Phytocompounds from Himalayan Medicinal Plants as Potential Drugs to Treat Multidrug-Resistant Salmonella typhimurium: An In Silico Approach
Abstract
1. Introduction
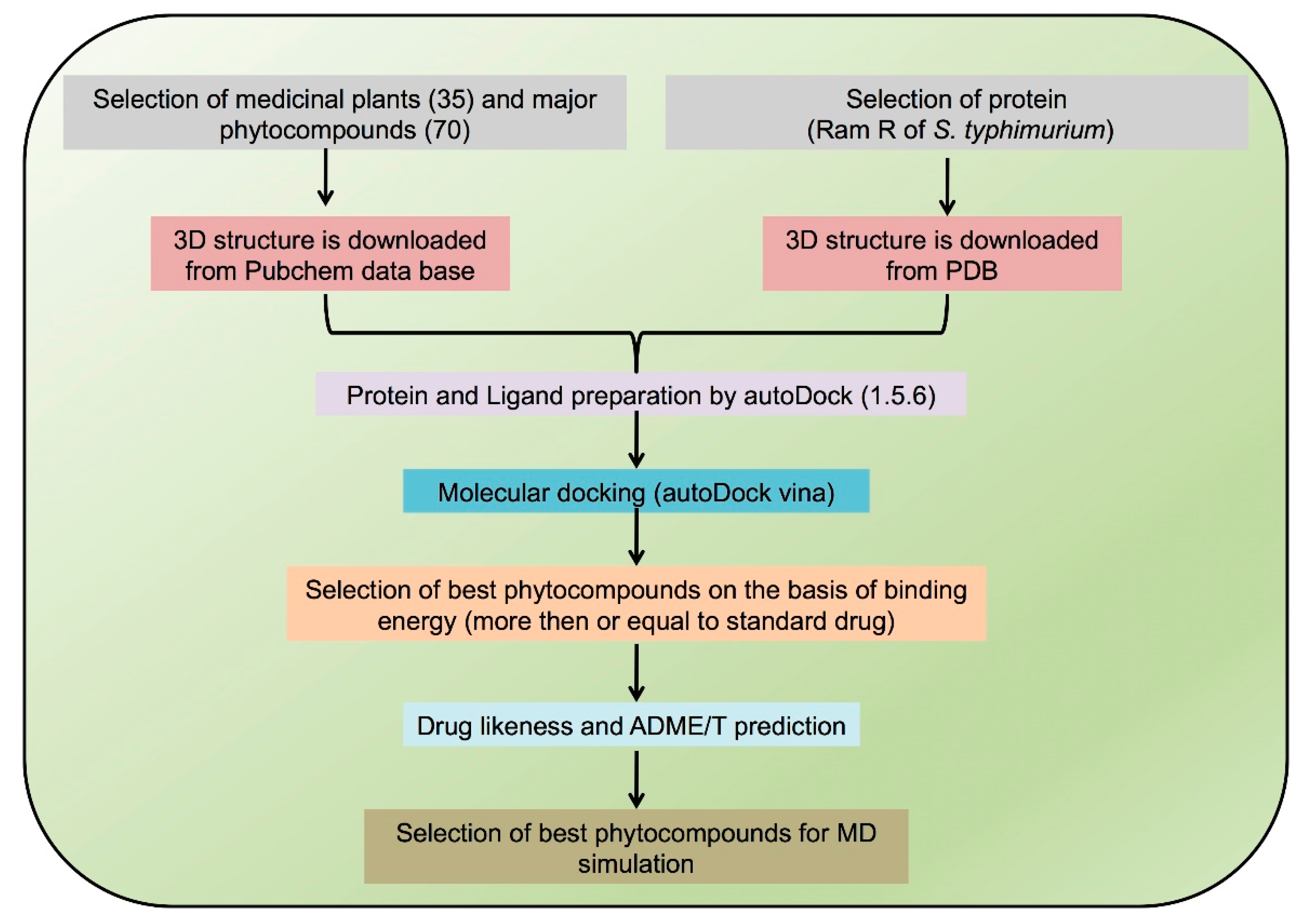
2. Methodology
2.1. Bioinformatics Tools
2.2. Ligand Preparation
2.3. Protein Preparation
2.4. Molecular Docking of Major Phytocompounds of Thirty-Five Medicinal Plants
2.5. Drug Likeness Calculations
2.6. ADMET Screening and Toxicity Prediction of Phytocompounds
2.7. MD Simulation of Protein Ligand Complexes
3. Results
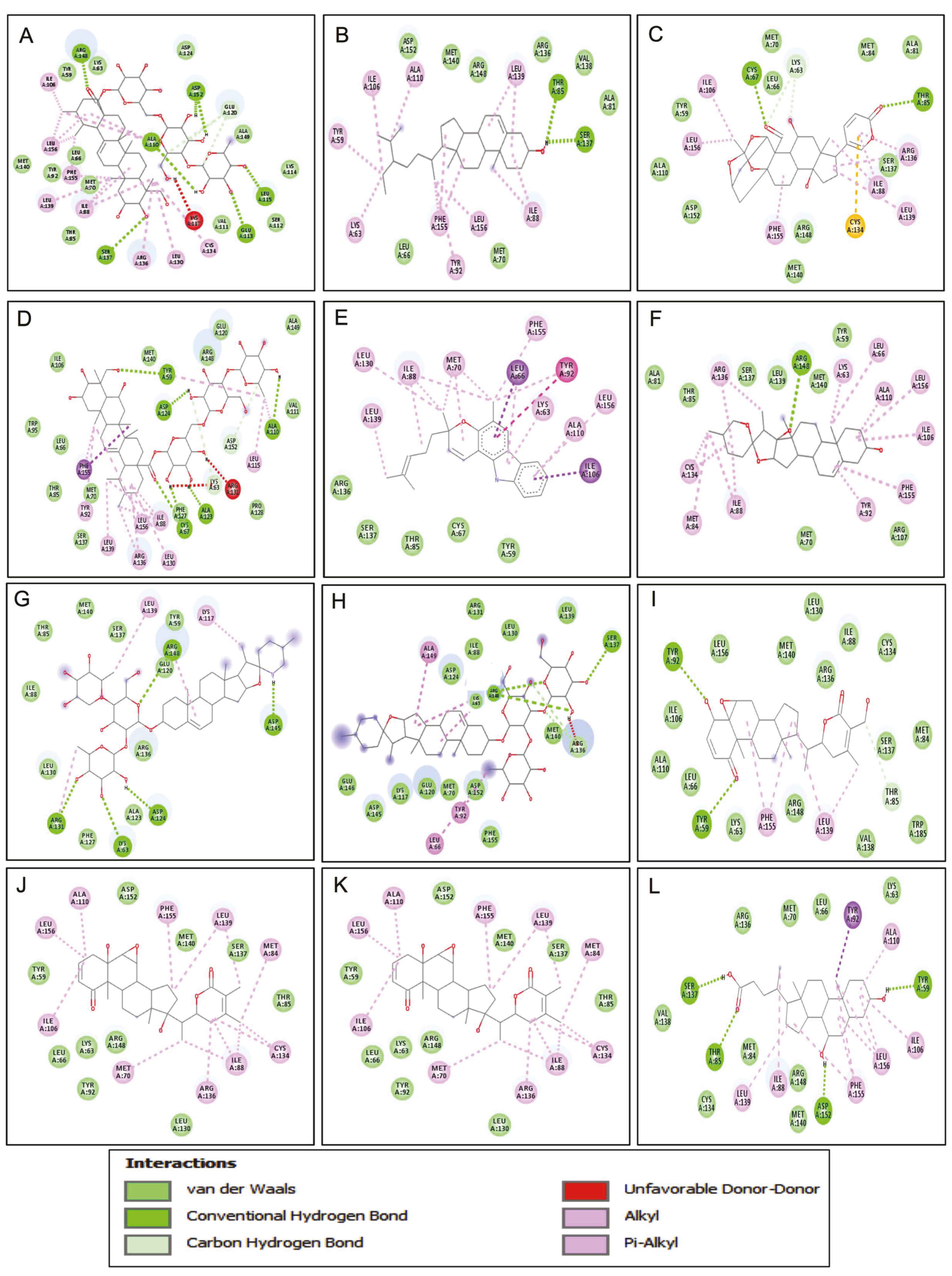
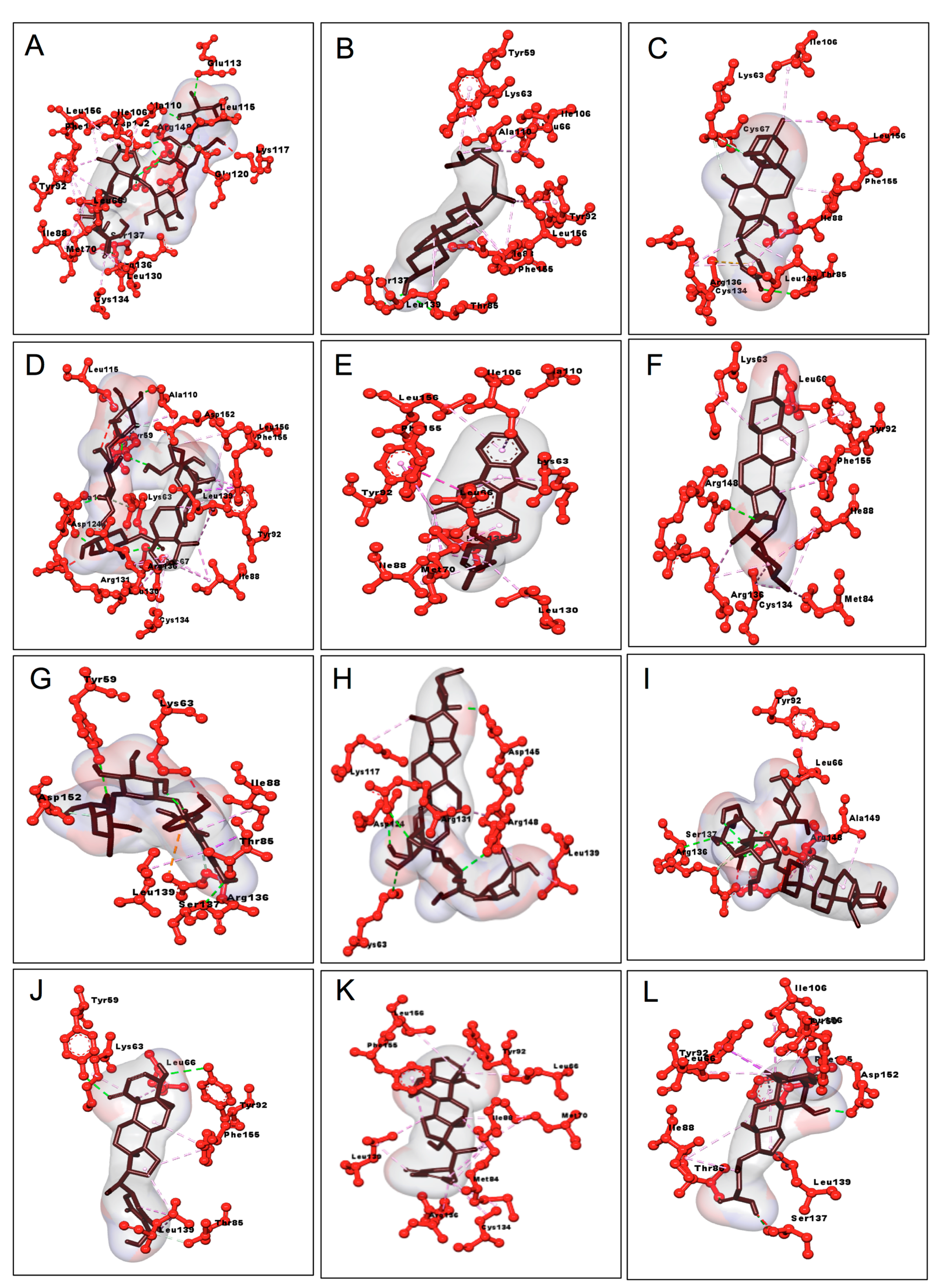
3.1. Molecular Docking of 70 Major Phytocompounds from 35 Medicinal Plants with Ram R Protein of S. typhimurium
3.2. Drug Likeness Prediction of Active Phytocompounds of Eight Medicinal Plants
3.3. Toxicity Prediction of Active Phytocompound and Chenodeoxycholic Acid
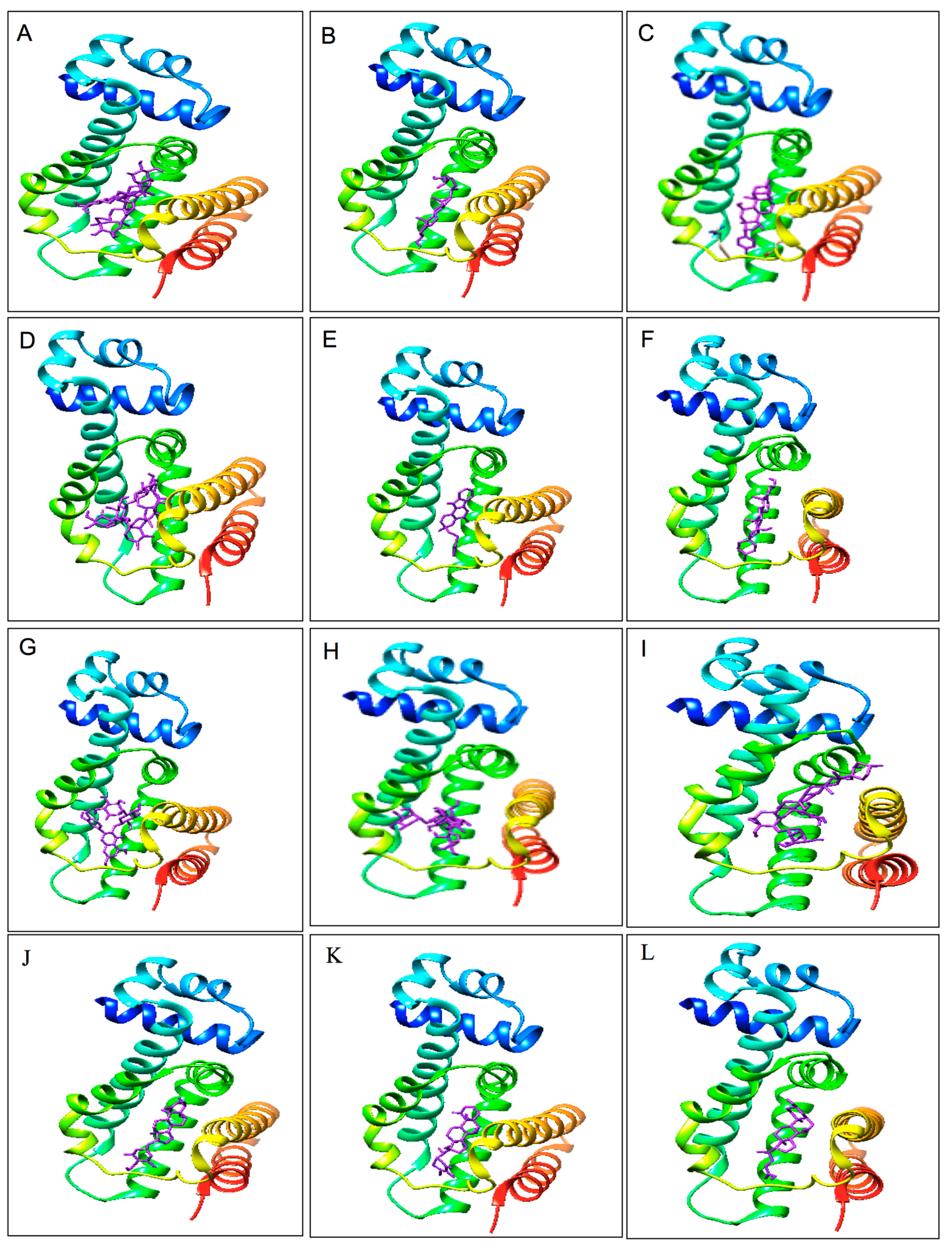
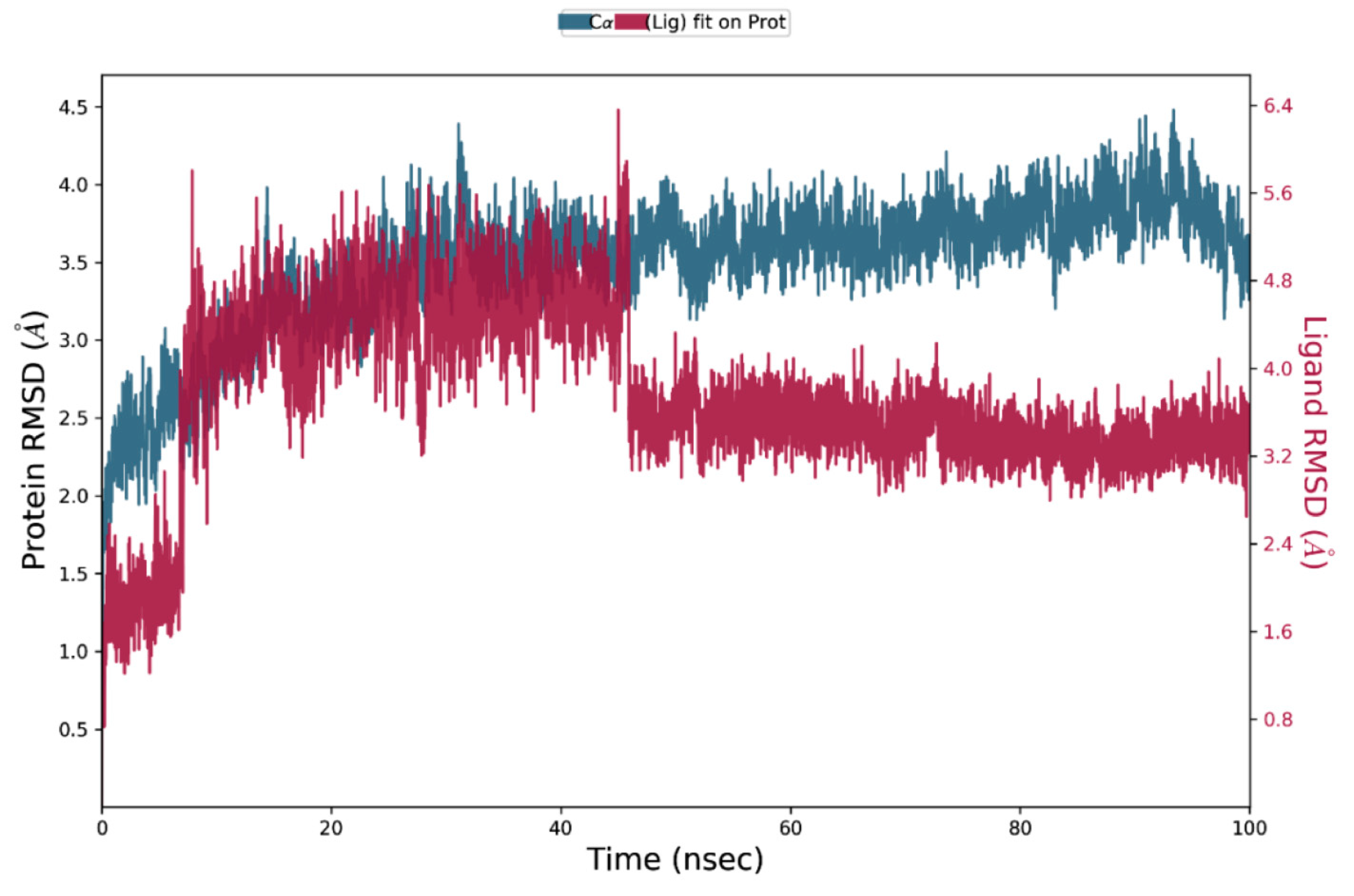
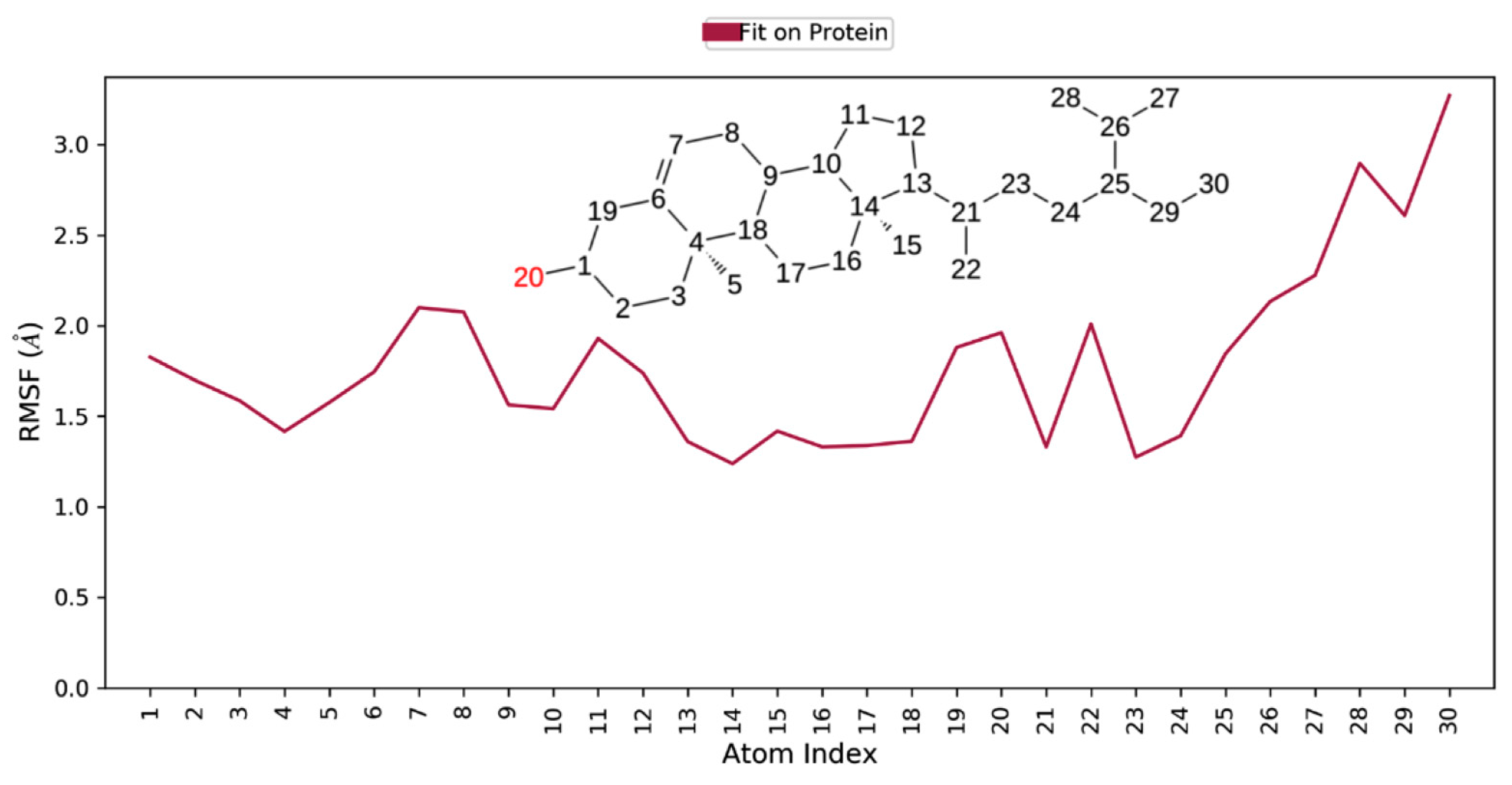
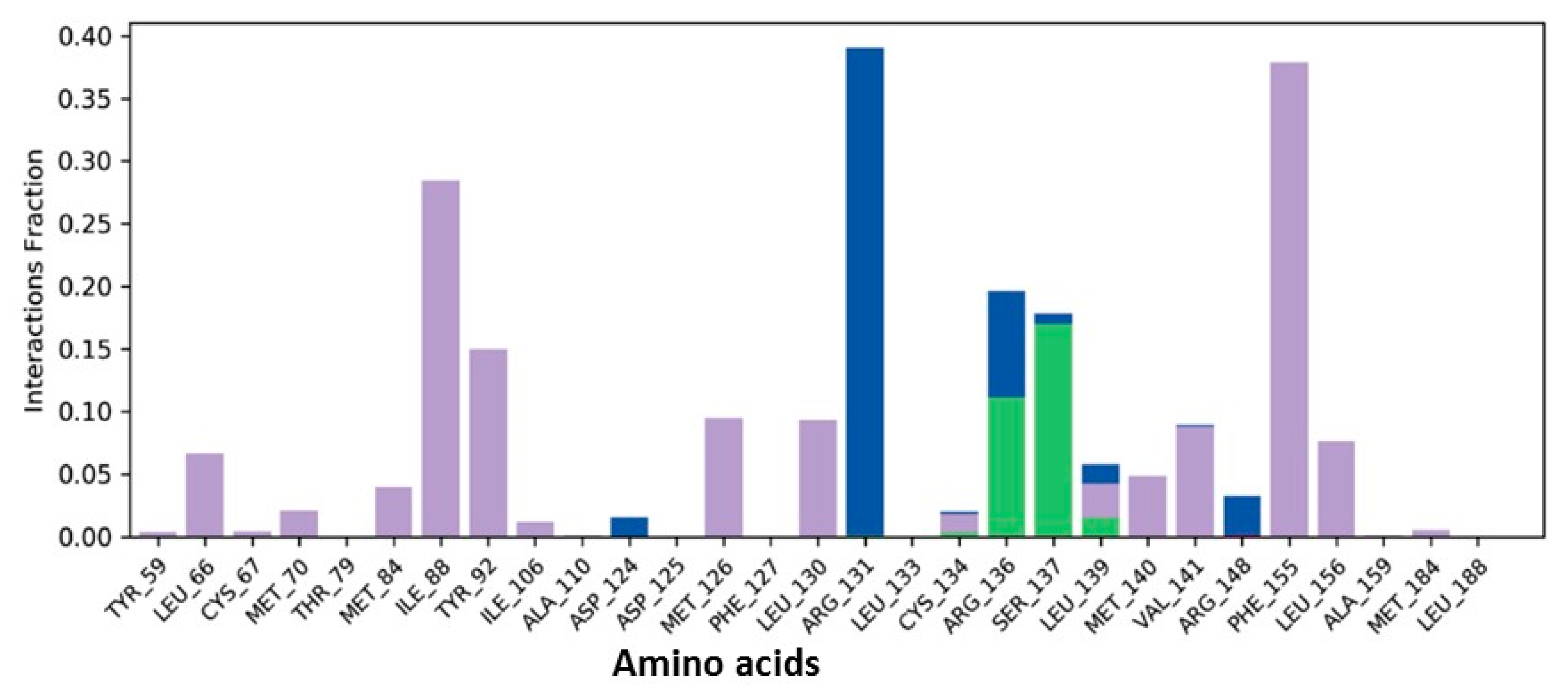
3.4. MD Simulation of Protein–Ligand Complexes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prouty, A.M.; Van Velkinburgh, J.C.; Gunn, J.S. Salmonella enterica serovar typhimurium resistance to bile: Identification and characterization of the tolQRA cluster. J. Bacteriol. 2002, 184, 1270–1276. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Begley, M.; Sleator, R.D.; Gahan, C.G.; Hill, C. Contribution of three bile-associated loci, bsh, pva, and btlB, to gastrointestinal persistence and bile tolerance of Listeria monocytogenes. Infect. Immun. 2005, 73, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Kabir, M.R.; Hossain, M.A.; Paul, S.K.; Mahmud, C.; Ahmad, S.; Mahmud, N.U.; Sultana, S.; Yesmin, T.; Hoque, S.M.; Habiba, U.; et al. Enteropathogens associated with acute diarrhea in a tertiary hospital of Bangladesh. Mymensingh Med. J. 2012, 21, 618–623. [Google Scholar]
- Kozak, G.K.; MacDonald, D.; Landry, L.; Farber, J.M. Foodborne outbreaks in Canada linked to produce: 2001 through 2009. J. Food Prot. 2013, 76, 173–183. [Google Scholar] [CrossRef]
- Scallan, E.; Hoekstra, R.M.; Angulo, F.J.; Tauxe, R.V.; Widdowson, M.A.; Roy, S.L.; Jones, J.L.; Griffin, P.M. Foodborne illness acquired in the United States—Major pathogens. Emerg. Infect. Dis. 2011, 17, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, S.; Lichtman, J.S.; Bouley, D.M.; Elias, J.E.; Monack, D.M. Role of disease-associated tolerance in infectious superspreaders. Proc. Natl. Acad. Sci. USA 2014, 111, 15780–15785. [Google Scholar] [CrossRef] [PubMed]
- Strugnell, R.A.; Scott, T.A.; Wang, N.; Yang, C.; Peres, N.; Bedoui, S.; Kupz, A. Salmonella vaccines: Lessons from the mouse model or bad teaching? Curr. Opin. Microbiol. 2014, 17, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Nishino, K.; Latifi, T.; Groisman, E.A. Virulence and drug resistance roles of multidrug efflux systems of Salmonella enterica serovar Typhimurium. Mol. Microbiol. 2006, 59, 126–141. [Google Scholar] [CrossRef]
- Prouty, A.M.; Brodsky, I.E.; Falkow, S.; Gunn, J.S. Bile-salt-mediated induction of antimicrobial and bile resistance in Salmonella typhimurium. Microbiology 2004, 150, 775–783. [Google Scholar] [CrossRef]
- Abouzeed, Y.M.; Baucheron, S.; Cloeckaert, A. RamR mutations involved in efflux-mediated multidrug resistance in Salmonella enterica serovar Typhimurium. Antimicrob. Agents Chemother. 2008, 52, 2428–2434. [Google Scholar] [CrossRef]
- Gordon, M.C.; David, J.N. Natural product drug discovery in the next millennium. Pharm. Biol. 2001, 39, 8–17. [Google Scholar]
- Lopez-Vallejo, F.; Caulfield, T.; Martínez-Mayorga, K.; Giulianotti, M.A.; Houghten, R.A.; Nefzi, A.; Medina-Franco, J.L. Integrating virtual screening and combinatorial chemistry for accelerated drug discovery. Comb. Chem. High Throughput Screen. 2011, 14, 475–487. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Sharma, R.; Kumar, A. Docking techniques in pharmacology: How much promising? Comput. Biol. Chem. 2018, 76, 210–217. [Google Scholar] [CrossRef] [PubMed]
- War, A.R.; Taggar, G.K.; Hussain, B.; Taggar, M.S.; Nair, R.M.; Sharma, H.C. Plant defence against herbivory and insect adaptations. AoB Plants 2018, 10, ply037. [Google Scholar]
- O’Boyle, N.M.; Banck, M.; James, C.A.; Morley, C.; Vandermeersch, T.; Hutchison, G.R. Open Babel: An open chemical toolbox. J. Cheminform. 2011, 3, 33. [Google Scholar] [CrossRef] [PubMed]
- Trott, O.; Olson, A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization and multithreading. J. Comput. Chem. 2010, 31, 455–461. [Google Scholar] [CrossRef]
