Analysis of Clinical Features in Children with Vasovagal Syncope Complicated by Convulsions or Incontinence
Abstract
1. Introduction
2. Materials and Methods
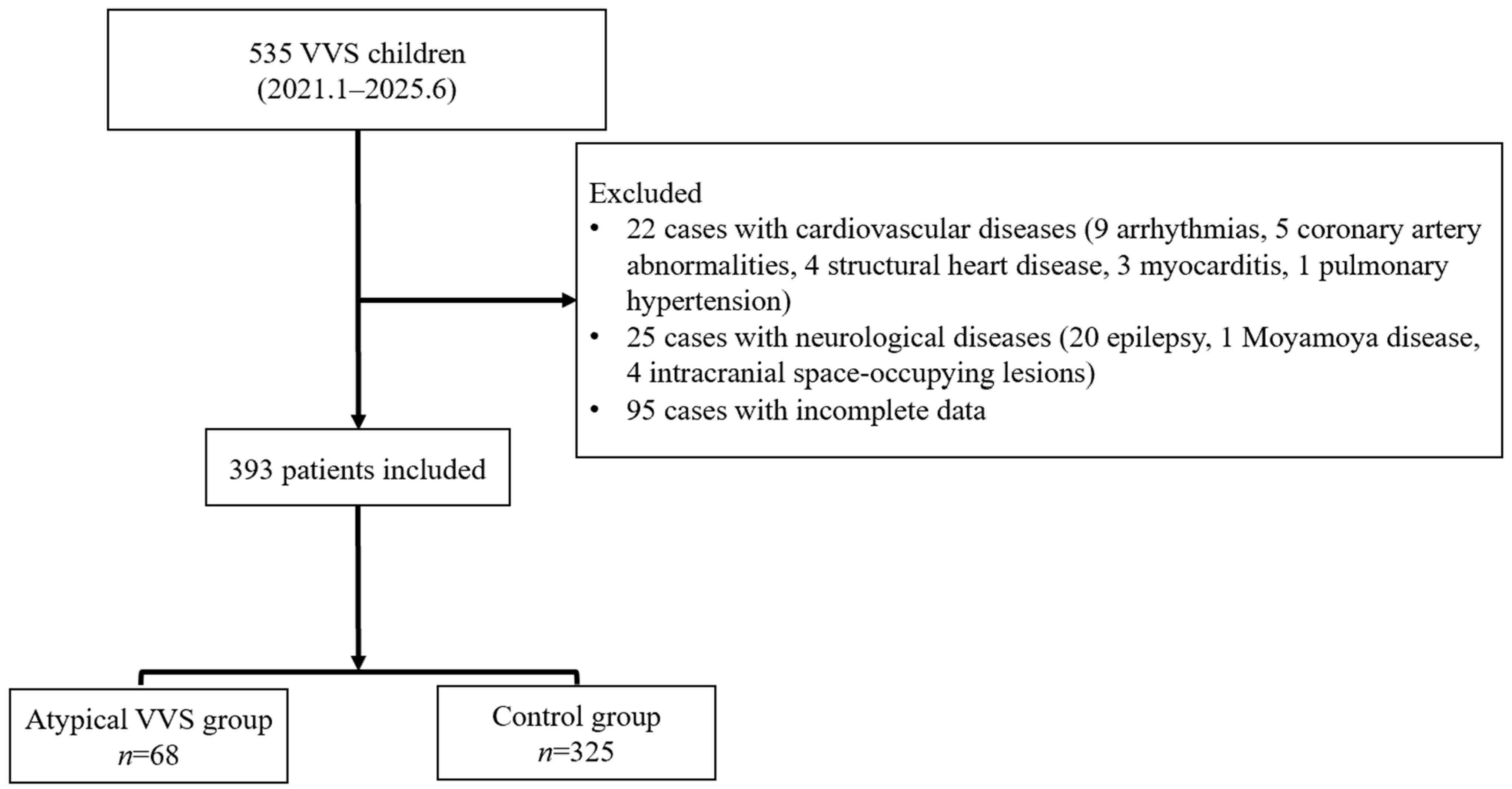
2.1. Study Participants
2.1.1. Inclusion Criteria for VVS
2.1.2. Exclusion Criteria for Other Etiologies
2.2. Study Methods
2.3. Statistical Analysis
3. Results
3.1. Decreased BMI in Atypical VVS Pediatric Cases Versus the Control Group
3.2. Children with Atypical VVS Have a Higher Proportion of Syncope-Related Trauma and More Frequent Central Triggers
3.3. Heart Rate Variability and Hemodynamic Characteristics in Children with Atypical VVS
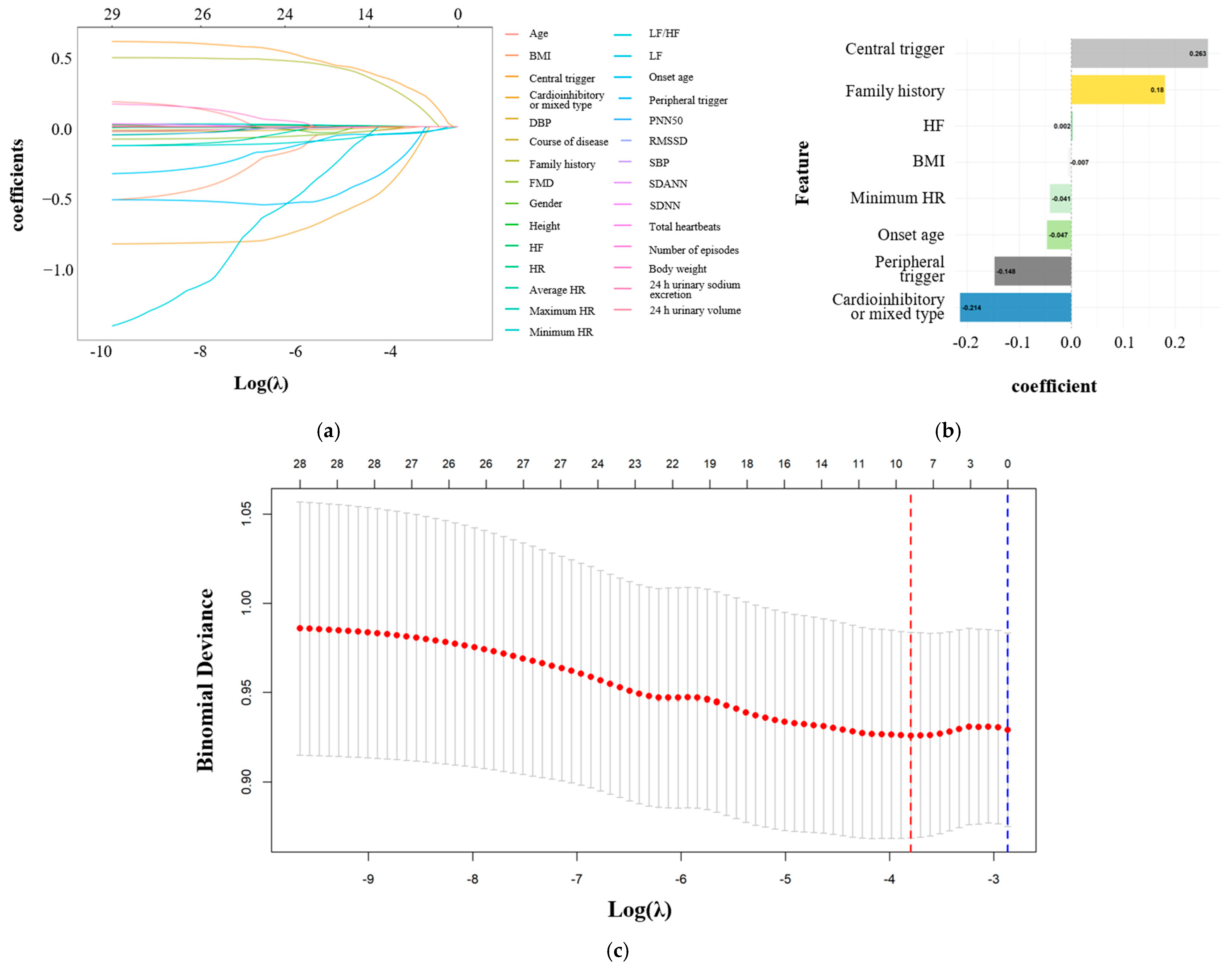
3.4. Age at the First Episode and Minimal Heart Rate as Independent Correlates of Atypical VVS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| DBP | Diastolic blood pressure |
| FMD | Flow-mediated vasodilation |
| HF | High frequency |
| HR | Heart rate |
| HRV | Heart rate variability |
| HUTT | Head-up tilt test |
| LF | Low frequency |
| pNN50 | Percentage of adjacent normal-to-normal interval differences greater than 50 ms |
| rMSSD | Root mean square of successive differences between adjacent normal cycles |
| SBP | Systolic blood pressure |
| SDANN | Standard deviation of the 5 min average normal-to-normal intervals |
| SDNN | Standard deviation of all normal-to-normal intervals |
| VIF | Variance inflation factor |
| VVS | Vasovagal syncope |
References
