Social Vulnerability and Access to Kidney Transplantation
Abstract
1. Background
2. Methods
2.1. Study Design and Participants
2.2. Exposure and Outcome Measures
- Poverty rate;
- Population with no diploma;
- Per capita income;
- Single parent household;
- No vehicle;
- People of color;
- More than 1 person per room;
- Unemployment rate;
- Population with disability;
- No English language;
- Age under 18;
- Multi-unit structures;
- Age 65 up;
- Mobile homes;
- In group quarters.
2.3. Primary Outcomes
2.4. Data Collection
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Participants and Descriptive Data
3.2. Main Results
3.2.1. Social Vulnerability and Its Association with Preemptive Transplant Access and Dialysis History (Table 2 and Table 3)
| Dialysis Vintage | N | Mean | Std Dev | Minimum | 25th Pctl | Median | 75th Pctl | Maximum |
|---|---|---|---|---|---|---|---|---|
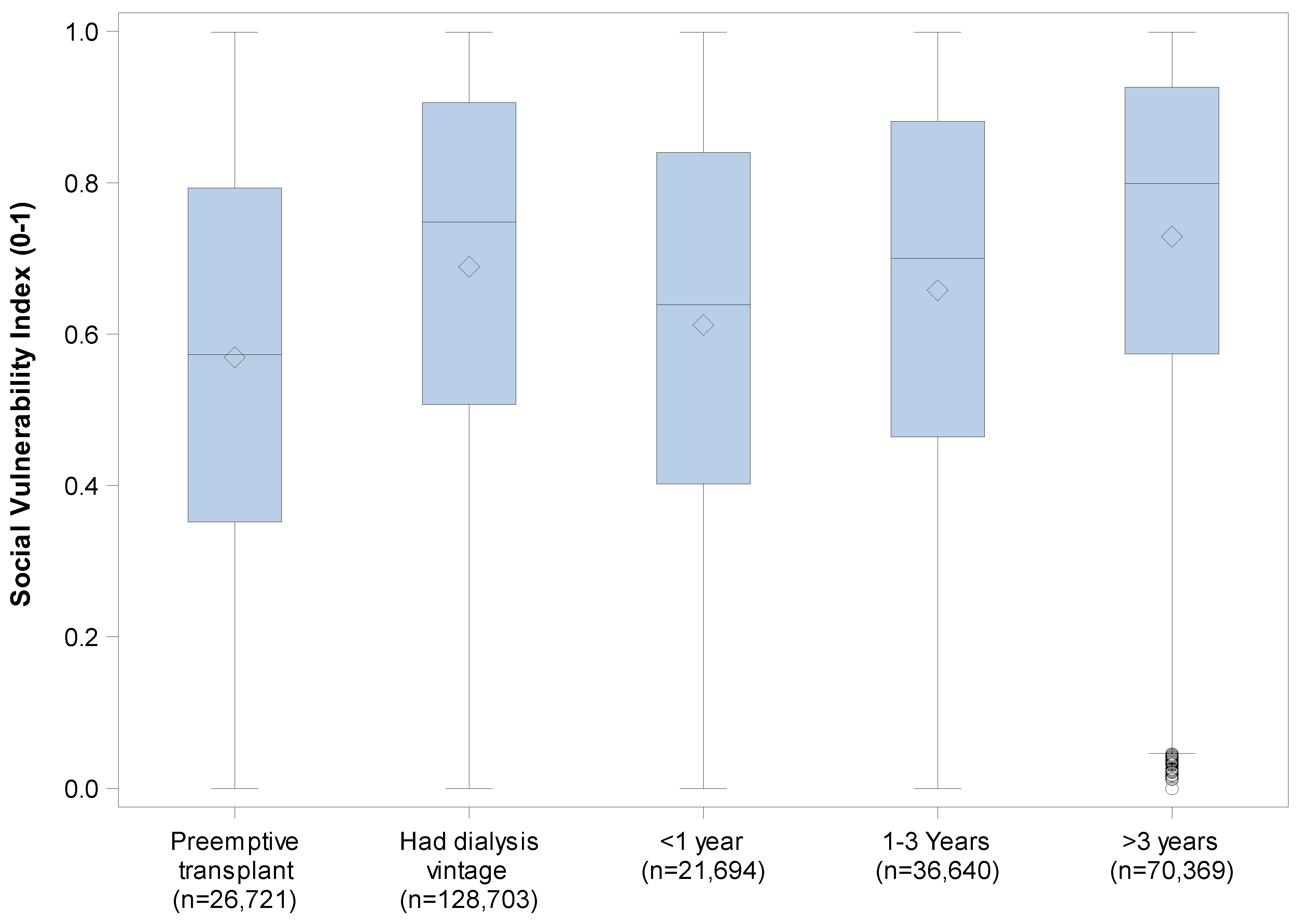
| Preemptive kidney transplant | 26,721 | 0.57 | 0.26 | 0.00 | 0.35 | 0.57 | 0.79 | 1.00 |
| Pre-transplant dialysis | 128,703 | 0.69 | 0.25 | 0.00 | 0.51 | 0.75 | 0.91 | 1.00 |
| SVI | [0, 0.25) (n = 11,787) | [0.25, 0.5) (n = 30,638) | [0.5, 0.75) (n = 40,855) | [0.5, 0.75) (n = 72,144) | Total (n = 155,424) |
|---|---|---|---|---|---|
| Preemptive Kidney transplant | 3581 (30.4%) | 7536 (24.6%) | 7599 (18.6%) | 8085 (11.1%) | 26,721 |
| Pre-transplant Dialysis | 8206 (69.6%) | 23,102 (75.4%) | 33,256 (81.4%) | 64,139 (88.9%) | 128,703 |
| Model # | Independent Variable | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|---|
| 1 | BMI ≥ 35 | 1.26 | 1.11–1.42 | 0.0002 |
| 1 | Patient/s Gender M vs. F | 1.70 | 1.57–1.84 | <0.0001 |
| 1 | Age at transplant (yrs) | 0.97 | 0.97–0.97 | <0.0001 |
| 1 | Symptomatic peripheral vascular disease | 1.53 | 1.32–1.76 | <0.0001 |
| 1 | Candidate had diabetes of any type | 1.72 | 1.58–1.88 | <0.0001 |
| 1 | Social Vulnerability Index (0–1) per 0.1 increase | 1.13 | 1.11–1.15 | <0.0001 |