- Boktapa, N.R.; Sharma, A.K. Wild medicinal plants used by local communities of Manali, Himachal Pradesh, India. Ethnobot. Leafl. 2010, 14, 259–267. [Google Scholar]
- Sharma, R.; Manhas, R.K.; Magotra, R. Ethnoveterinary remedies of diseases among milk yielding animals in Kathua, Jammu and Kashmir, India. J. Ethnopharmacol. 2012, 141, 265–272. [Google Scholar] [CrossRef]
- Baba, M.; Asano, R.; Takigami, I.; Takahashi, T.; Ohmura, M.; Okada, Y.; Sugimoto, H.; Arika, T.; Nishino, H.; Okuyama, T. Studies on Cancer Chemoprevention by Traditional Folk Medicines XXV.-Inhibitory Effect of Isoliquiritigenin on Azoxymethane-Induced Murine Colon Aberrant Crypt Focus Formation and Carcinogenesis. Biol. Pharm. Bull. 2002, 25, 247–250. [Google Scholar] [CrossRef]
- Kupeli, E.; Kosar, M.; Yesilada, E.; Baser, K.H.C. A comparative study on the anti-inflammatory, antinociceptive and antipyretic effects of isoquinoline alkaloids from the roots of Turkish Berberis species. Life Sci. 2002, 72, 645–657. [Google Scholar] [CrossRef]
- Duke, J.A.; Ayensu, E.S. Medicinal Plants of China; Reference Publications, Inc.: Algonac, MI, USA, 1985; ISBN 0-917256-20-4. [Google Scholar]
- Phillips, R.; Foy, N. Herbs; Pan Books Ltd.: London, UK, 1990; ISBN 0-330-30725-8. [Google Scholar]
- Kumar, S.; Chand, G.; Sankhyan, P. Herbal folk remedies for curing various ailments in lug valley of district kullu, himachal pradesh (n.w. himalaya). Int. J. Ayurvedic Herbmed. 2013, 3, 1308–1314. [Google Scholar]
- Dhananjay, J.; Deshpande, A. Hand Book of Medicinal Herbs; Agrobios: Jodhpur, India, 2006. [Google Scholar]
- Hasimi, N.; Ertas, A.; Oral, E.V.; Yener, I.; Alkan, H.; Boga, M.; Yılmaz, M.A.; Yener, I.; Gazioglu, I.; Ozaslan, C.; et al. Chemical profile of Malva neglecta and Malvellasherardiana by Lc-MS/MS, GC/MS and their anticholinesterase, antimicrobial and antioxidant properties with aflatoxin-contents. Marmara Pharm. J. 2017, 21, 471–484. [Google Scholar] [CrossRef]
- Taherian, R.; Taherian, M.; Maghsoudi, H.; Haj-alahyari, S. The effect of aqueous extract of Malva neglecta on expression of inflammatory biomarkers involved in pain in synoviocytes and THP -1 cells as a model of monocyte/macrophage and human cartilage cells in osteoarthritis. J. Cell. Mol. Anesth. 2017, 2, 149–156. [Google Scholar]
- Duke, J.A.; Bugenschutz-godwin, M.J.; Du collier, J.; Duke, P.K. Hand Book of Medicinal Herbs, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2002. [Google Scholar]
- Caliskan, O.; Polat, A.A. Phytochemical and antioxidant properties of selected fig (Ficus carica L.) accessions from the eastern Mediterranean region of Turkey. Sci. Hortic. 2011, 128, 473–478. [Google Scholar] [CrossRef]
- Sirohi, B.; Sagar, R. Antipyretic activity of hydroalcholic extract of D. hatagirea roots and Lavandula stoechas flowers on Brewers yeast induced Pyrexia in Wistar rats. J. Drug Discov. Ther. 2019, 9, 701–704. [Google Scholar]
- Sharma, S.; Jain, P.K.; Parkhe, G. Extraction, phytochemical screening and anti-inflammatory activity of hydro ethanolic extracts of roots of D. hatagirea. J. Drug Discov. Ther. 2020, 19, 86–90. [Google Scholar]
- Kumar, N.; Shikha, S.; George, V.C.; Suresh, P.K.; Kumar, R.A. Anticancer and anti-metastatic activities of rheum emodi rhizome chloroform extracts. Asian J. Pharm. Clin. Res. 2012, 5, 189–194. [Google Scholar]
- Arvindekar, A.U.; Laddha, K.S. An efficient microwave-assisted extraction of anthraquinones from Rheum emodi: Optimisation using RSM, UV and HPLC analysis and antioxidant studies. Ind. Crop. Prod. 2016, 83, 587–595. [Google Scholar] [CrossRef]
- Ahmad, W.; Zaidi, S.M.; Mujeeb, M.; Ansari, S.H.; Ahmad, S. HPLC and HPTLC methods by design for quantitative characterization and in vitro anti-oxidant activity of polyherbal formulation containing Rheum emodi. J. Chromatogr. Sci. 2014, 52, 911–918. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; Bhattacharya, S.; Jana, S.; Singh, D. Review on medicinally important species of picrorhiza. Int. J. Pharm. Res. Biosci. 2013, 2, 1–16. [Google Scholar]
- Bhattacharyya, P.; Kumaria, S.; Bose, B.; Paul, P.; Tandon, P. Evaluation of genetic stability and analysis of phytomedicinal potential in micro propagated plants of Rumex nepalensis—A medicinally important source of pharmaceutical biomolecules. J. Appl. Res. Med. Aromat. Plants 2017, 6, 80–91. [Google Scholar]
- Pandey, Y.; Bhatt, S.S. Overview of Himalayan yellow raspberry (Rubus ellipticus Smith): A nutraceutical plant. J. Appl. Nat. Sci. 2016, 8, 494–499. [Google Scholar] [CrossRef]
- Prajapati, S.N.; Parmar, K.A. Anti-viral and in-vitro free radical scavenging activity of leaves of Rubia cordifolia. Int. J. Phytomed. 2011, 3, 98–107. [Google Scholar]
