Febrile Illness of Bacterial Etiology in a Public Fever Hospital in Egypt: High Burden of Multidrug Resistance and WHO Priority Gram Negative Pathogens
Abstract
Introduction
Methods
Study design
Microbiological procedures
Antimicrobial susceptibility testing
Identification of MDR phenotypes
Phenotypic detection of ESBL producers
Genotypic detection of ESBL and carbapenemase-encoding genes
Statistical analyses
Results
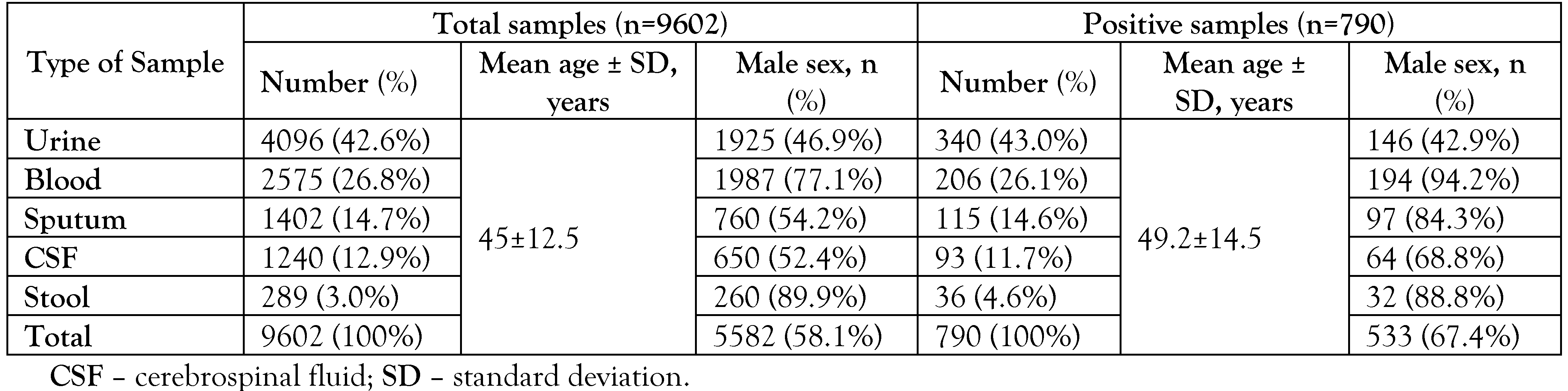
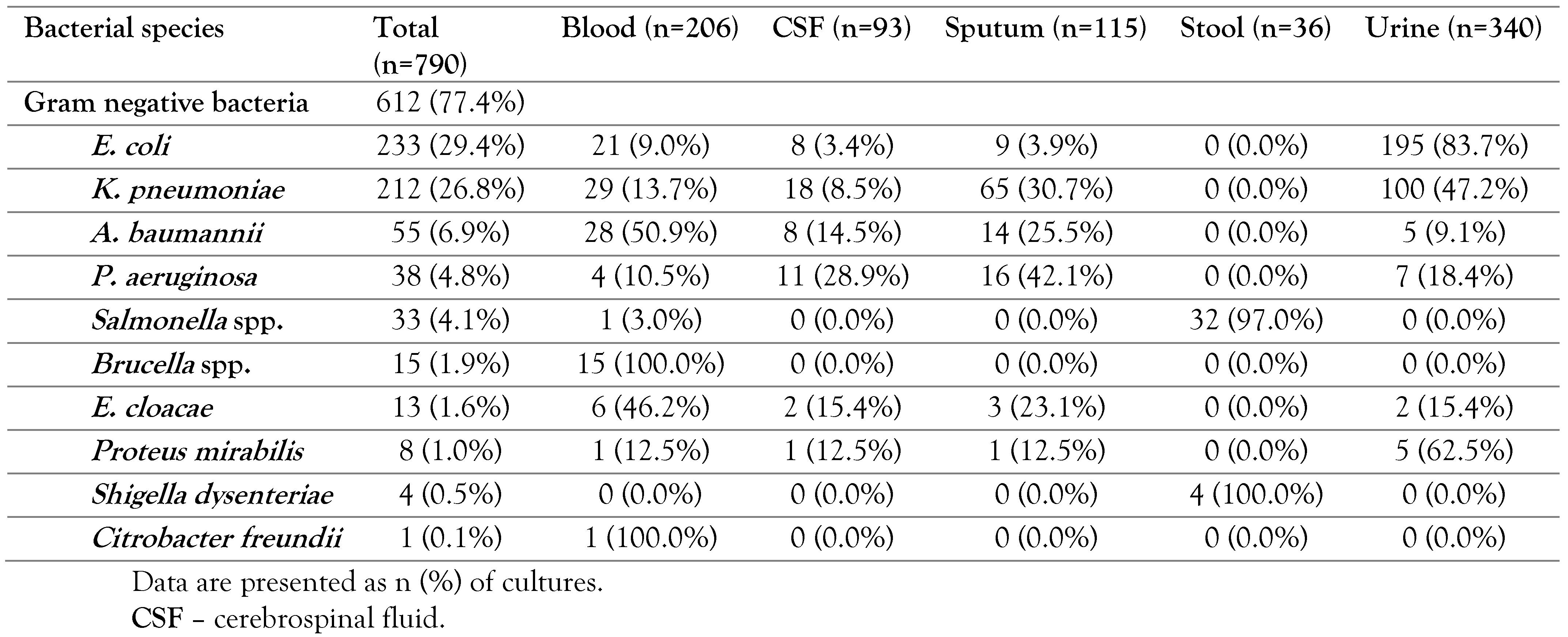
Bacterial pathogens causing febrile illness
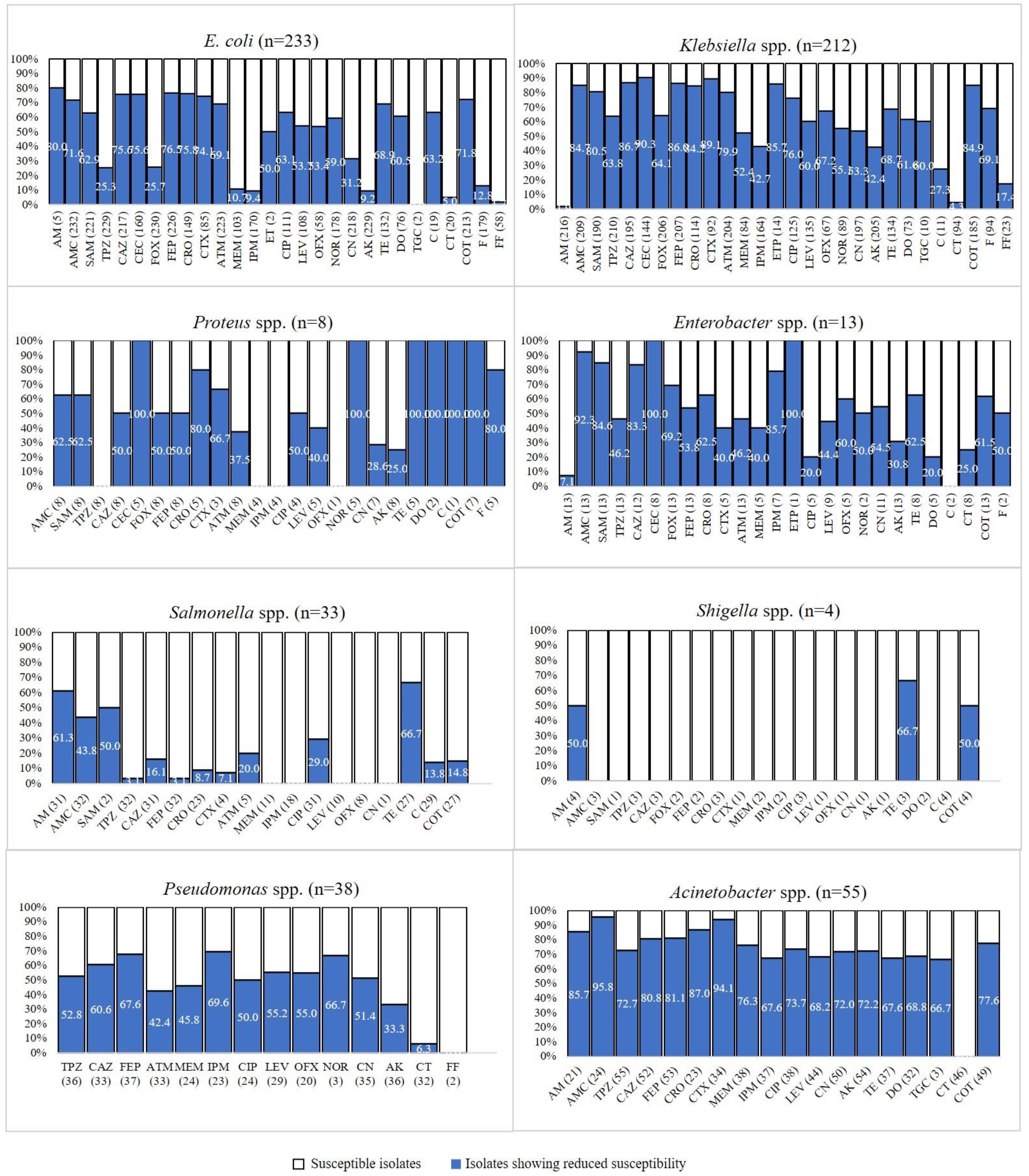
Antimicrobial susceptibility findings
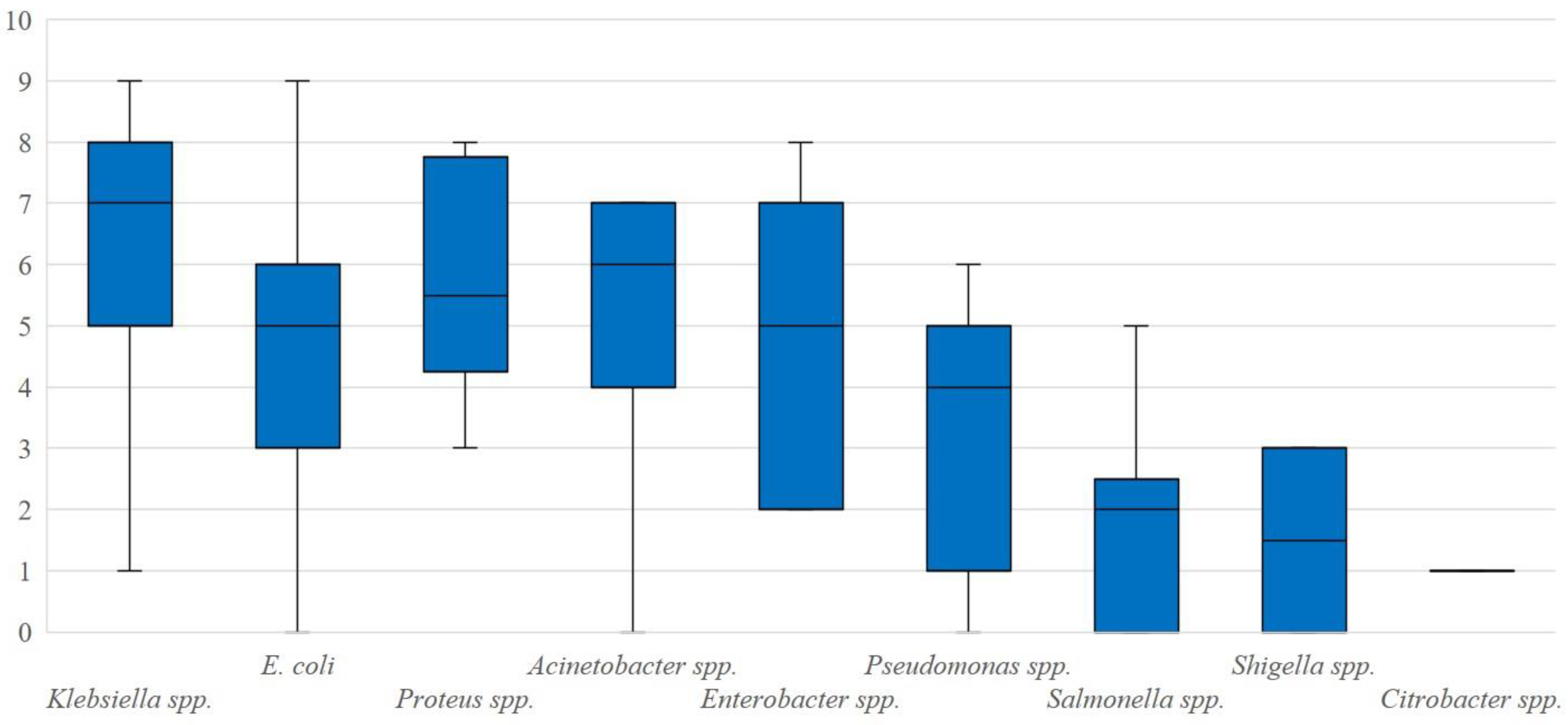
Antimicrobial susceptibility MDR pathogens
PCR detection of ESBL and carbapenemase-encoding genes
Discussion
Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of interest
References
- Steele, G.M.; Franco-Paredes, C.; Chastain, D.B. Noninfectious causes of fever in adults. Nurse Pract. 2018, 43, 38–44. [Google Scholar] [CrossRef]
- O’Grady, N.P.; Barie, P.S.; Bartlett, J.G.; et al. Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med. 2008, 36, 1330–1349. [Google Scholar] [CrossRef]
- Laxminarayan, R.; Matsoso, P.; Pant, S.; et al. Access to effective antimicrobials: A worldwide challenge. Lancet 2016, 387, 168–175. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Parker, T.M.; Murray, C.K.; Richards, A.L.; et al. Concurrent infections in acute febrile illness patients in Egypt. Am J Trop Med Hyg. 2007, 77, 390–392. [Google Scholar] [CrossRef]
