CT Radiomics and Clinical Feature Model to Predict Lymph Node Metastases in Early-Stage Testicular Cancer
Abstract
Simple Summary
Abstract
1. Introduction
- (1)
- The radiomics features extracted from retroperitoneal lymph nodes might potentially predict TGCT recurrence.
- (2)
- Integrating important clinical factors, including age, histotype, AFP, ß-HCG, and BMI, into a combined clinical-radiomics model might add an incremental value to predict TGCT recurrence.
2. Materials and Methods
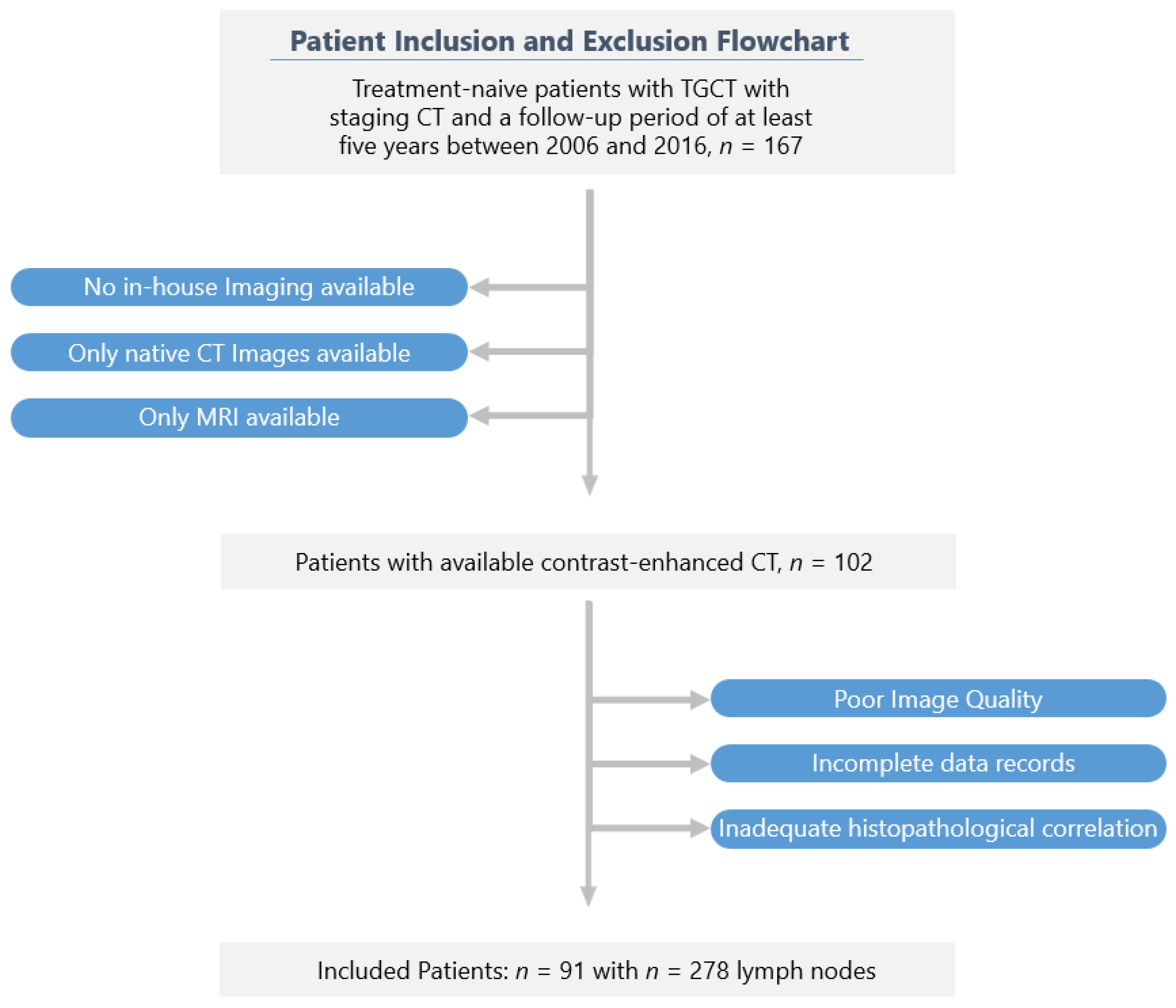
2.1. Patients and Imaging Protocol
2.2. Segmentation and Radiomic Feature Extraction
2.3. Feature Selection and Development of the Predictive Radiomics Model
2.4. Development of the Clinical and the Combined Prediction Models
3. Results
3.1. Clinical Features
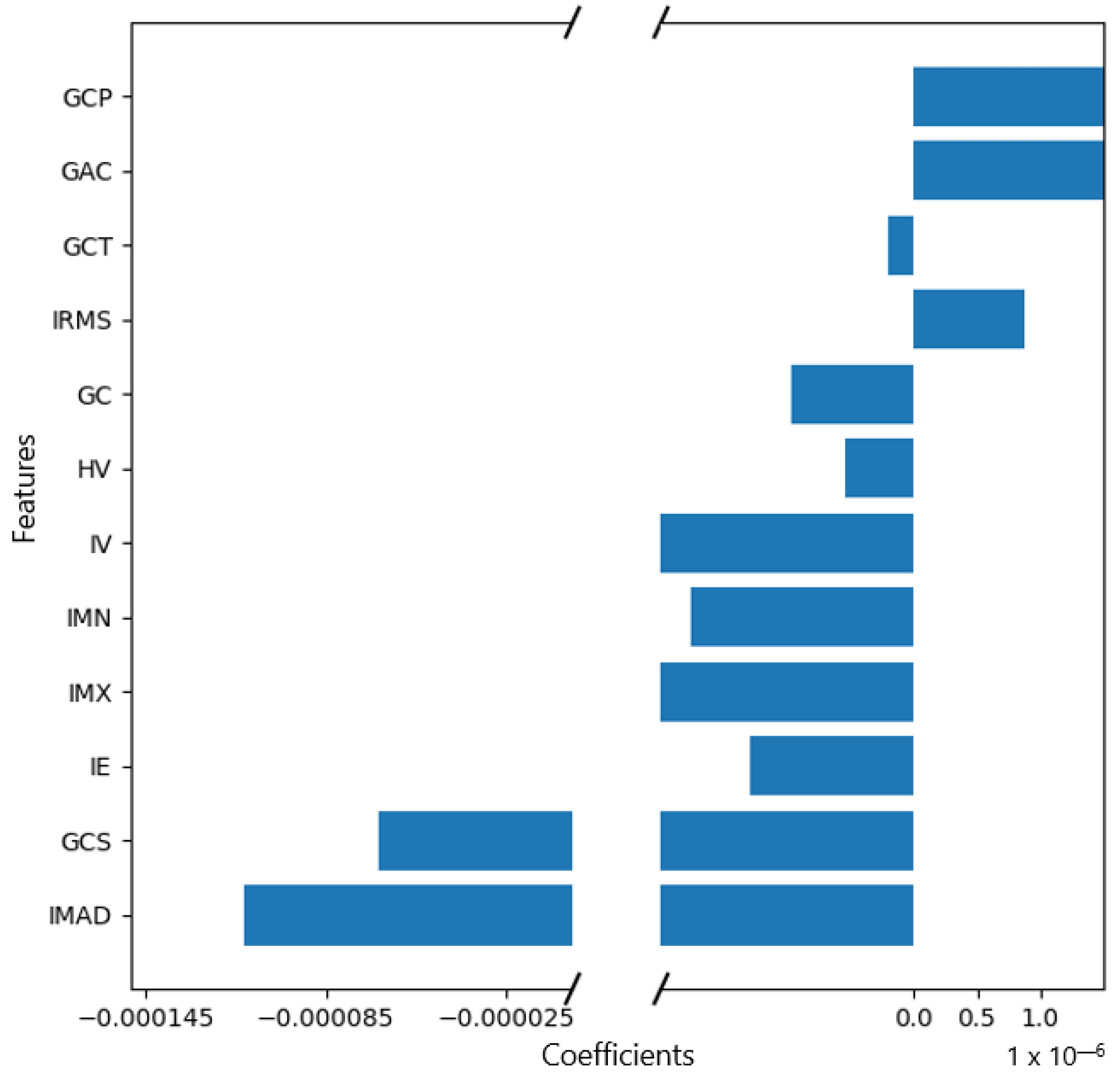
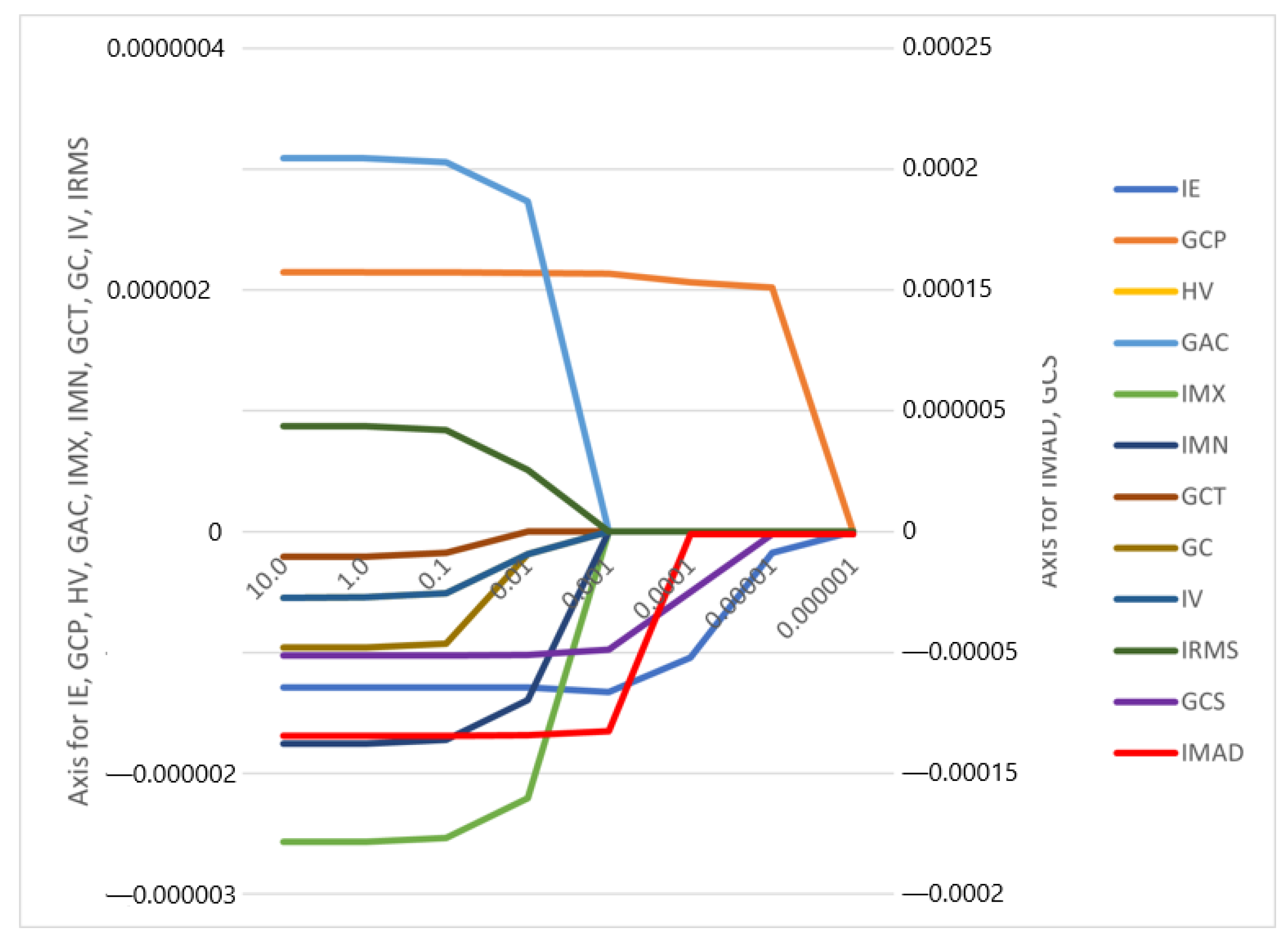
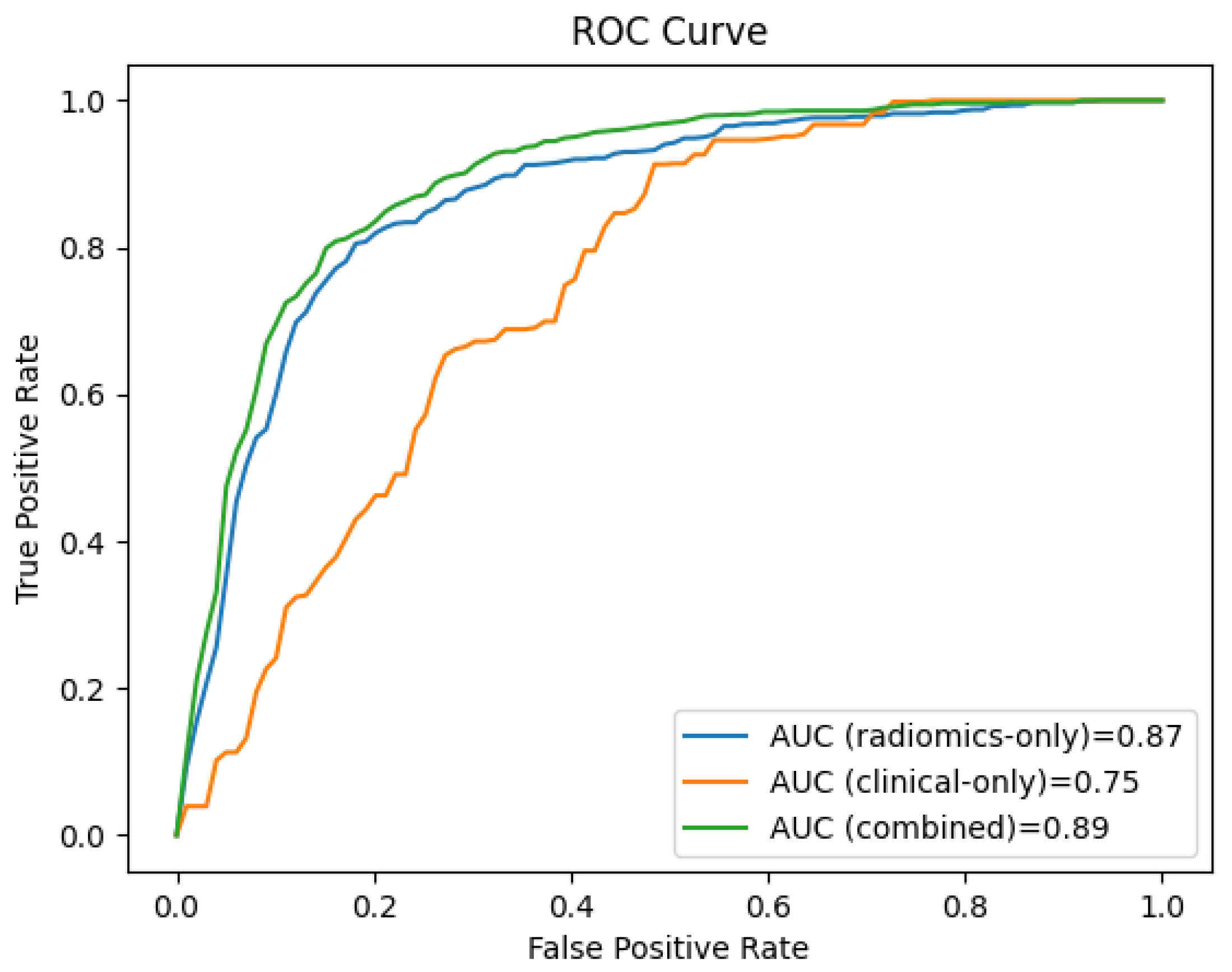
3.2. Feature Selection and Performance of the Radiomics Prediction Model
3.3. Performance of the Clinical and the Combined Prediction Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AFP | Alpha-fetoprotein |
| AUC | Area under the curve |
| CT | Computed tomography |
| β-HCG | Beta human chorionic gonadotropin |
| LNs | Lymph nodes |
| LNM | Lymph node metastases |
| LR | Logistic regression |
| ML | Machine learning |
| ROC | Receiver operating curve |
| ROI | Region of interest |
| TGCT | Testicular germ cell tumour |
Appendix A
| Setting | Determination |
|---|---|
| Bin Method | FBN |
| Bin Amount | 32 |
| LoG Filter | 0 |
| LoG Sigma | 2 |
| Matrix Aggregation | 3D Average |
| Method | Directions |
| Resample Filter | 1 |
| Resample Spacing X | 1 |
| Resample Spacing Y | 1 |
| Resample Spacing Z | 1 |
| Second-Order Distance | 1 |
| Threshold Filter | 0 |
| Radiomics Features of First Order | Radiomics Features of Second Order: Gray Level Co-Occurrence Matrix (GLCM) |
|---|---|
| Histogram Minimum | Joint Maximum |
| Histogram Maximum | Joint Average |
| Histogram Range | Standart Deviation |
| Histogram Mean | Joint Variance |
| Histogram Variance | Joint Entropy |
| Histogram Standart Deviation | Difference Average |
| Histogram Skewness | Difference Variance |
| Histogram Kurtosis | Difference Entropy |
| Histogram Entropy | Sum of Averages |
| Histogram Uniformity | Sum of Variance |
| Histogram Mean Absolute Deviation | Sum of Entropy |
| Histogram Robust Mean Absolute Deviation | Angular Second Moment |
| Histogram Median Absolute Deviation | Contrast |
| Histogram Coefficient Variation | Dissimilarity |
| Histogram Quartile Coefficient Dispersion | Inverse Difference |
| Histogram Interquartile Range | Inverse Difference Normalised |
| Histogram P10th | Inverse Difference Moment |
| Histogram P25th | Inverse Difference Moment Normalised |
| Histogram P50th | Joint Maximum |
| Histogram P75th | Joint Average |
| Histogram P90th | Standart Deviation |
