IoT Health Devices: Exploring Security Risks in the Connected Landscape
Abstract
1. Introduction
2. IoT Healthcare Components
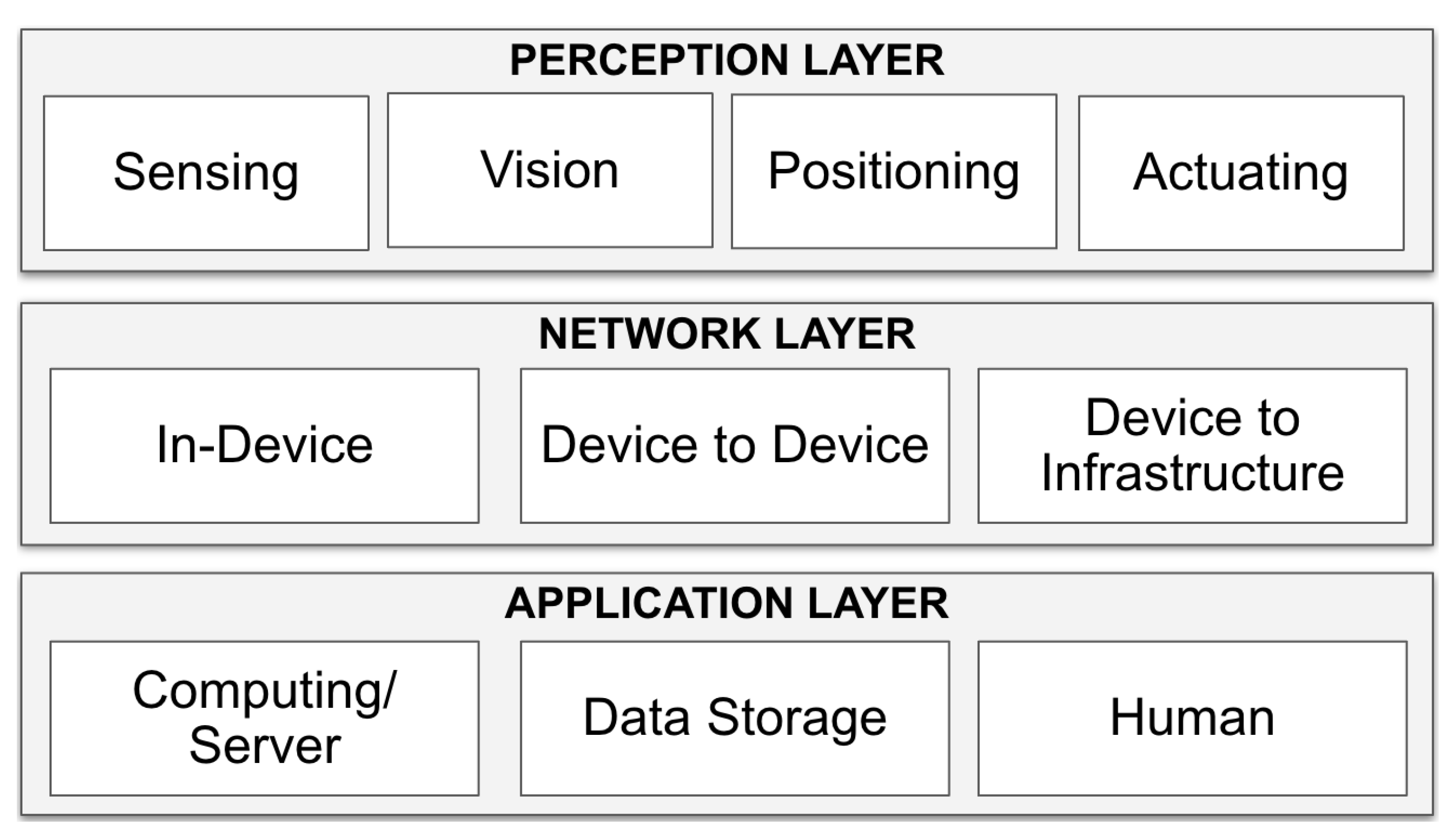
2.1. IoT System High-Level Architecture
2.1.1. Perception Layer
2.1.2. Network Layer
2.1.3. Application Layer
2.2. IoT Healthcare Devices
2.2.1. Medical Imaging
2.2.2. Medical Sensors
2.2.3. Implanted Medical Devices
2.2.4. Virtual Medical Home Assistants
2.3. IoT Healthcare Supporting Technologies
2.3.1. IoTHD Software Components
2.3.2. IoTHD Supporting Infrastructure
2.4. IoT Healthcare Stakeholders
2.4.1. Patients and Related Family Members
2.4.2. Healthcare Personnel
2.4.3. IoTHD Manufacturers
2.5. Security Risk Management
- Asset-related concepts—identify relevant assets for security risk analysis. It describes the business assets—that represent information, data, and processes that bring value to an organization—and system assets—that support business assets to protect. Asset-related concepts also describe the security criteria (in terms of confidentiality, integrity, and availability) that define the security needs of the assets [89].
- Risk-related concepts—illustrate the vulnerability, threat agent, threats, and risk impact analysis of the assets in scope. A security risk is a combination of a security event and its impact (negation of the security criterion), harming business and system assets. A vulnerability is a characteristic of system assets, constituting its flaws—an implementation defect that can lead to a vulnerability [89]. A threat agent refers to an entity that has the potential to cause damage to information system assets, thereby initiating a threat and becoming the origin of a risk. Typically, a threat agent is identified by their motivation, skills, capability, knowledge, available resources, and opportunity to carry out an attack [89,97]. A threat event is a component of security risk that occurs when a threat targets system assets and exploits their vulnerability. The STRIDE method [98] can then be used for security threat analysis [96]. The abbreviation STRIDE stands for spoofing (S)—pretending to be someone else to gain access to sensitive data or resources, tampering (T)—altering data or code to manipulate the application’s behavior or cause it to malfunction, repudiation (R)—denying ones actions or the actions of others and making it difficult to track down the source of an action, information disclosure (I)—exposing or gaining access to information one should not be able to access, denial of service (D)—preventing a system from providing its intended service by crashing it, slowing it down, or filling its storage, and elevation of privilege (E)—gaining access to functionality without authorization [98]. Further in this study, we use STRIDE to guide a security threat analysis due to its industrial usage, maturity, high research concentration within the security community, and applicability for guiding risk treatment.
- Risk treatment-related concepts—tackle mitigating the identified security risks, guiding risk mitigation decisions, security requirements, and controls to treat the risks. Security requirements aim to define conditions to be reached by mitigating identified security risks and are prerequisites to controls that implement the specified security requirements [89]. The STRIDE security requirements can thus guide requirements elicitation for risk treatment [96].
3. Security Risks in IoT Health Devices
3.1. IoTHD Assets
| Layer | System Assets | Business Assets | |
|---|---|---|---|
| Perception [23,25] | Sensing | Neural sensors, infrared sensors, RFID (Radio Frequency Identification) tags, light sensors, magnetometer, thermometers, smartwatches, monitoring patches, finger pulse oximeters | Patient biomedical status: patient activity, heart rate, sleep patterns, neural activity/brain signal, oxygen saturation levels, body temperature, glucose level in blood |
| Positioning | Location sensor, movement sensor, gyroscope, accelerometer | Pseudo-range measurements | |
| Visioning | Smart cameras, medical imaging systems (MRI and CT) | Surveillance (audio, picture, video) data, MRI and CT images | |
| Actuating | Medical device control unit, social robot actuators | Medical device commands | |
| Network [23,25,99] | In-device | DICOM, Bluetooth, WiFi, Zigbee, RFID, wireless sensor networks, NFC (Near-Field Communication), Z-wave, MQTT, LoRa and ultra-wide bandwidth (UWB), wireless body area networks (WBAN) | Transmitted perception data |
| Device-to- device | |||
| Device-to- infrastructure | |||
| Application [23] | Computing/Personal Servers | Web application platform, mobile application, PACS server | Application process, application data, perception data |
| Data Storage | Virtualized storage at edge computing, local database, PACS storage | Perception and application data | |
| End-user | Patients and related family members, healthcare personnel, IoTHD manufacturers | Application process, PII, patient biomedical status | |
3.2. IoTHD Vulnerabilities
3.2.1. Perception-Layer Vulnerabilities
3.2.2. Network-Layer Vulnerabilities
3.2.3. Application-Layer Vulnerabilities
3.3. Relevant Threat Agents
3.3.1. Nation and State Actors
- State actors continue to have the means to produce sophisticated works.
- APTs produced are likely to prioritize and maintain autonomy, allowing damages delivered to be sustained. Interference can be run through these to disrupt the operations of critical healthcare [122].
- If APTs can securely deliver hostile software into organizations with enough IoTHDs, and those devices are distributed widely enough and sufficiently evade patching, they can be a significant means of surveillance.
- The most relevant APTs toward IoTHDs appear to be those that would target both IP and operations of such IP. Such could deliver strategic technological gains to nation-states while offering positioning to control companies of rival nation-states and or their alliances.
- IoTHD developers should assume they are already targets and sharpen the protection of their most critical assets, including tighter protocols, vetting, and minimization of interactions with core IP assets. Further, as per BIO-ISAC’s reported recommendation for bio manufacturers, all IoTHD developers should similarly consider reviewing the degree of backups, networking segmentation, and product lead times [88].
