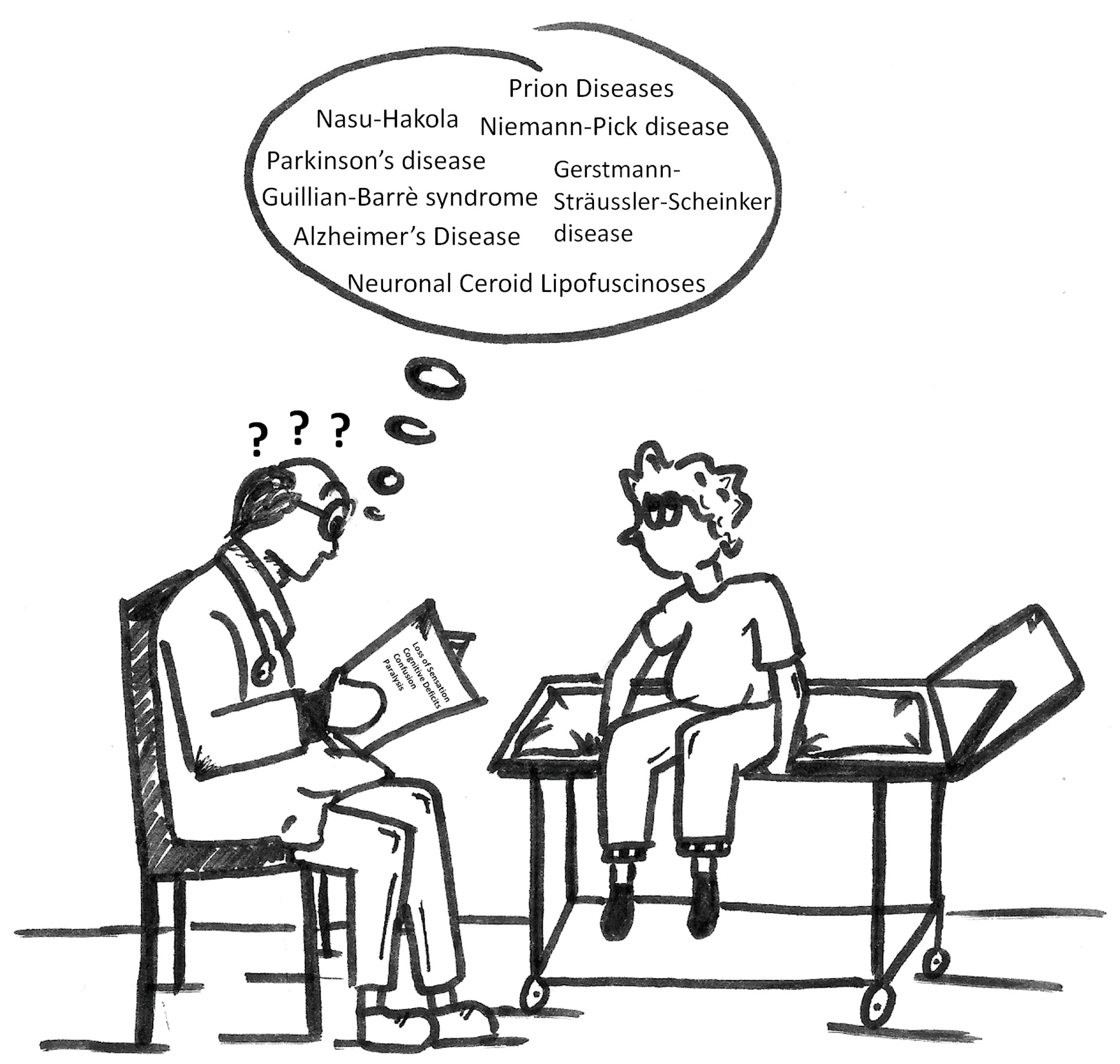
Could Proteomics Become a Future Useful Tool to Shed Light on the Mechanisms of Rare Neurodegenerative Disorders?