| 2 | BMI ≥ 35 | 1.26 | 1.12–1.42 | 0.0002 |
| 2 | Patient/s Gender M vs. F | 1.69 | 1.56–1.83 | <0.0001 |
| 2 | Age at transplant (yrs) | 0.97 | 0.97–0.97 | <0.0001 |
| 2 | Symptomatic peripheral vascular disease | 1.53 | 1.32–1.76 | <0.0001 |
| 2 | Candidate had diabetes of any type | 1.71 | 1.57–1.87 | <0.0001 |
| 2 | Social Vulnerability Index 4 groups-overall | <0.0001 | ||
| 2 | Social Vulnerability Index: [0.75, 1] vs. [0, 0.25) | 2.23 | 1.91–2.60 | <0.0001 |
| 2 | Social Vulnerability Index: [0.5, 0.75) vs. [0, 0.25) | 1.49 | 1.27–1.74 | <0.0001 |
| 2 | Social Vulnerability Index: [0.25, 0.5) vs. [0, 0.25) | 1.18 | 1.00–1.39 | 0.0479 |
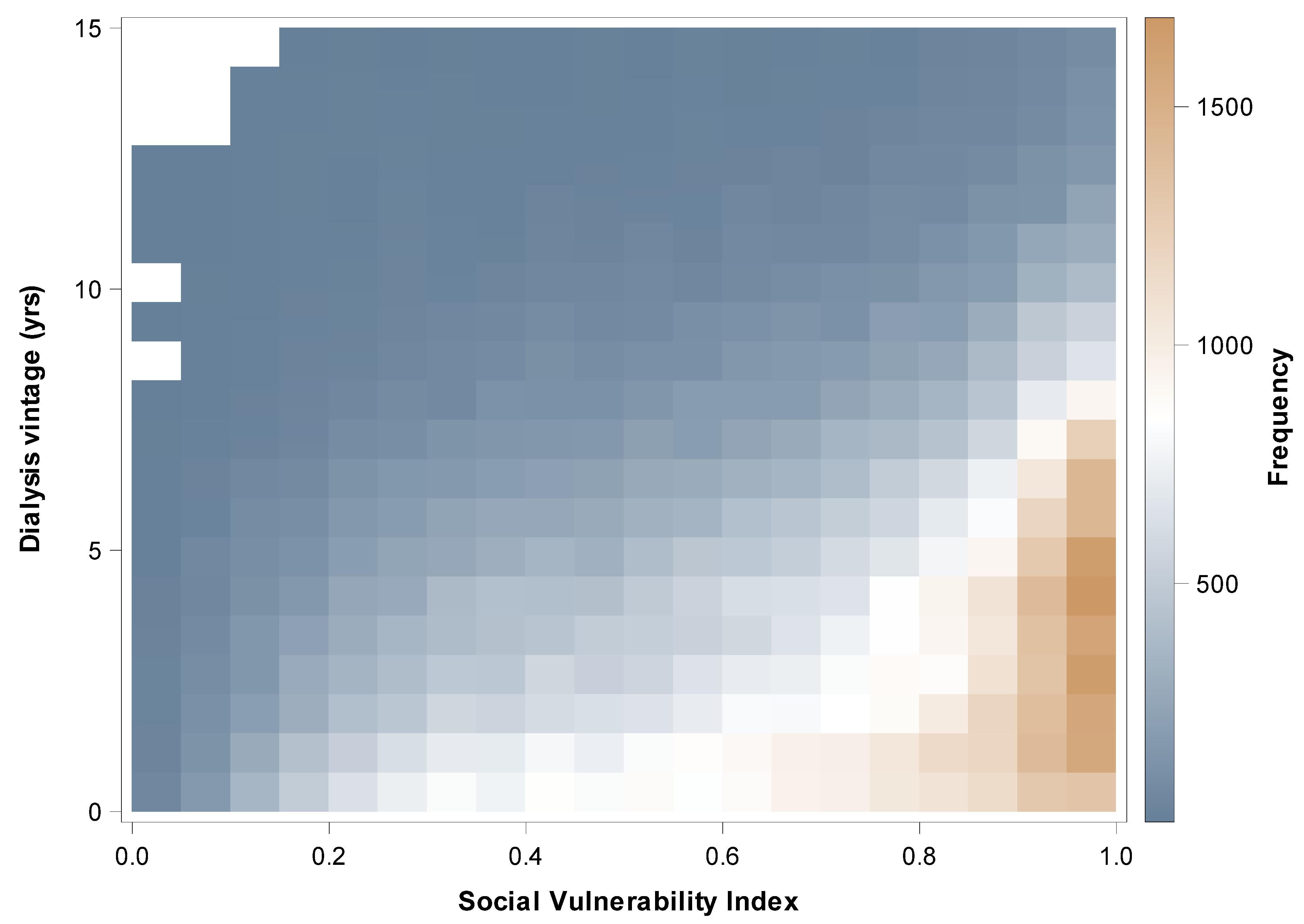
3.2.2. Pre-Transplant Dialysis Duration and SVI (Table 5, Table 6 and Table 7, Figure 1 and Figure 2)
| Dialysis Vintage | N | Mean | Std Dev | Minimum | 25th Pctl | Median | 75th Pctl | Maximum |
|---|---|---|---|---|---|---|---|---|
| <1 year | 21,694 | 0.61 | 0.26 | 0.00 | 0.40 | 0.64 | 0.84 | 1.00 |
| 1–3 Years | 36,640 | 0.66 | 0.25 | 0.00 | 0.46 | 0.70 | 0.88 | 1.00 |
| >3 years | 70,369 | 0.73 | 0.23 | 0.00 | 0.57 | 0.80 | 0.93 | 1.00 |
| Social Vulnerability Index Four Groups | N | Mean | Std Dev | Minimum | 25th Pctl | Median | 75th Pctl | Maximum |
|---|---|---|---|---|---|---|---|---|
| [0, 0.25) | 8206 | 2.84 | 2.52 | 0.00 | 0.89 | 2.20 | 4.13 | 14.93 |
| [0.25, 0.5) | 23,102 | 3.25 | 2.70 | 0.00 | 1.10 | 2.62 | 4.71 | 14.98 |
| [0.5, 0.75) | 33,256 | 3.66 | 2.84 | 0.00 | 1.37 | 3.07 | 5.30 | 15.00 |
| [0.75, 1] | 64,139 | 4.46 | 3.07 | 0.00 | 1.98 | 4.03 | 6.38 | 15.00 |
| Independent Variable | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| SVI: [0.75, 1] vs. [0, 0.25) | 3.43 | 3.31–3.55 | <0.0001 |
| SVI: [0.5, 0.75) vs. [0, 0.25) | 1.94 | 1.87–2.02 | <0.0001 |
| SVI: [0.25, 0.5) vs. [0, 0.25) | 1.37 | 1.32–1.43 | <0.0001 |
| BMI ≥ 35 | 1.22 | 1.18–1.26 | <0.0001 |
| Male vs. Female | 1.20 | 1.17–1.22 | <0.0001 |
| Age at transplant (yrs) | 0.999 | 0.998–1.000 | 00.0130 |