- Owing to automation in APTs and other means of automated attacks, we may see increased automation in defense.
3.3.2. Healthcare Facilities and Related Personnel
3.3.3. Independent and Unorthodox Communities
3.4. IoTHD Security Threats
| System Asset | Security Threats | |||||
|---|---|---|---|---|---|---|
| S | T | R | I | D | E | |
| Perception Layer: Sensing, Positioning, and Vision Technologies | Sensor spoofing, Sybil, node impersonation, replay, sending deceptive messages, device cloning, weak authentication scheme | Forgery, data/image manipulation, data tampering, falsification of device readings, data injection, device tampering | Bogus message | Eavesdropping | Message saturation, jamming, DoS, battery depletion | Backdoor, weak authentication scheme, malware, remote update of device control unit, hardware trojan, compromised node, password intrusion, physical theft |
| Network Layer: In-Device, Device-to-Device, Device-to-Infrastructure | Routing attacks, replay attack, masquerading, RF fingerprinting, impersonation attack, eavesdropping, position faking | Firmware modification, injection (message, command, code, packet), manipulation/alteration/fabrication, tampering, forgery, malicious update (software/firmware) | Bogus messages, message modification, rogue repudiation, loss of event traceability | Eavesdropping, man-in-the-middle, location tracking, sniffing, message interception, information disclosure, traffic analysis, side-channel, ARP Tab. Poisoning | DoS/DDoS, battery depletion attack, jamming, flooding, message suppression, Blackhole, Grayhole, Sinkhole, Wormhole, MIMO attacks | Malware, Brute Force, gaining control, social engineering, logical attacks, unauthorized access, session hijack |
| Application Layer: Human, Computing, Data Storage | Spoofing, impersonation, weak authentication scheme | Firmware/software modification, malicious update, SQL injection | Audit log tampering, forgery | Eavesdropping, location tracking, privacy leakage, SQL injection, data breach, message disclosure | DoS, DDoS, buffer overflows | Outdated OSs, social engineering/phishing, unauthorized access, malware, software hijacking, Dropbear SSH Server, IaaS cloud attack, password intrusion, ransomware |
3.5. IoTHD Countermeasures
3.5.1. Perception/Device-Level Controls
3.5.2. Network/Communication-Level Controls
3.5.3. Application-Level Controls
4. Practical Examples Inspired by Real-World Concerns
4.1. Risk 1: Medical Image Modification
4.1.1. Perception-Layer Risk Analysis
4.1.2. Network-Layer Risk Analysis
4.1.3. Application-Layer Risk Analysis
4.1.4. Summary
4.2. Risk 2: Malicious Synthesis and Camouflage of Genetic Sequences
4.2.1. Perception-Layer Risk Analysis
4.2.2. Network-Layer Risk Analysis
4.2.3. Application-Layer Risk Analysis
4.2.4. Summary
4.3. Risk 3: Transport of Critical Materials and Unintentional Advertising
4.3.1. Perception-Layer Risk Analysis
4.3.2. Network-Layer Risk Analysis
4.3.3. Application-Layer Risk Analysis
4.3.4. Summary
| Risk Scenario | Image Modification Using CT-GAN [117] | Genetic Sequences Attack [157] | Unintentional Advertising of Critical Materials [160] |
|---|---|---|---|
| Business Asset | Medical diagnoses, MRI/CT images | Patient genetic sequences | Critical material advertisement |
| Security Criteria | Integrity of medical diagnoses and MRI/CT images | Integrity of genetic sequences | Confidentiality of presence of radioactive isotopes communication protocols |
| System Asset | PACS medical imaging servers | DNA synthesizers | Medical devices using radioactive isotopes, medical materials, communication protocol |
| Vulnerability | PACS server accidentally exposed to the internet via web access solutions | Sound waves produced during the operation of the synthesizer can infer operational information | Improper development and application of communication protocols unintentionally advertise the availability of radioactive materials, making them a potential target for theft |
| Threat Agent | Attacker with knowledge of using the CT-GAN technique with interest in manipulating a patient’s MRI/CT images | Attackers with the capability and opportunity to record acoustic signals produced by the synthesizer and interest in manipulating genetic sequences for financial gain | Attacker seeking to steal radioactive materials for malicious purposes |
| Threat | An attacker gains unauthorized access to the PACS server and manipulates a patient’s MRI/CT image using the CT-GAN technique to cause a wrong diagnosis | Attacker records the acoustic signals produced by the synthesizer’s pumps to infer information about the synthesizer’s operation, including the synthesized DNA sequence | Attacker seeking to exploit the vulnerabilities to gain access to valuable materials through theft could lead to exposure and harm to unprepared and unshielded populations |
| Impact | Loss of integrity of MRI/CT images, misdiagnosis of a severe disease, delayed treatment, loss of trust in the medical system | Loss of integrity of genetic information, medical research disruption, and intellectual property theft | Leak of the presence of radioactive isotopes, severe health risks for the public, damage to the reputation of medical device manufacturers, legal consequences |
| Risk Treatment | (i) Encryption and secure storage of MRI/CT PACS servers and medical images (ii) Reduce sensitive data collection (iii) Authentication and authorization controls on PACS servers | (i) Encryption, access controls, monitoring for suspicious activity (ii) Routine risk assessments and vulnerability testing | (i) Specified security protocols to protect against theft (ii) Improved logistical efforts to ensure proper handling and disposal of the materials (iii) Revised education for law enforcement and peripheral agencies |
4.4. Lessons Learned
5. The Future of IoTHD Security
5.1. Administrative (Laws and Policy Changes)
5.2. Defending Forward
5.3. AI Innovations and New Directions
5.4. Innovations of Blockchain Technology
5.5. Genetic Engineering
5.6. Quantum Computing
5.7. Intersectional Fusions of 4th IR Technologies
6. Concluding Remarks
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Thomasian, N.M.; Adashi, E.Y. Cybersecurity in the internet of medical things. Health Policy Technol. 2021, 10, 100549. [Google Scholar] [CrossRef]
- Sadoughi, F.; Behmanesh, A.; Sayfouri, N. Internet of things in medicine: A systematic mapping study. J. Biomed. Inform. 2020, 103, 103383. [Google Scholar] [CrossRef] [PubMed]
- Annamalai, M.; Jesintha, D. Smart IoT system based patient monitoring and medicine reminder based on registry service selection scheme. Eur. J. Mol. Clin. Med. 2021, 7, 2710–2721. [Google Scholar]
- Martin, R. The Internet of Things (IoT)–Removing the Human Element. Infosec Writ. 2015, 28, 12. [Google Scholar]
- Richardson, L.C.; Lewis, S.M.; Burnette, R.N. Building capacity for cyberbiosecurity training. Front. Bioeng. Biotechnol. 2019, 7, 112. [Google Scholar] [CrossRef]
- Greenbaum, D. Cyberbiosecurity: An Emerging Field that has Ethical Implications for Clinical Neuroscience. Camb. Q. Healthc. Ethics 2021, 30, 662–668. [Google Scholar] [CrossRef] [PubMed]
- Adler, A.; Beal, J.; Lancaster, M.; Wyschogrod, D. Cyberbiosecurity and Public Health in the Age of COVID-19. In Emerging Threats of Synthetic Biology and Biotechnology; Springer: Dordrecht, The Netherlands, 2021; pp. 103–115. [Google Scholar]
- Perakslis, C. Cyberbiosecurity, Ecopsychology, and Beyond: Our Formidable PIT Community [Last Word]. IEEE Technol. Soc. Mag. 2020, 39, 84. [Google Scholar] [CrossRef]
- Potter, L.; Palmer, X.L. Human Factors in Biocybersecurity Wargames. In Proceedings of the Future of Information and Communication Conference, San Francisco, CA, USA, 29–30 April 2021; Springer: Berlin, Gemrany, 2021; pp. 666–673. [Google Scholar]
- Hester, R.J. Bioveillance: A Techno-security Infrastructure to Preempt the Dangers of Informationalised Biology. Sci. Cult. 2020, 29, 153–176. [Google Scholar] [CrossRef]
- Mazurczyk, W.; Drobniak, S.; Moore, S. Towards a systematic view on cybersecurity ecology. In Combatting Cybercrime and Cyberterrorism; Springer: Berlin, Gemrany, 2016; pp. 17–37. [Google Scholar]
- Potter, L.; Ayala, O.; Palmer, X.L. Biocybersecurity: A Converging Threat as an Auxiliary to War. In Proceedings of the ICCWS 2021 16th International Conference on Cyber Warfare and Security, Online, 25–26 February 2021; Academic Conferences Limited: Reading, UK, 2021; p. 291. [Google Scholar]
- Palmer, X.; Potter, L.N.; Karahan, S. COVID-19 and biocybersecurity’s increasing role on defending forward. Int. J. Cyber Warf. Terror. (IJCWT) 2021, 11, 15–29. [Google Scholar] [CrossRef]
- Amiri, A.; Shekarchizadeh, M.; Esfahani, A.R.S.; Masoud, G.H. Bio-Cyber Threats and Crimes, the Challenges of the Fourth Industrial Revolution. Bioethics 2021, 81, 97. [Google Scholar]
- Strielkina, A.; Illiashenko, O.; Zhydenko, M.; Uzun, D. Cybersecurity of healthcare IoT-based systems: Regulation and case-oriented assessment. In Proceedings of the 2018 IEEE 9th International Conference on Dependable Systems, Services and Technologies (DESSERT), Kyiv, Ukraine, 24–27 May 2018; IEEE: New York, NY, USA, 2018; pp. 67–73. [Google Scholar]
