Clinical Spectrum of Extrapulmonary Non-Tuberculous Mycobacterial Disease in Immunocompetent Patients: A Case Series
Abstract
Introduction
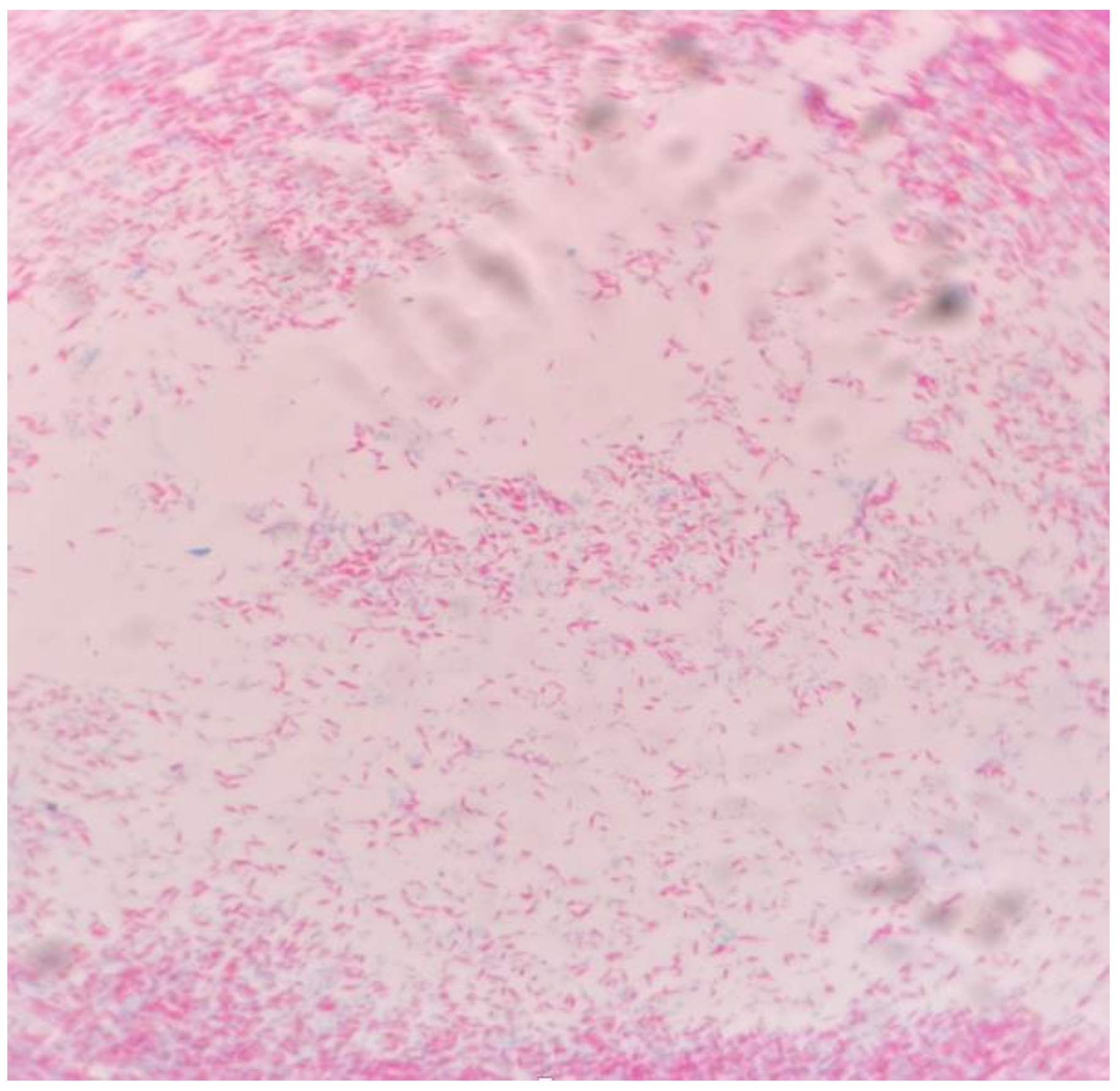
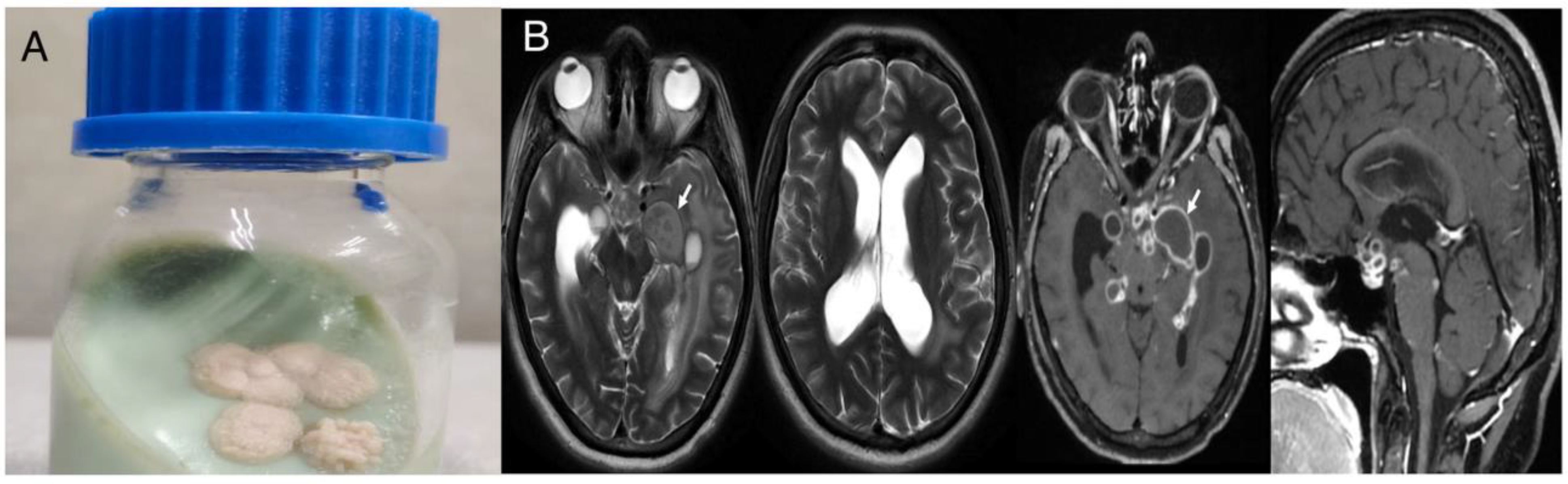
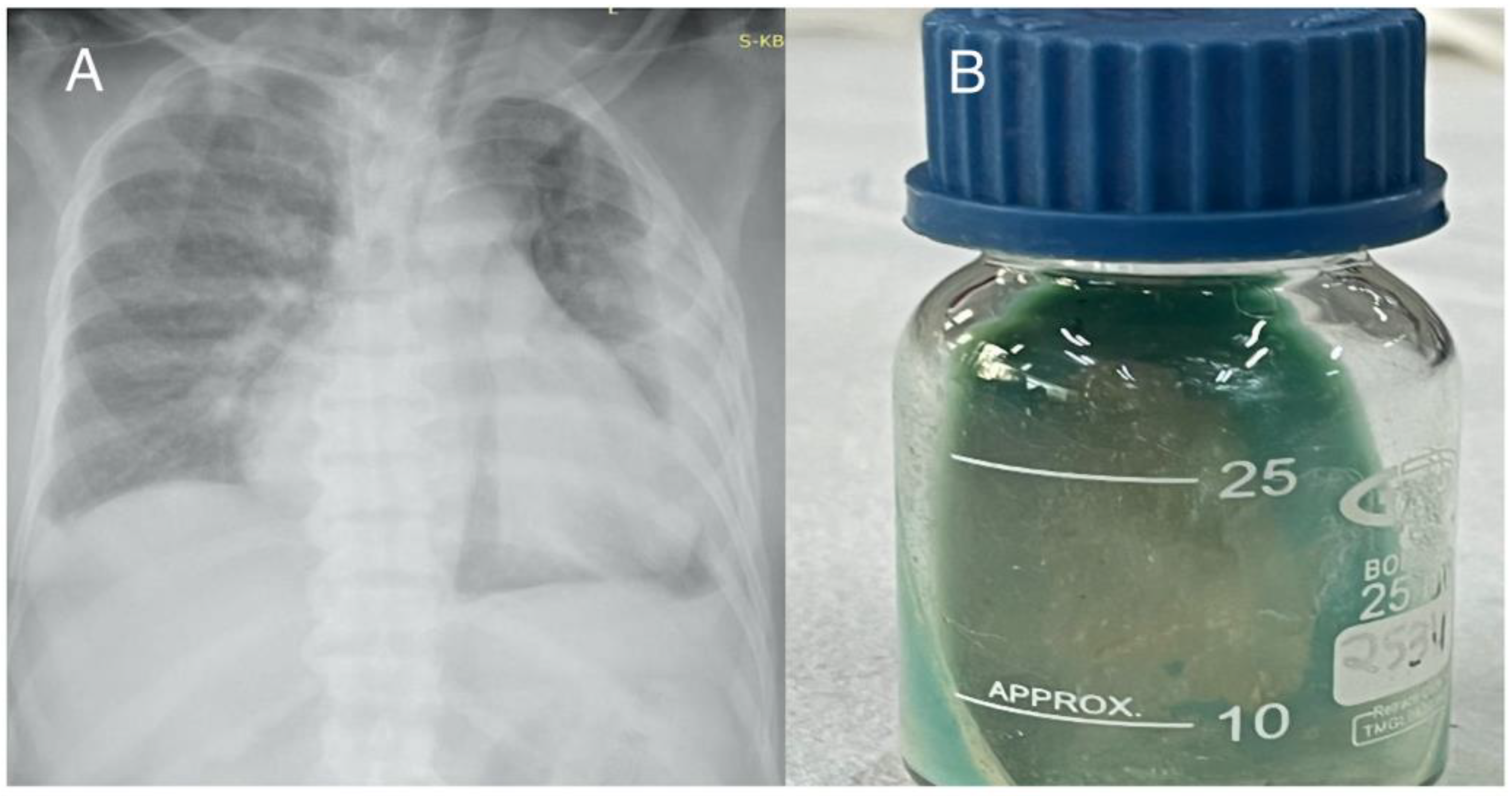
Case reports
Case 1
Case 2
Case 3
Case 4
Discussion
Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Gupta, N.; Mittal, A.; Niyas, V.K.M.; et al. Nontuberculous mycobacteria: A report of eighteen cases from a tertiary care center in India. Lung India. 2020, 37, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Tiberi, S.; Farooqi, J.; et al. Non-tuberculous mycobacterial infections-a neglected and emerging problem. Int. J. Infect. Dis. 2020, 92S, S46–S50. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K.; Sharma, R.; Singh, B.K.; et al. A prospective study of non-tuberculous mycobacterial disease among tuberculosis suspects at a tertiary care centre in north Indian. J. Med. Res. 2019, 150, 458–467. [Google Scholar] [CrossRef]
- Wani, S.R.; Wattal, C.; Raveendran, R. Epidemiology and risk factors associated with NTM pulmonary and extrapulmonary infections in a high tuberculosis endemic region. Indian. J. Med. Microbiol. 2020, 38, 16975. [Google Scholar] [CrossRef] [PubMed]
- Umrao, J.; Singh, D.; Zia, A.; et al. Prevalence and species spectrum of both pulmonary and extrapulmonary nontuberculous mycobacteria isolates at a tertiary care center. Int. J. Mycobacteriol. 2016, 5, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Mohajeri, P.; Norozi, B.; Atashi, S.; Farahani, A. Anti tuberculosis drug resistance in west of Iran. J. Glob. Infect. Dis. 2014, 6, 114–117. [Google Scholar] [CrossRef] [PubMed]
