Assessing the Quality of Reporting to China’s National TB Surveillance Systems
Abstract
1. Background
2. Methods
2.1. Study Setting
2.2. Study Design
2.3. Sampling Method
2.4. Eligibility Criteria
2.5. Data Collection
2.6. Data Deduplication
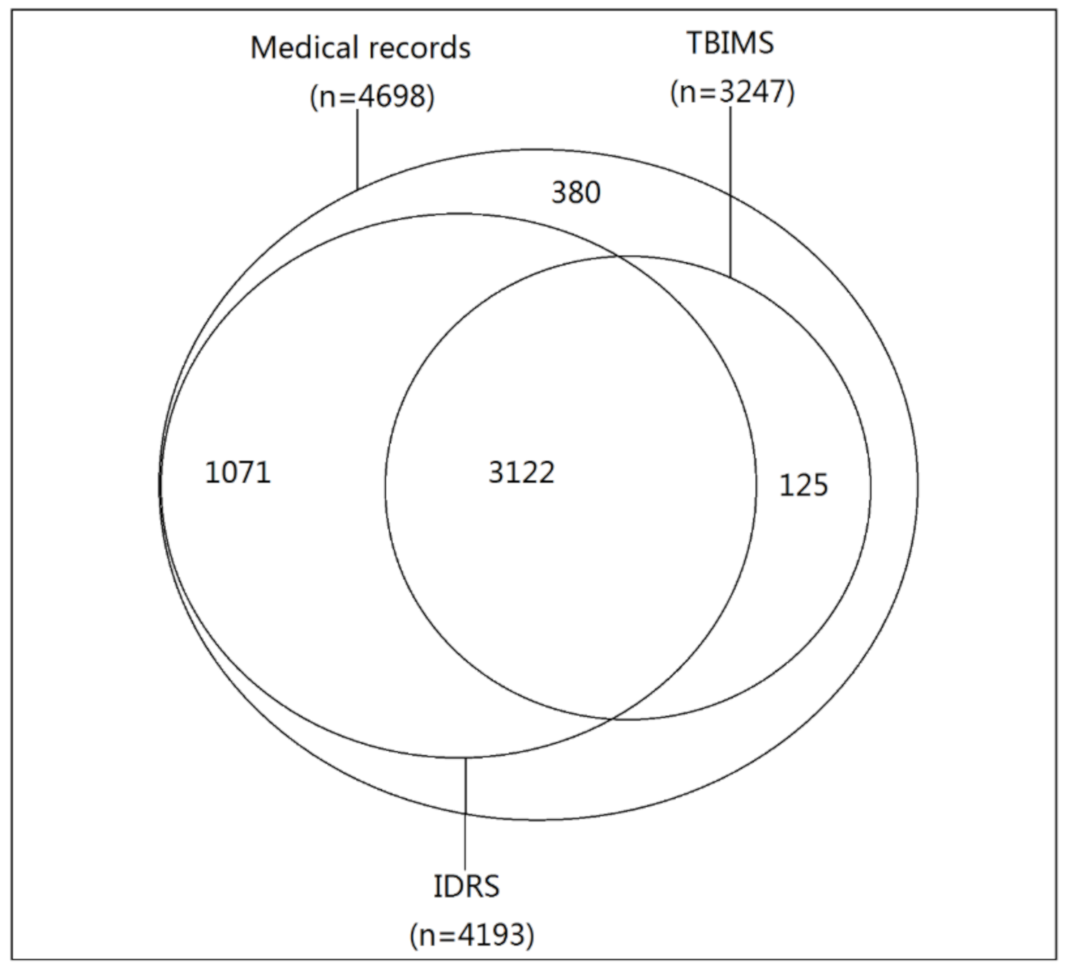
2.7. Record Linkage
2.8. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TB | tuberculosis; |
| WHO | World Health Organization; |
| PTB | pulmonary TB; |
| IDRS | Infectious Disease Reporting System; |
| TBIMS | Tuberculosis Information Management System; |
| CDC | Center for Disease Control and Prevention; |
| NTP | national TB program; |
| PLADs | provincial-level administrative divisions; |
| CXR | chest x-rays; |
| EPTB | extra-pulmonary TB; |
| OR | odds ratio |
References
- Van Leth, F.; Evenblij, K.; Wit, F.; Kiers, A.; Sprenger, H.; Verhagen, M.; Hillebregt, M.; Kalisvaart, N.; Schimmel, H.; Verbon, A. TB-HIV co-infection in the Netherlands: Estimating prevalence and under-reporting in national registration databases using a capture-recapture analysis. J. Epidemiol. Community Health 2016, 70, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Avong, Y.K.; Jatau, B.; Gurumnaan, R.; Danat, N.; Okuma, J.; Usman, I.; Mordi, D.; Ukpabi, B.; Kayode, G.A.; Dutt, S.; et al. Addressing the under-reporting of adverse drug reactions in public health programs controlling HIV/AIDS, Tuberculosis and Malaria: A prospective cohort study. PLoS ONE 2018, 13, e0200810. [Google Scholar] [CrossRef] [PubMed]
- Crowcroft, N.S.; Johnson, C.; Chen, C.; Li, Y.; Marchand-Austin, A.; Bolotin, S.; Schwartz, K.; Deeks, S.L.; Jamieson, F.; Drews, S.; et al. Under-reporting of pertussis in Ontario: A Canadian Immunization Research Network (CIRN) study using capture-recapture. PLoS ONE 2018, 13, e0195984. [Google Scholar] [CrossRef]