- Karthick, R.; Ramkumar, R.; Akram, M.; Kumar, M.V. Overcome the challenges in bio-medical instruments using IOT—A review. Mater. Today Proc. 2021, 45, 1614–1619. [Google Scholar] [CrossRef]
- Gui, Y.; Siddiqui, A.S.; Tamore, S.M.; Saqib, F. Investigation of vulnerabilities on smart grid end devices. In Proceedings of the 2019 IEEE CyberPELS (CyberPELS), Knoxville, TN, USA, 29 April–1 May 2019; IEEE: New York, NY, USA, 2019; pp. 1–6. [Google Scholar]
- Guttieres, D.; Stewart, S.; Wolfrum, J.; Springs, S.L. Cyberbiosecurity in advanced manufacturing models. Front. Bioeng. Biotechnol. 2019, 7, 210. [Google Scholar] [CrossRef] [PubMed]
- Schabacker, D.S.; Levy, L.A.; Evans, N.J.; Fowler, J.M.; Dickey, E.A. Assessing cyberbiosecurity vulnerabilities and infrastructure resilience. Front. Bioeng. Biotechnol. 2019, 7, 61. [Google Scholar] [CrossRef] [PubMed]
- Norman, I.; Aikins, M.; Binka, F.; Nyarko, K. Hospital all-risk emergency preparedness in Ghana. Ghana Med. J. 2012, 46, 1–6. [Google Scholar]
- Costa, L.; Barros, J.P.; Tavares, M. Vulnerabilities in IoT devices for smart home environment. In Proceedings of the 5th International Conference on Information Systems Security and Privacy, ICISSP, Prague, Czech Republic, 23–25 February 2019; SciTePress: Vienna, Austria, 2019; Volume 1, pp. 615–622. [Google Scholar]
- Khan, R.; Khan, S.U.; Zaheer, R.; Khan, S. Future internet: The internet of things architecture, possible applications and key challenges. In Proceedings of the 2012 10th International Conference on Frontiers of Information Technology, Islamabad, Pakistan, 17–19 December 2012; IEEE: New York, NY, USA, 2012; pp. 257–260. [Google Scholar]
- Kelly, J.T.; Campbell, K.L.; Gong, E.; Scuffham, P. The Internet of Things: Impact and implications for health care delivery. J. Med. Internet Res. 2020, 22, e20135. [Google Scholar] [CrossRef] [PubMed]
- Affia, A.A.O.; Matulevičius, R.; Nolte, A. Security risk management in cooperative intelligent transportation systems: A systematic literature review. In Proceedings of the OTM Confederated International Conferences on the Move to Meaningful Internet Systems, Rhodes, Greece, 21–25 October 2019; Springer: Berling, Germany, 2019; pp. 282–300. [Google Scholar]
- Sethi, P.; Sarangi, S.R. Internet of things: Architectures, protocols, and applications. J. Electr. Comput. Eng. 2017, 2017, 9324035. [Google Scholar] [CrossRef]
- Miller, D.D.; Brown, E.W. Artificial intelligence in medical practice: The question to the answer? Am. J. Med. 2018, 131, 129–133. [Google Scholar] [CrossRef]
- Dang, L.M.; Piran, M.J.; Han, D.; Min, K.; Moon, H. A survey on internet of things and cloud computing for healthcare. Electronics 2019, 8, 768. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Is the Product a Medical Device; US Food and Drug Administration: Silver Spring, MD, USA, 2018; Volume 17.
- Mahler, T.; Nissim, N.; Shalom, E.; Goldenberg, I.; Hassman, G.; Makori, A.; Kochav, I.; Elovici, Y.; Shahar, Y. Know your enemy: Characteristics of cyber-attacks on medical imaging devices. arXiv 2018, arXiv:1801.05583. [Google Scholar]
- Jesudoss, A.; Daniel, M.J.; Richard, J.J. Intelligent medicine management system and surveillance in IoT environment. In Proceedings of the IOP Conference Series: Materials Science and Engineering, Kazimierz Dolny, Poland, 21–23 November 2019; IOP Publishing: Bristol, UK, 2019; Volume 590, p. 012005. [Google Scholar]
- Peccoud, J.; Gallegos, J.E.; Murch, R.; Buchholz, W.G.; Raman, S. Cyberbiosecurity: From naive trust to risk awareness. Trends Biotechnol. 2018, 36, 4–7. [Google Scholar] [CrossRef]
- Larobina, M.; Murino, L. Medical image file formats. J. Digit. Imaging 2014, 27, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Eichelberg, M.; Kleber, K.; Kämmerer, M. Cybersecurity challenges for PACS and medical imaging. Acad. Radiol. 2020, 27, 1126–1139. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.K.; Anand, A.; Lv, Z.; Ko, H.; Mohan, A. A survey on healthcare data: A security perspective. ACM Trans. Multimid. Comput. Commun. Appl. 2021, 17, 1–26. [Google Scholar] [CrossRef]
- Zarour, M.; Alenezi, M.; Ansari, M.T.J.; Pandey, A.K.; Ahmad, M.; Agrawal, A.; Kumar, R.; Khan, R.A. Ensuring data integrity of healthcare information in the era of digital health. Healthc. Technol. Lett. 2021, 8, 66–77. [Google Scholar] [CrossRef]
- Wang, Z.; Li, Q.; Wang, Y.; Liu, B.; Zhang, J.; Liu, Q. Medical protocol security: DICOM vulnerability mining based on fuzzing technology. In Proceedings of the 2019 ACM SIGSAC Conference on Computer and Communications Security, London, UK, 11–15 November 2019; pp. 2549–2551. [Google Scholar]
- Erol, B.; Gurbuz, S.Z.; Amin, M.G. GAN-based synthetic radar micro-Doppler augmentations for improved human activity recognition. In Proceedings of the 2019 IEEE Radar Conference (RadarConf), Boston, MA, USA, 22–26 April 2019; IEEE: New York, NY, USA, 2019; pp. 1–5. [Google Scholar]
- Shen, Z.; Li, W.; Han, H. Deep Learning-Based Wavelet Threshold Function Optimization on Noise Reduction in Ultrasound Images. Sci. Program. 2021, 2021, 3471327. [Google Scholar] [CrossRef]
- Thiel, A. Biometric identification technologies and the Ghanaian ‘data revolution’. J. Mod. Afr. Stud. 2020, 58, 115–136. [Google Scholar] [CrossRef]
- Bhelonde, A.; Didolkar, N.; Jangale, S.; Kulkarni, N.L. Flexible wound assessment system for diabetic patient using android smartphone. In Proceedings of the 2015 International Conference on Green Computing and Internet of Things (ICGCIoT), Greater Noida, India, 8–10 October 2015; IEEE: New Yok, NY, USA, 2015; pp. 466–469. [Google Scholar]
- Połap, D.; Winnicka, A.; Serwata, K.; Kęsik, K.; Woźniak, M. An intelligent system for monitoring skin diseases. Sensors 2018, 18, 2552. [Google Scholar] [CrossRef]
- Shimizu, E.; Ogawa, Y.; Yazu, H.; Aketa, N.; Yang, F.; Yamane, M.; Sato, Y.; Kawakami, Y.; Tsubota, K. “Smart Eye Camera”: An innovative technique to evaluate tear film breakup time in a murine dry eye disease model. PLoS ONE 2019, 14, e0215130. [Google Scholar] [CrossRef]
- Ernst, T.; Guillemaud, R.; Mailley, P.; Polizzi, J.; Koenig, A.; Boisseau, S.; Pauliac-Vaujour, E.; Plantier, C.; Delapierre, G.; Saoutieff, E.; et al. Sensors and related devices for IoT, medicine and s mart-living. In Proceedings of the 2018 IEEE Symposium on VLSI Technology, Honolulu, HI, USA, 18–22 June 2018; IEEE: New York, NY, USA, 2018; pp. 35–36. [Google Scholar]
- Hameed, S.S.; Hassan, W.H.; Latiff, L.A.; Ghabban, F. A systematic review of security and privacy issues in the internet of medical things; the role of machine learning approaches. PeerJ Comput. Sci. 2021, 7, e414. [Google Scholar] [CrossRef]
- Debar, H.; Beuran, R.; Tan, Y. A Quantitative Study of Vulnerabilities in the Internet of Medical Things. In Proceedings of the ICISSP, Floriana, Malta, 25–27 February 2020; pp. 164–175. [Google Scholar]
- Hudson, F.; Clark, C. Wearables and medical interoperability: The evolving frontier. Computer 2018, 51, 86–90. [Google Scholar] [CrossRef]
- Valanarasu, M.R. Smart and secure IoT and AI integration framework for hospital environment. J. ISMAC 2019, 1, 172–179. [Google Scholar]
- Majumder, S.; Chen, L.; Marinov, O.; Chen, C.H.; Mondal, T.; Deen, M.J. Noncontact wearable wireless ECG systems for long-term monitoring. IEEE Rev. Biomed. Eng. 2018, 11, 306–321. [Google Scholar] [CrossRef] [PubMed]
- Sposaro, F.; Tyson, G. iFall: An Android application for fall monitoring and response. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–5 September 2009; IEEE: New York, NY, USA, 2009; pp. 6119–6122. [Google Scholar]
- Kakria, P.; Tripathi, N.; Kitipawang, P. A real-time health monitoring system for remote cardiac patients using smartphone and wearable sensors. Int. J. Telemed. Appl. 2015, 2015, 8. [Google Scholar] [CrossRef] [PubMed]
- Gruzelier, J.H. EEG-neurofeedback for optimising performance. I: A review of cognitive and affective outcome in healthy participants. Neurosci. Biobehav. Rev. 2014, 44, 124–141. [Google Scholar] [CrossRef] [PubMed]
- Tedesco, S.; Sica, M.; Ancillao, A.; Timmons, S.; Barton, J.; O’Flynn, B. Accuracy of consumer-level and research-grade activity trackers in ambulatory settings in older adults. PLoS ONE 2019, 14, e0216891. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, W.; Michael, K. The Implications of Neuralink and Brain Machine Interface Technologies. In Proceedings of the 2020 IEEE International Symposium on Technology and Society (ISTAS), Tempe, AZ, USA, 12–15 November 2020; IEEE: New York, NY, USA, 2020; pp. 201–203. [Google Scholar]
- Zhu, D.; Bieger, J.; Garcia Molina, G.; Aarts, R.M. A survey of stimulation methods used in SSVEP-based BCIs. Comput. Intell. Neurosci. 2010, 2010, 1–12. [Google Scholar] [CrossRef]
- Liu, Q.; Chen, K.; Ai, Q.; Xie, S.Q. Recent development of signal processing algorithms for SSVEP-based brain computer interfaces. J. Med. Biol. Eng. 2014, 34, 299–309. [Google Scholar] [CrossRef]
- Chevallier, S.; Kalunga, E.K.; Barthélemy, Q.; Monacelli, E. Review of Riemannian distances and divergences, applied to SSVEP-based BCI. Neuroinformatics 2021, 19, 93–106. [Google Scholar] [CrossRef]
- Moutinho, S. Scientists Entered People’s Dreams and Got Them ‘Talking’. 2021. Available online: https://www.science.org/content/article/scientists-entered-peoples-dreams-and-got-them-talking? (accessed on 3 January 2023).
