Abstract
Introduction: Brain abscess is defined as a suppurative collection resulting from hematogenous dissemination as an extension from otorhinolaryngologic infectious foci, or secondary to cranial trauma and neurosurgical procedures. Its evolution follows four histopathological stages, the most severe complication being intraventricular rupture, which is associated with extremely high mortality. Central nervous system infections caused by multidrug-resistant (MDR/XDR) Acinetobacter baumannii are rare but severe, significantly limiting therapeutic options due to the reduced penetration of the blood-brain barrier by active antimicrobial agents. Case report: We report the case of a 48-year-old patient with a history of hemorrhagic stroke treated surgically, who was admitted for fever, severe headache, and vomiting. On admission, lumbar puncture confirmed bacterial meningitis, with isolation of A. baumannii susceptible only to colistin. Brain magnetic resonance imaging revealed a postoperative cerebellar abscess. Initial empirical therapy consisted of meropenem and vancomycin, subsequently adjusted according to the susceptibility profile to cefiderocol, intravenous and intrathecal colistin, combined with ampicillin/sulbactam and minocycline. The clinical course was favorable with regard to meningitis, with partial regression of the cerebellar abscess. Follow-up lumbar punctures were sterile, and the patient’s neurological condition stabilized, allowing avoidance of neurosurgical drainage. Conclusions: Meningitis and brain abscess caused by MDR A. baumannii represent rare clinical entities with potentially severe outcomes. Intrathecal administration of colistin, in combination with systemic multidrug therapy, proved decisive in controlling the infection. An interdisciplinary approach and individualized antimicrobial regimens are essential to achieving a favorable prognosis in such complex cases.
Introduction
Brain abscess is defined as an intracranial suppurative collection resulting from hematogenous dissemination as an extension of an infectious focus (such as sinusitis, otitis, or mastoiditis), or secondary to cranial trauma and neurosurgical procedures. Brain abscess follows four histopathological stages: early cerebritis, late cerebritis, early capsule formation, and late capsule formation. The most severe complication is intraventricular rupture of the abscess, which transforms the condition into fulminant ventriculitis, associated with mortality rates of up to 80–85% in the absence of aggressive treatment [1].
Central nervous system (CNS) infections caused bymultidrug-resistant (MDR) Acinetobacter baumannii bacteria pose a major therapeutic challenge due to the pathogen’s extensive antimicrobial resistance profile and the limited penetration of most active antibiotics across the blood-brain barrier. In the context of neurosurgical procedures or cranial trauma, the risk of colonization and severe infections with A. baumannii increases significantly. The present article reports a rare case of postoperative meningitis complicated by brain abscess, with a favorable outcome under combined antimicrobial therapy, including intrathecal administration [2].
Case Report
A 48-year-old male patient presented to the Emergency Department of the Clinical Hospital of Infectious Diseases with fever, profuse sweating, vomiting, and sudden-onset severe headache, which began one day prior to admission.
The patient’s medical history is relevant for a hemorrhagic stroke in the left cerebellar hemisphere within the past three months. He underwent surgical evacuation of an intraparenchymal hematoma in the posterior cranial fossa, followed by a slowly favorable postoperative course. During his hospitalization in the Intensive Care Unit, the patient developed aspiration bronchopneumonia caused by Acinetobacter baumannii.
At the time of admission, the patient was afebrile but in a generally altered condition, conscious yet poorly cooperative, with a Glasgow Coma Scale score of 13, he exhibited neck stiffness and left-sided hemiparesis. Imaging studies and lumbar puncture supported the presumptive diagnosis of bacterial meningitis. Cerebrospinal fluid (CSF) analysis revealed 10713 leukocytes/mm3 (87.2% neutrophils), marked hypoglycorrhachia, and hyperproteinorrachia, consistent with bacterial meningitis. Microbiological examination of the CSF identified A. baumannii.
Empirical therapy was initiated with meropenem 2 g every 8 h and vancomycin 1 g every 12 h, in conjunction with corticosteroid therapy with dexamethasone, cerebral depletive measures, diuretics, and intravenous fluids for hydroelectrolytic rebalancing for 2 days, until the antibiotic susceptibility results were confirmed.