- Grieve, M. A Modern Herbal; Dover Publications Inc.: New York, NY, USA, 1981; Volume 2, pp. 562–566. [Google Scholar]
- Mabey, R. The New Age Herbalist; Macmillan Publishing Company: New York, NY, USA, 1988; p. 113. [Google Scholar]
- Junior, G.M.V.; Rocha, C.Q.; Rodrigues, T.S.; Hiruma-Lima, C.A.; Vilegas, W. New steroidal saponins and antiulcer activity from Solanum paniculatum L. Food Chem. 2015, 186, 160–167. [Google Scholar] [CrossRef]
- Kadima, J.N.; Kasali, F.M.; Bavhure, B.; Mahano, A.O.; Bwironde, F.M. Comparative antidiabetic potential and survival function of Harungana madagascariensis, Physalis peruviana, Solanum Americanum and Tithonia diversifolia extracts on alloxan-induced diabetes in guinea-pigs. Int. J. Pharm. Pharm. Res. 2016, 5, 196–206. [Google Scholar]
- Pant, S.; Samant, S.S. Ethnobotanical observations in the Mornaula reserve forest of Komoun, West Himalaya, India. Ethnobot. Leafl. 2010, 14, 193–217. [Google Scholar]
- Rani, S.; Rana, J.C.; Rana, P.K. Ethnomedicinal plants of Chamba district, Himachal Pradesh, India. J. Med. Plant Res. 2013, 7, 3147–3157. [Google Scholar]
- Jugran, A.K.; Rawat, S.; Bhatt, I.D.; Rawal, R.S. Valeriana jatamansi: An herbaceous plant with multiple medicinal uses. Phytother. Res. 2019, 33, 482–503. [Google Scholar] [CrossRef]
- Li, Y.B.; Chen, C.; Mao, S.; Guo, C.; Zhao, T.T.; Wu, L.L.; Wang, X.Y.; Liu, A.; Yang, Z.Y. Anti-depression Effect and Mechanism of Valerianae Jatamansi Rhizoma et Radix. Chin. J. Exp. Tradit. Med. Formulae 2020, 26, 235–240. [Google Scholar]
- Verma, G.; Dua, V.K.; Agarwal, D.D.; Atul, P.K. Anti-malarial activity of Holarrhenaantidysenterica and Viola canes-cens, plants traditionally used against malaria in the Garhwal region of north-west Himalaya. Malar. J. 2011, 10, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Masood, M.; Arshad, M.; Asif, S.; Chaudhari, S.K. Viola canescens: Herbal wealth to be conserved. J. Bot. 2014, 2014, 1–6. [Google Scholar] [CrossRef]
- Bhatti, V.; Vashishtha, D. Indigenous plants in traditional healthcare system in Kedarnath valley of western Himalaya. Indian J. Tradit. Knowl. 2008, 7, 300–310. [Google Scholar]
- Rokaya, M.B.; Münzbergová, Z.; Timsina, B. Ethnobotanical study of medicinal plants from the Humla district of western Nepal. J. Ethnopharmacol. 2010, 130, 485–504. [Google Scholar] [CrossRef]
- Shrestha, S.S.; Sut, S.; Ferrarese, I.; Marco, B.D.S.; Zengin, G.; De Franco, M.; Pant, D.R.; Mahomoodally, M.F.; Ferri, N.; Biancorosso, N.; et al. Himalayan Nettle Girardinia diversifolia as a Candidate Ingredient for Pharmaceutical and Nutraceutical Applications—Phytochemical Analysis and In Vitro Bioassays. Molecules 2020, 25, 1563. [Google Scholar] [CrossRef]
- Biswas, K.R.; Khan, T.; Monalisa, M.N.; Swarna, A.; Ishika, T.; Rahman, M. Medicinal plants used by folk medicinal practitioners of four adjoining villages of Narail and Jessore Districts, Bangladesh. Am. Eurasian J. Sustain. Agric. 2011, 5, 23–33. [Google Scholar]
- Pattanayak, P.; Behera, P.; Das, D.; Panda, S.K. Ocimum sanctum Linn. A reservoir plant for therapeutic applications: An overview. Pharmacogn. Rev. 2010, 4, 95. [Google Scholar] [CrossRef] [PubMed]
- Scartezzini, P.; Speroni, E. Review on some plants of Indian traditional medicine with antioxidant activity. J. Ethnopharmacol. 2000, 71, 23–43. [Google Scholar] [CrossRef]
- Pitipanapong, J.; Chitprasert, S.; Goto, M.; Jiratchariyakul, W.; Sasaki, M.; Shotipruk, A. New approach for extraction of charantin from Momordicacharantia with pressurized liquid extraction. Sep. Purif. Technol. 2007, 52, 416–422. [Google Scholar] [CrossRef]
- Omoya, F.O.; Akharaiyi, F.C. Mixture of honey and ginger extract for antibacterial assessment on some clinical isolates. Int. J. Pharm. Biomed. Res. 2011, 2, 39–47. [Google Scholar]
- Montalván, V.; Gallo, M.; Rojas, E. A 25 years-old woman with a postvaccine thalamic pseudotumoral lesion. Rev. Clin. Esp. 2015, 215, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Priya, G.; Parminder, N.; Jaspreet, S. Antimicrobial and antioxidant activity on Emblica officinalis seed extract. Int. J. Res. Ayurveda Pharm. 2012, 3, 591–596. [Google Scholar]
- Mahata, S.; Pandey, A.; Shukla, S.; Tyagi, A.; Husain, S.A.; Das, B.C.; Bharti, A.C. Anticancer Activity of Phyllanthus emblica Linn. (Indian Gooseberry): Inhibition of Transcription Factor AP-1 and HPV Gene Expression in Cervical Cancer Cells. Nutr. Cancer 2013, 65, 88–97. [Google Scholar] [CrossRef]
- Parvu, M.; Moţ, C.A.; Parvu, A.E.; Mircea, C.; Stoeber, L.; Rosca-Casian, O.; Ţigu, A.B. Allium sativum extract chemical composition, antioxidant activity and antifungal effect against Meyerozymaguillier mondii and Rhodotorula mucilaginosa causing onychomycosis. Molecules 2019, 24, 3958. [Google Scholar] [CrossRef] [PubMed]