| Histogram Minimum Histogram Gradient Intensity | Joint Variance |
| Histogram MaximumHistogram Gradient Intensity | Joint Entropy |
| Intensity Minimum | Difference Average |
| Intensity Maximum | Difference Variance |
| Intensity Range | Difference Entropy |
| Intensity Mean | Sum of Averages |
| Intensity Variance | Sum of Variance |
| Intensity Standart Deviation | Sum of Entropy |
| Intensity Skewness | Angular Second Moment |
| Intensity Kurtosis | Contrast |
| Intensity Energy | Dissimilarity |
| Intensity P10th | Inverse Variance |
| Intensity P25th | Correlation |
| Intensity P50th | Auto Correlation |
| Intensity P75th | Cluster Shade |
| Intensity P90th | Cluster Prominence |
| Intensity Root Mean Square | Cluster Tendency |
| Intensity Mean Absolute Deviation | Information Correlation 1 |
| Intensity Robust Mean Absolute Deviation | Information Correlation 2 |
| Intensity Median Absolute Deviation | Inverse Variance 41 |
| Intensity Coefficient Variation | |
| Intensity Quartile Coefficient Dispersion | |
| Intensity Interquartile Range 44 |
| Radiomics Features of First Order | Radiomics Features of Second Order: Gray Level Co-Occurrence Matrix (GLCM) |
|---|---|
| Histogram Variance | Auto Correlation |
| Intensity Maximum | Cluster Shade |
| Intensity Mean | Cluster Prominence |
| Intensity Variance | Cluster Tendency |
| Intensity Energy | Contrast |
| Intensity Root Mean Square | |
| Intensity Median Absolute Deviation |
References
- Ruf, C.G.; Isbarn, H.; Wagner, W.; Fisch, M.; Matthies, C.; Dieckmann, K.P. Changes in Epidemiologic Features of Testicular Germ Cell Cancer: Age at Diagnosis and Relative Frequency of Seminoma Are Constantly and Significantly Increasing; Elsevier: Amsterdam, The Netherlands, 2014; p. 33-e1. [Google Scholar]
- Bray, F.; Richiardi, L.; Ekbom, A.; Pukkala, E.; Cuninkova, M.; Møller, H. Trends in testicular cancer incidence and mortality in 22 European countries: Continuing increases in incidence and declines in mortality. Int. J. Cancer 2006, 118, 3099–3111. [Google Scholar] [CrossRef] [PubMed]
- Einhorn, L.H. Treatment of testicular cancer: A new and improved model. J. Clin. Oncol. 1990, 8, 1777–1781. [Google Scholar] [CrossRef] [PubMed]
- Kollmannsberger, C.; Tandstad, T.; Bedard, P.L.; Cohn-Cedermark, G.; Chung, P.W.; Jewett, M.A.; Powles, T.; Warde, P.; Daneshmand, S.; Protheroe, A.; et al. Patterns of relapse in patients with clinical stage I testicular cancer managed with active surveillance. J. Clin. Oncol. 2015, 33, 51–57. [Google Scholar] [CrossRef]
- Fung, C.; Sesso, H.D.; Williams, A.M.; Kerns, S.L.; Monahan, P.; Zaid, M.A.; Feldman, D.; Hamilton, R.J.; Vaughn, D.J.; Beard, C.J.; et al. Multi-institutional assessment of adverse health outcomes among North American testicular cancer survivors after modern cisplatin-based chemotherapy. J. Clin. Oncol. 2017, 35, 1211. [Google Scholar] [CrossRef]