Once the presence of Acinetobacter baumannii complex in the CSF was confirmed, showing extensive drug resistance and susceptibility only to colistin and cefiderocol, antibiotic therapy was escalated to cefiderocol 2 g every 8 h in combination with colistin 5,000,000 IU every 12 h, corticosteroid therapy with dexamethasone and cerebral depletive for 14 days.
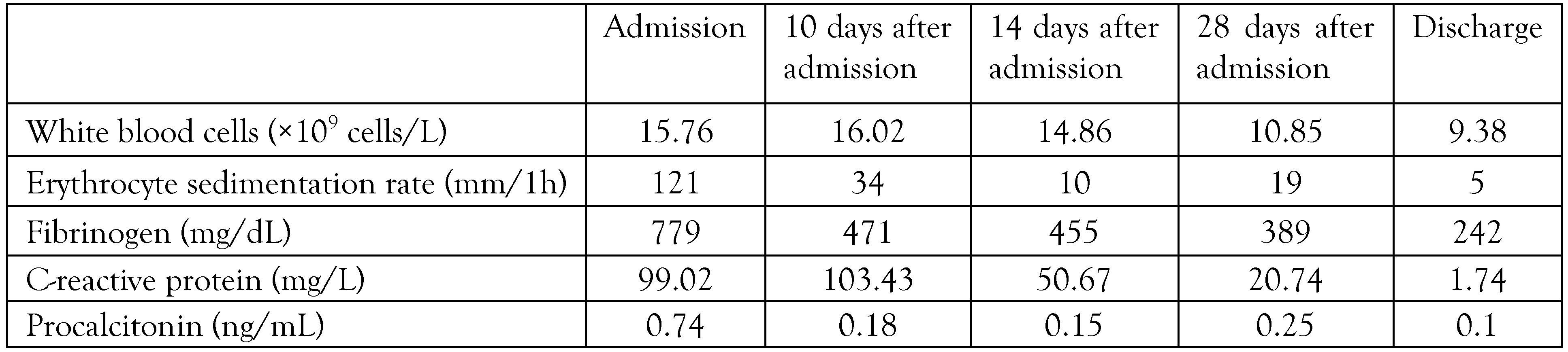
Dynamic follow-up included imaging studies and control lumbar punctures. Brain magnetic resonance imaging (MRI) at admission revealed findings consistent with occipital craniectomy, extensive postoperative occipital extracranial meningocele, a lesion in the left cerebellar hemisphere compatible with an abscess (25 × 10 mm), and chronic inflammatory changes of the bilateral maxillary sinuses (Figure 1).
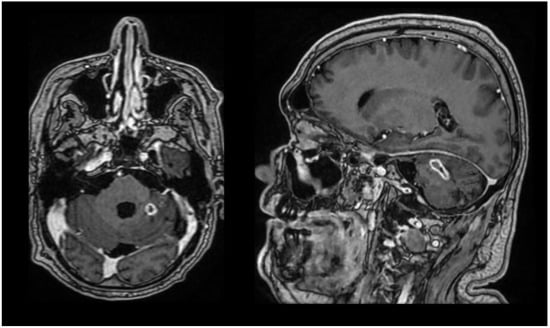
Figure 1.
Brain MRI at admission in axial and sagittal section.
Given the poor penetration of antibiotics across the blood-brain barrier and the complexity of the case, MDR bacterial meningitis with a probable brain abscess, the decision was made to insert an intrathecal catheter for colistin administration, in collaboration with the Neurosurgery Department. The catheter was placed in the operating room, and colistin was administered intrathecally at a dose of 300,000 IU/day, after first withdrawing an equal volume of CSF.
Due to the location of the lesion in a region requiring a high-risk neurosurgical approach, which could significantly impact the patient’s quality of life, conservative management of the cerebellar abscess was chosen. This included intravenous and intrathecal antibiotic therapy, cerebral depletive measures, and corticosteroid therapy, resulting in a slowly favorable course with progressive reduction of the abscess.