- Leavitt, N. Researchers fight to keep implanted medical devices safe from hackers. Computer 2010, 43, 11–14. [Google Scholar] [CrossRef]
- Rostami, M.; Juels, A.; Koushanfar, F. Heart-to-heart (H2H) authentication for implanted medical devices. In Proceedings of the 2013 ACM SIGSAC Conference on Computer & Communications Security, Berlin, Germany, 4–8 November 2013; pp. 1099–1112. [Google Scholar]
- Tabasum, A.; Safi, Z.; AlKhater, W.; Shikfa, A. Cybersecurity issues in implanted medical devices. In Proceedings of the 2018 International Conference on Computer and Applications (ICCA), Beirut, Lebanon, 25–26 August 2018; IEEE: New York, NY, USA, 2018; pp. 1–9. [Google Scholar]
- Zanjal, S.V.; Talmale, G.R. Medicine reminder and monitoring system for secure health using IOT. Procedia Comput. Sci. 2016, 78, 471–476. [Google Scholar] [CrossRef]
- Yaacoub, J.P.A.; Noura, M.; Noura, H.N.; Salman, O.; Yaacoub, E.; Couturier, R.; Chehab, A. Securing internet of medical things systems: Limitations, issues and recommendations. Future Gener. Comput. Syst. 2020, 105, 581–606. [Google Scholar] [CrossRef]
- Aman, A.H.M.; Hassan, W.H.; Sameen, S.; Attarbashi, Z.S.; Alizadeh, M.; Latiff, L.A. IoMT amid COVID-19 pandemic: Application, architecture, technology, and security. J. Netw. Comput. Appl. 2021, 174, 102886. [Google Scholar] [CrossRef] [PubMed]
- Sangave, N.A.; Aungst, T.D.; Patel, D.K. Smart connected insulin pens, caps, and attachments: A review of the future of diabetes technology. Diabetes Spectr. 2019, 32, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Thamilarasu, G.; Odesile, A.; Hoang, A. An intrusion detection system for internet of medical things. IEEE Access 2020, 8, 181560–181576. [Google Scholar] [CrossRef]
- Onik, M.F.A.; Anam, K.; Rashid, N. A secured cloud based health care data management system. Int. J. Comput. Appl. 2012, 49, 1–7. [Google Scholar]
- Ilievski, A.; Dojchinovski, D.; Gusev, M. Interactive voice assisted home healthcare systems. In Proceedings of the 9th Balkan Conference on Informatics, Sofia, Bulgaria, 26–28 September 2019; pp. 1–5. [Google Scholar]
- Tao, V.; Moy, K.; Amirfar, V.A. A little robot with big promise may be future of personalized health care. Pharm. Today 2016, 22, 38. [Google Scholar] [CrossRef]
- Vanhove, M.P.; Rochette, A.J.; de Bisthoven, L.J. Joining science and policy in capacity development for monitoring progress towards the Aichi Biodiversity Targets in the global South. Ecol. Indic. 2017, 73, 694–697. [Google Scholar] [CrossRef]
- Wall, P.; Saxena, D.; Brown, S. Artificial Intelligence in the Global South (AI4D): Potential and Risks. arXiv 2021, arXiv:2108.10093. [Google Scholar]
- Davies, M. Biometrics, surveillance technologies and the rise of the ‘security state’ in South Africa. Africa LSE. 2017. Available online: https://blogs.lse.ac.uk/africaatlse/2017/03/22/biometrics-surveillance-technologies-and-the-rise-of-the-security-state-in-south-africa/ (accessed on 1 July 2022).
- Gong, T.; Huang, H.; Li, P.; Zhang, K.; Jiang, H. A medical healthcare system for privacy protection based on IoT. In Proceedings of the 2015 Seventh International Symposium on Parallel Architectures, Algorithms and Programming (PAAP), Nanjing, China, 12–14 December 2015; IEEE: New York, NY, USA, 2015; pp. 217–222. [Google Scholar]
- Subramoniam, S.; Sadi, S. Healthcare 2.0. IT Prof. 2010, 12, 46–51. [Google Scholar] [CrossRef]
- Drake, R.; Ridder, E. Healthcare Cybersecurity Vulnerabilities. In Proceedings of the International Conference on Cybersecurity and Cybercrime, Boston, MA, USA, 16–18 November 2022; Volume 9, pp. 49–56. [Google Scholar]
- Alkinoon, M.; Choi, S.J.; Mohaisen, D. Measuring healthcare data breaches. In Proceedings of the Information Security Applications: 22nd International Conference, WISA 2021, Jeju Island, Republic of Korea, 11–13 August 2021; Revised Selected Papers 22. Springer: Berlin, Germany, 2021; pp. 265–277. [Google Scholar]
- Wang, W.; Kiik, M.; Peek, N.; Curcin, V.; Marshall, I.J.; Rudd, A.G.; Wang, Y.; Douiri, A.; Wolfe, C.D.; Bray, B. A systematic review of machine learning models for predicting outcomes of stroke with structured data. PLoS ONE 2020, 15, e0234722. [Google Scholar]
- Zuiderwijk, A.; Chen, Y.C.; Salem, F. Implications of the use of artificial intelligence in public governance: A systematic literature review and a research agenda. Gov. Inf. Q. 2021, 38, 101577. [Google Scholar] [CrossRef]
- Cuningkin, V.; Riley, E.; Rainey, L. Preventing Medjacking. AJN Am. J. Nurs. 2021, 121, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Draft Guidance for Industry and Food and Drug Administration Staff: Content of Premarket Submissions for Management of Cybersecurity in Medical Devices. 2014. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/content-premarket-submissions-management-cybersecurity-medical-devices (accessed on 1 July 2022).
- Food and Drug Administration. Medical Device Safety Action Plan: Protecting Patients, Promoting Public Health. 2019. Available online: https://www.fda.gov/about-fda/cdrh-reports/medical-device-safety-action-plan-protecting-patients-promoting-public-health (accessed on 1 July 2022).
- Akogo, D.A.; Appiah, V.; Palmer, X.L. CellLineNet: End-to-end learning and transfer learning for multiclass epithelial breast cell line classification via a convolutional neural network. arXiv 2018, arXiv:1808.06041. [Google Scholar]
- van der Wal, D.; Jhun, I.; Laklouk, I.; Nirschl, J.; Richer, L.; Rojansky, R.; Theparee, T.; Wheeler, J.; Sander, J.; Feng, F.; et al. Biological data annotation via a human-augmenting AI-based labeling system. NPJ Digit. Med. 2021, 4, 145. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.T.; Park, T.J.; Islam, A.N.; Tran, D.S.; Manna, S.; Wang, Q.; Mondal, S.; Yu, H.; Banik, S.; Cheng, S.; et al. Reconfigurable perovskite nickelate electronics for artificial intelligence. Science 2022, 375, 533–539. [Google Scholar] [CrossRef]
- Sibi Chakkaravarthy, S.; Sangeetha, D.; Venkata Rathnam, M.; Srinithi, K.; Vaidehi, V. Futuristic cyber-attacks. Int. J. Knowl.-Based Intell. Eng. Syst. 2018, 22, 195–204. [Google Scholar] [CrossRef]
- Srinivas, M.; Durgaprasadarao, P.; Raj, V.N.P. Intelligent medicine box for medication management using IoT. In Proceedings of the 2018 2nd International Conference on Inventive Systems and Control (ICISC), Coimbatore, India, 19–20 January 2018; IEEE: New York, NY, USA, 2018; pp. 32–34. [Google Scholar]
- Gehl Sampath, P. Governing artificial intelligence in an age of inequality. Glob. Policy 2021, 12, 21–31. [Google Scholar] [CrossRef]
- Hooker, S. Moving beyond “algorithmic bias is a data problem”. Patterns 2021, 2, 100241. [Google Scholar] [CrossRef]
- Web Titan. Tardigrade Malware Used in Targeted Attacks on Vaccine Manufacturers and Biomedical Firms. 2021. Available online: https://www.webtitan.com/blog/tardigrade-malware-vaccine-manufacturers-biomedical-firms/ (accessed on 3 January 2023).
