The Relationship between the Presence of White Nails and Mortality among Rural, Older, Admitted Patients: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
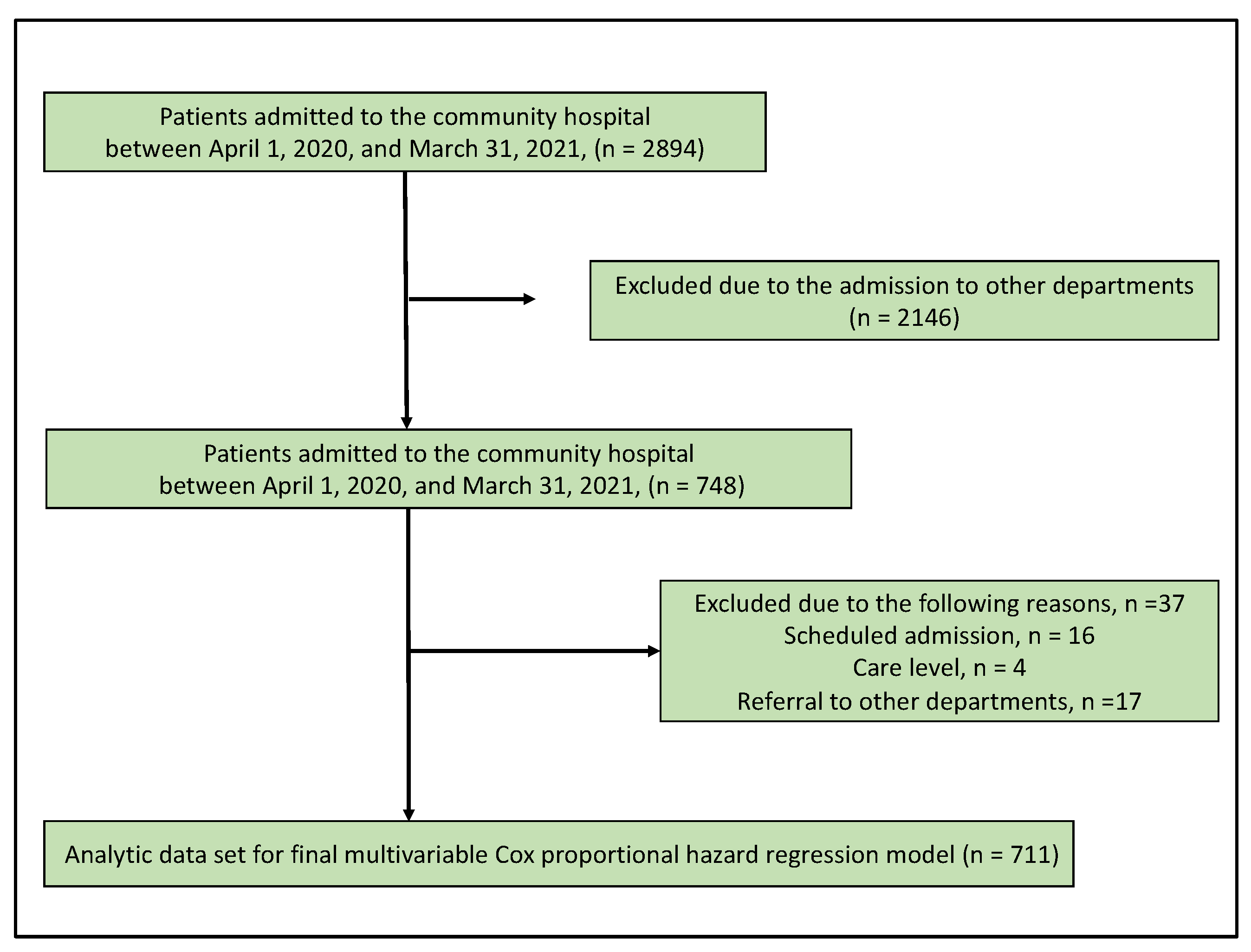
2.2. Participants
2.3. Measurements
2.3.1. Assessment of White Nails
2.3.2. The Patients’ Data
2.3.3. Analysis
2.3.4. Ethical Considerations
3. Results
3.1. The Demographic of the Participants
3.2. The Relationship between the Presence of White Nails and Mortality
3.3. Reasons for Hospital Admission
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fawcett, R.S.; Linford, S.; Stulberg, D.L. Nail Abnormalities: Clues to Systemic Disease. Am. Fam. Phys. 2004, 69, 1417–1424. [Google Scholar]
- Sharma, V.; Ramaiya, M. Nail Color and Texture Analysis for Disease Detection. Int. J. Bio-Sci. Bio-Technol. 2015, 7, 351–358. [Google Scholar] [CrossRef]
- Ohta, R. Deformed Nail from Stress Related to Childbearing. J. Gen. Fam. Med. 2020, 21, 29. [Google Scholar] [CrossRef]
- Baby, T.; Prasad, G.C.; Sunil, S. Nail Changes in Oral Lesions: A Clue to Diagnosis. Trop. J. Med. Res. 2017, 20, 115. [Google Scholar] [CrossRef]
- Lipner, S.R.; Scher, R.K. Evaluation of Nail Lines: Color and Shape Hold Clues. Clevel. Clin. J. Med. 2016, 83, 385–391. [Google Scholar] [CrossRef]
- Jacobsen, E.; Blenning, C.; Judkins, D. Clinical Inquiry: What Nutritional Deficiencies and Toxic Exposures Are Associated with Nail Changes? J. Fam. Pract. 2012, 61, 164–165. [Google Scholar]
- Witkowska, A.B.; Jasterzbski, T.J.; Schwartz, R.A. Terry’s Nails: A Sign of Systemic Disease. Indian J. Derm. 2017, 62, 309–311. [Google Scholar]
- Khichar, S.; Choudhary, S. Terry Nails in a Patient with Chronic Alcoholic Liver Disease. Clevel. Clin. J. Med. 2014, 81, 603–604. [Google Scholar] [CrossRef]
- Yaemsiri, S.; Hou, N.; Slining, M.M.; He, K. Growth Rate of Human Fingernails and Toenails in Healthy American Young Adults. J. Eur. Acad. Derm. Venereol. 2010, 24, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Pitukweerakul, S.; Pilla, S. Terry’s Nails and Lindsay’s Nails: Two Nail Abnormalities in Chronic Systemic Diseases. J. Gen. Intern. Med. 2016, 31, 970. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ohta, R.; Sano, C. White Nail as a Static Physical Finding: Revitalization of Physical Examination. Clin. Pract. 2021, 11, 36. [Google Scholar] [CrossRef]