| Symptomatic peripheral vascular disease | 1.20 | 1.16–1.24 | <0.0001 |
| Candidate had diabetes of any type | 1.27 | 1.24–1.30 | <0.0001 |
3.2.3. Spearman Correlation Coefficients Between 15 Indicators and SVI (Table 8)
| Item | N | Rho |
|---|---|---|
| Poverty rate % | 155,383 | 0.89 |
| Population with no diploma % | 155,394 | 0.84 |
| Per capita income | 155.367 | −0.80 |
| Single parent households % | 133.350 | 0.79 |
| No vehicle % | 155.371 | 0.70 |
| People of color % | 155,396 | 0.65 |
| More than one person per room % | 155,371 | 0.64 |
| Unemployment rate | 155,370 | 0.64 |
| Population with disability % | 155,389 | 0.50 |
| No English language % | 155,396 | 0.46 |
| Age under 18% | 155,396 | 0.24 |
| Multi unit structures % | 155,382 | 0.22 |
| Age 65 up % | 155,396 | −0.20 |
| Mobile homes % | 155,382 | 0.16 |
| In group quarters % | 155,396 | 0.14 |
4. Discussion
4.1. Socioeconomic Factors and Access to Kidney Transplant
4.2. Benefits of Using the Social Vulnerability Index (SVI) Compared to Other Indices
4.3. Key Indicators Within the SVI and Access to Kidney Transplant
4.4. Use of SVI and Suggested Target Interventions for Improving Access to Kidney Transplant
4.5. The Uniqueness of Our Study
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACS | American Community Survey |
| CDC | Centers for Disease Control and Prevention |
| SES | Socio-economic status |
| SVI | Social Vulnerability Index |
| U.S. | United States |
| SVI | Social Vulnerability Index |
| SRTR | Scientific Registry of Transplant Recipients |
References
- Schold, J.D.; Gregg, J.A.; Harman, J.S.; Hall, A.G.; Patton, P.R.; Meier-Kriesche, H.U. Barriers to evaluation and wait listing for kidney transplantation. Clin. J. Am. Soc. Nephrol. 2011, 6, 1760–1767. [Google Scholar] [CrossRef] [PubMed]