Abstract
:1. Introduction
2. Outline of the Article
3. Prion Disease
4. Nasu-Hakola Disease
5. Guillain-Barrè Syndrome
6. Niemann-Pick Disease
7. Neuronal Ceroid Lipofuscinoses
8. Pros and cons of Techniques Mentioned in this Report
9. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ross, C.A.; Poirier, M.A. Protein aggregation and neurodegenerative disease. Nat. Med. 2004, 10, S10–S17. [Google Scholar] [CrossRef] [PubMed]
- Agresta, A.M.; De Palma, A.; Bardoni, A.; Salvini, R.; Iadarola, P.; Mauri, P.L. Proteomics as an innovative tool to investigate frontotemporal disorders. Proteom. Clin. Appl. 2016, 10, 457–469. [Google Scholar] [CrossRef] [PubMed]
- Regan, L.; Preston, N.J.; Eccles, F.J.R.; Simpson, J. The views of adults with neurodegenerative diseases on end-of-life care: A metasynthesis. Aging Ment. Health 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, B.; Walgaard, C.; Drenthen, J.; Fokke, C.; Jacobs, B.C.; van Doorn, P.A. Guillain-Barré syndrome: Pathogenesis, diagnosis, treatment and prognosis. Nat. Rev. Neurol. 2014, 10, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Hendriksz, C.J.; Anheim, M.; Bauer, P.; Bonnot, O.; Chakrapani, A.; Corvol, J.C.; de Koning, T.J.; Degtyareva, A.; Dionisi-Vici, C.; Doss, S.; et al. The hidden Niemann-Pick type C patient: Clinical niches for a rare inherited metabolic disease. Curr. Med. Res. Opin. 2017, 33, 877–890. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.R.; Hendriksz, C.J. Niemann-Pick type C disease-the tip of the iceberg? A review of neuropsychiatric presentation, diagnosis and treatment. BJPsych Bull. 2017, 41, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Roos, A.; Thompson, R.; Horvath, R.; Lochmüller, H.; Sickmann, A. Intersection of Proteomics and Genomics to “Solve the Unsolved” in Rare Disorders such as Neurodegenerative and Neuromuscular Diseases. Proteom. Clin. Appl. 2017. [Google Scholar] [CrossRef] [PubMed]
- PubMed. Available online: https://www.ncbi.nlm.nih.gov/pubmed (accessed on 20 September 2017).
- Mays, C.E.; Soto, C. The stress of prion disease. Brain Res. 2016, 1648, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, M.; Dittmar, K.; Llorens, F.; Gelpi, E.; Ferrer, I.; Schulz-Schaeffer, W.J.; Zerr, I. Hereditary human prion diseases: An update. Mol. Neurobiol. 2017, 54, 4138–4149. [Google Scholar] [CrossRef] [PubMed]
- Righetti, P.G.; Castagna, A.; Antonucci, F.; Piubelli, C.; Cecconi, D.; Campostrini, N.; Rustichelli, C.; Antonioli, P.; Zanusso, G.; Monaco, S.; et al. Proteome analysis in the clinical chemistry laboratory: Myth or reality? Clin. Chim. Acta 2005, 357, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.N.; Shi, Q.; Zhang, B.Y.; Zhang, X.M.; Wang, J.; Xiao, K.; Lv, Y.; Sun, J.; Yang, X.D.; Chen, C.; et al. Proteomic analyses for the global S-nitrosylated proteins in the brain tissues of different human prion diseases. Mol. Neurobiol. 2016, 53, 5079–5096. [Google Scholar] [CrossRef] [PubMed]
- Romeo, M.J.; Espina, V.; Lowenthal, M.; Espina, B.H.; Petricoin, E.F., 3rd; Liotta, L.A. CSF proteome: A protein repository for potential biomarker identification. Expert Rev. Proteom. 2005, 2, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Sheikh, I.A.; Mirza, Z.; Gan, S.H.; Kamal, M.A.; Abuzenadah, A.M.; Damanhouri, G.A.; Ashraf, G.M. Application of proteomic tools in modern nanotechnological approaches towards effective management of neurodegenerative disorders. Curr. Drug Metab. 2015, 16, 376–388. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Chen, L.N.; Zhang, B.Y.; Xiao, K.; Zhou, W.; Chen, C.; Zhang, X.M.; Tian, C.; Gao, C.; Wang, J.; et al. Proteomics analyses for the global proteins in the brain tissues of different human prion diseases. Mol. Cell. Proteom. 2015, 14, 854–869. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhao, D.; Shah, S.Z.A.; Yang, W.; Li, C.; Yang, L. Proteome analysis of potential synaptic vesicle cycle biomarkers in the cerebrospinal fluid of patients with sporadic Creutzfeldt-Jakob disease. Mol. Neurobiol. 2017, 54, 5177–5191. [Google Scholar] [CrossRef]
