A Multi-State Model for Lung Cancer Mortality in Survival Progression
Abstract
1. Introduction
2. Materials and Methods
2.1. Lung Cancer
2.1.1. Basic Survival Analysis Concepts
2.1.2. Survival Analysis
- The Kaplan–Meier estimator, which estimates the probability of survival over time while accounting for censored data.
- The Nelson–Aalen estimator, which estimates the cumulative hazard function over time, providing an alternative to the Kaplan–Meier for hazard-based interpretation.
- The Cox proportional hazards model, which examines how different factors affect the risk, assuming the ratio of risks stays the same between individuals is constant over time.
- Parametric models, which assume the time-to-event follows a specific distribution (e.g., exponential, Weibull, gamma, log-normal).
2.1.3. Survival and Hazard Functions
2.1.4. Explanatory Variables
2.1.5. Multi-State Markov Models and the Markov Property
- It simplifies the mathematical modeling but may not fully capture the complexity of disease progression
- It assumes that the time spent in the current state does not affect transition probabilities (memoryless property)
- In reality, the duration of illness or time since diagnosis often influences future progression
- Patient history and previous treatments may impact future transitions in ways not captured by the Markov property
- Semi-Markov models or hidden Markov models may be more appropriate when the Markov assumption is violated
2.1.6. Dataset Description
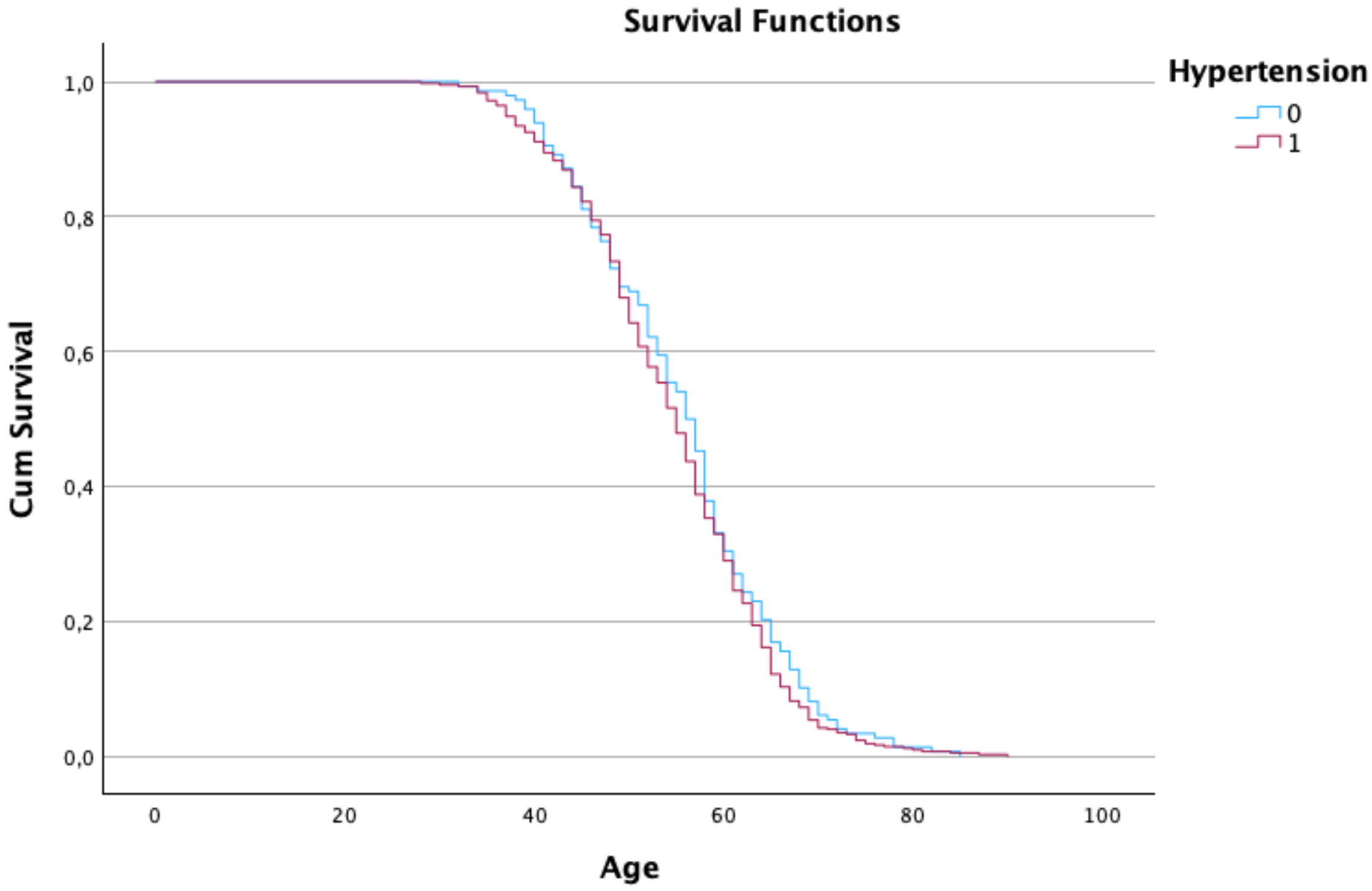
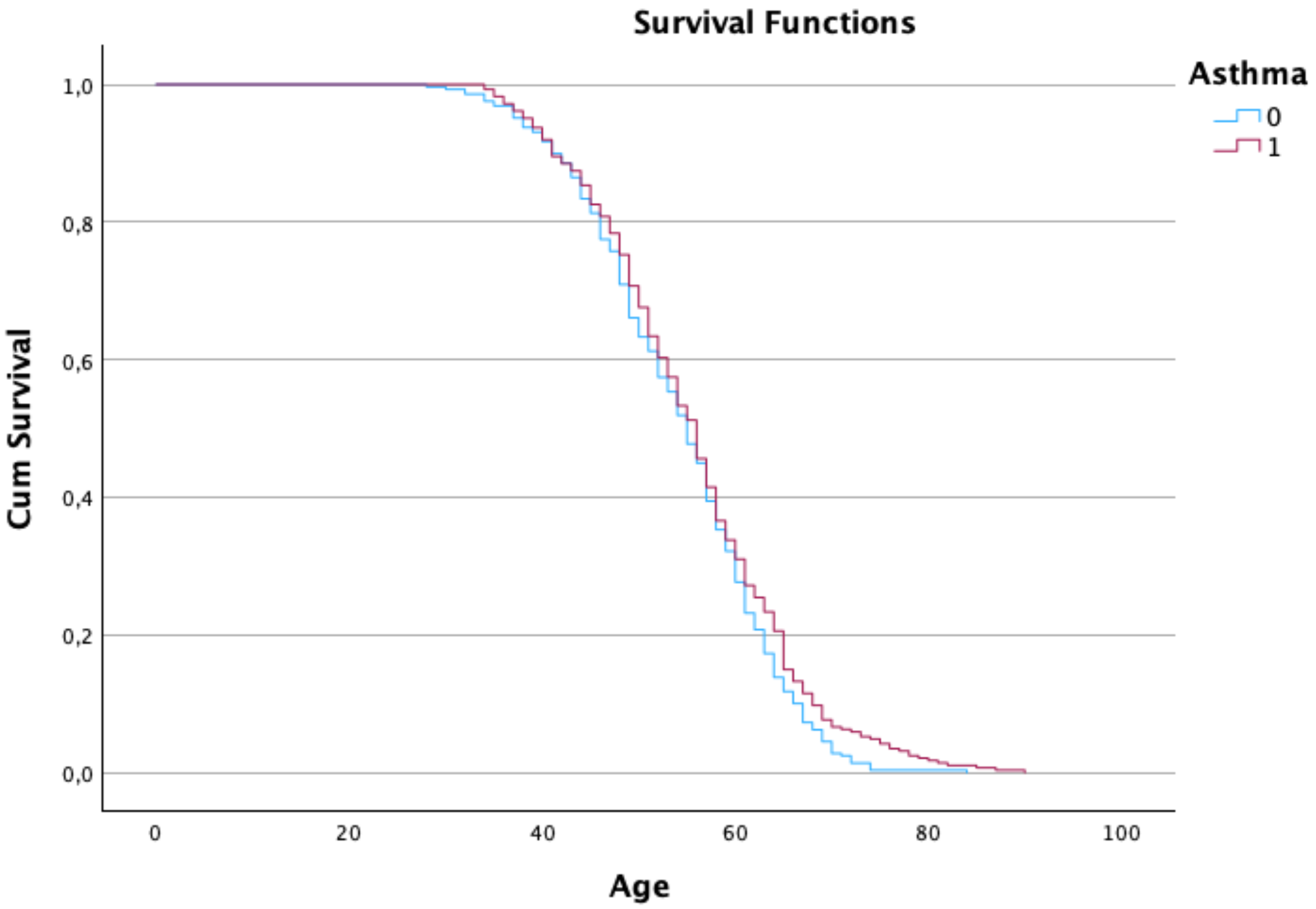