- Guo, K.; Yin, P.; Wang, L.; Ji, Y.; Li, Q.; Bishai, D.; Liu, S.; Liu, Y.; Astell-Burt, T.; Feng, X.; et al. Propensity score weighting for addressing under-reporting in mortality surveillance: A proof-of-concept study using the nationally representative mortality data in China. Popul. Health Metr. 2015, 13, 1–11. [Google Scholar] [CrossRef]
- Kustec, T.; Keše, D.; Klavs, I. Under-reporting of sexually transmitted infection with chlamydia trachomatis—A revision of surveillance system is required. Slov. J. Public Health 2016, 55, 174–178. [Google Scholar] [CrossRef]
- Shankar, M.B.; Rodríguez-Acosta, R.L.; Sharp, T.M.; Tomashek, K.M.; Margolis, H.S.; Meltzer, M.I. Estimating dengue under-reporting in Puerto Rico using a multiplier model. PLoS Negl. Trop. Dis. 2018, 12, e0006650. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report 2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/250441/9789241565394-eng.pdf?sequence=1 (accessed on 15 January 2020).
- World Health Organization. Global Tuberculosis Report 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1 (accessed on 15 January 2020).
- World Health Organization. Implementing the End TB Strategy: The Essentials. 2015. Available online: https://www.who.int/tb/publications/2015/The_Essentials_to_End_TB/en/ (accessed on 15 January 2020).
- Lin, H.H.; Wang, L.; Zhang, H.; Ruan, Y.; Chin, D.P.; Dye, C. Tuberculosis control in China: Use of modelling to develop targets and policies. Bull. World Health Organ. 2015, 93, 790–798. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China. Progress in Disease Control and Prevention in China in 2015. Available online: http://www.nhc.gov.cn/jkj/s7915v/201504/d5f3f871e02e4d6e912def7ced719353.shtml (accessed on 15 January 2020).