- Tahir, W.; Zafar, S.; Llorens, F.; Arora, A.S.; Thüne, K.; Schmitz, M.; Gotzmann, N.; Kruse, N.; Mollenhauer, B.; Torres, J.M.; et al. Molecular alterations in the cerebellum of sporadic Creutzfeldt-Jakob disease subtypes with DJ-1 as a key regulator of oxidative stress. Mol. Neurobiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Madry, H.; Prudlo, J.; Grgic, A.; Freyschmidt, J. Nasu-Hakola disease (PLOSL): Report of five cases and review of the literature. Clin. Orthop. Relat. Res. 2007, 454, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Montalbetti, L.; Soragna, D.; Ratti, M.T.; Bini, P.; Buscone, S.; Moglia, A. Nasu-Hakola disease: A rare entity in Italy. Critical review of the literature. Funct. Neurol. 2004, 19, 171–179. [Google Scholar] [PubMed]
- Paloneva, J.; Manninen, T.; Christman, G.; Hovanes, K.; Mandelin, J.; Adolfsson, R.; Bianchin, M.; Bird, T.; Miranda, R.; Salmaggi, A.; et al. Mutations in two genes encoding different subunits of a receptor signaling complex result in an identical disease phenotype. Am. J. Hum. Genet. 2002, 71, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Hakola, H.P.A.; Jarvi, O.H.; Sourander, P. Osteodysplasia polycystica hereditaria combined with sclerosing leucoencephalopathy. Acta Neurol. Scand. Suppl. 1970, 43, 79–80. [Google Scholar] [CrossRef]
- Verloes, A.; Maquet, P.; Sadzot, B.; Vivario, M.; Thiry, A.; Franck, G. Nasu-Hakola syndrome: Polycystic lipomembranous osteodysplasia with sclerosing leucoencephalopathy and presenile dementia. J. Med. Genet. 1997, 34, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Bianchin, M.M.; Capella, H.M.; Chaves, D.L.; Steindel, M.; Grisard, E.C.; Ganev, G.G.; da Silva Júnior, J.P.; Neto Evaldo, S.; Poffo, M.A.; Walz, R.; et al. Nasu-Hakola disease (polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy-PLOSL): A dementia associated with bone cystic lesions. From clinical to genetic and molecular aspects. Cell. Mol. Neurobiol. 2004, 24, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Nakano-Yokomizo, T.; Tahara-Hanaoka, S.; Nakahashi-Oda, C.; Nabekura, T.; Tchao, N.K.; Kadosaki, M.; Totsuka, N.; Kurita, N.; Nakamagoe, K.; Tamaoka, A.; et al. The immunoreceptor adapter protein DAP12 suppresses B lymphocyte-driven adaptive immune responses. J. Exp. Med. 2011, 208, 1661–1671. [Google Scholar] [CrossRef] [PubMed]
- Satoh, J.I.; Kino, Y.; Yanaizu, M.; Tosaki, Y.; Sakai, K.; Ishidam, T.; Saito, Y. Expression of GPR17, a regulator of oligodendrocyte differentiation and maturation, in Nasu-Hakola disease brains. Intractable Rare Dis. Res. 2017, 6, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, S.; Agresta, A.M.; De Palma, A.; Viglio, S.; Mauri, P.; Fumagalli, M.; Iadarola, P.; Montalbetti, L.; Salvini, R.; Bardoni, A. Proteomic analysis of lymphoblastoid cells from Nasu-Hakola patients: A step forward in our understanding of this neurodegenerative disorder. PLoS ONE 2014, 9, e110073. [Google Scholar] [CrossRef] [PubMed]
- Hughes, R.A.; Rees, J.H. Clinical and epidemiological features of Guillain–Barré syndrome. J. Infect. Dis. 1997, 176, S92–S98. [Google Scholar] [CrossRef] [PubMed]