- Afifi, S.; Earhart, K.; Azab, M.A.; et al. Hospital-based surveillance for acute febrile illness in Egypt: A focus on community-acquired bloodstream infections. Am J Trop Med Hyg. 2005, 73, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Mabrouk, S.S.; Abdellatif, G.R.; El-Ansary, M.R.; Aboshanab, K.M.; Ragab, Y.M. Carbapenemase producers among extensive drug-resistant gram-negative pathogens recovered from febrile neutrophilic patients in Egypt. Infect Drug Resist. 2020, 13, 3113–3124. [Google Scholar] [CrossRef] [PubMed]
- Masoud, S.M.; Abd El-Baky, R.M.; Aly, S.A.; Ibrahem, R.A. Co-existence of certain ESBLs, MBLs and plasmid mediated quinolone resistance genes among MDR E. coli isolated from different clinical specimens in Egypt. Antibiotics (Basel) 2021, 10, 835. [Google Scholar] [CrossRef]
- Abdelkader, M.M.; Aboshanab, K.M.; El-Ashry, M.A.; Aboulwafa, M.M. Prevalence of MDR pathogens of bacterial meningitis in Egypt and new synergistic antibiotic combinations. PLoS ONE 2017, 12, e0171349. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; Twenty-second informational supplement, in CLSI supplement M100; CLSI: Wayne, PA, 2018. [Google Scholar]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- Kamel, N.A.; Elsayed, K.M.; Awad, M.F.; Aboshanab, K.M.; El Borhamy, M.I. Multimodal interventions to prevent and control carbapenem-resistant Enterobacteriaceae and extended-spectrum beta-lactamase producer-associated infections at a tertiary care hospital in Egypt. Antibiotics (Basel) 2021, 10, 509. [Google Scholar] [CrossRef]
- Sambrook, J.; Fritsch, E.F.; Maniatis, T. Molecular cloning: A laboratory manual; Cold Spring Harbor Laboratory Press: Cold Spring Harbor, NY, USA, 1989. [Google Scholar]