- Li, T.; Shewade, H.D.; Soe, K.T.; Rainey, J.J.; Zhang, H.; Du, X.; Wang, L. Under-reporting of diagnosed tuberculosis to the national surveillance system in China: An inventory study in nine counties in 2015. BMJ Open 2019, 9, e021529. [Google Scholar] [CrossRef] [PubMed]
- Tollefson, D.; Ngari, F.; Mwakala, M.; Gethi, D.; Kipruto, H.; Cain, K.; Bloss, E. Under-reporting of sputum smear-positive tuberculosis cases in Kenya. Int. J. Tuberc. Lung Dis. 2016, 20, 1334–1341. [Google Scholar] [CrossRef]
- Morales-Garcia, C.; Rodrigo, T.; Garcia-Clemente, M.M.; Munoz, A.; Bermudez, P.; Casas, F.; Somoza, M.; Mila, C.; Penas, A.; Hidalgo, C.; et al. Factors associated with unreported tuberculosis cases in Spanish hospitals. BMC Infect. Dis. 2015, 15, 295. [Google Scholar] [CrossRef]
- Hong, S.J.; Park, Y.S.; An, H.; Kang, S.M.; Cho, E.H.; Shin, S.S. Factors leading to under-reporting of tuberculosis in the private sector in Korea. Int. J. Tuberc. Lung Dis. 2012, 16, 1221–1227. [Google Scholar] [CrossRef] [PubMed]
- Furtado da Luz, E.; Braga, J.U. Under-reporting of tuberculosis in Praia, Cape Verde, from 2006 to 2012. Int. J. Tuberc. Lung Dis. 2018, 22, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Bassili, A.; Grant, A.D.; El-Mohgazy, E.; Galal, A.; Glaziou, P.; Seita, A.; Abubakar, I.; Bierrenbach, A.L.; Crofts, J.P.; van Hest, N.A. Estimating tuberculosis case detection rate in resource-limited countries: A capture-recapture study in Egypt. Int. J. Tuberc. Lung Dis. 2010, 14, 727–732. [Google Scholar]
- World Health Organization. Assessing Tuberculosis Under-Reporting through Inventory Studies. 2012. Available online: https://apps.who.int/iris/bitstream/handle/10665/78073/9789241504942_eng.pdf?sequence=1 (accessed on 15 January 2020).
- National Bureau of Statistics. China Statistical Yearbook. 2018. Available online: http://www.stats.gov.cn/tjsj/ndsj/2018/indexch.htm (accessed on 15 January 2020).
- Fan, C.; Rongsheng, Z.; Jing, Z.; Yun, X.; Fan, Y. Current status and prospects of tuberculosis prevention and control in China. J. Public Health Prev. Med. 2019, 30, 8–11. [Google Scholar] [CrossRef]
- Ministry of Health. Guidelines for Implementing the National Tuberculosis Control Program in China (2008); China Union Medical University Press: Beijing, China, 2009.
- Ministry of Health. National Tuberculosis Diagnostic Criteria (WS288-2008); People’s Health Publishing House: Beijing, China, 2008.
- World Health Organization. Global Tuberculosis Report 2017. Available online: https://www.who.int/tb/publications/2017/en/ (accessed on 15 January 2020).
