A Case of Brachial Artery Thrombosis Caused by Massage of an Occluded Arteriovenous Graft
Abstract
:1. Introduction
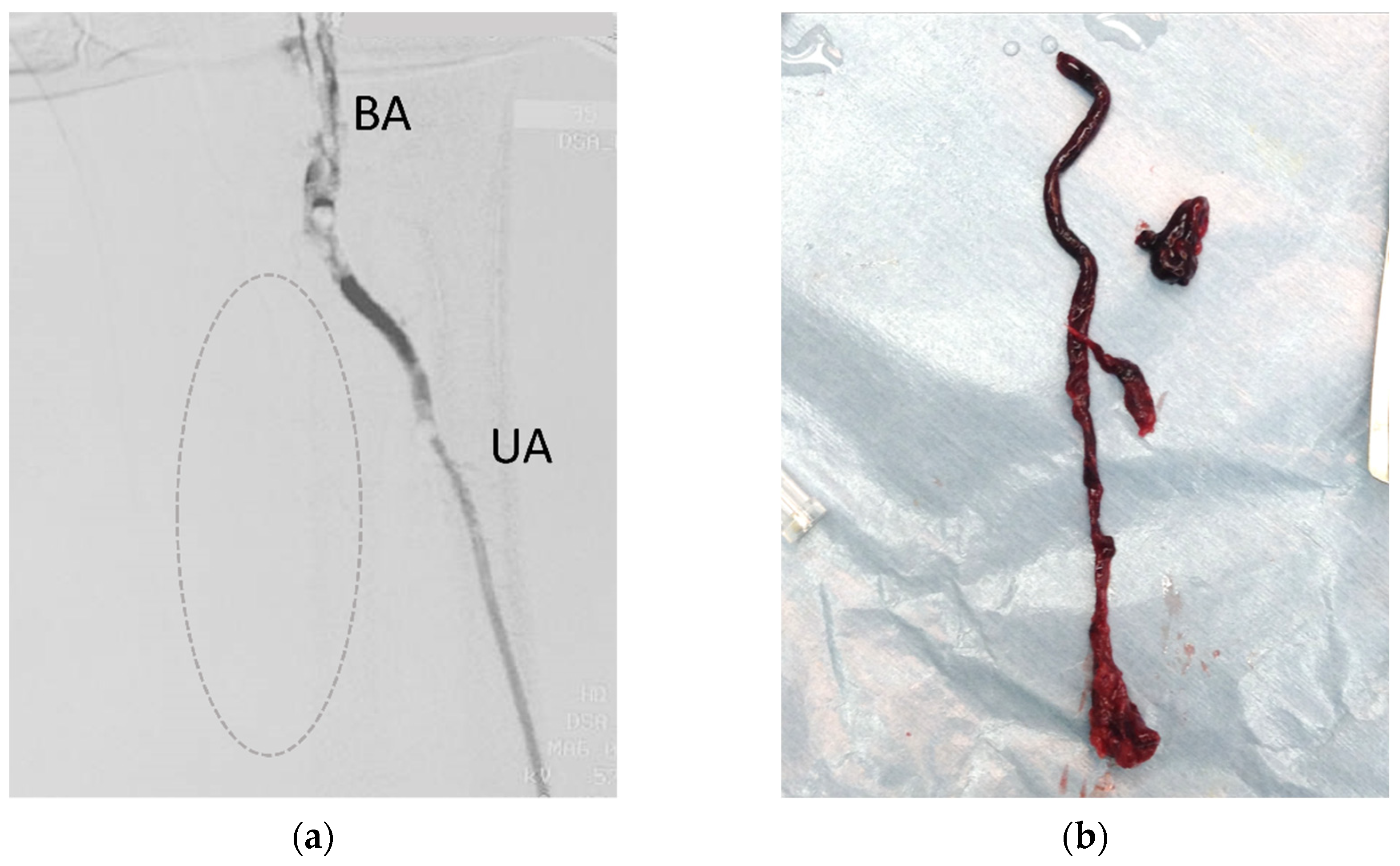
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- MacRae, J.M.; Dipchand, C.; Oliver, M.; Moist, L.; Lok, C.; Clark, E.; Hiremath, S.; Kappel, J.; Kiaii, M.; Luscombe, R.; et al. Arteriovenous Access Failure, Stenosis, and Thrombosis. Can. J. Kidney Health Dis. 2016, 3, 2054358116669126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhan, G.; Antoniou, G.A.; Nikam, M.; Mitra, S.; Farquharson, F.; Brittenden, J.; Chalmers, N. A Meta-analysis of Randomized Trials Comparing Surgery versus Endovascular Therapy for Thrombosed Arteriovenous Fistulas and Grafts in Hemodialysis. Cardiovasc. Interv. Radiol. 2013, 36, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, B. Massaging Thrombosed PTFE Hemodialysis Access Graft—Recipe for Disaster. J. Vasc. Access 2007, 8, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Major, M.R.; Higgins, J.P. Nonoperative Management of Acute Upper Limb Ischemia. Hand 2016, 11, 131–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017, 135, e686–e725. [Google Scholar] [CrossRef] [PubMed]
- Gallieni, M.; Hollenbeck, M.; Inston, N.; Kumwenda, M.; Powell, S.; Tordoir, J.; Al Shakarchi, J.; Berger, P.; Bolignano, D.; Cassidy, D.; et al. Clinical practice guideline on peri- and postoperative care of arteriovenous fistulas and grafts for haemodialysis in adults. Nephrol. Dial. Transplant. 2019, 34, ii1–ii42. [Google Scholar] [CrossRef] [PubMed]
- Schmidli, J.; Widmer, M.K.; Basile, C.; de Donato, G.; Gallieni, M.; Gibbons, C.P.; Haage, P.; Hamilton, G.; Hedin, U.; Kamper, L.; et al. Editor’s Choice—Vascular Access: 2018 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2018, 55, 757–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharif-Hassanabadi, M. Fatal pulmonary embolism after hemodialysis vascular access declotting. Am. J. Case Rep. 2014, 15, 172–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCarthy, W.J.; Flinn, W.R.; Yao, J.S.; Williams, L.R.; Bergan, J.J. Result of bypass grafting for upper limb ischemia. J. Vasc. Surg. 1986, 3, 741–746. [Google Scholar] [CrossRef] [Green Version]
- Bae, M.; Chung, S.W.; Lee, C.W.; Choi, J.; Song, S.; Kim, A.S.-P. Upper Limb Ischemia: Clinical Experiences of Acute and Chronic Upper Limb Ischemia in a Single Center. Korean J. Thorac. Cardiovasc. Surg. 2015, 48, 246–251. [Google Scholar] [CrossRef]