- Mohajeri, P.; Moradi, S.; Atashi, S.; Farahani, A. Mycobacterium tuberculosis Beijing genotype in western Iran: Distribution and drug resistance. J Clin Diagn Res. 2016, 10, DC05–DC07. [Google Scholar] [CrossRef] [PubMed]
- Porvaznik, I.; Solovič, I.; Mokrý, J. Non-tuberculous mycobacteria: Classification, diagnostics, and therapy. Exp. Med. Biol. 2017, 944, 19–25. [Google Scholar] [CrossRef]
- Johansen, M.D.; Herrmann, J.L.; Kremer, L. Nontuberculous mycobacteria and the rise of Mycobacterium abscessus. Nat. Rev. Microbiol. 2020, 18, 392–407. [Google Scholar] [CrossRef] [PubMed]
- Griffith, D.E.; Aksamit, T.; Brown-Elliott, B.A.; et al. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 2007, 175, 367–416. [Google Scholar] [CrossRef] [PubMed]
- Stout, J.E.; Koh, W.J.; Yew, W.W. Update on pulmonary disease due to non-tuberculous mycobacteria. Int. J. Infect. Dis. 2016, 45, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Mandell, D.L.; Wald, E.R.; Michaels, M.G.; Dohar, J.E. Management of nontuberculous mycobacterial cervical lymphadenitis. Arch. Otolaryngol. Head. Neck Surg. 2003, 129, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Meena, D.S.; Kumar, D.; Meena, V.; Bohra, G.K.; Tak, V.; Garg, M.K. Epidemiology, clinical presentation, and predictors of outcome in nontuberculous mycobacterial central nervous system infection: A systematic review. Trop. Med. Health. 2023, 51, 54. [Google Scholar] [CrossRef] [PubMed]