- Dunbar, R.; van Hest, R.; Lawrence, K.; Verver, S.; Enarson, D.A.; Lombard, C.; Beyers, N.; Barnes, J.M. Capture-recapture to estimate completeness of tuberculosis surveillance in two communities in South Africa. Int. J. Tuberc. Lung Dis. 2011, 15, 1038–1043. [Google Scholar] [CrossRef] [PubMed]
- Alkhalawi, M.J.; McNabb, S.J.; Assiri, A.M.; Memish, Z.A. Evaluation of tuberculosis public health surveillance, Al-Madinah province, Kingdom of Saudi Arabia, 2012. J. Epidemiol. Glob. Health 2016, 6, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Ibarz-Pavon, A.B.; Papaventsis, D.; Kalkouni, R.; Metaxas, G.; Spala, G.; Georgakopoulou, T.; Gerakis, T.; Pefanis, A.; Vogiatzakis, E. Pilot study of the completeness of notification of adult tuberculosis in Athens, Greece. Int. J. Tuberc. Lung Dis. 2016, 20, 920–925. [Google Scholar] [CrossRef]
- Fatima, R.; Harris, R.J.; Enarson, D.A.; Hinderaker, S.G.; Qadeer, E.; Ali, K.; Bassili, A. Estimating tuberculosis burden and case detection in Pakistan. Int. J. Tuberc. Lung Dis. 2014, 18, 55–60. [Google Scholar] [CrossRef]
- Kang, H.Y.; Yoo, H.; Park, W.; Go, U.; Jeong, E.; Jung, K.S.; Son, H. Tuberculosis Notification Completeness and Timeliness in the Republic of Korea During 2012–2014. Osong Public Health Res. Perspect. 2016, 7, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Salyer, S.J.; Fitter, D.L.; Milo, R.; Blanton, C.; Ho, J.L.; Geffrard, H.; Morose, W.; Marston, B.J. Evaluation of the national tuberculosis surveillance program in Haiti. Int. J. Tuberc. Lung Dis. 2015, 19, 1045–1050. [Google Scholar] [CrossRef]
- Gimenez Duran, J.; Galmes Truyols, A.M.; Herrera Guibert, D.; Bonilla Vargas, L.A.; Luque Fernandez, M.A.; Bosch Isabel, C.; Nicolau Riutort, A.; Cayla Buqueras, J. Tuberculosis surveillance in the Balearic Islands and characteristics of unreported cases from 2005 to 2007. Gac. Sanit. 2011, 25, 84–86. [Google Scholar] [CrossRef]
- Melosini, L.; Vetrano, U.; Dente, F.L.; Cristofano, M.; Giraldi, M.; Gabbrielli, L.; Novelli, F.; Aquilini, F.; Rindi, L.; Menichetti, F.; et al. Evaluation of underreporting tuberculosis in Central Italy by means of record linkage. BMC Public Health 2012, 12, 472. [Google Scholar] [CrossRef] [PubMed]
- Lo, H.Y.; Yang, S.L.; Chou, P.; Chuang, J.H.; Chiang, C.Y. Completeness and timeliness of tuberculosis notification in Taiwan. BMC Public Health 2011, 11, 915. [Google Scholar] [CrossRef]
- Yichen, C.; Jiehua, L. The Main Factors Affecting the Inter-provincial Floating Population’s Unemployment in China:An Analysis of the Data of the Dynamic Monitoring Survey of Migrants by National Health and Family Planning Commission in 2015. South China Popul. 2018, 33, 10–19. [Google Scholar] [CrossRef]
- Podewils, L.J.; Bantubani, N.; Bristow, C.; Bronner, L.E.; Peters, A.; Pym, A.; Mametja, L.D. Completeness and Reliability of the Republic of South Africa National Tuberculosis (TB) Surveillance System. BMC Public Health 2015, 15, 765. [Google Scholar] [CrossRef] [PubMed]