- Mahata, S.; Maru, S.; Shukla, S.; Pandey, A.; Mugesh, G.; Das, B.C.; Bharti, A.C. Anticancer property of Bryophyllum pinnata (Lam.) Oken. leaf on human cervical cancer cells. BMC Complement. Altern. Med. 2012, 12, 15. [Google Scholar] [CrossRef]
- Satyal, P.; Paudel, P.; Raut, J.; Deo, A.; Dosoky, N.S.; Setzer, W.N. Volatile constitu-ents of Pinus roxburghii from Nepal. Pharmacogn. Res. 2013, 5, 43–48. [Google Scholar]
- Lutterodt, H.; Luther, M.; Slavin, M.; Yin, J.J.; Parry, J.; Gao, J.-M.; Yu, L. Fatty acid profile, thymoquinone content, oxidative stability, and antioxidant properties of cold-pressed black cumin seed oils. Food Sci. Technol. 2010, 43, 1409–1413. [Google Scholar]
- Ali, A.A.; Al-Rahwi, K.; Lindequist, U. Some medicinal plants used in Yemeni herbal medicine to treat malaria. Afr. J. Tradit. Complementary Altern. Med. 2004, 1, 72–76. [Google Scholar] [CrossRef]
- Desai, S.N.; Patel, D.K.; Devkar, R.V.; Patel, P.V.; Ramachandran, A.V. Hepatoprotective potential of polyphenol rich extract of Murrayakoenigii, L.: An in vivo study. Food Chem. Toxicol. 2012, 50, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Mahipal, P.; Pawar, R.S. Nephroprotective effect of Murraya koenigii on cyclophosphamide induced nephrotoxicity in rats. Asian Pac. J. Trop. Med. 2017, 10, 808–812. [Google Scholar] [CrossRef]
- Defillipo, P.P.; Raposo, A.H.; Fedoce, A.G.; Ferreira, A.S.; Polonini, H.C.; Gattaz, W.F.; Raposo, N.R. Inhibition of cPLA2 and sPLA2 activities in primary cultures of rat cortical neurons by Centella asiatica water extract. Nat. Prod. Commun. 2012, 7, 841–843. [Google Scholar] [CrossRef]
- Yamasaki, S.; Nakashima, R.; Sakurai, K.; Baucheron, S.; Giraud, E.; Doublet, B.; Cloeckaert, A.; Nishino, K. Crystal structure of the multidrug resistance regulator RamR complexed with bile acids. Sci. Rep. 2019, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rosell, R.; Crinó, L. Pemetrexed combination therapy in the treatment of non–small cell lung cancer. Semin. Oncol. 2002, 29, 23–29. [Google Scholar]
- Banerjee, P.; Eckert, A.O.; Schrey, A.K.; Preissner, R. ProTox-II: A webserver for the prediction of toxicity of chemicals. Nucleic Acids Res. 2018, 46, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Rolta, R.; Yadav, R.; Salaria, D.; Trivedi, S.; Imran, M.; Sourirajan, A.; Baumler, D.J.; Dev, K. In silico screening of hundred phytocompounds of ten medicinal plants as potential inhibitors of nucleocapsid phosphoprotein of COVID-19: An approach to prevent virus assembly. J. Biomol. Struct. Dyn. 2020, 1–8. [Google Scholar] [CrossRef]
- Rolta, R.; Salaria, D.; Kumar, V.; Sourirajan, A.; Dev, K. Phytocompounds of Rheum emodi, Thymus serpyllum and Artemisia annua inhibit COVID-19 binding to ACE2 receptor: In silico approach. Curr. Pharmacol. Rep. 2021, 7, 135–149. [Google Scholar] [CrossRef]
- Salaria, D.; Rolta, R.; Sharma, N.; Dev, K.; Sourirajan, A.; Kumar, V. In silico and In vitro evaluation of the anti-inflammatory and antioxidant potential of Cymbopogon citratus from North-western Himalayas. BioRxiv 2020. [Google Scholar] [CrossRef]
- Cheng, F.; Li, W.; Zhou, Y.; Shen, J.; Wu, Z.; Liu, G.; Lee, P.W.; Tang, Y. AdmetSAR: A comprehensive source and free tool for assessment of chemical ADMET properties. J. Chem. Inf. Model. 2012, 52, 3099–3105. [Google Scholar] [CrossRef]
- Yang, H.; Lou, C.; Sun, L.; Li, J.; Cai, Y.; Wang, Z.; Tang, Y. AdmetSAR 2.0: Web-service for prediction and optimization of chemical ADMET properties. Bioinformatics 2019, 35, 1067–1069. [Google Scholar]
- Schrodinger, S. Release 2020-1: Protein Preparation Wizard; Epik, LLC: New York, NY, USA; Impact, Schrödinger, LLC: New York, NY, USA; Prime, Schrodinger, LLC: New York, NY, USA, 2020. [Google Scholar]
- Kennedy, T. Managing the drug discovery/development interface. Drug Discov. Today 1997, 2, 436–444. [Google Scholar] [CrossRef]
- Kala, C.P. Ethnomedicinal botany of the Apatani in the eastern Himalayan region of India. J. Ethnobiol. Ethnomed. 2005, 1, 11–18. [Google Scholar] [CrossRef]
- World Health Organization: Drug-Resistant Salmonella. 2016. Available online: http://www.who.int/mediacentre/factsheets/fs139/en/ (accessed on 15 May 2021).
- Koronakis, V.; Sharff, A.; Koronakis, E.; Luisi, B.; Hughes, C. Crystal structure of the bacterial membrane protein TolC central to multidrug efflux and protein export. Nature 2000, 405, 914–919. [Google Scholar] [CrossRef]
- Nikaido, H. Multidrug efflux pumps of gram-negative bacteria. J. Bacteriol. 1996, 178, 5853–5859. [Google Scholar] [CrossRef]