- Shrestha, P.; Dahal, P.; Ogbonnaa-Njoku, C.; et al. Non-malarial febrile illness: A systematic review of published aetiological studies and case reports from Southern Asia and South-eastern Asia, 1980–2015. BMC Med. 2020, 18, 299. [Google Scholar] [CrossRef]
- Shortliffe, L.M.; McCue, J.D. Urinary tract infection at the age extremes: Pediatrics and geriatrics. Am J Med. 2002, 113 (Suppl. 1A), 55s–66s. [Google Scholar] [CrossRef]
- Wright, W.F.; Auwaerter, P.G. Fever and fever of unknown origin: Review, recent advances, and lingering dogma. Open Forum Infect Dis. 2020, 7, ofaa132. [Google Scholar] [CrossRef]
- Kalal, B.S.; Nagaraj, S. Urinary tract infections: A retrospective, descriptive study of causative organisms and antimicrobial pattern of samples received for culture, from a tertiary care setting. Germs 2016, 6, 132–138. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Benaissa, E.; Belouad, E.; Mechal, Y.; et al. Multidrug-resistant community-acquired urinary tract infections in a northern region of Morocco: Epidemiology and risk factors. Germs 2021, 11, 562–569. [Google Scholar] [CrossRef]
- El-Sokkary, R.H.; Ramadan, R.A.; El-Shabrawy, M.; et al. Community acquired pneumonia among adult patients at an Egyptian university hospital: Bacterial etiology, susceptibility profile and evaluation of the response to initial empiric antibiotic therapy. Infect Drug Resist. 2018, 11, 2141–2150. [Google Scholar] [CrossRef]
- Wasfi, R.; Rasslan, F.; Hassan, S.S.; Ashour, H.M.; Abd El-Rahman, O.A. Co-existence of carbapenemase-encoding genes in Acinetobacter baumannii from cancer patients. Infect Dis Ther. 2021, 10, 291–305. [Google Scholar] [CrossRef]
- Higgins, P.G.; Dammhayn, C.; Hackel, M.; Seifert, H. Global spread of carbapenem-resistant Acinetobacter baumannii. J Antimicrob Chemother. 2010, 65, 233–238. [Google Scholar] [CrossRef]