- Patzer, R.E.; McClellan, W.M. Influence of race, ethnicity, and socioeconomic status on kidney disease. Nat. Rev. Nephrol. 2012, 8, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K. Area deprivation and widening inequalities in US mortality, 1969–1998. Am. J. Public Health 2003, 93, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Aufhauser, D.D.J.; Peng, A.W.; Murken, D.R.; Concors, S.J.; Abt, P.L.; Sawinski, D.; Bloom, R.D.; Reese, P.P.; Levine, M.H. Impact of prolonged dialysis prior to renal transplantation. Clin. Transplant. 2018, 32, e13260. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, B.E.; Gregory, E.W.; Hallisey, E.J.; Heitgerd, J.L.; Lewis, B. A social vulnerability index for disaster management. J. Homel. Secur. Emerg. Manag. 2011, 8, 3. [Google Scholar] [CrossRef]
- Meier-Kriesche, H.U.; Kaplan, B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: A paired donor kidney analysis. Transplantation 2002, 74, 1377–1381. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Schappe, T.; Peskoe, S.; Mohottige, D.; Chan, N.W.; Bhavsar, N.A.; Boulware, L.E.; Pendergast, J.; Kirk, A.D.; McElroy, L.M. A comparison of deprivation indices and application to transplant populations. Am. J. Transplant. 2023, 23, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Butani, L.; Perez, R.V. Effect of pretransplant dialysis modality and duration on long-term outcomes of children receiving renal transplants. Transplant. 2011, 91, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Cutter, S.L.; Boruff, B.J.; Shirley, W.L. Social vulnerability to environmental hazards. Soc. Sci. Q. 2003, 84, 242–261. [Google Scholar] [CrossRef]
- Axelrod, D.A.; Guidinger, M.K.; Finlayson, S.; Schaubel, D.E.; Goodman, D.C.; Chobanian, M.; Merion, R.M. Rates of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA 2008, 299, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Kind, A.J.H.; Buckingham, W.R. Making neighborhood-disadvantage metrics accessible—the Neighborhood Atlas. N. Engl. J. Med. 2018, 378, 2456–2458. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.A.; Cubbin, C.; Egerter, S.; Chideya, S.; Marchi, K.S.; Metzler, M.; Posner, S. Socioeconomic status in health research: One size does not fit all. JAMA 2005, 294, 2879–2888. [Google Scholar] [CrossRef]