- Nakae, T.; Saito, K.; Nakajima, A. Effect of sulbactam on anti-pseudomonal activity of beta-lactam antibiotics in cells producing various levels of the MexAB-OprM efflux pump and beta-lactamase. Microbiol. Immunol. 2000, 44, 997–1001. [Google Scholar] [CrossRef]
- Mehta, J.; Jandaik, S.U. Evaluation of phytochemicals and synergistic interaction between plant extracts and antibiotics for efflux pump inhibitory activity against salmonella enterica serovar typhimurium strains. Int. J. Pharm. Pharm. Sci. 2016, 8, 217–223. [Google Scholar] [CrossRef]
- Jandaik, S.U.; Mehta, J.; Mohan, M. Synergistic and efflux pump inhibitory activity of plant extracts and antibiotics on staphylococcus aureus strains. Asian J. Pharm. Clin. Res. 2016, 9, 277–282. [Google Scholar]
- Mehta, J.; Rolta, R.; Dev, K. Role of medicinal plants from Northwestern Himalayas as an efflux pump inhibitor against MDR AcrAB-TolC Salmonella enterica serovar typhimurium: In vitro and In silico studies. J. Ethanopharmacol. 2021, 114589. [Google Scholar] [CrossRef] [PubMed]
- Luhata, L.P.; Usuki, T. Antibacterial activity of β-sitosterol isolated from the leaves of Odontonema strictum (Acanthaceae). Bioorg. Med. Chem. Lett. 2021, 48, 128248. [Google Scholar] [CrossRef]
- Sen, A.; Dhavan, P.; Shukla, K.K.; Singh, S.; Tejovathi, G. Analysis of IR, NMR and antimicrobial activity of β-sitosterol isolated from Momordica charantia. Sci. Secur. J. Biotechnol. 2012, 1, 9–13. [Google Scholar]
- Rolta, R.; Salaria, D.; Kumar, V.; Patel, C.N.; Sourirajan, A.; Baumler, D.J.; Dev, K. Molecular docking studies of phytocompounds of Rheum emodi Wall with proteins responsible for antibiotic resistance in bacterial and fungal pathogens: In silico approach to enhance the bio-availability of antibiotics. J. Biomol. Struct. Dyn. 2020, 1–5. [Google Scholar] [CrossRef]
- Salaria, D.; Rolta, R.; Patel, C.N.; Dev, K.; Saurirajan, A.; Kumar, V. In vitro and in silico analysis of Thymus serpyllum essential oil as bioactivity enhancer of antibacterial and antifungal agents. J. Biomol. Struct. Dyn. 2021, 1–20. [Google Scholar] [CrossRef]
- Li, W.; Shen, J.; Liu, G.; Tang, Y.; Hoshino, T. Exploring coumarin egress channels in human cytochrome p450 2a6 by random acceleration and steered molecular dynamics simulations. Proteins 2011, 79, 271–281. [Google Scholar] [CrossRef] [PubMed]
| S. No. | Phytocompounds | Botanical Names (Family) | Common/Local Name | Ailments |
|---|---|---|---|---|
| 1. | (Z)-Ligustilide | Angelica glauca Edgew. (Apiaceae) | Chora | Stimulant, appetizer, arthritis, carminative, diaphoretic, diuretic, constipation, debility, joint problems, bronchitis, dysentery, menorrhea, stomach disorders, vomiting [17,18]. |
| Angelicide | ||||
| 2. | P-coumaric acid | Heracleum lanatum Michx (Apiaceae) | Patrala | Fever, abdominal cramps, leukoderma, aphrodisiac, digestive, mildly expectorant and sedative, nausea, tumor [19]. |
| Scopoletin | ||||
| 3. | Palmatine | Berberis aristata DC. (Berberidaceae) | Kashmal | Acidity, eye infection, microbes, fever, hepatotoxic, hyperglycemic, lipidemic, cancer, oxidative stress diarrhea, hemorrhoids, osteoporosis, HIV-AIDS, diabetes, jaundice, wound healing [20]. |
| Rutin | ||||
| 4. | Podophyllotoxin | Sinopodophyllum hexandrum (Royle) T.S. Ying (Berberidaceae) | Bankakdi | Cancer, snakebite, jaundice, stomachache, intestinal purgative, vomiting, necrotic wounds, tumor, arthritis [21,22]. |
| Quercetin | ||||
| 5. | Astragalin | Chenopodium album L. (Amaranthaceae) | Baathu | Parasitic worms, inflammation, fever, arthritis, constipation, toothache, bug bites, sunstroke, tooth decay [21]. |
| Kaempferol | ||||
| 6. | Apigenin | Sedum glaucophyllum R.T. Clausen (Crassulaceae) | Mochu-gha, ludru | Burn, cut, abscesses, blisters [23]. |
| Luteolin | ||||
| 7. | Phytol | Solena amplexicaulis (Lam.) Gandhi (Cucurbitaceae) | Kakdi | Cancer, oxidative stress, inflammation, tumor, antimicrobial, diuretic, fever, jaundice [24]. |
| Carane | ||||
| 8. | Hydroxytyrosol | Malva neglecta Wall (Malvaceae) | Sonchal | Constipation, women sterility, wound healing, hemorrhoids, asthma, diarrhea, rheumatic pain, stomachache, abdominal pain, renal diseases, throat infection, common cold, stomachache, antimicrobial, oxidative stress, inflammation, stress, liver damage, ulcer, cancer, bronchitis, kidney stone [25,26]. |
| Hexatriacontane | ||||
| 9. | Cyanidin | Ficus carica L. (Moraceae) | Common fig | Oxidative stress, Cancer, colic, indigestion, loss of appetite, diarrhea, sore throats, coughs, bronchial problems, heart disease, liver problem, lowering of blood sugar, cholesterol-lowering, inflammation, Antimicrobial, relieve spasm of involuntary muscle, fever, TB, platelet aggregation inhibitor, mutagen [27,28]. |