- Flor, A.; Capdevila, J.A.; Martin, N.; Gavaldà, J.; Pahissa, A. Nontuberculous mycobacterial meningitis: Report of two cases and review. Clin. Infect. Dis. 1996, 23, 1266–1273. [Google Scholar] [CrossRef] [PubMed]
- Talati, N.J.; Rouphael, N.; Kuppalli, K.; Franco-Paredes, C. Spectrum of CNS disease caused by rapidly growing mycobacteria. Lancet Infect. Dis. 2008, 8, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Bourlon, C.; Vargas-Serafín, C.; López-Karpovitch, X. Mycobacterium genavense invading the bone marrow in a HIV-positive patient. Clin. Case Rep. 2017, 5, 1043–1045. [Google Scholar] [CrossRef] [PubMed]
- Yazisiz, V.; Erbasan, F.; Inan, D.; et al. Bone marrow infection caused by Mycobacterium avium complex in a patient with systemic lupus erythematosus. Lupus 2010, 19, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Mohajeri, P.; Yazdani, L.; Shahraki, A.H.; et al. Verification of frequency in species of nontuberculous mycobacteria in Kermanshah drinking water supplies using the PCRsequencing method. Microb. Drug Resist. 2017, 23, 35964. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, A.D.; Mirsaeidi, M.; Farahani, A.; et al. Prevalence of nontuberculous mycobacteria and high efficacy of dcycloserine and its synergistic effect with clarithromycin against Mycobacterium fortuitum and Mycobacterium abscessus. Infect. Drug Resist. 2018, 11, 2521–2532. [Google Scholar] [CrossRef] [PubMed]