- Carino Mason, M.R.; Vu, L.; Horn, D.; Tiu, T. Convulsive syncope as a complication of outpatient procedures: A case series and review of the literature. Clin. J. Sport Med. 2024, 34, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, A.Z.; Blackmore, D.; Siddiqi, Z.A. “Complex” vasovagal syncope: A zebra among horses. Front. Neurol. 2020, 11, 550982. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Zhang, C.; Du, J.; Jin, H.; Liao, Y. Features of clinical manifestations and heart rate variability in children with malignant vasovagal syncope. Children 2025, 12, 636. [Google Scholar] [CrossRef] [PubMed]
- Vaksmann, G.; Bouzguenda, I.; Lamblin, M.D. The slow-flat-slow sequence in malignant vasovagal syncope. Ann. Pediatr. Cardiol. 2021, 14, 128–129. [Google Scholar] [CrossRef]
- Hussong, J.; Greiner, M.; Schiedermaier, U.; Mattheus, H.; von Gontard, A. Anxiety disorders, depression and incontinence in preschool children-A population-based study. Neurourol. Urodyn. 2022, 41, 1800–1808. [Google Scholar] [CrossRef]
- Wang, C.; Du, J.; Li, Y.; Liao, Y.; Tian, H.; Huang, M.; Dong, X.; Shi, L.; Sun, J.; Jin, H. 2018 Chinese Pediatric Cardiology Society (CPCS) guideline for diagnosis and treatment of syncope in children and adolescents. Sci. Bull. 2018, 63, 1558–1564. [Google Scholar] [CrossRef]
- Šišáková, M.; Helánová, K.; Hnatkova, K.; Andršová, I.; Novotný, T.; Malik, M. Speed of heart rate changes during postural provocations in children and adolescents. Sci. Rep. 2024, 14, 11938. [Google Scholar] [CrossRef]
- Shvartz, V.; Danilov, V.; Koroleva, S.; Shvartz, E.; Donakanyan, S.; Permyakov, V.; Erastova, N.; Golukhova, E. “Become a Champion” Trial Investigators. Reference ranges of gender- and age-related heart rate variability parameters in Russian children. Sci. Rep. 2025, 15, 5274. [Google Scholar] [CrossRef]
