposure, histologic types, and lung cancer risk. A case-control study in Galicia, Spain. Cancer Epidemiol. Biomarkers Prev. 2012, 21, 951–958. [Google Scholar] [CrossRef]
- Baias, P.F.; Hofmann, W.; Winkler-Heil, R.; Cosma, C.; Duliu, O.G. Lung dosimetry for inhaled radon progeny in smokers. Radiat. Prot. Dosim. 2010, 138, 111–118. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Tomasek, L. Lung Cancer Risk from Occupational and Environmental Radon and Role of Smoking in Two Czech Nested Case-Control Studies. Int. J. Environ. Res. Public Health 2013, 10, 963-979. https://doi.org/10.3390/ijerph10030963
Tomasek L. Lung Cancer Risk from Occupational and Environmental Radon and Role of Smoking in Two Czech Nested Case-Control Studies. International Journal of Environmental Research and Public Health. 2013; 10(3):963-979. https://doi.org/10.3390/ijerph10030963
Chicago/Turabian StyleTomasek, Ladislav. 2013. "Lung Cancer Risk from Occupational and Environmental Radon and Role of Smoking in Two Czech Nested Case-Control Studies" International Journal of Environmental Research and Public Health 10, no. 3: 963-979. https://doi.org/10.3390/ijerph10030963
APA StyleTomasek, L. (2013). Lung Cancer Risk from Occupational and Environmental Radon and Role of Smoking in Two Czech Nested Case-Control Studies. International Journal of Environmental Research and Public Health, 10(3), 963-979. https://doi.org/10.3390/ijerph10030963