| Psoralen | ||||
| 10. | Militarine | Dactylorhiza hatagirea (D.Don) Soo (Orchidaceae) | Panja, Salampanja | Wound healing, inflammation, bleeding, fever, cancer, diabetes, neurological function, burns, and bronchitis [29,30]. |
| Resveratrol | ||||
| 11. | Gallic acid | Rheum australe D.Don (Polygonaceae) | Chuchi, Chukari | Diabetes, inflammation, oxidative stress, cancer, gastric disorder, cuts & wounds, fractured bones, liver damage, immune-enhancing, lower blood glucose, smallpox, muscle sprain [31,32]. |
| Rhein | ||||
| 12. | Nepodin | Rumex hastatus D.Don (Polygonaceae) | Almoru | Jaundice, hepatitis, Blood purification, Scurvy, Diuretic, cooling, astringent, constipation, oxidative stress, snakebites, foot and mouth infections, asthma, cough, headache, diarrhea, dysentery, fever, weakness, and scabies [33]. |
| Rumexoside | ||||
| 13. | Kutkoside | Picrorrhizakurooa Royle (Plantaginaceae) | Karu | Liver damage, oxidative stress, cancer, asthma, stimulate immune system, neuritogenic, neuron degeneration, jaundice, allergy, piles, leukoderma, snake bite, liver disease, fever, parasitic worms, improving heart muscle contraction, high blood pressure, diabetes, cold, cough, stomach ache [34]. |
| Picroside III | ||||
| 14. | Aloesin | Rumex nepalensis Meisn (Polygonaceae) | Nepal dock | Purgative, oxidative stress, fever, inflammation, tumor, diabetic, mental disorder, Wound healing, analgesic and CNS depressant, skeletal muscle relaxant [35]. |
| Orcinol glucoside | ||||
| 15. | Catechin | Rubus ellipticus Sm. (Rosaceae) | Akhe, Yellow Himalayan raspberry | Dysentery, oxidative stress, diabetes, tumor, Nephroprotective, sore throats, cold, colic, constipation, gastritis, dysentery, diarrhea [36]. |
| Caffeic acid | ||||
| 16. | Rubiadin | Rubia cordifolia L. (Rubiaceae) | Mishtu | Immune-related diseases inflammation, urinary infections, bone ache, skin diseases, vertigo, insomnia, rheumatism, tuberculosis, hematemesis, menstrual disorders, contusions [37]. |
| Mollugin | ||||
| 17. | Verbascoside | Verbascum thapsus L. (Scrophulariaceae) | Janglitamaku | Pain, muscle spasm, bleeding, nerve tonic, wounds, allergy, cancer, oxidative stress, blood pressure, anxiety, inflammation, sepsis, diuretic, cough, skin diseases, cuts, wounds and swelling, diarrhea [38,39]. |
| Aucubin | ||||
| 18. | Solasonine | Solanum americanum Mill. (Solanaceae) | Bara lianchu | Healing, dental caries, bladder spasm, joint pains, cooling, cough, gastric ulcer, protozoal infections, diabetes, inflammation [40,41]. |
| Solamargine | ||||
| 19. | Pennogenin | Trilliumgovanianum Wall. Ex D. Don (Melanthiaceae) | Nag Chhatri | Dysentery, wounds, inflammation, antiseptic, boils, menstrual and sexual disorders, pain, inflammation, Leishmanial infection, cancer, wound [42,43]. |
| 2,4-Decadienal | ||||
| 20. | Protocatechuic acid | Valeriana jatamansi Jones (Caprifoliaceae) | Nihani | Cuts, wounds, skin disorders, analgesic, anxiety disorder, tranquilizing hypnotic, irritable bowel syndrome, epilepsy, snake poisoning, hyperlipidemia, depressive insomnia, rotavirus enteritis [44,45]. |
| Valtrate | ||||
| 21. | Methyl salicylate | Viola canescens Wall. (Violaceae) | Banksha | Cough, cold, fever, jaundice, malaria, protozoa infection, cancer, flatulence, inflammation or irritation, bleeding abrations, fever, respiratory problems, sepsis, fever [46,47]. |
| Emetine | ||||
| 22. | β-sitosterol | Girardinia diversifolia (Link) Friis (Urticaceae) | Zaran | Cytotoxic, Snake bite, Muscles sprain, constipation, headaches, fever, ringworm, gastric troubles, eczema, chest and joint pain, rheumatism, tuberculosis, headache, joint aches, diabetes, asthma, stomach inflammation, gonorrhea, delivery problems, bone fracture, internal injury, blood purification [48,49,50]. |
| Scopoletin | ||||
| 23. | Atropine | Datura stramonium L. (Solanaceae) | Dhatura | Asthma, inflammation, pain and spasm in irritable bowel, gout, madness, epilepsy, depression, burns, rheumatism Parkinson’s disease, piles, pain [51]. |
| Scopolamine | ||||
| 24. | Eugenol | Ocimum sanctum L. (Labiatae) | Tulsi | Bronchial asthma, fever, cold, cough, malaria, dysentery, convulsions, diarrhea, arthritis, skin diseases, insect bites, gastric, liver and heart disorder, diabetes stomachache, headache, inflammation, tuberculosis, stress, poisoning, leukoderma [52]. |
| Cirsilineol | ||||
| 25. | Charantin | Momordica charantia L. (Cucurbitaceae) | Bitter Gourd | Cholesterol, HIV, gout, jaundice, abdominal pain, kidney (stone), rheumatism, fever, scabies, ulcer, inflammation, leukemia, diabetes, tumor, diabetes [53,54]. |