Following the 14-day course of intravenous and intrathecal cefiderocol and colistin, therapy was de-escalated to ampicillin/sulbactam 6 g every 8 h, colistin 5000000 IU every 12 h IV, and oral minocycline 200 mg every 12 h. This regimen was administered in combination with dexamethasone corticosteroid therapy, cerebral anti-depletive measures, loop diuretics, hepatoprotective and gastric protective agents, and intravenous fluids for hydroelectrolytic rebalancing for an additional 21 days. The dynamics of inflammatory markers and CSF examination are presented in Table 1 and Table 2.

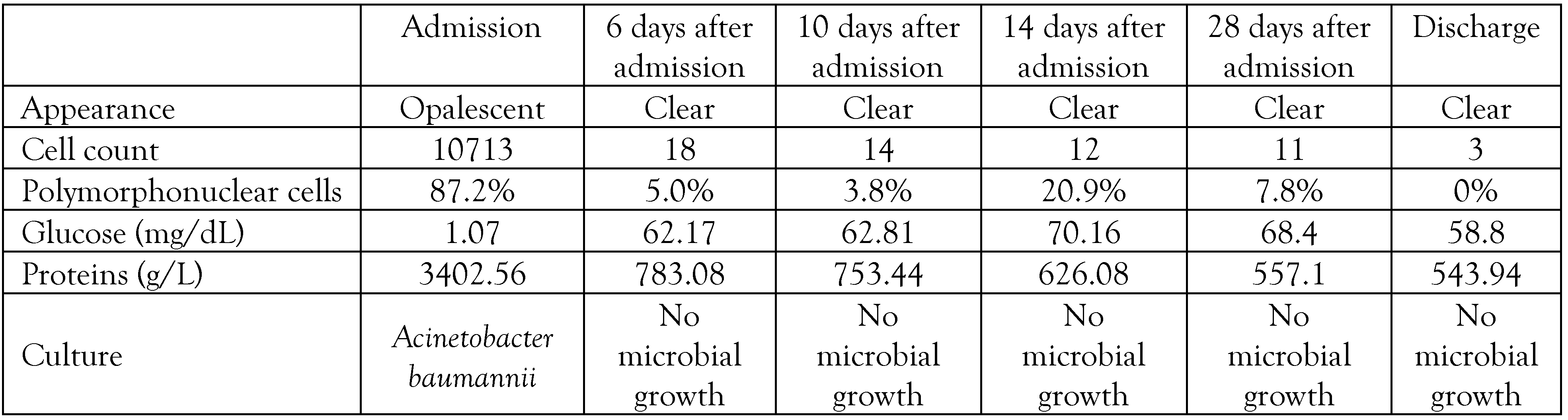
Table 1.
Dynamics of inflammatory markers.

Table 2.
Dynamics of cerebrospinal fluid (CSF) analysis.
One week before discharge, the brain MRI (Figure 2) showed a postoperative meningocele unchanged compared to the previous examination, occipital craniectomy, and a lesion in the left cerebellar hemisphere, imaging-compatible with an abscess, relatively stable in size compared to the prior study, with chronic inflammatory changes in the bilateral maxillary sinuses.

Figure 2.
Brain MRI one week before discharge in axial and sagittal section.
After 41 days of hospitalization in Infectious Diseases Department the patient was transferred to the Neurosurgery Department for re-evaluation of the possibility of surgical management of the cerebellar abscess. At the time of transfer from our clinic, the patient exhibited no signs of meningeal irritation, was conscious, cooperative, afebrile, with a Glasgow Coma Scale score of 15, and stable cardiorespiratory and digestive status.
Discussion
Multidrug-resistant (MDR) and extensively drug-resistant (XDR) Acinetobacter baumannii represent a growing challenge in neurosurgical and critical care settings. These pathogens are predominantly associated with post-neurosurgical infections or infections related to ventricular devices. Their high potential for multidrug resistance, reported in over 50% of clinical isolates, severely limits therapeutic options. The treatment of A. baumannii meningitis is particularly difficult due to the poor penetration of most antibiotics across the blood-brain barrier. Conventional intravenous therapy often fails to achieve bactericidal concentrations in the CSF, necessitating consideration of intrathecal or intraventricular routes for effective management. In the absence of standardized treatment protocols, individualized approaches based on antimicrobial susceptibility, clinical status, and drug availability are recommended, in accordance with IDSA guidelines [3].