- Pogue, J.M.; Mann, T.; Barber, K.E.; Kaye, K.S. Carbapenem-resistant Acinetobacter baumannii: Epidemiology, surveillance and management. Expert Rev Anti Infect Ther. 2013, 11, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Talaat, M.; Saied, T.; Kandeel, A.; et al. A point prevalence survey of antibiotic use in 18 hospitals in Egypt. Antibiotics (Basel) 2014, 3, 450–460. [Google Scholar] [CrossRef]
- Dooling, K.L.; Kandeel, A.; Hicks, L.A.; et al. Understanding antibiotic use in Minya District, Egypt: Physician and pharmacist prescribing and the factors influencing their practices. Antibiotics (Basel) 2014, 3, 233–243. [Google Scholar] [CrossRef]
- Grundmann, H.; Glasner, C.; Albiger, B.; et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): A prospective, multinational study. Lancet Infect Dis. 2017, 17, 153–163. [Google Scholar] [CrossRef]
- Ghaith, D.M.; Zafer, M.M.; Said, H.M.; et al. Genetic diversity of carbapenem-resistant Klebsiella pneumoniae causing neonatal sepsis in intensive care unit, Cairo, Egypt. Eur J Clin Microbiol Infect Dis. 2020, 39, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Jin, L.; Ouyang, P.; et al. Evolution of hypervirulence in carbapenem-resistant Klebsiella pneumoniae in China: A multicentre, molecular epidemiological analysis. J Antimicrob Chemother. 2020, 75, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Shane, A.L.; Mody, R.K.; Crump, J.A.; et al. 2017 Infectious Diseases Society of America Clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin Infect Dis. 2017, 65, 1963–1973. [Google Scholar] [CrossRef]