- Huddart, R.; Norman, A.; Shahidi, M.; Horwich, A.; Coward, D.; Nicholls, J.; Dearnaley, D.P. Cardiovascular disease as a long-term complication of treatment for testicular cancer. J. Clin. Oncol. 2003, 21, 1513–1523. [Google Scholar] [CrossRef] [PubMed]
- Travis, L.B.; Ng, A.K.; Allan, J.M.; Pui, C.H.; Kennedy, A.R.; Xu, X.G.; Purdy, J.A.; Applegate, K.; Yahalom, J.; Constine, L.S.; et al. Second malignant neoplasms and cardiovascular disease following radiotherapy. J. Natl. Cancer Inst. 2012, 104, 357–370. [Google Scholar] [CrossRef]
- Kerns, S.L.; Fung, C.; Monahan, P.O.; Ardeshir-Rouhani-Fard, S.; Zaid, M.I.A.; Williams, A.M.; Stump, T.E.; Sesso, H.D.; Feldman, D.R.; Hamilton, R.J.; et al. Cumulative burden of morbidity among testicular cancer survivors after standard cisplatin-based chemotherapy: A multi-institutional study. J. Clin. Oncol. 2018, 36, 1505. [Google Scholar] [CrossRef]
- Agrawal, V.; Dinh, P.C., Jr.; Fung, C.; Monahan, P.O.; Althouse, S.K.; Norton, K.; Cary, C.; Einhorn, L.; Fossa, S.D.; Adra, N.; et al. Adverse health outcomes among US testicular cancer survivors after cisplatin-based chemotherapy vs surgical management. JNCI Cancer Spectr. 2020, 4, pkz079. [Google Scholar] [CrossRef]
- Tandstad, T.; Kollmannsberger, C.K.; Roth, B.J.; Jeldres, C.; Gillessen, S.; Fizazi, K.; Daneshmand, S.; Lowrance, W.T.; Hanna, N.H.; Albany, C.; et al. Practice makes perfect: The rest of the story in testicular cancer as a model curable neoplasm. J. Clin. Oncol. 2017, 35, 3525. [Google Scholar] [CrossRef]
- Rajpert-De Meyts, E.; McGlynn, K.A.; Okamoto, K.; Jewett, M.A.; Bokemeyer, C. Testicular germ cell tumours. Lancet 2016, 387, 1762–1774. [Google Scholar] [CrossRef]
- Cheng, L.; Albers, P.; Berney, D.M.; Feldman, D.R.; Daugaard, G.; Gilligan, T.; Looijenga, L.H. Testicular cancer. Nat. Rev. Dis. Prim. 2018, 4, 29. [Google Scholar] [CrossRef]
- Dieckmann, K.P.; Simonsen-Richter, H.; Kulejewski, M.; Anheuser, P.; Zecha, H.; Isbarn, H.; Pichlmeier, U. Serum tumour markers in testicular germ cell tumours: Frequencies of elevated levels and extents of marker elevation are significantly associated with clinical parameters and with response to treatment. BioMed Res. Int. 2019, 2019, 5030349. [Google Scholar] [CrossRef] [PubMed]
- Gilligan, T.D.; Hayes, D.F.; Seidenfeld, J.; Temin, S. ASCO clinical practice guideline on uses of serum tumor markers in adult males with germ cell tumors. J. Oncol. Pract. 2010, 6, 199. [Google Scholar] [CrossRef] [PubMed]
- Kliesch, S.; Schmidt, S.; Wilborn, D.; Aigner, C.; Albrecht, W.; Bedke, J.; Beintker, M.; Beyersdorff, D.; Bokemeyer, C.; Busch, J.; et al. Management of germ cell tumours of the testis in adult patients. German clinical practice guideline part I: Epidemiology, classification, diagnosis, prognosis, fertility preservation, and treatment recommendations for localized stages. Urol. Int. 2021, 105, 169–180. [Google Scholar] [CrossRef]