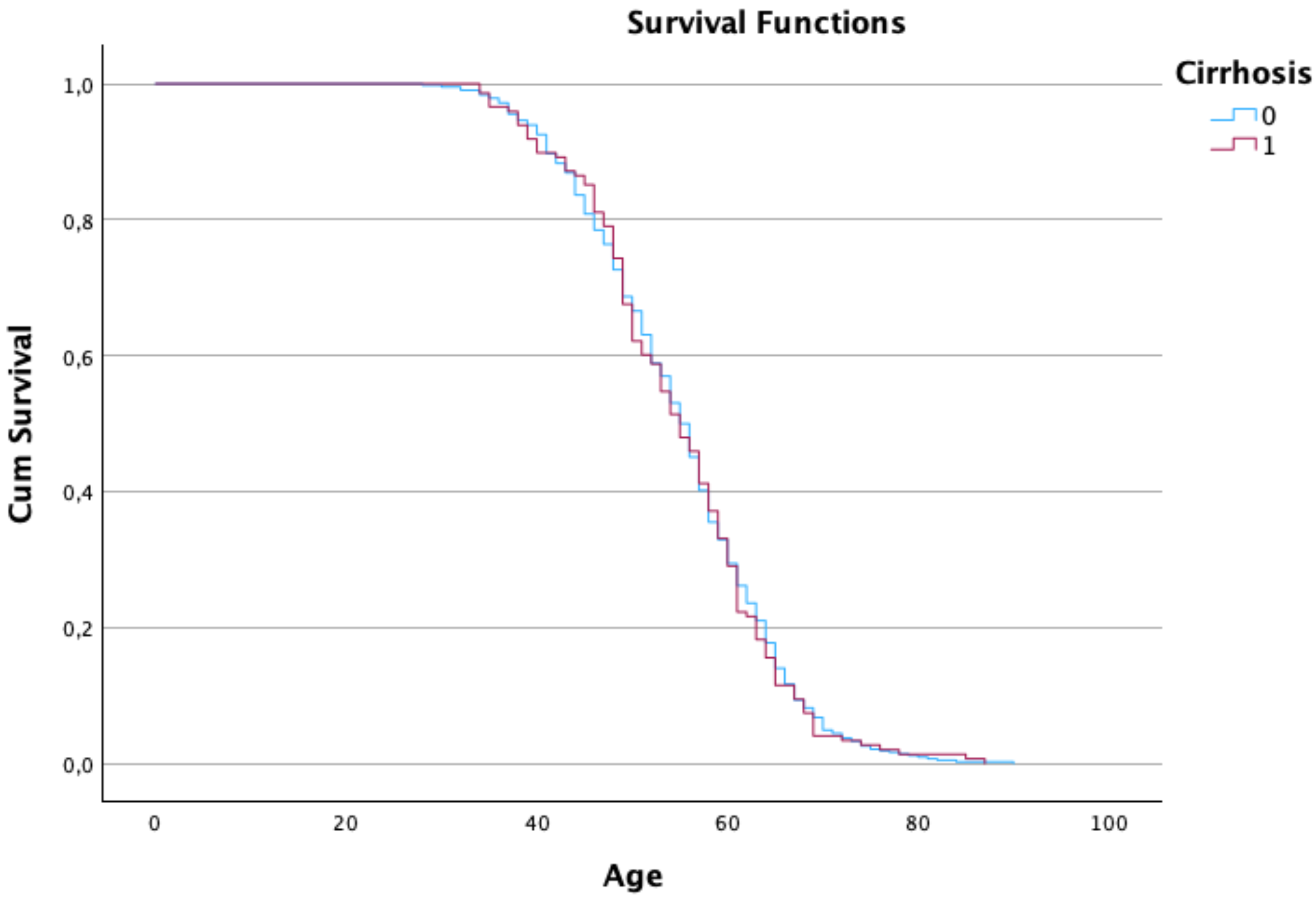
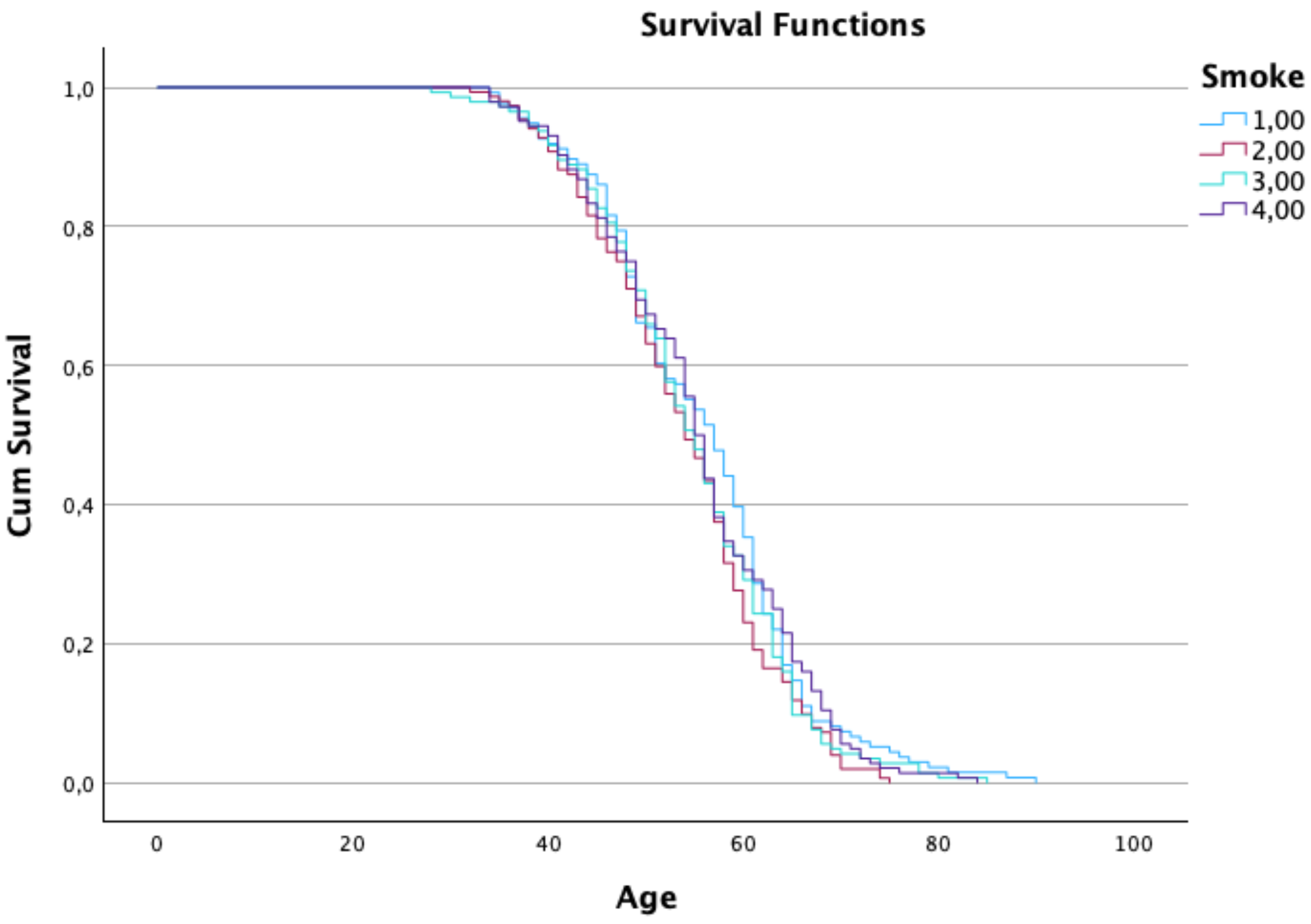
- Medical History: This section includes information about each patient’s medical background, such as smoking status (26.4% current smokers, 23.6% former smokers, 25.0% never smoked, and 25.0% passive smokers), Body Mass Index (mean = 30.26, SD = 8.40), and the presence of other health conditions such as hypertension (74.3%), asthma (49.8%), cirrhosis (25.7%), and other cancers (11.1%). It is crucial to identify potential risk factors and comorbidities.