- Mlotshwa, M.; Smit, S.; Williams, S.; Reddy, C.; Medina-Marino, A. Evaluating the electronic tuberculosis register surveillance system in Eden District, Western Cape, South Africa, 2015. Glob. Health Action 2017, 10, 1360560. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Ndisha, M.; Ngari, F.; Kipruto, H.; Cain, K.P.; Sitienei, J.; Bloss, E. A review of data quality of an electronic tuberculosis surveillance system for case-based reporting in Kenya. Eur. J. Public Health 2015, 25, 1095–1097. [Google Scholar] [CrossRef] [PubMed]
- Craig, G.M.; Daftary, A.; Engel, N.; O’Driscoll, S.; Ioannaki, A. Tuberculosis stigma as a social determinant of health: A systematic mapping review of research in low incidence countries. Int. J. Tuberc. Lung Dis. 2017, 56, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.G.; Williams, J.; Lee, A.; Bradley, K.K. Completeness and timeliness of electronic vs. conventional laboratory reporting for communicable disease surveillance—Oklahoma, 2011. Public Health Rep. 2014, 129, 261–266. [Google Scholar] [CrossRef]
- Silin, M.; Laraque, F.; Munsiff, S.S.; Crossa, A.; Harris, T.G. The impact of monitoring tuberculosis reporting delays in New York City. J. Public Health Manag. Pract. 2010, 16, E09–E17. [Google Scholar] [CrossRef]
- Garcell, H.G.; Hernandez, T.M.; Abdo, E.A.; Arias, A.V. Evaluation of the timeliness and completeness of communicable disease reporting: Surveillance in The Cuban Hospital, Qatar. Qatar Med. J. 2014, 2014, 50–56. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saeed, K.M.; Bano, R.; Asghar, R.J. Evaluation of the national tuberculosis surveillance system in Afghanistan. East Mediterr. Health J. 2013, 19, 200–207. [Google Scholar] [CrossRef] [PubMed]
| Diagnosed | ||
|---|---|---|
| Patients | % | |
| Total | 4698 | 100 |
| Age | ||
| ≤15 | 40 | 0.9 |
| 15–64 | 3658 | 77.9 |
| ≥65 | 1000 | 21.3 |
| Sex | ||
| Male | 3127 | 66.6 |
| Female | 1571 | 33.4 |
| Type of TB | ||
| PTB clinically diagnosed | 3028 | 64.5 |
| PTB laboratory-confirmed | 1299 | 27.7 |
| Pleurisy or other EPTB | 371 | 7.9 |
| Patient type | ||
| Outpatient | 3419 | 72.8 |
| Inpatient | 919 | 19.6 |
| Lab | 360 | 7.7 |
| Level of health facility | ||
| ≤1 | 702 | 14.9 |
| 2 | 1479 | 31.5 |
| 3 | 2517 | 53.6 |
| Residence | ||
| Resident | 4117 | 87.6 |
| Non-resident | 581 | 12.4 |
| County | ||
| Nanshan | 819 | 17.4 |
| Liyang | 379 | 8.1 |
| Xingyang | 441 | 9.4 |
| Yilan | 320 | 6.8 |
| Lu | 932 | 19.8 |
| Simao | 1807 | 38.5 |
| County | Total | IDRS | TBIMS | ||
|---|---|---|---|---|---|
| Missing Patients | Proportion (%) | Missing Patients | Proportion (%) | ||
| Nanshan | 819 | 50 | 6.1 | 283 | 34.6 |
| Liyang | 379 | 52 | 13.7 | 112 | 29.6 |
| Xingyang | 441 | 33 | 7.5 | 43 | 9.8 |