- Patel, H.D.; Joice, G.A.; Schwen, Z.R.; Semerjian, A.; Alam, R.; Srivastava, A.; Allaf, M.E.; Pierorazio, P.M. Retroperitoneal lymph node dissection for testicular seminomas: Population-based practice and survival outcomes. World J. Urol. 2018, 36, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.J.; Huddart, R.A.; Coleman, N. The present and future of serum diagnostic tests for testicular germ cell tumours. Nat. Rev. Urol. 2016, 13, 715–725. [Google Scholar] [CrossRef]
- Albers, P.; Albrecht, W.; Algaba, F.; Bokemeyer, C.; Cohn-Cedermark, G.; Fizazi, K.; Horwich, A.; Laguna, M.P.; Nicolai, N.; Oldenburg, J. Guidelines on testicular cancer: 2015 update. Eur. Urol. 2015, 68, 1054–1068. [Google Scholar] [CrossRef]
- Hudolin, T.; Kastelan, Z.; Knezevic, N.; Goluza, E.; Tomas, D.; Coric, M. Correlation between retroperitoneal lymph node size and presence of metastases in nonseminomatous germ cell tumors. Int. J. Surg. Pathol. 2012, 20, 15–18. [Google Scholar] [CrossRef]
- Hale, G.R.; Teplitsky, S.; Truong, H.; Gold, S.A.; Bloom, J.B.; Agarwal, P.K. Lymph node imaging in testicular cancer. Transl. Androl. Urol. 2018, 7, 864. [Google Scholar] [CrossRef]
- Obermeyer, Z.; Emanuel, E.J. Predicting the future—Big data, machine learning, and clinical medicine. N. Engl. J. Med. 2016, 375, 1216. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.; Deist, T.M.; Peerlings, J.; De Jong, E.E.; Van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalised medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images are more than pictures, they are data. Radiology 2016, 278, 563. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The image biomarker standardisation initiative: Standardised quantitative radiomics for high-throughput image-based phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Sollini, M.; Antunovic, L.; Chiti, A.; Kirienko, M. Towards clinical application of image mining: A systematic review on artificial intelligence and radiomics. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2656–2672. [Google Scholar] [CrossRef]
- Ibrahim, A.; Primakov, S.; Beuque, M.; Woodruff, H.; Halilaj, I.; Wu, G.; Refaee, T.; Granzier, R.; Widaatalla, Y.; Hustinx, R.; et al. Radiomics for precision medicine: Current challenges, future prospects, and the proposal of a new framework. Methods 2021, 188, 20–29. [Google Scholar] [CrossRef]
- Dong, D.; Tang, L.; Li, Z.Y.; Fang, M.J.; Gao, J.B.; Shan, X.H.; Ying, X.-J.; Sun, Y.-S.; Fu, J.; Wang, X.-X.; et al. Development and validation of an individualised nomogram to identify occult peritoneal metastasis in patients with advanced gastric cancer. Ann. Oncol. 2019, 30, 431–438. [Google Scholar] [CrossRef]
- Huang, Y.; Liang, C.; He, L.; Tian, J.; Liang, C.; Chen, X.; Ma, Z.-L.; Liu, Z.-Y. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J. Clin. Oncol. 2016, 34, 2157–2164. [Google Scholar] [CrossRef]