In this case, the patient developed MDR A. baumannii meningitis and a probable cerebellar abscess following neurosurgical intervention for a hemorrhagic stroke. Initial empirical therapy with meropenem and vancomycin was chosen pending microbiological confirmation. Once the pathogen was identified as extensively drug-resistant and susceptible only to colistin and cefiderocol, therapy was escalated to intravenous cefiderocol and colistin. Given the limited CSF penetration of intravenous antibiotics and the complexity of the CNS infection, an intrathecal catheter was placed for colistin administration, following IDSA dosage recommendations [4].
Surgical intervention for the cerebellar abscess was deferred due to its high-risk location and potential impact on the patient’s quality of life. Instead, conservative management was employed, combining intravenous and intrathecal antibiotics, corticosteroids, cerebral depletive measures, and supportive care. Dynamic imaging and serial lumbar punctures guided therapy and allowed progressive reduction of the abscess. After 14 days of intensive therapy, a de-escalation regimen with ampicillin/sulbactam, oral minocycline, and continued colistin was implemented for an additional 21 days, ensuring continued pathogen suppression while minimizing toxicity.
This case illustrates the necessity of an interdisciplinary approach, integrating infectious disease specialists, neurologists, neurosurgeons, and intensive care teams, to optimize outcomes in complex MDR CNS infections [5].
It also highlights the importance of individualized therapy based on microbiological data, drug pharmacokinetics, and patient-specific surgical risk considerations.
Conclusions
MDR Acinetobacter baumannii represents an important etiologic agent in post-neurosurgical infections and infections associated with ventricular devices. Antimicrobial therapy for A. baumannii meningitis is often suboptimal due to the limited penetration of most antibiotics into the CSF. Nevertheless, intrathecal or intraventricular administration of colistin has been increasingly utilized as an adjunctive strategy to rapidly achieve bactericidal concentrations. Interdisciplinary collaboration among infectious disease specialists, neurologists, neurosurgeons, and intensivists is essential for the management of these complex cases.
Author Contributions
Study conception and design: MEV, NMM, AEP. Acquisition of data: MEV, NC, BFN. Analysis and interpretation of data: MEV, LZ. Drafting of manuscript: MEV, OEI. Critical revision: RCC, SCC, IMD.All authors read and approved the final version of the manuscript.
Funding
None to declare.
Institutional Review Board Statement
Approval of this case report was obtained from the Ethics Committee of the Clinical Hospital of Infectious Diseases Constanța. Informed consent was obtained in writing.
Informed Consent Statement
Written informed consent was obtained from the patient for publication of their case report and the accompanying images.
Conflicts of Interest
All authors—none to declare.
References
- Kasper, D.L.; Fauci, A.S. (Eds.) Harrison’s Infectious Diseases, 3rd ed.; McGraw-Hill Education: New York, NY, USA, 2017; pp. 353–356. [Google Scholar]
- Khawcharoenporn, T.; Apisarnthanarak, A.; Mundy, L.M. Intrathecal colistin for drug-resistant Acinetobacter baumannii central nervous system infection: A case series and systematic review. Clin. Microbiol. Infect. 2010, 16, 888–894. [Google Scholar] [CrossRef]
- Karaiskos, I.; Galani, L.; Baziaka, F.; Giamarellou, H. Intraventricular and intrathecal colistin as the last therapeutic resort for the treatment of multidrug-resistant and extensively drug-resistant Acinetobacter baumannii ventriculitis and meningitis: A literature review. Int. J. Antimicrob. Agents 2013, 41, 499–508. [Google Scholar] [CrossRef]
- Sollima, A.; Rossini, F.; Lanza, P.; et al. Role of cefiderocol in multidrug-resistant gram-negative central nervous system infections: Real life experience and state-of-the-art. Antibiotics 2024, 13, 453. [Google Scholar] [CrossRef] [PubMed]
- Cascio, A.; Conti, A.; Sinardi, L.; et al. Post-neurosurgical multidrug-resistant Acinetobacter baumannii meningitis successfully treated with intrathecal colistin. A new case and a systematic review of the literature. Int. J. Infect. Dis. 2010, 14, e572–e579. [Google Scholar] [CrossRef] [PubMed]
© GERMS 2025.