- Griffin, J.W.; Li, C.Y.; Ho, T.W.; Tian, M.; Gao, C.Y.; Xue, P.; Mishu, B.; Cornblath, D.R.; Macko, C.; McKhann, G.M.; et al. Pathology of the motor-sensory axonal Guillain-Barré syndrome. Ann. Neurol. 1996, 39, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Ropper, A.H. The Guillain-Barré syndrome. N. Engl. J. Med. 1992, 326, 1130–1136. [Google Scholar] [PubMed]
- Rosinska, J.; Lukasik, M.; Kozubski, W. Neuropathies in the course of primary hepatotropic virus infections. Neurol. Neurochir. Pol. 2012, 46, 263–270. [Google Scholar] [PubMed]
- Estanislao, L.B.; Morgello, S.; Simpson, D.M. Peripheral neuropathies associated with HIV and hepatitis C coinfection: A review. AIDS 2005, 19, S135–S139. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, S. Guillain-Barré syndrome: Epidemiology, pathophysiology and management. Drugs 2004, 64, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Ang, C.W.; Jacobs, B.C.; Laman, J.D. The Guillain–Barré syndrome: A true case of molecular mimicry. Trends Immunol. 2004, 25, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Lehmensiek, V.; Süssmuth, S.D.; Brettschneider, J.; Tauscher, G.; Felk, S.; Gillardon, F.; Tumani, H. Proteome analysis of cerebrospinal fluid in Guillain-Barré syndrome (GBS). J. Neuroimmunol. 2007, 185, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Jin, T.; Hu, L.S.; Chang, M.; Wu, J.; Winblad, B.; Zhu, J. Proteomic identification of potential protein markers in cerebrospinal fluid of GBS patients. Eur. J. Neurol. 2007, 14, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.H.; Lyu, R.K.; Tseng, M.Y.; Ro, L.S.; Wu, Y.R.; Chang, H.S.; Hsu, W.C.; Kuo, H.C.; Huang, C.C.; Chu, C.C.; et al. Elevated haptoglobin level of cerebrospinal fluid in Guillain-Barré syndrome revealed by proteomics analysis. Proteom. Clin. Appl. 2007, 1, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Fiorini, M.; Zanusso, G.; Benedetti, M.D.; Righetti, P.G.; Monaco, S. Cerebrospinal fluid biomarkers in clinically isolated syndromes and multiple sclerosis. Proteom. Clin. Appl. 2007, 1, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.R.; Liu, S.L.; Qin, Z.Y.; Liu, F.J.; Qin, Y.J.; Bai, S.M.; Chen, Z.Y. Comparative proteomics analysis of cerebrospinal fluid of patients with Guillain-Barré syndrome. Cell. Mol. Neurobiol. 2008, 28, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Sawai, S.; Satoh, M.; Mori, M.; Misawa, S.; Sogawa, K.; Kazami, T.; Ishibashi, M.; Beppu, M.; Shibuya, K.; Ishige, T.; et al. Moesin is a possible target molecule for cytomegalovirus-related Guillain-Barré syndrome. Neurology 2014, 83, 113–117. [Google Scholar] [CrossRef] [PubMed]
- BLAST: Basic Local Alignment Search Tool. Available online: https://blast.ncbi.nlm.nih.gov/Blast.cgi (accessed on 20 September 2017).
- Loshaj-Shala, A.; Regazzoni, L.; Daci, A.; Orioli, M.; Brezovska, K.; Panovska, A.P.; Beretta, G.; Suturkova, L. Guillain Barré syndrome (GBS): New insights in the molecular mimicry between C. jejuni and human peripheral nerve (HPN) proteins. J. Neuroimmunol. 2015, 289, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Gundelfinger, E.D.; Reissner, C.; Garner, C.C. Role of Bassoon and Piccolo in assembly and molecular organization of the active zone. Front. Synaptic Neurosci. 2016, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Mateos-Hernández, L.; Villar, M.; Doncel-Pérez, E.; Trevisan-Herraz, M.; García-Forcada, Á.; Ganuza, F.R.; Vázquez, J.; de la Fuente, J. Quantitative proteomics reveals Piccolo as a candidate serological correlate of recovery from Guillain-Barré syndrome. Oncotarget 2016, 7, 74582–74591. [Google Scholar] [CrossRef] [PubMed]
- STRING: Functional Protein Association Networks. Available online: https://string-db.org (accessed on 20 September 2017).