| Yilan | 320 | 6 | 1.9 | 7 | 2.2 |
| Lu | 932 | 4 | 0.4 | 87 | 9.3 |
| Simao | 1807 | 360 | 19.9 | 919 | 50.9 |
| Total | 4698 | 505 | 10.8 | 1451 | 30.9 |
| Variables | Total | Under-Reporting | Pearson’s Chi-Square p-Value | Crude OR (95%CI) | Adjusted OR (95%CI) | p-Value | |
|---|---|---|---|---|---|---|---|
| N | % | ||||||
| Total | 4698 | 505 | 10.7 | ||||
| Age in years | |||||||
| <15 | 40 | 9 | 22.5 | 0.04 | 2.5 (1.2–5.3) | 1.5 (0.6–3.7) | 0.4 |
| 15–64 | 3658 | 383 | 10.5 | ref | ref | ||
| ≥65 | 1000 | 113 | 11.3 | 1.1 (0.9–1.4) | 1.3 (1.0–1.6) | 0.09 | |
| Sex | |||||||
| Male | 3127 | 301 | 9.6 | 0.0005 | ref | ref | |
| Female | 1571 | 204 | 13.0 | 1.4 (1.2–1.7) | 1.1 (0.9–1.4) | 0.4 | |
| Data source | |||||||
| Outpatient | 3419 | 359 | 10.5 | 0.06 | 1.3 (0.9–1.9) | 2.7 (1.8–4.1) | <0.001 |
| Inpatient | 919 | 116 | 12.6 | 1.6 (1.0–2.4) | 0.7 (0.4–1.1) | 0.08 | |
| Lab | 360 | 30 | 8.3 | ref | ref | ||
| Level of health facility | |||||||
| ≤1 | 702 | 14 | 2.0 | <0.0001 | ref | ||
| 2 | 1479 | 110 | 7.4 | 4.0 (2.3–6.9) | 1.7 (0.8–3.6) | 0.1 | |
| 3 | 2517 | 381 | 15.1 | 8.8 (5.1–15.1) | 12.9 (6.4–25.8) | <0.001 | |
| Residence | |||||||
| Resident | 4117 | 465 | 11.3 | 0.0013 | ref | ref | |
| Non-resident | 581 | 40 | 6.9 | 0.6 (0.4–0.8) | 2.2 (1.2–4.0) | 0.009 | |
| County | |||||||
| Nanshan | 819 | 50 | 6.1 | <0.0001 | ref | ref | |
| Liyang | 379 | 52 | 13.7 | 2.5 (1.6–3.7) | 5.7 (2.8–11.6) | <0.001 | |
| Xingyang | 441 | 33 | 7.5 | 1.2 (0.8–2.0) | 4.5 (2.1–9.8) | <0.001 | |
| Yilan | 320 | 6 | 1.9 | 0.3 (0.1–0.7) | 1.3 (0.4–3.8) | 0.6 | |
| Lu | 932 | 4 | 0.4 | 0.1 (0.0–0.2) | 0.0 (0.0–0.1) | <0.001 | |
| Simao | 1807 | 360 | 19.9 | 3.8 (2.8–5.2) | 4.1 (2.2–7.6) | <0.001 | |
| Variables | Total | Under-Reporting | Pearson’s Chi-Square p-Value | Crude OR (95%CI) | Adjusted OR (95%CI) | p-Value | |
|---|---|---|---|---|---|---|---|
| N | % | ||||||
| Total | 4698 | 1451 | 30.9 | ||||
| Age in years | |||||||
| <15 | 40 | 16 | 40.0 | 0.0005 | 1.6 (0.8–3.0) | 1.0 (0.5–2.0) | 0.9 |
| 15–64 | 3658 | 1079 | 29.5 | ref | ref | ||
| ≥65 | 1000 | 356 | 35.6 | 1.3 (1.1–1.5) | 1.7 (1.4–2.0) | <0.001 | |
| Sex | |||||||
| Male | 3127 | 909 | 29.07 | 0.0001 | ref | ref | |
| Female | 1571 | 542 | 34.50 | 1.29 (1.13–1.46) | 1.04 (0.89–1.21) | 0.6 | |
| Data source | |||||||
| Outpatient | 3419 | 807 | 23.60 | <0.0001 | 0.54 (0.43–0.68) | 0.30 (0.21–0.43) | <0.001 |
| Inpatient | 919 | 513 | 55.82 | 2.21 (1.72–2.84) | 0.54 (0.37–0.79) | 0.002 | |
| Lab | 360 | 131 | 36.39 | ref | ref | ||
| Type of TB | |||||||
| PTB clinically diagnosed | 3028 | 984 | 32.50 | <0.0001 | 1.98 (1.69–2.32) | 2.54 (1.94–3.32) | <0.001 |
| PTB laboratory-confirmed | 1299 | 254 | 19.55 | ref | ref | ||
| Pleurisy or other EPTB | 371 | 213 | 57.41 | 5.55 (4.33–7.10) | 9.27 (6.50–13.23) | <0.001 | |
| Level of medical institution | |||||||