| Momordicine | ||||
| 26. | Gingerol | Zingiber officinale Roscoe (Zingiberaceae) | Ginger | Inflammation, nausea, analgesic, fever, dysentery, heartburn, flatulence, diarrhea, diabetes, carminative, stimulant to GIT, relieve spasm of involuntary muscle, digestion, vasodilation, cough, asthma, pain, flatulence, constipation [55]. |
| Lariciresinol | ||||
| 27. | Withanone | Withania somnifera (L.) Dunal (Solanaceae) | Ashwagandha | Abortion, clear or open the natural ducts of the fluids and secretions, pain, promoting calm and sleep, miscarriage, post-partum difficulties, inflammation, tumor, stress, oxidative stress, mind-booster, rejuvenation [56]. |
| Withaferin A | ||||
| 28. | Geraniin | Phyllanthus emblica L. (Phyllanthaceae) | Indian gooseberry | Tumor, pain, fever, stress, inflammation, oxidative stress, depression, liver damage, ulcer, radioprotective, diabetes, cancer, wound healing, cytotoxic [57,58]. |
| Phyllanthin | ||||
| 29. | Allicin | Allium sativum L. (Amaryllidaceae) | Garlic | Cold, influenza, dyspepsia, loss of appetite, snake bites, stress, inflammation, diabetes, aging effects, cancer, lung disorders, whooping cough, stomach disorders, cold, earache, cardiovascular disorder, Alzheimer’s disease [59]. |
| Pyrogallol | ||||
| 30. | Quercitrin | Bryophyllum pinnatum (Lam.) Oken (Crassulaceae) | Pattharcaṭṭa | Ulcer, inflammation, analgesic, jaundice, kidney stones, respiratory tract infections, boils, insect bites, hypertension, diabetes, cancer, HPV [60]. |
| Bryophyllin A | ||||
| 31. | Alpha-pinene | Pinus roxburghii Sarg. (Pinaceae) | Chir pine | Dyslipidemia, oxidative stress, wound healing, analgesic, inflammation, cytotoxic [61]. |
| Abietic acid | ||||
| 32. | Thymoquinone | Nigella sativa L. (Ranunculaceae) | Black cumin | Asthma, hypertension, diabetes, inflammation, cough, bronchitis, headache, eczema, fever, dizziness, influenza, carminative, stimulant, diuretic [62]. |
| Thymol | ||||
| 33. | Aloe-emodin | Aloe barbadensis Miller (Asphodelaceae) | (Aloe vera ) | Burn injury, eczema, cosmetics, inflammation, fever, malaria [63]. |
| Emodin | ||||
| 34. | Koenimbine | Murraya koenigii (L.) Spreng. (Rutaceae) | Curry tree | Piles, inflammation, itching, fresh cuts, dysentery, bruises, and edema, helminth infection, analgesics, digestives, and appetizers, oxidative stress, inflammation, nephroprotective [64,65]. |
| Mahanimbine | ||||
| 35. | Asiaticoside | Centella asiatica (L.) Urb. (Apiaceae) | Brahma manduki | Ulcerous skin, weakness, burns, duodenal, stomach ulcers, lupus, antinociceptive, inflammation, scleroderma, leprosy vein disorder, neuroprotection, wound healing, eczema, dermatitis, psoriasis [66]. |
| Madecassoside |
| Name of Compound | Plant Source | Binding Energy (KJ/Mol) | No. of Hydrogen Bonds | Hydrogen Bonds | Interactive Amino Acids |
|---|---|---|---|---|---|
| Asiaticoside | Centella asiatica (L.) Urb. | −10.9 | 6 | Ser137, Glu113, Leu115, Asp152, Ala110, Arg148 | Ile106, Tyr59, Lys63, Asp124, Glu120, Ala149, Lys114, Ser112, Val111, Lys117, Cys134, Leu130, Arg136, Thr85, Ile88, Met70, Leu139, Phe155, Leu66, Tyr92, Leu156, Met140 |
| Madecassoside | Centella asiatica (L.) Urb. | −9.7 | 5 | Tyr59, Asp124, Ala110, Ala123, Cys67 | Trp95, Leu66, Phe155, Thr85, Met70, Tyr92, Ser137, Leu139, Arg136, Leu130, Leu156, Ile88, Phe127, Lys63, Arg131, Pro128, Leu115, Asp152, Val11, Ala149, Glu120, Arg148, Met140, Ile106 |
| Beta-sitosterol | Girardinia diversifolia (Link) Friis | −9.1 | 2 | Thr85, Ser137 | Tyr59, Ile106, Ala110, Asp152, Met140, Arg148, Leu139, Arg136, Val138, Ala81, Ile88, Leu156, Met70, Tyr92, Phe155, Leu66, Lys63 |
| Bryophyllin A | Bryophyllum pinnatum (Lam.) Oken | −10.6 | 2 | Thr85, Cys67 | Phe155, Arg148, Met140, Cys134, Ile88, Leu139, Ser137, Arg136, Ala81, Met84, Lys63, Leu66, Met70, Ile106, Tyr59, Leu156, Ala110, Asp152 |
| Mahanimbine | Murraya koenigii (L.) Spreng | −9.4 | - | - | Arg136, Ser137, Thr85, Cys67, Tyr59, Ile106, Ala110, Leu156, Lys63, Tyr92, Leu66, Phe155, Met70, Ile88, Leu139, Leu130 |
| Pennogenin | Trilliumgovanianum Wall. Ex D.Don | −10.3 | 1 | Arg148 | Cys134, Met84, Ile88, Met70, Tyr92, Arg107, Phe155, Ile106, Leu156, Ala110, Leu66, Lys63, Met140, Tyr59, Leu139, Ser137, Arg136, Thr85, Ala81 |
| Rutin | Berberis aristata DC. | −9.2 | 3 | Ser137, Thr85, Tyr59 | Cys134, Met84, Glu120, Asp152, Arg148, Ala110, Leu156, Ala123, Asp124, Tyr92, Leu66, Phe155, Met70, Lys63, Cys67, Phe127, Arg136, Leu130, Ile88, Leu139 |
| Solasonine | Solanum americanum Mill. | −9.7 | 2 | Arg148, Ser137 | Glu146, Asp145, Lys117, Glu120, Met70, Tyr92, Leu66, Phe155, Asp152, Met140, Arg136, Leu139, Leu130, Lys68, Ile88, Arg131, Asp124, Ala149 |