- Srikantiah, P.; Girgis, F.Y.; Luby, S.P.; et al. Population-based surveillance of typhoid fever in Egypt. Am J Trop Med Hyg. 2006, 74, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Li, S.; Li, Z.; et al. Enzootic situation and molecular epidemiology of Brucella in livestock from 2011 to 2015 in Qingyang, China. Emerg Microbes Infect. 2018, 7, 58. [Google Scholar] [CrossRef]
- Theuretzbacher, U.; Van Bambeke, F.; Cantón, R.; et al. Reviving old antibiotics. J Antimicrob Chemother. 2015, 70, 2177–2181. [Google Scholar] [CrossRef]
 |
 |
 |
 |
© GERMS 2022.
Share and Cite
Mostafa, S.H.; Saleh, S.E.; Hamed, S.M.; Aboshanab, K.M. Febrile Illness of Bacterial Etiology in a Public Fever Hospital in Egypt: High Burden of Multidrug Resistance and WHO Priority Gram Negative Pathogens. Germs 2022, 12, 75-85. https://doi.org/10.18683/germs.2022.1308
Mostafa SH, Saleh SE, Hamed SM, Aboshanab KM. Febrile Illness of Bacterial Etiology in a Public Fever Hospital in Egypt: High Burden of Multidrug Resistance and WHO Priority Gram Negative Pathogens. Germs. 2022; 12(1):75-85. https://doi.org/10.18683/germs.2022.1308
Chicago/Turabian StyleMostafa, Shimaa H., Sarra E. Saleh, Samira M. Hamed, and Khaled M. Aboshanab. 2022. "Febrile Illness of Bacterial Etiology in a Public Fever Hospital in Egypt: High Burden of Multidrug Resistance and WHO Priority Gram Negative Pathogens" Germs 12, no. 1: 75-85. https://doi.org/10.18683/germs.2022.1308
APA StyleMostafa, S. H., Saleh, S. E., Hamed, S. M., & Aboshanab, K. M. (2022). Febrile Illness of Bacterial Etiology in a Public Fever Hospital in Egypt: High Burden of Multidrug Resistance and WHO Priority Gram Negative Pathogens. Germs, 12(1), 75-85. https://doi.org/10.18683/germs.2022.1308