| ≤1 | 702 | 14 | 1.99 | <0.0001 | ref | ref | |
| 2 | 1479 | 110 | 7.44 | 3.95 (2.25–6.94) | 1.77 (0.86–3.65) | 0.1 | |
| 3 | 2517 | 381 | 15.14 | 8.77 (5.11–15.05) | 10.01 (4.99–20.11) | <0.001 | |
| Residence | |||||||
| Local | 4117 | 1147 | 27.86 | <0.0001 | ref | ref | |
| Non-resident | 581 | 304 | 52.32 | 2.84 (2.38–3.39) | 18.80 (13.77–25.67) | <0.0001 | |
| County | |||||||
| Nanshan | 819 | 283 | 34.55 | <0.0001 | ref | ref | |
| Liyang | 379 | 112 | 29.55 | 0.79 (0.61–1.03) | 1.56 (1.10–2.20) | 0.01 | |
| Xingyang | 441 | 43 | 9.75 | 0.20 (0.14–0.29) | 0.47 (0.31–0.70) | <0.001 | |
| Yilan | 320 | 7 | 2.19 | 0.04 (0.02–0.09) | 0.31 (0.14–0.69) | 0.004 | |
| Lu | 932 | 87 | 9.33 | 0.20 (0.15–0.25) | 0.11 (0.08–0.16) | <0.001 | |
| Simao | 1807 | 919 | 50.86 | 1.96 (1.65–2.33) | 5.00 (3.80–6.57) | <0.001 | |
| Key Variables | Medical Records and IDRS | Medical Records and TBIMS | ||
|---|---|---|---|---|
| Patients Reviewed in IDRS | Inconsistent with Medical Records | Patients Reviewed in TBIMS | Inconsistent with Medical Records | |
| Total records | ||||
| National ID number | 161 | 3 (1.9%) | 148 | 3 (2.0%) |
| Patient name | 171 | 1 (0.6%) | 170 | 0 (0%) |
| Address | 169 | 18 (10.7%) | 170 | 12 (7.1%) |
| Smear status | - | - | 170 | 4 (2.4%) |
| DST status | - | - | 17 | 0 (0%) |
| Diagnosis | - | - | 170 | 1 (0.6%) |
| Treatment outcome | - | - | 168 | 1 (0.6%) |
| Diagnosis date | 171 | 14 (8.2%) | 170 | 5 (2.9%) |
| Registration | - | - | 170 | 1 (0.6%) |
| Date of follow-up examination at the end of 2nd month | - | - | 152 | 6 (3.9%) |
| Date of end course examination | - | - | 157 | 22 (14.0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, T.; Yang, L.; Smith-Jeffcoat, S.E.; Wang, A.; Guo, H.; Chen, W.; Du, X.; Zhang, H. Assessing the Quality of Reporting to China’s National TB Surveillance Systems. Int. J. Environ. Res. Public Health 2021, 18, 2264. https://doi.org/10.3390/ijerph18052264
Li T, Yang L, Smith-Jeffcoat SE, Wang A, Guo H, Chen W, Du X, Zhang H. Assessing the Quality of Reporting to China’s National TB Surveillance Systems. International Journal of Environmental Research and Public Health. 2021; 18(5):2264. https://doi.org/10.3390/ijerph18052264
Chicago/Turabian StyleLi, Tao, Lijia Yang, Sarah E. Smith-Jeffcoat, Alice Wang, Hui Guo, Wei Chen, Xin Du, and Hui Zhang. 2021. "Assessing the Quality of Reporting to China’s National TB Surveillance Systems" International Journal of Environmental Research and Public Health 18, no. 5: 2264. https://doi.org/10.3390/ijerph18052264
APA StyleLi, T., Yang, L., Smith-Jeffcoat, S. E., Wang, A., Guo, H., Chen, W., Du, X., & Zhang, H. (2021). Assessing the Quality of Reporting to China’s National TB Surveillance Systems. International Journal of Environmental Research and Public Health, 18(5), 2264. https://doi.org/10.3390/ijerph18052264