- Dubois, É.; Heymans, P.; Mayer, N.; Matulevičius, R. A systematic approach to define the domain of information system security risk management. In Intentional Perspectives on Information Systems Engineering; Springer: Berlin Germany, 2010; pp. 289–306. [Google Scholar]
- Affia, A.A.O.; Matulevičius, R. Securing an MQTT-based Traffic Light Perception System for Autonomous Driving. In Proceedings of the 2021 IEEE International Conference on Cyber Security and Resilience (CSR), Rhodes, Greece, 26–28 July 2021; IEEE: New York, NY, USA, 2021; pp. 255–260. [Google Scholar]
- Abasi-amefon, O.A.; Matulevičius, R.; Tõnisson, R. Security Risk Estimation and Management in Autonomous Driving Vehicles. In Proceedings of the International Conference on Advanced Information Systems Engineering, Melbourne, VIC, Australia, 28 June–2 July 2021; Springer: Berlin, Germany, 2021; pp. 11–19. [Google Scholar]
- Nist, N. Risk management guide for information technology systems. NIST Spec. Publ. 2002, 800, 800–830. [Google Scholar]
- Caralli, R.A.; Stevens, J.F.; Young, L.R.; Wilson, W.R. Introducing Octave Allegro: Improving the Information Security Risk Assessment Process; Technical report; Carnegie-Mellon University, Software Engineering Institute: Pittsburgh, PA, USA, 2007. [Google Scholar]
- Wynn, J.; Whitmore, J.; Upton, G.; Spriggs, L.; McKinnon, D.; McInnes, R.; Graubart, R.; Clausen, L. Threat Assessment & Remediation Analysis (TARA): Methodology Description Version 1.0; Technical report; The MITRE Corporation: Bedford, MA, USA, 2011. [Google Scholar]
- Affia, A.A.O.; Nolte, A.; Matulevičius, R. IoT Security Risk Management: A Framework and Teaching Approach. Informatics Educ. 2023, 22. [Google Scholar] [CrossRef]
- Affia, A.a.O.; Matulevičius, R.; Nolte, A. Security Risk Management in E-commerce Systems: A Threat-driven Approach. Balt. J. Mod. Comput. 2020, 8, 213–240. [Google Scholar]
- Matulevičius, R. Fundamentals of Secure System Modelling; Springer: Berlin, Germany, 2017. [Google Scholar]
- Shostack, A. Threat Modeling: Designing for Security; John Wiley & Sons: Hoboken, NJ, USA, 2014. [Google Scholar]
- Jabeen, T.; Ashraf, H.; Ullah, A. A survey on healthcare data security in wireless body area networks. J. Ambient. Intell. Humaniz. Comput. 2021, 12, 9841–9854. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.A.; Woodward, A.J. Cybersecurity vulnerabilities in medical devices: A complex environment and multifaceted problem. Med. Devices 2015, 8, 305. [Google Scholar] [CrossRef] [PubMed]
- Aghili, S.F.; Mala, H.; Kaliyar, P.; Conti, M. SecLAP: Secure and lightweight RFID authentication protocol for Medical IoT. Future Gener. Comput. Syst. 2019, 101, 621–634. [Google Scholar] [CrossRef]
- Cummins, G. Smart pills for gastrointestinal diagnostics and therapy. Adv. Drug Deliv. Rev. 2021, 177, 113931. [Google Scholar] [CrossRef]
- Mancini, M. Medical identity theft in the emergency department: Awareness is crucial. West. J. Emerg. Med. 2014, 15, 899. [Google Scholar] [CrossRef]
- Stine, I.; Rice, M.; Dunlap, S.; Pecarina, J. A cyber risk scoring system for medical devices. Int. J. Crit. Infrastruct. Prot. 2017, 19, 32–46. [Google Scholar] [CrossRef]
- Lesaja, S.; Palmer, X.L. Brain-Computer Interfaces and the Dangers of Neurocapitalism. arXiv 2020, arXiv:2009.07951. [Google Scholar]
- Pycroft, L.; Boccard, S.G.; Owen, S.L.; Stein, J.F.; Fitzgerald, J.J.; Green, A.L.; Aziz, T.Z. Brainjacking: Implant security issues in invasive neuromodulation. World Neurosurg. 2016, 92, 454–462. [Google Scholar] [CrossRef]
- Wood, D.; Apthorpe, N.; Feamster, N. Cleartext data transmissions in consumer iot medical devices. In Proceedings of the 2017 Workshop on Internet of Things Security and Privacy, Dallas, TX, USA, 3 November 2017; pp. 7–12. [Google Scholar]
- Kim, J. Energy-efficient dynamic packet downloading for medical IoT platforms. IEEE Trans. Ind. Inform. 2015, 11, 1653–1659. [Google Scholar] [CrossRef]
- Chauhan, A. Robotics and automation: The rescuers of COVID era. In Artificial Intelligence for COVID-19; Springer: Berlin Germany, 2021; pp. 119–151. [Google Scholar]
- Lepasepp, T.K.; Hurst, W. A systematic literature review of industry 4.0 technologies within medical device manufacturing. Future Internet 2021, 13, 264. [Google Scholar] [CrossRef]
- Richmond, S. Stopping The Attacks: Cybersecurity In Healthcare Manufacturing. 2021. Available online: https://www.forbes.com/sites/forbestechcouncil/2021/08/17/stopping-the-attacks-cybersecurity-in-healthcare-manufacturing/?sh=4db312231a8d (accessed on 3 January 2023).
- Shen, M.; Deng, Y.; Zhu, L.; Du, X.; Guizani, N. Privacy-preserving image retrieval for medical IoT systems: A blockchain-based approach. IEEE Netw. 2019, 33, 27–33. [Google Scholar] [CrossRef]
- Sun, Y.; Lo, F.P.W.; Lo, B. Security and privacy for the internet of medical things enabled healthcare systems: A survey. IEEE Access 2019, 7, 183339–183355. [Google Scholar] [CrossRef]
- Hatzivasilis, G.; Soultatos, O.; Ioannidis, S.; Verikoukis, C.; Demetriou, G.; Tsatsoulis, C. Review of security and privacy for the Internet of Medical Things (IoMT). In Proceedings of the 2019 15th international conference on distributed computing in sensor systems (DCOSS), Santorini Island, Greece, 29–31 May 2019; IEEE: New York, NY, USA, 2019; pp. 457–464. [Google Scholar]
- Arpaia, P.; Bonavolontà, F.; Cioffi, A.; Moccaldi, N. Power Measurement-based Vulnerability Assessment of IoT medical devices at varying countermeasures for cybersecurity. IEEE Trans. Instrum. Meas. 2021, 70, 1–9. [Google Scholar] [CrossRef]
- Jackson, G.W., Jr.; Rahman, S. Exploring Challenges and Opportunities in Cybersecurity Risk and Threat Communications Related To The Medical Internet Of Things (MIoT). arXiv 2019, arXiv:1908.00666. [Google Scholar] [CrossRef]
- Mirsky, Y.; Mahler, T.; Shelef, I.; Elovici, Y. {CT-GAN}: Malicious Tampering of 3D Medical Imagery using Deep Learning. In Proceedings of the 28th USENIX Security Symposium (USENIX Security 19), Santa Clara, CA, USA, 14–16 August 2019; pp. 461–478. [Google Scholar]
- Chen, P.; Desmet, L.; Huygens, C. A study on advanced persistent threats. In Proceedings of the Communications and Multimedia Security: 15th IFIP TC 6/TC 11 International Conference, CMS 2014, Aveiro, Portugal, 25–26 September 2014; Proceedings 15. Springer: Berlin, Germany, 2014; pp. 63–72. [Google Scholar]
- Moore, T. The economics of cybersecurity: Principles and policy options. Int. J. Crit. Infrastruct. Prot. 2010, 3, 103–117. [Google Scholar] [CrossRef]
- Hu, P.; Li, H.; Fu, H.; Cansever, D.; Mohapatra, P. Dynamic defense strategy against advanced persistent threat with insiders. In Proceedings of the 2015 IEEE Conference on Computer Communications (INFOCOM), Hong Kong, China, 26 April–1 May 2015; IEEE: New York, NY, USA, 2015; pp. 747–755. [Google Scholar]
- Palmer, X.L.; Potter, L.; Karahan, S. An Exploration on APTs in Biocybersecurity and Cyberbiosecurity. In Proceedings of the International Conference on Cyber Warfare and Security, Albany, NY, USA, 17–18 March 2022; Volume 17, pp. 532–535. [Google Scholar]
- BIO-ISAC Media. BIO-ISAC Releases Advisory to Biomanufacturers. 2021. Available online: https://www.isac.bio/post/tardigrade (accessed on 3 January 2023).