- Wu, S.; Zheng, J.; Li, Y.; Yu, H.; Shi, S.; Xie, W.; Liu, H.; Su, Y.; Huang, J.; Lin, T.; et al. A Radiomics Nomogram for the Preoperative Prediction of Lymph Node Metastasis in Bladder CancerA Radiomics Nomogram for Bladder Cancer. Clin. Cancer Res. 2017, 23, 6904–6911. [Google Scholar] [CrossRef]
- Gao, J.; Han, F.; Jin, Y.; Wang, X.; Zhang, J. A radiomics nomogram for the preoperative prediction of lymph node metastasis in pancreatic ductal adenocarcinoma. Front. Oncol. 2020, 10, 1654. [Google Scholar] [CrossRef]
- Haralick, R.M.; Shanmugam, K.; Dinstein, I.H. Textural features for image classification. IEEE Trans. Syst. Man Cybern. 1973, SMC-3, 610–621. [Google Scholar] [CrossRef]
- Shen, C.; Liu, Z.; Guan, M.; Song, J.; Lian, Y.; Wang, S.; Tang, Z.; Dong, D.; Kong, L.; Wang, M.; et al. 2D and 3D CT radiomics features prognostic performance comparison in non-small cell lung cancer. Transl. Oncol. 2017, 10, 886–894. [Google Scholar] [CrossRef]
- Duin, R.P.; Pekalska, E. Dissimilarity Representation for Pattern Recognition. In Foundations And Applications; World Scientific: Singapore, 2005; Volume 64. [Google Scholar]
- Tibshirani, R. The lasso method for variable selection in the Cox model. Stat. Med. 1997, 16, 385–395. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression shrinkage and selection via the lasso: A retrospective. J. R. Stat. Soc. Ser. B 2011, 73, 273–282. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Agrawal, T. Hyperparameter Optimization Using Scikit-Learn. In Hyperparameter Optimization in Machine Learning: Make Your Machine Learning and Deep Learning Models More Efficient [Internet]; Apress: Berkeley, CA, USA, 2021; pp. 31–51. [Google Scholar] [CrossRef]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- van Rossum, G.; Drake, F.L. Python/C API Manual-Python 2.6; CreateSpace: Scotts Valley, CA, USA, 2009. [Google Scholar]
- Fosså, S.D.; Cvancarova, M.; Chen, L.; Allan, A.L.; Oldenburg, J.; Peterson, D.R.; Travis, L.B. Adverse prognostic factors for testicular cancer–specific survival: A population-based study of 27,948 patients. J. Clin. Oncol. 2011, 29, 963–970. [Google Scholar] [CrossRef]
- Parker, C.; Milosevic, M.; Panzarella, T.; Banerjee, D.; Jewett, M.; Catton, C.; Tew-George, B.; Gospodarowicz, M.; Warde, P. The prognostic significance of the tumour infiltrating lymphocyte count in stage I testicular seminoma managed by surveillance. Eur. J. Cancer 2002, 38, 2014–2019. [Google Scholar] [CrossRef] [PubMed]
- Lerro, C.; McGlynn, K.; Cook, M. A systematic review and meta-analysis of the relationship between body size and testicular cancer. Br. J. Cancer 2010, 103, 1467–1474. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.P.; Hartmann, J.T.; Classen, J.; Diederichs, M.; Pichlmeier, U. Is increased body mass index associated with the incidence of testicular germ cell cancer? J. Cancer Res. Clin. Oncol. 2009, 135, 731–738. [Google Scholar] [CrossRef]