- Córdova, M.D. Acute ischaemia as a consequence of arteriovenous fistula massage in haemodialysis. Nefrología 2009, 29, 367–368. [Google Scholar] [CrossRef]
- Comerota, A.J.; Weaver, F.A.; Hosking, J.D.; Froehlich, J.; Folander, H.; Sussman, B.; Rosenfield, K. Results of a prospective, randomized trial of surgery versus thrombolysis for occluded lower extremity bypass grafts. Am. J. Surg. 1996, 172, 105–112. [Google Scholar] [CrossRef]
- Ravn, H.; Björck, M. Popliteal Artery Aneurysm with Acute Ischemia in 229 Patients. Outcome after Thrombolytic and Surgical Therapy. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 690–695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olinic, D.-M.; Stanek, A.; Tătaru, D.-A.; Homorodean, C.; Olinic, M. Acute Limb Ischemia: An Update on Diagnosis and Management. J. Clin. Med. 2019, 8, 1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-Niedenfuhr, M.; Vazquez, T.; Nearn, L.; Ferreira, B.; Parkin, I.; Sanudo, J.R. Variations of the arterial pattern in the upper limb revisited: A morphological and statistical study, with a review of the literature. J. Anat. 2001, 199, 547–566. [Google Scholar] [CrossRef] [PubMed]
- Daenen, K.; Andries, A.; Mekahli, D.; Van Schepdael, A.; Jouret, F.; Bammens, B. Oxidative stress in chronic kidney disease. Pediatr. Nephrol. 2018, 34, 975–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norgren, L.; Hiatt, W.; Dormandy, J.; Nehler, M.; Harris, K.; Fowkes, F. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45, S5–S67. [Google Scholar] [CrossRef] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsue, T.; Kuroki, Y.; Naganuma, T.; Takemoto, Y.; Uchida, J. A Case of Brachial Artery Thrombosis Caused by Massage of an Occluded Arteriovenous Graft. Kidney Dial. 2021, 1, 74-78. https://doi.org/10.3390/kidneydial1010011
Matsue T, Kuroki Y, Naganuma T, Takemoto Y, Uchida J. A Case of Brachial Artery Thrombosis Caused by Massage of an Occluded Arteriovenous Graft. Kidney and Dialysis. 2021; 1(1):74-78. https://doi.org/10.3390/kidneydial1010011
Chicago/Turabian StyleMatsue, Taisuke, Yoshikazu Kuroki, Toshihide Naganuma, Yoshiaki Takemoto, and Junji Uchida. 2021. "A Case of Brachial Artery Thrombosis Caused by Massage of an Occluded Arteriovenous Graft" Kidney and Dialysis 1, no. 1: 74-78. https://doi.org/10.3390/kidneydial1010011