- Chi, W.C.; Wolff, J.; Greer, R.; Dy, S. Multimorbidity and Decision-Making Preferences among Older Adults. Ann. Fam. Med. 2017, 15, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Murdan, S. Nail Disorders in Older People, and Aspects of Their Pharmaceutical Treatment. Int. J. Pharm. 2016, 512, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Haneef, N.S.; Uday, A. Nail Changes and Disorders among the Elderly. Indian J. Derm. Venereol. Leprol. 2005, 71, 386–392. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kataoka, D.; Sano, C. Effectiveness and Challenges in Local Self-Governance: Multifunctional Autonomy in Japan. Int. J. Environ. Res. Public Health 2021, 18, 574. [Google Scholar] [CrossRef]
- Ohta, R.; Sano, C. Risk of Hospital Readmission among Older Patients Discharged from the Rehabilitation Unit in a Rural Community Hospital: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 659. [Google Scholar] [CrossRef]
- Shimizutani, S. The Future of Long-Term Care in Japan. Asia Pac. Rev. 2014, 21, 88–119. [Google Scholar] [CrossRef]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a Combined Comorbidity Index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Garg, T.; Polenick, C.A.; Schoenborn, N.; Jih, J.; Hajduk, A.; Wei, M.Y.; Hughes, J. Innovative Strategies to Facilitate Patient-Centered Research in Multiple Chronic Conditions. J. Clin. Med. 2021, 10, 2112. [Google Scholar] [CrossRef] [PubMed]
- Skinner, H.G.; Coffey, R.; Jones, J.; Heslin, K.C.; Moy, E. The Effects of Multiple Chronic Conditions on Hospitalization Costs and Utilization for Ambulatory Care Sensitive Conditions in the United States: A Nationally Representative Cross-Sectional Study. BMC Health Serv. Res. 2016, 16, 77. [Google Scholar] [CrossRef]
- Larsen, A.; Broberger, E.; Petersson, P. Complex Caring Needs without Simple Solutions: The Experience of Interprofessional Collaboration among Staff Caring for Older Persons with Multimorbidity at Home Care Settings. Scand. J. Caring Sci. 2017, 31, 342–350. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cereda, E.; Cruz-Jentoft, A.; Goisser, S.; de Groot, L.; Großhauser, F.; Kiesswetter, E.; Norman, K.; et al. Management of Malnutrition in Older Patients-Current Approaches, Evidence and Open Questions. J. Clin. Med. 2019, 8, 974. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, Y.; Wakabayashi, H.; Bise, T.; Nagano, F.; Shimazu, S.; Shiraishi, A.; Yamaga, M.; Koga, H. Sarcopenia Is Associated with Worse Recovery of Physical Function and Dysphagia and a Lower Rate of Home Discharge in Japanese Hospitalized Adults Undergoing Convalescent Rehabilitation. Nutrition 2019, 61, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Short, N.; Shah, C. Muehrcke’s Lines. Am. J. Med. 2010, 123, 991–992. [Google Scholar] [CrossRef]