- Cancer Diagnosis: Detailed data about the cancer diagnosis itself, including the stage of cancer at the time of diagnosis (Stage I: 25.9%, Stage II: 25.9%, Stage III: 25.2%, Stage IV: 23.1%). These variables are critical for tracking the progression and severity of the disease.
- Treatment Details: Information about the type of treatment each patient received (Chemotherapy: 25.9%, Radiation: 26.2%, Surgery: 25.9%, Combined: 22.0%), along with end date of the treatment, and the outcome (21.0% survived, 79.0% did not survive).
2.1.7. Missing Data and Censoring
2.1.8. Ethical Considerations
2.2. Statistical Analysis
2.3. Multi-State Model
Variance of Time to Absorption
2.4. Likelihood Function
3. Results
- According to Figure 1, survival probability decreased with increasing age. Patients over 80 years exhibited a pronounced decline in survival, and female patients maintained higher survival probabilities after age 80 compared to males.
Mean Waiting Time Analysis
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gao, S.; Zhang, G.; Lian, Y.; Li, Y.; Gao, H. Exploration and analysis of the value of tumor-marker joint detection in the pathological type of lung cancer. Cell. Mol. Biol. 2020, 99, 93–97. [Google Scholar] [CrossRef]
- World Health Organization. Cancer. Fact Sheets. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 21 September 2024).
- World Cancer Research Fund International. Lung Cancer Statistics. Available online: https://www.wcrf.org/cancertrends/lung-cancer-statistics/ (accessed on 21 September 2024).
- Gottlin, E.B.; Bentley, R.C.; Campa, M.J.; Pisetsky, D.S.; Herndon, J.E.; Patz, E.F. The association of intratumoral germinal centers with early-stage non-small cell lung cancer. J. Thorac. Oncol. 2011, 6, 1687–1690. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Caini, S.; Del Riccio, M.; Vettori, V.; Scotti, V.; Martinoli, C.; Raimondi, S.; Cammarata, G.; Palli, D.; Banini, M.; Masala, G.; et al. Quitting smoking at or around diagnosis improves lung cancer survival: A systematic review and meta-analysis. J. Thorac. Oncol. 2022, 17, 623–636. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Romero-Gutierrez, C.W.; Kothari, J.; Shafer, A.; Li, Y.; Christiani, D.C. Prediagnosis smoking cessation and overall survival among patients with non–small cell lung cancer. JAMA Netw. Open 2023, 6, e2311966. [Google Scholar] [CrossRef] [PubMed]
- Parkin, D.M.; Bray, F.I.; Devesa, S. Cancer burden in the year 2000: The global picture. Eur. J. Cancer 2001, 37, 4–66. [Google Scholar] [CrossRef] [PubMed]
- Peto, R.; Darby, S.; Deo, H.; Silcocks, P.; Whitley, E.; Doll, R. Smoking, smoking cessation, and lung cancer in the UK since 1950: Combination of national statistics with two case-control studies. BMJ 2000, 321, 323. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Utrero, A.; San-Román-Montero, J.M.; Gil-Prieto, R.; Gil-de-Miguel, A. Trends in hospitalization and in-hospital mortality rates among patients with lung cancer in Spain between 2010 and 2020. BMC Cancer 2022, 22, 1199. [Google Scholar] [CrossRef] [PubMed]
- Zarbakhsh, P. Spatial attention in U-Net for breast tumor segmentation. Appl. Sci. 2023, 13, 8758. [Google Scholar] [CrossRef]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC lung cancer staging project: Proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Greene, C.M.; Abdulkadir, M. Global respiratory health priorities at the beginning of the 21st century. Eur. Respir. Rev. 2024, 33, 230205. [Google Scholar] [CrossRef] [PubMed]