- Mickey, R.M.; Greenland, S. The impact of confounder selection criteria on effect estimation. Am. J. Epidemiol. 1989, 129, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Bendel, R.B.; Afifi, A.A. Comparison of stopping rules in forward “stepwise” regression. J. Am. Stat. Assoc. 1977, 72, 46–53. [Google Scholar]
- Powles, T.B.; Bhardwa, J.; Shamash, J.; Mandalia, S.; Oliver, T. The changing presentation of germ cell tumours of the testis between 1983 and 2002. BJU Int. 2005, 95, 1197–1200. [Google Scholar] [CrossRef] [PubMed]
- Albers, P.; Siener, R.; Kliesch, S.; Weissbach, L.; Krege, S.; Sparwasser, C.; Schulze, H.; Heidenreich, A.; de Riese, W.; Loy, V.; et al. Risk factors for relapse in clinical stage I nonseminomatous testicular germ cell tumors: Results of the German Testicular Cancer Study Group Trial. J. Clin. Oncol. 2003, 21, 1505–1512. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, J.; Fosså, S.; Nuver, J.; Heidenreich, A.; Schmoll, H.J.; Bokemeyer, C.; Horwich, A.; Beyer, J.; Kataja, V. Testicular seminoma and non-seminoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013, 24, vi125–vi132. [Google Scholar] [CrossRef]
- Kier, M.G.; Hansen, M.K.; Lauritsen, J.; Mortensen, M.S.; Bandak, M.; Agerbaek, M.; Holm, N.V.; Dalton, S.O.; Andersen, K.K.; Johansen, C.; et al. Second malignant neoplasms and cause of death in patients with germ cell cancer: A Danish nationwide cohort study. JAMA Oncol. 2016, 2, 1624–1627. [Google Scholar] [CrossRef]
- von Eyben, F.E. Laboratory markers and germ cell tumors. Crit. Rev. Clin. Lab. Sci. 2003, 40, 377–427. [Google Scholar] [CrossRef] [PubMed]
- Lobo, J.; Leão, R.; Jerónimo, C.; Henrique, R. Liquid biopsies in the clinical management of germ cell tumor patients: State-of-the-art and future directions. Int. J. Mol. Sci. 2021, 22, 2654. [Google Scholar] [CrossRef]
- Trigo, J.M.; Tabernero, J.M.; Paz-Ares, L.; García-Llano, J.L.; Mora, J.; Lianes, P.; Esteban, E.; Salazar, R.; López-López, J.J.; Cortés-Funes, H.; et al. Tumor markers at the time of recurrence in patients with germ cell tumors. Cancer 2000, 88, 162–168. [Google Scholar] [CrossRef]
- Steyerberg, E.; Gerl, A.; Fossa, S.; Sleijfer, D.; de Wit, R.; Kirkels, W.; Schmeller, N.; Clemm, C.; Habbema, J.D.; Keizer, H.J. Validity of predictions of residual retroperitoneal mass histology in nonseminomatous testicular cancer. J. Clin. Oncol. 1998, 16, 269–274. [Google Scholar] [CrossRef]
- Vergouwe, Y.; Steyerberg, E.W.; Foster, R.S.; Habbema, J.D.F.; Donohue, J.P. Validation of a prediction model and its predictors for the histology of residual masses in nonseminomatous testicular cancer. J. Urol. 2001, 165, 84–88. [Google Scholar] [CrossRef]
- Andersen, M.B.; Harders, S.W.; Ganeshan, B.; Thygesen, J.; Torp Madsen, H.H.; Rasmussen, F. CT texture analysis can help differentiate between malignant and benign lymph nodes in the mediastinum in patients suspected for lung cancer. Acta Radiol. 2016, 57, 669–676. [Google Scholar] [CrossRef]