- Feliu, J.; Pinto, A.; Basterretxea, L.; López-San Vicente, B.; Paredero, I.; Llabrés, E.; Jiménez-Munárriz, B.; Antonio-Rebollo, M.; Losada, B.; Espinosa, E.; et al. Development and Validation of an Early Mortality Risk Score for Older Patients Treated with Chemotherapy for Cancer. J. Clin. Med. 2021, 10, 1615. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Tajiri, K.; Nagata, H.; Kojima, M. Determinants of in-Hospital Mortality in Elderly Patients Aged 80 Years or above with Acute Heart Failure: A Retrospective Cohort Study at a Single Rural Hospital. J. Clin. Med. 2021, 10, 1468. [Google Scholar] [CrossRef]
- Akirov, A.; Masri-Iraqi, H.; Atamna, A.; Shimon, I. Low Albumin Levels Are Associated with Mortality Risk in Hospitalized Patients. Am. J. Med. 2017, 130, 1465.e11–1465.e19. [Google Scholar] [CrossRef]
- Crimmins, E.M.; Shim, H.; Zhang, Y.S.; Kim, J.K. Differences between Men and Women in Mortality and the Health Dimensions of the Morbidity Process. Clin. Chem. 2019, 65, 135–145. [Google Scholar] [CrossRef]
- Gordon, E.H.; Peel, N.M.; Samanta, M.; Theou, O.; Howlett, S.E.; Hubbard, R.E. Sex Differences in Frailty: A Systematic Review and Meta-Analysis. Exp. Gerontol. 2017, 89, 30–40. [Google Scholar] [CrossRef]
- Sirri, L.; Fava, G.A.; Sonino, N. The Unifying Concept of Illness Behavior. Psychother. Psychosom. 2013, 82, 74–81. [Google Scholar] [CrossRef]
- Ohta, R.; Sakamoto, N.; Maeno, T. Home Care Workers’ Judgment of Acute Conditions in Home Care Patients: A Retrospective Cohort Study. Home Health Care Manag. Pract. 2020, 32, 3–9. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Gomi, T.; Katsube, T. Challenges and Solutions in the Continuity of Home Care for Rural Older People: A Thematic Analysis. Home Health Care Serv. Q. 2020, 39, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Ryu, Y.; Katsube, T.; Sano, C. Rural Homecare Nurses’ Challenges in Providing Seamless Patient Care in Rural Japan. Int. J. Env. Res. Public Health 2020, 17, 9330. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Katsube, T. Care Managers in Rural Japan: Challenges to Interprofessional Collaboration. Home Health Care Serv. Q. 2019, 38, 270–285. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Katsube, T. Challenges for Japanese Rural Home Care Workers in Interprofessional Collaboration: A Qualitative Study. Home Health Care Serv. Q. 2018, 37, 313–324. [Google Scholar] [CrossRef]