- Blast2GO—Functional Annotation and Genomics. Available online: https://www.blast2go.com (accessed on 20 September 2017).
- Ziganshin, R.H.; Ivanova, O.M.; Lomakin, Y.A.; Belogurov, A.A., Jr.; Kovalchuk, S.I.; Azarkin, I.V.; Arapidi, G.P.; Anikanov, N.A.; Shender, V.O.; Piradov, M.A.; et al. The pathogenesis of the demyelinating form of Guillain-Barre Syndrome (GBS): Proteo-peptidomic and immunological profiling of physiological fluids. Mol. Cell. Proteom. 2016, 15, 2366–2378. [Google Scholar] [CrossRef] [PubMed]
- D’Aguanno, S.; Franciotta, D.; Lupisella, S.; Barassi, A.; Pieragostino, D.; Lugaresi, A.; Centonze, D.; D’Eril, G.M.; Bernardini, S.; Federici, G.; et al. Protein profiling of Guillain-Barrè syndrome cerebrospinal fluid by two-dimensional electrophoresis and mass spectrometry. Neurosci. Lett. 2010, 485, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Schuchman, E.H.; Desnick, R.J. Types A and B Niemann-Pick disease. Mol. Genet. Metab. 2017, 120, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Cologna, S.M.; Jiang, X.S.; Backlund, P.S.; Cluzeau, C.V.; Dail, M.K.; Yanjanin, N.M.; Siebel, S.; Toth, C.L.; Jun, H.S.; Wassif, C.A.; et al. Quantitative proteomic analysis of Niemann-Pick disease, type C1 cerebellum identifies protein biomarkers and provides pathological insight. PLoS ONE 2012, 7, e47845. [Google Scholar] [CrossRef] [PubMed]
- Ory, D.S. The Niemann-Pick disease genes; regulators of cellular cholesterol homeostasis. Trends Cardiovasc. Med. 2004, 14, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Gelsthorpe, M.E.; Baumann, N.; Millard, E.; Gale, S.E.; Langmade, S.J.; Schaffer, J.E.; Ory, D.S. Niemann-Pick type C1 I1061T mutant encodes a functional protein that is selected for endoplasmic reticulum-associated degradation due to protein misfolding. J. Biol. Chem. 2008, 283, 8229–8236. [Google Scholar] [CrossRef] [PubMed]
- Rauniyar, N.; Subramanian, K.; Lavallée-Adam, M.; Martínez-Bartolomé, S.; Balch, W.E.; Yates, J.R., 3rd. Quantitative proteomics of human fibroblasts with i1061t mutation in Niemann-Pick C1 (NPC1) Protein provides insights into the disease pathogenesis. Mol. Cell. Proteom. 2015, 14, 1734–1749. [Google Scholar] [CrossRef] [PubMed]
- Bauer, S.; Grossmann, S.; Vingron, M.; Robinson, P.N. Ontologizer 2.0—A multifunctional tool for GO term enrichment analysis and data exploration. Bioinformatics 2008, 24, 1650–1651. [Google Scholar] [CrossRef] [PubMed]
- Macías-Vidal, J.; Guerrero-Hernández, M.; Estanyol, J.M.; Aguado, C.; Knecht, E.; Coll, M.J.; Bachs, O. Identification of lysosomal Npc1-binding proteins: Cathepsin D activity is regulated by NPC1. Proteomics 2016, 16, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Tharkeshwar, A.K.; Trekker, J.; Vermeire, W.; Pauwels, J.; Sannerud, R.; Priestman, D.A.; TeVruchte, D.; Vints, K.; Baatsen, P.; Decuypere, J.P.; et al. A novel approach to analyze lysosomal dysfunctions through subcellular proteomics and lipidomics: The case of NPC1 deficiency. Sci. Rep. 2017, 7, 41408. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Hao, J.; Fujiwara, H.; Xu, M.; Yang, S.; Dai, S.; Long, Y.; Swaroop, M.; Li, C.; Vu, M.; et al. Analytical characterization of methyl-β-cyclodextrin for pharmacological activity to reduce lysosomal cholesterol accumulation in Niemann-Pick disease type C1 cells. Assay Drug Dev. Technol. 2017, 15, 154–166. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, K.; Rauniyar, N.; Lavalleé-Adam, M.; Yates, J.R., 3rd; Balch, W.E. Quantitative analysis of the proteome response to the histone deacetylase inhibitor (HDACi) vorinostat in Niemann-Pick Type C1 disease. Mol. Cell. Proteom. 2017, 16, 1938–1957. [Google Scholar] [CrossRef] [PubMed]