- Patzer, R.E.; Paul, S.; Plantinga, L.; Krisher, J.; Pastan, S.O. Variation in dialysis facility referral for kidney transplantation among patients with end-stage renal disease in Georgia. JAMA 2015, 314, 582–594. [Google Scholar] [CrossRef]
- Epstein, A.M.; Ayanian, J.Z.; Keogh, J.H.; Noonan, S.J.; Armistead, N.; Cleary, P.D.; Weissman, J.S.; David-Kasdan, J.A.; Carlson, D.; Fuller, J.; et al. Racial disparities in access to renal transplantation—Clinically appropriate or due to underuse or overuse? N. Engl. J. Med. 2000, 343, 1537–1544. [Google Scholar] [CrossRef]
- Taylor, L.A.; Coyle, C.E.; Ndumele, C.; Rogan, E.; Canavan, M.; Curry, L.A.; Bradley, E.H. Leveraging the social determinants of health: What works? PLoS ONE 2016, 11, e0160217. [Google Scholar] [CrossRef] [PubMed]
- Beach, M.C.; Price, E.G.; Gary, T.L.; Robinson, K.A.; Gozu, A.; Palacio, A.; Smarth, C.; Jenckes, M.W.; Feuerstein, C.; Bass, E.B.; et al. Cultural competence: A systematic review of healthcare provider educational interventions. Med. Care 2005, 43, 356–373. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Grams, M.E.; Massie, A.B.; Schold, J.D.; Chen, B.P.; Segev, D.L. Trends in the inactive kidney transplant waitlist and implications for candidate survival. Am. J. Transplant. 2017, 17, 3134–3141. [Google Scholar] [CrossRef] [PubMed]
- Massie, A.B.; Caffo, B.S.; Gentry, S.E.; Hall, E.C.; Axelrod, D.A.; Lentine, K.L.; Schnitzler, M.A.; Gheorghian, A.; Salvalaggio, P.R.; Segev, D.L. MELD exceptions and rates of waiting list outcomes. Am. J. Transplant. 2011, 11, 2362–2371. [Google Scholar] [CrossRef] [PubMed]
- Health Resources and Services Administration (HRSA). Scientific Registry of Transplant Recipients (SRTR). 2020. Available online: https://www.srtr.org/ (accessed on 10 October 2023).