- Taylor, J.K.; Fleming, G.B.; Singanayagam, A.; Hill, A.T.; Chalmers, J.D. Risk Factors for Aspiration in Community-Acquired Pneumonia: Analysis of a Hospitalized UK Cohort. Am. J. Med. 2013, 126, 995–1001. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC) Developed with the Special Contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [PubMed]
- Stall, N.; Nowaczynski, M.; Sinha, S.K. Systematic Review of Outcomes from Home-Based Primary Care Programs for Homebound Older Adults. J. Am. Geriatr. Soc. 2014, 62, 2243–2251. [Google Scholar] [CrossRef]
- Ohta, R.; Ueno, A.; Kitayuguchi, J.; Moriwaki, Y.; Otani, J.; Sano, C. Comprehensive Care through Family Medicine: Improving the Sustainability of Aging Societies. Geriatrics 2021, 6, 59. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Orzol, S.; Peikes, D.; Oh, E.G.; Dale, S. Participation in the Comprehensive Primary Care Plus Initiative. Ann. Fam. Med. 2020, 18, 309–317. [Google Scholar] [CrossRef]
- Sung, N.J.; Choi, Y.J.; Lee, J.H. Primary Care Comprehensiveness Can Reduce Emergency Department Visits and Hospitalization in People with Hypertension in South Korea. Int. J. Environ. Res. Public Health 2018, 15, 272. [Google Scholar] [CrossRef] [PubMed]
- Yani, M.; Si, S.; Budhi Irawan, M.T.; Casi Setiningsih, M.T.S.T. Application of Transfer Learning Using Convolutional Neural Network Method for Early Detection of Terry’s Nail. J. Phys. Conf. Ser. 2019, 1201, 012052. [Google Scholar] [CrossRef]
| Death | ||||
|---|---|---|---|---|
| Factor | Total | Yes | No | p-Value |
| n | 711 | 74 | 637 | |
| Age (years), mean (SD) | 81.95 (13.63) | 88.41 (6.59) | 81.20 (14.03) | <0.001 |
| male sex (%) | 316 (44.4) | 41 (55.4) | 275 (43.2) | 0.049 |
| albumin, mean (SD) | 3.49 (0.66) | 2.96 (0.54) | 3.55 (0.64) | <0.001 |
| height, mean (SD) | 153.37 (10.44) | 152.73 (9.91) | 153.45 (10.51) | 0.577 |
| body weight, mean (SD) | 48.69 (11.69) | 44.51 (8.67) | 49.18 (11.90) | 0.001 |
| BMI, mean (SD) | 20.59 (3.93) | 19.10 (3.34) | 20.76 (3.96) | 0.001 |
| creatinine | 1.05 (1.09) | 1.07 (0.78) | 1.04 (1.12) | 0.865 |
| eGFR | 58.75 (22.41) | 57.85 (25.78) | 58.86 (22.01) | 0.714 |
| white nail (%) | 212 (29.8) | 54 (73.0) | 158 (24.8) | <0.001 |
| Admission duration (IQR]) | 15.00 (1.00, 167.00) | 24.50 (1.00, 146.00) | 15.00 (1.00, 167.00) | <0.001 |
| CCI ≥ 5 (%) | 423 (59.5) | 55 (74.3) | 368 (57.8) | 0.006 |
| CCI (%) | ||||
| 0 | 26 (3.7) | 0 (0.0) | 26 (4.1) | |
| 1 | 17 (2.4) | 0 (0.0) | 17 (2.7) | |
| 2 | 28 (3.9) | 0 (0.0) | 28 (4.4) | |
| 3 | 50 (7.0) | 2 (2.7) | 48 (7.5) | |
| 4 | 167 (23.5) | 17 (23.0) | 150 (23.5) | |