| Solamargine | Solanum americanum Mill. | −9.5 | 5 | Arg131, Lys63, Asp124, Asp145, Arg148 | Phe127, Ala123, Leu130, Arg136, Glu120, Lys117, Tyr59, Leu139, Ser137, Met140, Thr85, Ile88 |
| Withaferin A | Withania somnifera (L.) Dunal | −10.2 | 2 | Tyr59, Tyr92 | Ile106, Ala110, Leu66, Lys63, Phe155, Arg148, Leu139, Val138, Thr85, Trp185, Ser137, Met84, Cys134, Arg136, Ile88, Leu130, Met140, Leu156 |
| Withanone | Withania somnifera (L.) Dunal | −9.3 | - | - | Ile106, Leu66, Lys63, Arg148, Tyr92, Met70, Leu130, Arg136, Ile88, Cys134, Thr85, Met84, Ser137, Leu139, Met140, Phe155, Asp152, Ala110, Leu156, Tyr59 |
| Chenodeoxycholic acid | Bile component | −10.8 | 4 | Ser137, Thr85, Asp152, Tyr59 | Val138, Cys134, Met84, Leu139, Ile88, Arg148, Met140, Phe155, Leu156, Ile106, Ala110, Lys63, Tyr92, Leu66, Met70, Arg136 |
| Phytocompounds | miLogP | TPSA | MW | nON | nOHNH | Nviolations |
|---|---|---|---|---|---|---|
| Chenodeoxycholic acid | 4.25 | 77.75 | 392.28 | 4 | 3 | 0 |
| Asiaticoside | 0.37 | 315.21 | 959.13 | 19 | 12 | 3 |
| Beta-sitosterol | 8.62 | 20.23 | 414.72 | 1 | 1 | 1 |
| Bryophyllin A | 2.09 | 115.44 | 472.53 | 8 | 2 | 0 |
| Madecassoside | −0.55 | 335.44 | 975.13 | 20 | 13 | 3 |
| Mahanimbine | 7.10 | 25.02 | 331.46 | 2 | 1 | 1 |
| Pennogenin | 4.99 | 58.92 | 430.63 | 4 | 2 | 0 |
| Rutin | −1.06 | 269.43 | 610.52 | 16 | 10 | 3 |
| Solasonine | 1.40 | 258.72 | 884.07 | 17 | 10 | 3 |
| Solamargine | 2.41 | 238.49 | 868.07 | 16 | 9 | 3 |
| Withaferin A | 3.86 | 96.36 | 470.61 | 6 | 2 | 0 |
| Withanone | 4.15 | 96.36 | 470.61 | 6 | 2 | 0 |
| Phytocompounds | ProTox-II | |||||
|---|---|---|---|---|---|---|
| LD50(mg/kg) | Hepato-Toxicity | Carcino-Genecity | Immuno Toxicity | Muta-Genicity | Cyto-Toxicity | |
| Chenodeoxycholic acid | 2000 (Class 4) | Active | Inactive | Inactive | Inactive | Inactive |
| Asiaticoside | 4000 (Class 5) | Inactive | Inactive | Active | Inactive | Inactive |
| Beta-sitosterol | 890 (Class 4) | Inactive | Inactive | Active | Inactive | Inactive |
| Bryophyllin A | 31 (Class 2) | Inactive | Inactive | Active | Inactive | Active |
| Madecassoside | 1190 (Class 4) | Active | Inactive | Active | Inactive | Inactive |
| Mahanimbine | 4000 (Class 5) | Inactive | Inactive | Active | Inactive | Inactive |
| Pennogenin | 1190 (Class 4) | Active | Inactive | Active | Inactive | Inactive |
| Rutin | 1190 (Class 4) | Active | Inactive | Active | Inactive | Active |
| Solasonine | 500 (Class4) | Inactive | Inactive | Active | Inactive | Active |
| Solamargine | 1190 (Class 4) | Inactive | Inactive | Active | Inactive | Active |
| Withaferin A | 300 (Class 3) | Inactive | Inactive | Active | Inactive | Active |
| Withanone | 7 (Class 2) | Inactive | Inactive | Active | Inactive | Active |
| Title | MMGBSA (kcal/mol) |
|---|---|
| Frame 1 | −105.8395994 |
| Frame 2 | −122.4871042 |
| Frame 3 | −131.2524436 |
| Frame 4 | −113.052146 |
| Frame 5 | −139.4301793 |
| Frame 6 | −154.7243297 |
| Frame 7 | −149.2144921 |
| Frame 8 | −157.1657804 |
| Frame 9 | −164.8064715 |
| Frame 10 | −148.5722473 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mehta, J.; Rolta, R.; Salaria, D.; Awofisayo, O.; Fadare, O.A.; Sharma, P.P.; Rathi, B.; Chopra, A.; Kaushik, N.; Choi, E.H.; et al. Phytocompounds from Himalayan Medicinal Plants as Potential Drugs to Treat Multidrug-Resistant Salmonella typhimurium: An In Silico Approach. Biomedicines 2021, 9, 1402. https://doi.org/10.3390/biomedicines9101402
Mehta J, Rolta R, Salaria D, Awofisayo O, Fadare OA, Sharma PP, Rathi B, Chopra A, Kaushik N, Choi EH, et al. Phytocompounds from Himalayan Medicinal Plants as Potential Drugs to Treat Multidrug-Resistant Salmonella typhimurium: An In Silico Approach. Biomedicines. 2021; 9(10):1402. https://doi.org/10.3390/biomedicines9101402
Chicago/Turabian StyleMehta, Jyoti, Rajan Rolta, Deeksha Salaria, Oladoja Awofisayo, Olatomide A. Fadare, Prem Prakash Sharma, Brijesh Rathi, Adity Chopra, Neha Kaushik, Eun Ha Choi, and et al. 2021. "Phytocompounds from Himalayan Medicinal Plants as Potential Drugs to Treat Multidrug-Resistant Salmonella typhimurium: An In Silico Approach" Biomedicines 9, no. 10: 1402. https://doi.org/10.3390/biomedicines9101402
APA StyleMehta, J., Rolta, R., Salaria, D., Awofisayo, O., Fadare, O. A., Sharma, P. P., Rathi, B., Chopra, A., Kaushik, N., Choi, E. H., & Kaushik, N. K. (2021). Phytocompounds from Himalayan Medicinal Plants as Potential Drugs to Treat Multidrug-Resistant Salmonella typhimurium: An In Silico Approach. Biomedicines, 9(10), 1402. https://doi.org/10.3390/biomedicines9101402