- Newaz, A.I.; Sikder, A.K.; Rahman, M.A.; Uluagac, A.S. A survey on security and privacy issues in modern healthcare systems: Attacks and defenses. ACM Trans. Comput. Healthc. 2021, 2, 1–44. [Google Scholar] [CrossRef]
- Martínez, A.L.; Pérez, M.G.; Ruiz-Martínez, A. A comprehensive review of the state of the art on security and privacy issues in Healthcare. ACM Comput. Surv. 2022, 55, 1–38. [Google Scholar] [CrossRef]
- Zubair, M.; Unal, D.; Al-Ali, A.; Shikfa, A. Exploiting bluetooth vulnerabilities in e-health IoT devices. In Proceedings of the 3rd International Conference on Future Networks and Distributed Systems, Paris, France, 1–2 July 2019; pp. 1–7. [Google Scholar]
- Perez, A.J.; Zeadally, S. Recent advances in wearable sensing technologies. Sensors 2021, 21, 6828. [Google Scholar] [CrossRef]
- Choi, J.; Choi, C.; Kim, S.; Ko, H. Medical information protection frameworks for smart healthcare based on IoT. In Proceedings of the 9th International Conference on Web Intelligence, Mining and Semantics, Seoul, Republic of Korea, 26–28 June 2019; pp. 1–5. [Google Scholar]
- Mohanthy, S.B. Real time internet application with distributed flow environment for medical IoT. In Proceedings of the 2015 International Conference on Green Computing and Internet of Things (ICGCIoT), Greater Noida, India, 8–10 October 2015; IEEE: New York, NY, USA, 2015; pp. 832–837. [Google Scholar]
- Roy, M.; Chowdhury, C.; Aslam, N. Designing transmission strategies for enhancing communications in medical IoT using Markov decision process. Sensors 2018, 18, 4450. [Google Scholar] [CrossRef]
- Xu, B.; Da Xu, L.; Cai, H.; Xie, C.; Hu, J.; Bu, F. Ubiquitous data accessing method in IoT-based information system for emergency medical services. IEEE Trans. Ind. Infom. 2014, 10, 1578–1586. [Google Scholar]
- Elhoseny, M.; Ramírez-González, G.; Abu-Elnasr, O.M.; Shawkat, S.A.; Arunkumar, N.; Farouk, A. Secure medical data transmission model for IoT-based healthcare systems. IEEE Access 2018, 6, 20596–20608. [Google Scholar] [CrossRef]
- Atat, R.; Liu, L.; Ashdown, J.; Medley, M.J.; Matyjas, J.D.; Yi, Y. A physical layer security scheme for mobile health cyber-physical systems. IEEE Internet Things J. 2017, 5, 295–309. [Google Scholar] [CrossRef]
- Mashima, D.; Ahamad, M. Enabling Robust Information Accountability in E-healthcare Systems. In Proceedings of the HealthSec, Bellevue, WA, USA, 8–10 August 2012. [Google Scholar]
- Blough, D.M.; Liu, L.; Sainfort, F.; Ahamad, M. CT-T: MedVault-Ensuring Security and Privacy for Electronic Medical Records; Technical report; Georgia Institute of Technology: Atlanta, GA, USA, 2011. [Google Scholar]
- Mashima, D.; Srivastava, A.; Giffin, J.T.; Ahamad, M. Protecting E-healthcare Client Devices against Malware and Physical Theft. In Proceedings of the HealthSec, Washington, DC, USA, 11–13 August 2010. [Google Scholar]
- Halstead, S. Educating Health Organization on Cyber Threats. Ph.D. Thesis, Utica College, Utica, NY, USA, 2021. [Google Scholar]
- McMahon, E.; Williams, R.; El, M.; Samtani, S.; Patton, M.; Chen, H. Assessing medical device vulnerabilities on the Internet of Things. In Proceedings of the 2017 IEEE International Conference on Intelligence and Security Informatics (ISI), Beijing, China, 22–24 July 2017; IEEE: New York, NY, USA, 2017; pp. 176–178. [Google Scholar]
- Lee, Y.S.; Alasaarela, E.; Lee, H. Secure key management scheme based on ECC algorithm for patient’s medical information in healthcare system. In Proceedings of the The International Conference on Information Networking 2014 (ICOIN2014), Phuket, Thailand, 10–12 February 2014; IEEE: New York, NY, USA, 2014; pp. 453–457. [Google Scholar]
- Wu, L.; Chi, H.; Du, X. A Secure Proxy-based Access Control Scheme for Implantable Medical Devices. arXiv 2018, arXiv:1803.07751. [Google Scholar]
- Marwan, M.; Karti, A.; Ouahmane, H. Proposal for a secure data sharing and processing in cloud applications for healthcare domain. Int. J. Inf. Technol. Appl. Sci. 2021, 3, 10–17. [Google Scholar] [CrossRef]
- Ren, J.; Li, J.; Liu, H.; Qin, T. Task offloading strategy with emergency handling and blockchain security in SDN-empowered and fog-assisted healthcare IoT. Tsinghua Sci. Technol. 2021, 27, 760–776. [Google Scholar] [CrossRef]
- Mehta, R.; Parmar, M. Trust based mechanism for securing iot routing protocol rpl against wormhole & grayhole attacks. In Proceedings of the 2018 3rd International Conference for Convergence in Technology (I2CT), Pune, India, 6–8 April 2018; IEEE: New York, NY, USA, 2018; pp. 1–6. [Google Scholar]
- Rizvi, S.; Kurtz, A.; Pfeffer, J.; Rizvi, M. Securing the internet of things (IoT): A security taxonomy for IoT. In Proceedings of the 2018 17th IEEE International Conference On Trust, Security and Privacy in Computing and Communications/12th IEEE International Conference on Big Data Science and Engineering (TrustCom/BigDataSE), New York, NY, USA, 1–3 August 2018; IEEE: New York, NY, USA, 2018; pp. 163–168. [Google Scholar]
- Dinculeană, D.; Cheng, X. Vulnerabilities and limitations of MQTT protocol used between IoT devices. Appl. Sci. 2019, 9, 848. [Google Scholar] [CrossRef]
- Tang, W.; Ren, J.; Deng, K.; Zhang, Y. Secure data aggregation of lightweight E-healthcare IoT devices with fair incentives. IEEE Internet Things J. 2019, 6, 8714–8726. [Google Scholar] [CrossRef]
- Chen, Y.; Qin, X.; Wang, J.; Yu, C.; Gao, W. Fedhealth: A federated transfer learning framework for wearable healthcare. IEEE Intell. Syst. 2020, 35, 83–93. [Google Scholar] [CrossRef]
- Cao, F.; Huang, H.K.; Zhou, X. Medical image security in a HIPAA mandated PACS environment. Comput. Med. Imaging Graph. 2003, 27, 185–196. [Google Scholar] [CrossRef]
- Singh, A.K.; Kumar, B.; Singh, G.; Mohan, A. Medical image watermarking techniques: A technical survey and potential challenges. In Medical Image Watermarking: Techniques and Applications; Springer: Berlin Germany, 2017; pp. 13–41. [Google Scholar]
- Ghoneim, A.; Muhammad, G.; Amin, S.U.; Gupta, B. Medical image forgery detection for smart healthcare. IEEE Commun. Mag. 2018, 56, 33–37. [Google Scholar] [CrossRef]
- Huang, H. Pacs-Based Multimedia Imaging Informatics: Basic Principles and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Widup, S.; Bassett, G.; Hylender, D.; Rudis, B.; Spitler, M. 2015 Verizon Protected Health Information Data Breach Report. 2015. Available online: https://www.researchgate.net/publication/289254312_2015_Verizon_Protected_Health_Information_Data_Breach_Report (accessed on 1 July 2022).
- Epia Realpe, L.F.; Parra, O.J.S.; Velandia, J.B. Use of KRACK Attack to Obtain Sensitive Information. In Proceedings of the Mobile, Secure, and Programmable Networking: 4th International Conference, MSPN 2018, Paris, France, 18–20 June 2018; Revised Selected Papers 4. Springer: Berlin, Germany, 2019; pp. 270–276. [Google Scholar]
- Seri, B.; Vishnepolsky, G.; Zusman, D. BLEEDINGBIT: The Hidden Attack Surface within BLE Chips. 2019. Available online: https://info.armis.com/rs/645-PDC-047/images/Armis-BLEEDINGBIT-Technical-White-Paper-WP.pdf (accessed on 1 July 2022).
- Siwicki, B. Cloud-Based Pacs System Cuts Imaging Costs by Half for Rural Hospital | Healthcare IT News. Available online: https://www.healthcareitnews.com/news/cloud-based-pacs-system-cuts-imaging-costs-half-rural-hospital (accessed on 3 January 2023).