- Tan, X.; Ma, Z.; Yan, L.; Ye, W.; Liu, Z.; Liang, C. Radiomics nomogram outperforms size criteria in discriminating lymph node metastasis in resectable esophageal squamous cell carcinoma. Eur. Radiol. 2019, 29, 392–400. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, Z.; Cui, W.; Zheng, C.; Li, H.; Li, Y.; Lu, L.; Mao, J.; Zeng, W.; Yang, X.; et al. Preoperative prediction of axillary sentinel lymph node burden with multiparametric MRI-based radiomics nomogram in early-stage breast cancer. Eur. Radiol. 2021, 31, 5924–5939. [Google Scholar] [CrossRef] [PubMed]
- Xiao, M.; Ma, F.; Li, Y.; Li, Y.; Li, M.; Zhang, G.; Qiang, J. Multiparametric MRI-Based Radiomics Nomogram for Predicting Lymph Node Metastasis in Early-Stage Cervical Cancer. J. Magn. Reson. Imaging 2020, 52, 885–896. [Google Scholar] [CrossRef] [PubMed]
- Baessler, B.; Nestler, T.; Pinto dos Santos, D.; Paffenholz, P.; Zeuch, V.; Pfister, D.; Maintz, D.; Heidenreich, A. Radiomics allows for detection of benign and malignant histopathology in patients with metastatic testicular germ cell tumors prior to post-chemotherapy retroperitoneal lymph node dissection. Eur. Radiol. 2020, 30, 2334–2345. [Google Scholar] [CrossRef] [PubMed]
- Harrell, F.E., Jr.; Lee, K.L.; Mark, D.B. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Lewin, J.; Dufort, P.; Halankar, J.; O’Malley, M.; Jewett, M.A.; Hamilton, R.J.; Gupta, A.; Lorenzo, A.; Traubici, J.; Nayan, M.; et al. Applying radiomics to predict pathology of postchemotherapy retroperitoneal nodal masses in germ cell tumors. JCO Clin. Cancer Inform. 2018, 2, 1–12. [Google Scholar] [CrossRef]
- Leão, R.; Nayan, M.; Punjani, N.; Jewett, M.A.S.; Fadaak, K.; Garisto, J.; Lewin, J.; Atenafu, E.; Sweet, J.; Anson-Cartwright, L.; et al. A New Model to Predict Benign Histology in Residual Retroperitoneal Masses After Chemotherapy in Nonseminoma. Eur. Urol. Focus 2018, 4, 995–1001. [Google Scholar] [CrossRef]
- Vergouwe, Y.; Steyerberg, E.W.; Foster, R.S.; Sleijfer, D.T.; Fosså, S.D.; Gerl, A.; de Wit, R.; Roberts, J.T.; Habbema, J.D.F. Predicting Retroperitoneal Histology in Postchemotherapy Testicular Germ Cell Cancer: A Model Update and Multicentre Validation with More Than 1000 Patients. Eur. Urol. 2007, 51, 424–432. [Google Scholar] [CrossRef]
- Peter, A.; Lothar, W.; Susanne, K.; Sabine, K.; Michael, H.; Axel, H.; Walz, P.; Kuczyk, M.; Fimmers, R.; for the German Testicular Cancer Study Group. Prediction of Necrosis After Chemotherapy of Advanced Germ Cell Tumors: Results of a Prospective Multicenter Trial of the German Testicular Cancer Study Group. J. Urol. 2004, 171, 1835–1838. [Google Scholar]