| 5 | 147 (20.7) | 15 (20.3) | 132 (20.7) | |
| 6 | 112 (15.8) | 15 (20.3) | 97 (15.2) | |
| 7 | 92 (12.9) | 12 (16.2) | 80 (12.6) | |
| 8 | 34 (4.8) | 4 (5.4) | 30 (4.7) | |
| 9 | 21 (3.0) | 2 (2.7) | 19 (3.0) | |
| 10 | 7 (1.0) | 3 (4.1) | 4 (0.6) | |
| 11 | 5 (0.7) | 3 (4.1) | 2 (0.3) | |
| 12 | 2 (0.3) | 0 (0.0) | 2 (0.3) | |
| 13 | 1 (0.1) | 0 (0.0) | 1 (0.2) | |
| 14 | 1 (0.1) | 1 (1.4) | 0 (0.0) | |
| 15 | 1 (0.1) | 0 (0.0) | 1 (0.2) | |
| heart failure (%) | 126 (17.7) | 17 (23.0) | 109 (17.1) | 0.202 |
| MI (%) | 56 (7.9) | 9 (12.2) | 47 (7.4) | 0.168 |
| asthma (%) | 36 (5.1) | 4 (5.4) | 32 (5.0) | 0.782 |
| peptic ulcer (%) | 60 (8.5) | 2 (2.7) | 58 (9.1) | 0.074 |
| kidney disease (%) | 55 (7.7) | 5 (6.8) | 50 (7.8) | 1 |
| liver disease (%) | 26 (3.7) | 2 (2.7) | 24 (3.8) | 1 |
| COPD (%) | 41 (5.8) | 8 (10.8) | 33 (5.2) | 0.062 |
| DM (%) | 106 (14.9) | 9 (12.2) | 97 (15.2) | 0.605 |
| brain infarction (%) | 128 (18.0) | 11 (14.9) | 117 (18.4) | 0.525 |
| brain hemorrhage (%) | 53 (7.5) | 7 (9.5) | 46 (7.2) | 0.482 |
| hemiplegia (%) | 23 (3.2) | 2 (2.7) | 21 (3.3) | 1 |
| connective tissue disease (%) | 26 (3.7) | 2 (2.7) | 24 (3.8) | 1 |
| dementia (%) | 131 (18.4) | 16 (21.6) | 115 (18.1) | 0.432 |
| cancer (%) | 141 (19.8) | 27 (36.6) | 114 (17.9) | 0.001 |
| caregiver dependence (%) | 313 (44.0) | 55 (74.3) | 258 (40.5) | <0.001 |
| care level (%) | ||||
| 0 | 398 (56.0) | 19 (25.7) | 379 (59.5) | |
| 1 | 51 (7.2) | 4 (5.4) | 47 (7.4) | |
| 2 | 83 (11.7) | 16 (21.6) | 67 (10.5) | |
| 3 | 78 (11.0) | 15 (20.3) | 63 (9.9) | |
| 4 | 57 (8.0) | 11 (14.9) | 46 (7.2) | |
| 5 | 44 (6.2) | 9 (12.2) | 35 (5.5) | |
| Factor | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Age | 1.03 | 1.00–1.07 | 0.069 |
| Male sex | 2.05 | 1.18–3.53 | 0.01 |
| Albumin concentration | 0.44 | 0.27–0.72 | <0.001 |
| BMI | 0.97 | 0.90–1.04 | 0.39 |
| CCI ≥ 5 | 0.92 | 0.49–1.72 | 0.79 |
| Caregiver dependence | 1.92 | 1.00–3.67 | 0.049 |
| White nail | 3.47 | 1.85–6.49 | <0.001 |
| Admission duration | 1.00 | 1.00–1.01 | 0.5 |
| Disease | N | Percentage | Disease | N | Percentage |
|---|---|---|---|---|---|
| heart failure | 84 | 11.8% | Hypothyroidism | 5 | 0.7% |
| urinary tract infection | 82 | 11.5% | Hypoglycemia | 5 | 0.7% |
| brain stroke | 58 | 8.2% | hepatic encephalopathy | 5 | 0.7% |
| bacterial pneumonia | 43 | 6.0% | Clostridium difficile colitis | 5 | 0.7% |
| aspiration pneumonia | 42 | 5.9% | vitamin B1 sufficiency | 5 | 0.7% |
| cancer | 23 | 3.2% | transient ischemic attack | 4 | 0.6% |