| Patient Characteristics | n | Statistics | Median (IQR) Min Max |
|---|---|---|---|
| Patient’s Gender, n (%) | 155,424 | ||
| Female | 60,777 (39.1%) | ||
| Male | 94,647 (60.9%) | ||
| Age at transplant (yrs), mean (sd) | 155,424 | 52.1 (13.8) | 54.0 (42.0–63.0) 18.0 89.0 |
| Patient’s Race, n (%) | 155,424 | ||
| White | 72,809 (46.8%) | ||
| Black or African American | 41,884 (26.9%) | ||
| Hispanic/Latino | 26,944 (17.3%) | ||
| Asian | 10,772 (6.9%) | ||
| American Indian or Alaska Native | 1354 (0.9%) | ||
| Multi-racial | 1005 (0.6%) | ||
| Native Hawaiian or Other Pacific Islander | 656 (0.4%) | ||
| Social Vulnerability Index (0–1), mean (sd) | 155,424 | 0.67 (0.25) | 0.72 (0.47–0.89) 0.0 1.0 |
| Social Vulnerability Index, n (%) | 155,424 | ||
| [0, 0.25) | 11,787 (7.6%) | ||
| [0.25, 0.5) | 30,638 (19.7%) | ||
| [0.5, 0.75) | 40,855 (26.3%) | ||
| [0.75, 1] | 72,144 (46.4%) | ||
| First graft for patient, n (%) | 155,424 | 138,500 (89.1%) | |
| Had previous Transplants, n (%) | 155,424 | 19,262 (12.4%) | |
| Donor Type, n (%) | 155,424 | ||
| Deceased | 106,463 (68.5%) | ||
| Living | 48,961 (31.5%) | ||
| Pre-transplant dialysis, n (%) | 155,424 | 128,703 (82.8%) | |
| Dialysis Vintage duration, n (%) | 155,424 | ||
| <1 year | 21,694 (14.0%) | ||
| 1–3 Years | 36,640 (23.6%) | ||
| >3 years | 70,369 (45.3%) | ||
| Preemptive transplant | 26,721 (17.2%) | ||
| Dialysis Vintage duration (yrs), mean (sd) | 155,424 | 3.3 (3.1) | 2.6 (0.6–5.1) 0.0 15.0 |
| Dialysis Vintage duration in those who had dialysis (yrs), mean (sd) | 128,703 | 3.9 (3.0) | 3.4 (1.5–5.7) 0.0 15.0 |
| Symptomatic peripheral vascular disease, n (%) | 154,230 | 15,083 (9.8%) | |
| Diabetes of any type, n (%) | 155,305 | 53,417 (34.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adebiyi, O.; Li, Y.; Lane, K.; Ahsan, R.; Sharfuddin, A.; Yenebere, P.; Jan, M.Y.; Yaqub, M.S. Social Vulnerability and Access to Kidney Transplantation. Kidney Dial. 2025, 5, 27. https://doi.org/10.3390/kidneydial5030027
Adebiyi O, Li Y, Lane K, Ahsan R, Sharfuddin A, Yenebere P, Jan MY, Yaqub MS. Social Vulnerability and Access to Kidney Transplantation. Kidney and Dialysis. 2025; 5(3):27. https://doi.org/10.3390/kidneydial5030027
Chicago/Turabian StyleAdebiyi, Oluwafisayo, Yang Li, Kathleen Lane, Raza Ahsan, Asif Sharfuddin, Priya Yenebere, Muhammad Y. Jan, and Muhammad Sohail Yaqub. 2025. "Social Vulnerability and Access to Kidney Transplantation" Kidney and Dialysis 5, no. 3: 27. https://doi.org/10.3390/kidneydial5030027
APA StyleAdebiyi, O., Li, Y., Lane, K., Ahsan, R., Sharfuddin, A., Yenebere, P., Jan, M. Y., & Yaqub, M. S. (2025). Social Vulnerability and Access to Kidney Transplantation. Kidney and Dialysis, 5(3), 27. https://doi.org/10.3390/kidneydial5030027