- Ney, P.; Koscher, K.; Organick, L.; Ceze, L.; Kohno, T. Computer Security, Privacy, and DNA Sequencing: Compromising Computers with Synthesized DNA, Privacy Leaks, and More. In Proceedings of the USENIX Security Symposium, Vancouver, BC, Canada, 16–18 August 2017; Volume 26, pp. 765–779. [Google Scholar]
- Puzis, R.; Farbiash, D.; Brodt, O.; Elovici, Y.; Greenbaum, D. Increased cyber-biosecurity for DNA synthesis. Nat. Biotechnol. 2020, 38, 1379–1381. [Google Scholar] [CrossRef] [PubMed]
- Faezi, S.; Chhetri, S.R.; Malawade, A.V.; Chaput, J.C.; Grover, W.; Brisk, P.; Al Faruque, M.A. Oligo-snoop: A non-invasive side channel attack against DNA synthesis machines. In Proceedings of the Network and Distributed Systems Security (NDSS) Symposium, San Diego, CA, USA, 24–27 February 2019. [Google Scholar]
- Faezi, S.; Chhetri, S.R.; Malawade, A.V.; Chaput, J.C.; Grover, W.; Brisk, P.; Al Faruque, M.A. Acoustic Side Channel Attack Against DNA Synthesis Machines. In Proceedings of the 2020 ACM/IEEE 11th International Conference on Cyber-Physical Systems (ICCPS), Sydney, NSW, Australia, 21–25 April 2020; IEEE: New York, NY, USA, 2020; pp. 186–187. [Google Scholar]
- Oliveira, A.R.d.; Hunt, J.; Valverde, N.; Brandao-Mello, C.; Farina, R. Medical and related aspects of the Goiania accident: An overview. Health Phys. 1991, 60, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Kurnot, J.; Kuca, M.; Neidigk, S. Case Study on the Effectiveness of Mechanical Attack Testing to Help Determine Vulnerabilities of a Device that Contains Radiological Material and Proven Methods of Addressing such Vulnerabilities. In Proceedings of the International Conference on the Security of Radioactive Material: The Way Forward for Prevention and Detection, Vienna, Austria, 3–7 December 2018. [Google Scholar]
- Choo, K.K.R.; Gai, K.; Chiaraviglio, L.; Yang, Q. A multidisciplinary approach to Internet of Things (IoT) cybersecurity and risk management. Comput. Secur. 2021, 102, 102136. [Google Scholar] [CrossRef]
- International Atomic Energy Agency. Security of Radioactive Material in Use and Storage and of Associated Facilities; Number 11-G (Rev.1) in Implementing Guides; International Atomic Energy Agency (IAEA): Vienna, Austria, 2019. [Google Scholar]
- Darwish, S.; Nouretdinov, I.; Wolthusen, S.D. Towards composable threat assessment for medical IoT (MIoT). Procedia Comput. Sci. 2017, 113, 627–632. [Google Scholar] [CrossRef]
- Umayam, M.L. Possibilities of Blockchain Technology for Nuclear Security. In Blockchain for International Security: The Potential of Distributed Ledger Technology for Nonproliferation and Export Controls; Springer: Berlin, Germany, 2021; pp. 55–73. [Google Scholar]
- Rane, S.; Harris, J.T. A Game Theoretical Model of Radiological Terrorism Defense. Int. J. Nucl. Secur. 2021, 7, 7. [Google Scholar] [CrossRef]
- Mueller, S. Facing the 2020 pandemic: What does cyberbiosecurity want us to know to safeguard the future? Biosaf. Health 2021, 3, 11–21. [Google Scholar] [CrossRef]
- Mantle, J.L.; Rammohan, J.; Romantseva, E.F.; Welch, J.T.; Kauffman, L.R.; McCarthy, J.; Schiel, J.; Baker, J.C.; Strychalski, E.A.; Rogers, K.C.; et al. Cyberbiosecurity for biopharmaceutical products. Front. Bioeng. Biotechnol. 2019, 7, 116. [Google Scholar] [CrossRef]
- Millett, K.; Dos Santos, E.; Millett, P.D. Cyber-biosecurity risk perceptions in the biotech sector. Front. Bioeng. Biotechnol. 2019, 7, 136. [Google Scholar] [CrossRef]
- Lee, K.F.; Qiufan, C. AI 2041: Ten Visions for Our Future; Currency: Sydney, NSW, Australia, 2021. [Google Scholar]
- Schlatt, V.; Guggenberger, T.; Schmid, J.; Urbach, N. Attacking the trust machine: Developing an information systems research agenda for blockchain cybersecurity. Int. J. Inf. Manag. 2022, 68, 102470. [Google Scholar] [CrossRef]
- Alblooshi, M.; Salah, K.; Alhammadi, Y. Blockchain-based ownership management for medical IoT (MIoT) devices. In Proceedings of the 2018 International Conference on Innovations in Information Technology (IIT), Al Ain, United Arab Emirates, 18–19 November 2018; IEEE: New York, NY, USA, 2018; pp. 151–156. [Google Scholar]
- Chandrasekaran, S.; Subramaniam, R. Why IoT Sensors Need Standards—They Could Improve Performance and Spur Development of New Applications. 2022. Available online: https://spectrum.ieee.org/why-iot-sensors-need-standards (accessed on 3 January 2023).
- Hardman, A.; Martin, W. Risk Management Framework for DoD Medical Devices. In Proceedings of the HIMSS’18, Las Vegas, NV, USA, 5–9 March 2019. [Google Scholar]
- George, A.M. The national security implications of cyberbiosecurity. Front. Bioeng. Biotechnol. 2019, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.; Rudzicz, F.; Jamieson, T.; Goldfarb, A. Artificial intelligence and the implementation challenge. J. Med. Internet Res. 2019, 21, e13659. [Google Scholar] [CrossRef]
- Jia, Z.; Wang, Z.; Hong, F.; Ping, L.; Shi, Y.; Hu, J. Personalized deep learning for ventricular arrhythmias detection on medical IoT systems. In Proceedings of the 39th International Conference on Computer-Aided Design, Online, 2–5 November 2020; pp. 1–9. [Google Scholar]
- Fang, L.; Li, Y.; Liu, Z.; Yin, C.; Li, M.; Cao, Z.J. A practical model based on anomaly detection for protecting medical IoT control services against external attacks. IEEE Trans. Ind. Inform. 2020, 17, 4260–4269. [Google Scholar] [CrossRef]
- Kruk, M.E.; Gage, A.D.; Joseph, N.T.; Danaei, G.; García-Saisó, S.; Salomon, J.A. Mortality due to low-quality health systems in the universal health coverage era: A systematic analysis of amenable deaths in 137 countries. Lancet 2018, 392, 2203–2212. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.x.; Qian, P.; Bi, D.; Ye, Z.w.; He, X.; Zhao, Y.h.; Su, L.; Li, S.l.; Zhu, Z.l. Application of AI and IoT in clinical medicine: Summary and challenges. Curr. Med. Sci. 2021, 41, 1134–1150. [Google Scholar] [CrossRef]
- Isgut, M.; Gloster, L.; Choi, K.; Venugopalan, J.; Wang, M.D. Systematic Review of Advanced AI Methods for Improving Healthcare Data Quality In Post COVID-19 Era. IEEE Rev. Biomed. Eng. 2022, 16, 53–69. [Google Scholar] [CrossRef]
- Wahl, B.; Cossy-Gantner, A.; Germann, S.; Schwalbe, N.R. Artificial intelligence (AI) and global health: How can AI contribute to health in resource-poor settings? BMJ Glob. Health 2018, 3, e000798. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Jiang, Y.; Zhi, H.; Dong, Y.; Li, H.; Ma, S.; Wang, Y.; Dong, Q.; Shen, H.; Wang, Y. Artificial intelligence in healthcare: Past, present and future. Stroke Vasc. Neurol. 2017, 2, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Antwi, W.K.; Akudjedu, T.N.; Botwe, B.O. Artificial intelligence in medical imaging practice in Africa: A qualitative content analysis study of radiographers’ perspectives. Insights Imaging 2021, 12, 80. [Google Scholar] [CrossRef]
- Ali, O.; Abdelbaki, W.; Shrestha, A.; Elbasi, E.; Alryalat, M.A.A.; Dwivedi, Y.K. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. J. Innov. Knowl. 2023, 8, 100333. [Google Scholar] [CrossRef]
- Urbina, F.; Lentzos, F.; Invernizzi, C.; Ekins, S. Dual use of artificial-intelligence-powered drug discovery. Nat. Mach. Intell. 2022, 4, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Kumar, Y.; Koul, A.; Singla, R.; Ijaz, M.F. Artificial intelligence in disease diagnosis: A systematic literature review, synthesizing framework and future research agenda. J. Ambient. Intell. Humaniz. Comput. 2022, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Bajgain, B.; Lorenzetti, D.; Lee, J.; Sauro, K. Determinants of implementing artificial intelligence-based clinical decision support tools in healthcare: A scoping review protocol. BMJ Open 2023, 13, e068373. [Google Scholar] [CrossRef] [PubMed]
- Kleinberg, G.; Diaz, M.J.; Batchu, S.; Lucke-Wold, B. Racial underrepresentation in dermatological datasets leads to biased machine learning models and inequitable healthcare. J. Biomed Res. 2022, 3, 42–47. [Google Scholar]