- Lam, D.C.; Liam, C.K.; Andarini, S.; Park, S.; Tan, D.S.; Singh, N.; Jang, S.H.; Vardhanabhuti, V.; Ramos, A.B.; Nakayama, T.; et al. Lung cancer screening in Asia: An expert consensus report. J. Thorac. Oncol. 2023, 18, 1303–1322. [Google Scholar] [CrossRef] [PubMed]
- Shankar, A.; Dubey, A.; Saini, D.; Singh, M.; Prasad, C.P.; Roy, S.; Bharati, S.J.; Rinki, M.; Singh, N.; Seth, T.; et al. Environmental determinants of lung cancer. Transl. Lung Cancer Res. 2019, 8, S31–S49. [Google Scholar] [CrossRef] [PubMed]
- Grover, G.; Sabharwal, A.; Kumar, S.; Thakura, A.K. A multi-state Markov model for the progression of chronic kidney disease. Turkiye Klinikleri J. Biostat. 2019, 11, 1–14. [Google Scholar] [CrossRef]
- Lintu, M.K.; Shreyas, K.M.; Kamath, A. Multi-state model for kidney disease. Clin. Epidemiol. Glob. Health 2022, 13, 100946. [Google Scholar] [CrossRef]
- Jeong, W.G.; Choi, H.; Chae, K.J.; Kim, J. Recurrence in early-stage lung cancer: A multistate model. Transl. Lung Cancer Res. 2022, 11, 1279–1291. [Google Scholar] [CrossRef] [PubMed]
- Tesfaw, L.M.; Dessie, Z.G.; Mekonnen Fenta, H. Lung cancer mortality and associated predictors: Systematic review using 32 scientific research findings. Front. Oncol. 2023, 13, 1308897. [Google Scholar] [CrossRef] [PubMed]

| Stage | TNM Stage | State |
|---|---|---|
| 1 | T1, N0, M0 | Localized |
| 2 | T2, N0/N1, M0 | Early |
| 3 | T3, N1/N2, M0 | Locally Advanced |
| 4 | T4, Any N, M0 | Advanced |
| 5 | Any T, Any N, M1 | Severe |
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Age group | ||
| <30 years | 2 | 0.3 |
| 31–40 years | 45 | 7.8 |
| 41–50 years | 152 | 26.4 |
| 51–60 years | 187 | 32.5 |
| >60 years | 190 | 33.0 |
| Gender | ||
| Male | 298 | 51.7 |
| Female | 278 | 48.3 |
| Smoking status | ||
| Current smoker | 152 | 26.4 |
| Former smoker | 136 | 23.6 |
| Never smoked | 144 | 25.0 |
| Passive smoker | 144 | 25.0 |
| Hypertension | ||
| Yes | 428 | 74.3 |
| No | 148 | 25.7 |
| Asthma | ||
| Yes | 287 | 49.8 |
| No | 289 | 50.2 |
| Cirrhosis | ||
| Yes | 148 | 25.7 |
| No | 428 | 74.3 |
| Variable | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Age (years) | 54.9 | 10.1 | 28.0 | 90.0 |
| BMI (kg/m2) | 30.3 | 8.4 | 16.0 | 45.0 |
| Cholesterol (mg/dL) | 231.6 | 44.4 | 150.0 | 300.0 |
| Percentile | Age | BMI | Cholesterol |
|---|---|---|---|
| 25th percentile | 48.0 | 23.3 | 191.0 |
| 50th percentile (Median) | 55.0 | 29.8 | 238.5 |
| 75th percentile | 62.0 | 37.8 | 272.0 |
| State | Mean Time (Years) | Standard Error | 95% CI (Lower–Upper) |
|---|---|---|---|
| State 1 | 5.8 | 1.0 | (4.1–8.0) |
| State 2 | 1.0 | 0.4 | (0.7–1.8) |
| State 3 | 4.9 | 0.8 | (2.9–6.9) |
| State 4 | 1.5 | 0.7 | (0.6–3.6) |
| State 5 | 3.6 | 0.7 | (1.9–6.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raman, V.; Ferreira, S.S.; Ferreira, D.; Alzaatreh, A. A Multi-State Model for Lung Cancer Mortality in Survival Progression. Stats 2025, 8, 106. https://doi.org/10.3390/stats8040106
Raman V, Ferreira SS, Ferreira D, Alzaatreh A. A Multi-State Model for Lung Cancer Mortality in Survival Progression. Stats. 2025; 8(4):106. https://doi.org/10.3390/stats8040106
Chicago/Turabian StyleRaman, Vinoth, Sandra S. Ferreira, Dário Ferreira, and Ayman Alzaatreh. 2025. "A Multi-State Model for Lung Cancer Mortality in Survival Progression" Stats 8, no. 4: 106. https://doi.org/10.3390/stats8040106
APA StyleRaman, V., Ferreira, S. S., Ferreira, D., & Alzaatreh, A. (2025). A Multi-State Model for Lung Cancer Mortality in Survival Progression. Stats, 8(4), 106. https://doi.org/10.3390/stats8040106