- Zengerling, F.; Kunath, F.; Jensen, K.; Ruf, C.; Schmidt, S.; Spek, A. Prognostic factors for tumor recurrence in patients with clinical stage I seminoma undergoing surveillance—A systematic review. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Zengerling, F.; Beyersdorff, D.; Busch, J.; Heinzelbecker, J.; Pfister, D.; Ruf, C.; Winter, C.; Albers, P.; Kliesch, S.; Schmidt, S. Prognostic factors in patients with clinical stage I nonseminoma—Beyond lymphovascular invasion: A systematic review. World J. Urol. 2022, 40, 2879–2887. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.P.; Radtke, A.; Spiekermann, M.; Balks, T.; Matthies, C.; Becker, P.; Ruf, C.; Oing, C.; Oechsle, K.; Bokemeyer, C.; et al. Serum Levels of MicroRNA miR-371a-3p: A Sensitive and Specific New Biomarker for Germ Cell Tumours. Eur. Urol. 2017, 71, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Bezan, A.; Gerger, A.; Pichler, M. MicroRNAs in testicular cancer: Implications for pathogenesis, diagnosis, prognosis and therapy. Anticancer. Res. 2014, 34, 2709–2713. [Google Scholar] [PubMed]


| Average age (range) | 35.2 ± 9.4 Years (18–63) |
| Histological type | |
| Seminoma | 60 Patients (66%) |
| Non-seminoma | 31 Patients (34%) |
| Tumour classification (T) | |
| T1a | 64 (70%) |
| T1b | 27 (30%) |
| Tumour marker | |
| AFP positive | 21 Patients (19%) |
| Β-HCG positive | 40 Patients (44%) |
| AFP und Β-HCG positive | 10 Patients (11%) |
| BMI (range) | 25.9 ± 4.6 (19.3–43.9) |
| Patients’ status in 6-year follow up | |
| Complete remission (CR) | 81 (89%) |
| Relapse of disease (RD) with metastatic lymph nodes | 10 (11%) |
| Model | AUC (95% CI) | Accuracy | Precision | Recall | F1 Score |
|---|---|---|---|---|---|
| Radiomics-only | 0.87± 0.04 | 0.80 ± 0.06 | 0.81 ± 0.06 | 0.80 ± 0.08 | 0.80 ± 0.06 |
| Clinical-only | 0.75 ± 0.08 | 0.68 ± 0.10 | 0.66 ± 0.11 | 0.71 ± 0.16 | 0.68 ± 0.12 |
| Combined clinical-radiomics | 0.89 ± 0.03 | 0.81 ± 0.04 | 0.80 ± 0.07 | 0.83 ± 0.06 | 0.81 ± 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lisson, C.S.; Manoj, S.; Wolf, D.; Schrader, J.; Schmidt, S.A.; Beer, M.; Goetz, M.; Zengerling, F.; Lisson, C.G.S. CT Radiomics and Clinical Feature Model to Predict Lymph Node Metastases in Early-Stage Testicular Cancer. Onco 2023, 3, 65-80. https://doi.org/10.3390/onco3020006
Lisson CS, Manoj S, Wolf D, Schrader J, Schmidt SA, Beer M, Goetz M, Zengerling F, Lisson CGS. CT Radiomics and Clinical Feature Model to Predict Lymph Node Metastases in Early-Stage Testicular Cancer. Onco. 2023; 3(2):65-80. https://doi.org/10.3390/onco3020006
Chicago/Turabian StyleLisson, Catharina Silvia, Sabitha Manoj, Daniel Wolf, Jasper Schrader, Stefan Andreas Schmidt, Meinrad Beer, Michael Goetz, Friedemann Zengerling, and Christoph Gerhard Sebastian Lisson. 2023. "CT Radiomics and Clinical Feature Model to Predict Lymph Node Metastases in Early-Stage Testicular Cancer" Onco 3, no. 2: 65-80. https://doi.org/10.3390/onco3020006
APA StyleLisson, C. S., Manoj, S., Wolf, D., Schrader, J., Schmidt, S. A., Beer, M., Goetz, M., Zengerling, F., & Lisson, C. G. S. (2023). CT Radiomics and Clinical Feature Model to Predict Lymph Node Metastases in Early-Stage Testicular Cancer. Onco, 3(2), 65-80. https://doi.org/10.3390/onco3020006