| brain hemorrhage | 20 | 2.8% | myocardial infarction | 4 | 0.6% |
| trauma | 19 | 2.7% | Dehydration | 4 | 0.6% |
| syncope | 18 | 2.5% | gastroesophageal reflux disease | 4 | 0.6% |
| pseudogout | 17 | 2.4% | varicella zoster virus infection | 3 | 0.4% |
| sepsis | 17 | 2.4% | Type 2 respiratory failure | 3 | 0.4% |
| gastrointestinal bleeding | 16 | 2.3% | temporal arteritis | 3 | 0.4% |
| epilepsy | 15 | 2.1% | septic vertebritis | 3 | 0.4% |
| cellulitis | 14 | 2.0% | Pancreatitis | 3 | 0.4% |
| chronic obstructive lung disease | 11 | 1.5% | diabetic ketoacidosis | 3 | 0.4% |
| ischemic colitis | 11 | 1.5% | polymyalgia rheumatica | 3 | 0.4% |
| peripheral vertigo | 11 | 1.5% | urinary stone | 2 | 0.3% |
| fever | 9 | 1.3% | Tuberculosis | 2 | 0.3% |
| unconsciousness | 9 | 1.3% | Tsutsugamushi | 2 | 0.3% |
| loss of appetite | 8 | 1.1% | normal pressure hydrocephalus | 2 | 0.3% |
| acute enteritis | 8 | 1.1% | liver abscess | 2 | 0.3% |
| cholangitis | 7 | 1.0% | iron deficiency anemia | 2 | 0.3% |
| Parkinson’s syndrome | 6 | 0.8% | Headache | 2 | 0.3% |
| angina | 6 | 0.8% | Guillain–Barré syndrome | 2 | 0.3% |
| peptic ulcer | 6 | 0.8% | Constipation | 2 | 0.3% |
| medication-induced | 6 | 0.8% | Anaphylaxis | 2 | 0.3% |
| electrolyte disturbance | 6 | 0.8% | Alcoholism | 2 | 0.3% |
| pneumothorax | 5 | 0.7% | anterior cutaneous nerve entrapment syndrome | 2 | 0.3% |
| Ileus | 5 | 0.7% | hypertensive emergency | 2 | 0.3% |
| meningitis | 5 | 0.7% | Others | 36 | 5.1% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohta, R.; Ryu, Y.; Sano, C. The Relationship between the Presence of White Nails and Mortality among Rural, Older, Admitted Patients: A Prospective Cohort Study. Healthcare 2021, 9, 1611. https://doi.org/10.3390/healthcare9121611
Ohta R, Ryu Y, Sano C. The Relationship between the Presence of White Nails and Mortality among Rural, Older, Admitted Patients: A Prospective Cohort Study. Healthcare. 2021; 9(12):1611. https://doi.org/10.3390/healthcare9121611
Chicago/Turabian StyleOhta, Ryuichi, Yoshinori Ryu, and Chiaki Sano. 2021. "The Relationship between the Presence of White Nails and Mortality among Rural, Older, Admitted Patients: A Prospective Cohort Study" Healthcare 9, no. 12: 1611. https://doi.org/10.3390/healthcare9121611
APA StyleOhta, R., Ryu, Y., & Sano, C. (2021). The Relationship between the Presence of White Nails and Mortality among Rural, Older, Admitted Patients: A Prospective Cohort Study. Healthcare, 9(12), 1611. https://doi.org/10.3390/healthcare9121611