- Lindeboom, J.A.; Kuijper, E.J.; Bruijnesteijn van Coppenraet, E.S.; Lindeboom, R.; Prins, J.M. Surgical excision versus antibiotic treatment for nontuberculous mycobacterial cervicofacial lymphadenitis in children: A multicenter, randomized, controlled trial. Clin. Infect. Dis. 2007, 44, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
 |
© GERMS 2025.
Share and Cite
Yadav, P.; Meena, D.S.; Kumar, D.; John, N.; Kaur, N.; Kombade, S.; Bohra, G.K.; Tiwari, S.; Nag, V. Clinical Spectrum of Extrapulmonary Non-Tuberculous Mycobacterial Disease in Immunocompetent Patients: A Case Series. GERMS 2024, 14, 197-203. https://doi.org/10.18683/germs.2024.1431
Yadav P, Meena DS, Kumar D, John N, Kaur N, Kombade S, Bohra GK, Tiwari S, Nag V. Clinical Spectrum of Extrapulmonary Non-Tuberculous Mycobacterial Disease in Immunocompetent Patients: A Case Series. GERMS. 2024; 14(2):197-203. https://doi.org/10.18683/germs.2024.1431
Chicago/Turabian StyleYadav, Prakrati, Durga Shankar Meena, Deepak Kumar, Nikhil John, Navneet Kaur, Sarika Kombade, Gopal Krishana Bohra, Sarvesh Tiwari, and Vijaylaxmi Nag. 2024. "Clinical Spectrum of Extrapulmonary Non-Tuberculous Mycobacterial Disease in Immunocompetent Patients: A Case Series" GERMS 14, no. 2: 197-203. https://doi.org/10.18683/germs.2024.1431
APA StyleYadav, P., Meena, D. S., Kumar, D., John, N., Kaur, N., Kombade, S., Bohra, G. K., Tiwari, S., & Nag, V. (2024). Clinical Spectrum of Extrapulmonary Non-Tuberculous Mycobacterial Disease in Immunocompetent Patients: A Case Series. GERMS, 14(2), 197-203. https://doi.org/10.18683/germs.2024.1431