- Gebru, T. Race and gender. In The Oxford Handbook of Ethics of AI; Oxfornd University Press: Oxford, UK, 2020; pp. 251–269. [Google Scholar]
- Buolamwini, J.; Gebru, T. Gender shades: Intersectional accuracy disparities in commercial gender classification. In Proceedings of the Conference on Fairness, Accountability and Transparency PMLR, New York, NY, USA, 23–24 February 2018; pp. 77–91. [Google Scholar]
- Hoffmann, A.L. Where fairness fails: Data, algorithms, and the limits of antidiscrimination discourse. Inform. Commun. Soc. 2019, 22, 900–915. [Google Scholar] [CrossRef]
- John-Mathews, J.M.; Cardon, D.; Balagué, C. From reality to world. A critical perspective on AI fairness. J. Bus. Ethics 2022, 178, 945–959. [Google Scholar] [CrossRef]
- Jo, E.S.; Gebru, T. Lessons from archives: Strategies for collecting sociocultural data in machine learning. In Proceedings of the 2020 Conference on Fairness, Accountability, and Transparency, Barcelona, Spain, 27–30 July 2020; pp. 306–316. [Google Scholar]
- Manyika, J. Getting AI right: Introductory notes on AI & society. Daedalus 2022, 151, 5–27. [Google Scholar]
- Zhou, J.; Chen, F.; Holzinger, A. Towards explainability for AI fairness. In Proceedings of the xxAI-Beyond Explainable AI: International Workshop, Held in Conjunction with ICML 2020, Vienna, Austria, 18 July 2020; Revised and Extended Papers. Springer: Berlin, Germany, 2022; pp. 375–386. [Google Scholar]
- Gull, S.; Mansour, R.F.; Aljehane, N.O.; Parah, S.A. A self-embedding technique for tamper detection and localization of medical images for smart-health. Multimed. Tools Appl. 2021, 80, 29939–29964. [Google Scholar] [CrossRef]
- Levy, M.; Amit, G.; Elovici, Y.; Mirsky, Y. The security of deep learning defences for medical imaging. arXiv 2022, arXiv:2201.08661. [Google Scholar]
- Chui, M.; Evers, M.; Manyika, J.; Zheng, A.; Nisbet, T. The bio revolution: Innovations transforming economies, societies, and our lives. In Augmented Education in the Global Age; Routledge: Abingdon, UK, 2023; pp. 48–74. [Google Scholar]
- Albahri, A.; Duhaim, A.M.; Fadhel, M.A.; Alnoor, A.; Baqer, N.S.; Alzubaidi, L.; Albahri, O.; Alamoodi, A.; Bai, J.; Salhi, A.; et al. A systematic review of trustworthy and explainable artificial intelligence in healthcare: Assessment of quality, bias risk, and data fusion. Inf. Fusion 2023, 96, 156–191. [Google Scholar] [CrossRef]
- Arshad, S.; Arshad, J.; Khan, M.M.; Parkinson, S. Analysis of security and privacy challenges for DNA-genomics applications and databases. J. Biomed. Inform. 2021, 119, 103815. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Vaidya, T.; Gupta, A.; Rane, S.; Gupta, S. Artificial intelligence in healthcare in developing nations: The beginning of a transformative journey. Cancer Res. Stat. Treat. 2019, 2, 182–189. [Google Scholar] [CrossRef]
- Samori, I.A.; Palmer, X.L.; Potter, L.; Karahan, S. Commentary on Biological Assets Cataloging and AI in the Global South. In Proceedings of the Intelligent Systems and Applications: Proceedings of the 2022 Intelligent Systems Conference (IntelliSys), Amsterdam, The Netherlands, 1–2 September 2022; Springer: Berlin, Germany, 2022; Volume 3, pp. 734–744. [Google Scholar]
- Powell, E.; Akogo, D.; Potter, L.; Palmer, X.L. Co-leadership and Cross-pollination of University and DIY Bio Spaces: An Exploration in Consideration of Biocybersecurity. In Proceedings of the Future Technologies Conference (FTC), Vancouver, BC, Canada, 28–29 November 2021; Springer: Berlin, Germany, 2022; Volume 3, pp. 610–621. [Google Scholar]
- 247 Crypto. JPMorgan becomes First Bank to enter Metaverse Launching Virtual Lounge in Decentraland. 2022. Available online: https://24-7-crypto.com/jpmorgan-enter-metaverse-onyx-lounge-decentraland/ (accessed on 3 January 2023).
- Kumar, M.; Chand, S. MedHypChain: A patient-centered interoperability hyperledger-based medical healthcare system: Regulation in COVID-19 pandemic. J. Netw. Comput. Appl. 2021, 179, 102975. [Google Scholar] [CrossRef] [PubMed]
- Sneha, S.; Panjwani, A.; Lade, B.; Randolph, J.; Vickery, M. Alleviating challenges related to FDA-approved medical wearables using blockchain technology. IT Prof. 2021, 23, 21–27. [Google Scholar] [CrossRef]
- West, R.M.; Gronvall, G.K. CRISPR Cautions: Biosecurity implications of gene editing. Perspect. Biol. Med. 2020, 63, 73–92. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.; Ma, Y.; Ding, M.; Wang, C.; Du, G.; Zhou, Y.; Guo, L.; Kang, H.; Wang, C.; Gu, B. Preliminary exploration on the serum biomarkers of bloodstream infection with carbapenem-resistant Klebsiella pneumoniae based on mass spectrometry. J. Clin. Lab. Anal. 2021, 35, e23915. [Google Scholar] [CrossRef]
- Bush, J.; Hu, C.H.; Veneziano, R. Mechanical properties of DNA hydrogels: Towards highly programmable biomaterials. Appl. Sci. 2021, 11, 1885. [Google Scholar] [CrossRef]
- Al-Husainy, M.A.F.; Al-Shargabi, B.; Aljawarneh, S. Lightweight cryptography system for IoT devices using DNA. Comput. Electr. Eng. 2021, 95, 107418. [Google Scholar] [CrossRef]
- Dey, S.; Fan, C.; Gothelf, K.V.; Li, J.; Lin, C.; Liu, L.; Liu, N.; Nijenhuis, M.A.; Saccà, B.; Simmel, F.C.; et al. DNA origami. Nat. Rev. Methods Prim. 2021, 1, 13. [Google Scholar] [CrossRef]
- Liu, A.P.; Appel, E.A.; Ashby, P.D.; Baker, B.M.; Franco, E.; Gu, L.; Haynes, K.; Joshi, N.S.; Kloxin, A.M.; Kouwer, P.H.; et al. The living interface between synthetic biology and biomaterial design. Nat. Mater. 2022, 21, 390–397. [Google Scholar] [CrossRef]
- Li, Y.C.; Zhang, Y.S.; Akpek, A.; Shin, S.R.; Khademhosseini, A. 4D bioprinting: The next-generation technology for biofabrication enabled by stimuli-responsive materials. Biofabrication 2016, 9, 012001. [Google Scholar] [CrossRef] [PubMed]
- Bilooei, S.F.; Jovicevic, D.; Iranzadeh, A.; Thomas, A.; Muscat, I.; Mpofu, C.; Steiner, H.; Meany, T. Rapid genome surveillance of SARS-CoV-2 and study of risk factors using shipping container laboratories and portable DNA sequencing technology. medRxiv 2022. medRxiv:2022-02. [Google Scholar]
- Rahman, A.; Hossain, M.S.; Alrajeh, N.A.; Alsolami, F. Adversarial examples—Security threats to COVID-19 deep learning systems in medical IoT devices. IEEE Internet Things J. 2020, 8, 9603–9610. [Google Scholar] [CrossRef] [PubMed]
- Girgis, S.T.; Adika, E.; Nenyewodey, F.E.; Senoo Jnr, D.K.; Ngoi, J.M.; Bandoh, K.; Lorenz, O.; van de Steeg, G.; Nsoh, S.; Judge, K.; et al. Nanopore sequencing for real-time genomic surveillance of Plasmodium falciparum. bioRxiv, 2022; bioRxiv:2022-12. [Google Scholar]
- Gault, M. The Plan to Put Bitcoin in Mouse DNA with a Genetically Engineered Virus. 2022. Available online: https://www.vice.com/en/article/5dg5az/the-quest-to-put-bitcoin-in-mouse-dna-with-a-genetically-engineered-virus (accessed on 3 January 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Affia, A.-a.O.; Finch, H.; Jung, W.; Samori, I.A.; Potter, L.; Palmer, X.-L. IoT Health Devices: Exploring Security Risks in the Connected Landscape. IoT 2023, 4, 150-182. https://doi.org/10.3390/iot4020009
Affia A-aO, Finch H, Jung W, Samori IA, Potter L, Palmer X-L. IoT Health Devices: Exploring Security Risks in the Connected Landscape. IoT. 2023; 4(2):150-182. https://doi.org/10.3390/iot4020009
Chicago/Turabian StyleAffia, Abasi-amefon Obot, Hilary Finch, Woosub Jung, Issah Abubakari Samori, Lucas Potter, and Xavier-Lewis Palmer. 2023. "IoT Health Devices: Exploring Security Risks in the Connected Landscape" IoT 4, no. 2: 150-182. https://doi.org/10.3390/iot4020009
APA StyleAffia, A.-a. O., Finch, H., Jung, W., Samori, I. A., Potter, L., & Palmer, X.-L. (2023). IoT Health Devices: Exploring Security Risks in the Connected Landscape. IoT, 4(2), 150-182. https://doi.org/10.3390/iot4020009