- Schirmer, E.C.; Yates, J.R.; Gerace, L. MudPIT: A powerful proteomics tool for discovery. Discov. Med. 2003, 3, 38–39. [Google Scholar] [PubMed]
- Bennett, M.J.; Rakheja, D. The neuronal ceroid-lipofuscinoses. Dev. Disabil. Res. Rev. 2013, 17, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Mink, J.W.; Augustine, E.F.; Adams, H.R.; Marshall, F.J.; Kwon, J.M. Classification and natural history of the neuronal ceroid lipofuscinoses. J. Child Neurol. 2013, 28, 1101–1105. [Google Scholar] [CrossRef] [PubMed]
- Mole, S.E.; Cotman, S.L. Genetics of the neuronal ceroid lipofuscinoses (Batten disease). Biochim. Biophys. Acta 2015, 1852, 2237–2241. [Google Scholar] [CrossRef] [PubMed]
- Sleat, D.E.; Ding, L.; Wang, S.; Zhao, C.; Wang, Y.; Xin, W.; Zheng, H.; Moore, D.F.; Sims, K.B.; Lobel, P. Mass spectrometry-based protein profiling to determine the cause of lysosomal storage diseases of unknown etiology. Mol. Cell. Proteom. 2009, 8, 1708–1718. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Ju, W.; Wu, D.; Wang, L.; Yan, M.; Zou, J.; He, B.; Jenkins, E.C.; Brown, W.T.; Zhong, N. A two-dimensional protein fragmentation-proteomic study of neuronal ceroid lipofuscinoses: Identification and characterization of differentially expressed proteins. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2011, 879, 304–316. [Google Scholar] [CrossRef] [PubMed]
- DAVID Functional Annotation Bioinformatics Microarray Analysis. Available online: https://david.ncifcrf.gov (accessed on 20 September 2017).
- Haddad, S.E.; Khoury, M.; Daoud, M.; Kantar, R.; Harati, H.; Mousallem, T.; Alzate, O.; Meyer, B.; Boustany, R.M. CLN5 and CLN8 protein association with ceramide synthase: Biochemical and proteomic approaches. Electrophoresis 2012, 33, 3798–3809. [Google Scholar] [CrossRef] [PubMed]
- Scifo, E.; Szwajda, A.; Dębski, J.; Uusi-Rauva, K.; Kesti, T.; Dadlez, M.; Gingras, A.C.; Tyynelä, J.; Baumann, M.H.; Jalanko, A.; et al. Drafting the CLN3 protein interactome in SH-SY5Y human neuroblastoma cells: A label-free quantitative proteomics approach. J. Proteome Res. 2013, 12, 2101–2115. [Google Scholar] [CrossRef] [PubMed]
- Scifo, E.; Szwajda, A.; Soliymani, R.; Pezzini, F.; Bianchi, M.; Dapkunas, A.; Dębski, J.; Uusi-Rauva, K.; Dadlez, M.; Gingras, A.C.; et al. Proteomic analysis of the palmitoyl protein thioesterase 1 interactome in SH-SY5Y human neuroblastoma cells. J. Proteom. 2015, 123, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Scifo, E.; Szwajda, A.; Soliymani, R.; Pezzini, F.; Bianchi, M.; Dapkunas, A.; Dębski, J.; Uusi-Rauva, K.; Dadlez, M.; Gingras, A.C.; et al. Quantitative analysis of PPT1 interactome in human neuroblastoma cells. Data Brief 2015, 4, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Hersrud, S.L.; Geraets, R.D.; Weber, K.L.; Chan, C.H.; Pearce, D.A. Plasma biomarkers for neuronal ceroid lipofuscinosis. FEBS J. 2016, 283, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Henderson, M.X.; Wirak, G.S.; Zhang, Y.Q.; Dai, F.; Ginsberg, S.D.; Dolzhanskaya, N.; Staropoli, J.F.; Nijssen, P.C.; Lam, T.T.; Roth, A.F.; et al. Neuronal ceroid lipofuscinosis with DNAJC5/CSPα mutation has PPT1 pathologyand exhibit aberrant protein palmitoylation. Acta Neuropathol. 2016, 131, 621–637. [Google Scholar] [CrossRef] [PubMed]
| Type of Neurodegenerative Disease | Type of Samples Analyzed | Number of Proteins Identified | Proteomic Approach | Ref. |
|---|---|---|---|---|
| Prion disease | Cortex and cerebellum | 2287 | iTRAQ, LC-MS/MS | [15] |
| CSF | 1670 | iTRAQ, LC-MS/MS | [16] | |
| Cerebellum | 83 | 2-DE, MS | [17] | |
| Nasu-Hakola disease | Lymphoblastoid cells | 21 | 2-DE, nLC-MS/MS | [26] |
| Guillain-Barré syndrome | CSF | 12 | 2D-DIGE, MALDI-TOF MS | [34] |
| CSF | 47 | 2D-DIGE, MALDI-TOF MS | [35] | |
| CSF | 6 | 2-DE, MALDI-TOF MS | [36] | |
| CSF | 3 | 2-DE | [37] | |
| CSF | 10 | 2-DE, MALDI-TOF MS | [38] | |
| Schwannoma cell line YST-1 | 6 | 2-DE | [39] | |
| HPN tissue | 3 | 1-DE, nHPLC-nESI-HRMS | [41] | |
| Serum | 330 | iTRAQ, LC-MS/MS | [43] | |
| CSF | 854 | 1-DE, LC-MS/MS | [46] | |
| CSF | 17 | 2-DE, MALDI-TOF/TOF | [47] | |
| Niemann-Pick disease | CSF | 109 | 2-DE, MALDI-TOF/TOF, LC-ESI-MS/MS | [49] |
| NPC1I1061T fibroblasts | 4308 | TMT labelling, MudPIT | [52] | |
| NPC fibroblasts | 114 | 1-DE, LC-MS/MS | [54] | |
| NPC1 deficient cells | 7342 | 1-DE, LC-MS/MS | [55] | |
| Human fibroblasts | 19 | 1-DE, LC-MS/MS | [56] | |
| NPC1 I1061T fibroblasts | 2916 | TMT, MudPIT | [57] | |
| Neuronal ceroid lipofuscinoses | Human brains | 320 | 1-DE, LC-MS/MS | [62] |
| Human fibroblasts | 24 | PF2D, MALDI-TOF-MS, LC-ESI-MS/MS | [63] | |
| Human fibroblasts | 8 | 2-DE, MALDI-TOF/TOF | [65] | |
| Human neuroblastoma cells | 58 | TAP-MS | [66] | |
| Human neuroblastoma cells | 23 | TAP-MS | [67,68] | |
| Plasma | 27 | 2D-DIGE, LC-MS/MS | [69] | |
| Human brains | 17 | LC-MS/MS | [70] |
| Technique | Pros | Cons |
|---|---|---|
| 1-DE |
|
|
| 2-DE |
|
|
| 2D-DIGE |
|
|
| LC-MS |
|
|
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cagnone, M.; Bardoni, A.; Iadarola, P.; Viglio, S. Could Proteomics Become a Future Useful Tool to Shed Light on the Mechanisms of Rare Neurodegenerative Disorders? High-Throughput 2018, 7, 2. https://doi.org/10.3390/ht7010002
Cagnone M, Bardoni A, Iadarola P, Viglio S. Could Proteomics Become a Future Useful Tool to Shed Light on the Mechanisms of Rare Neurodegenerative Disorders? High-Throughput. 2018; 7(1):2. https://doi.org/10.3390/ht7010002
Chicago/Turabian StyleCagnone, Maddalena, Anna Bardoni, Paolo Iadarola, and Simona Viglio. 2018. "Could Proteomics Become a Future Useful Tool to Shed Light on the Mechanisms of Rare Neurodegenerative Disorders?" High-Throughput 7, no. 1: 2. https://doi.org/10.3390/ht7010002
APA StyleCagnone, M., Bardoni, A., Iadarola, P., & Viglio, S. (2018). Could Proteomics Become a Future Useful Tool to Shed Light on the Mechanisms of Rare Neurodegenerative Disorders? High-Throughput, 7(1), 2. https://doi.org/10.3390/ht7010002