- Zhang, Q.; Jin, H.; Qi, J.; Yan, H.; Du, J. Diagnostic value of serum brain natriuretic peptide in syncope in children and adolescents. Acta Paediatr. 2013, 102, e210–e214. [Google Scholar] [CrossRef]
- Jardine, D.L.; Wieling, W.; Brignole, M.; Lenders, J.W.M.; Sutton, R.; Stewart, J. The pathophysiology of the vasovagal response. Heart Rhythm 2018, 15, 921–929. [Google Scholar] [CrossRef]
- Xu, W.R.; Jin, H.F.; Du, J.B.; Liao, Y. Malignant vasovagal syncope in children. World J. Pediatr. 2025, 21, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Morillo, C.A.; Eckberg, D.L.; Ellenbogen, K.A.; Beightol, L.A.; Hoag, J.B.; Tahvanainen, K.U.; Kuusela, T.A.; Diedrich, A.M. Vagal and sympathetic mechanisms in patients with orthostatic vasovagal syncope. Circulation 1997, 96, 2509–2513. [Google Scholar] [CrossRef] [PubMed]
- de Geus, E.J.C.; Gianaros, P.J.; Brindle, R.C.; Jennings, J.R.; Berntson, G.G. Should heart rate variability be “corrected” for heart rate? Biological, quantitative, and interpretive considerations. Psychophysiology 2019, 56, e13287. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, G.E.; Balomenou, F.; Sakellariou, X.M.; Tassopoulos, C.; Nikas, D.N.; Giapros, V.; Kolettis, T.M. Autonomic function in obese children and adolescents: Systematic review and meta-analysis. J. Clin. Med. 2024, 13, 1854. [Google Scholar] [CrossRef]
- Pham, T.; Lau, Z.J.; Chen, S.H.A.; Makowski, D. Heart rate variability in psychology: A review of HRV indices and an analysis tutorial. Sensors 2021, 21, 3998. [Google Scholar] [CrossRef]
- Lovelace, J.W.; Ma, J.; Yadav, S.; Chhabria, K.; Shen, H.; Pang, Z.; Qi, T.; Sehgal, R.; Zhang, Y.; Bali, T.; et al. Vagal sensory neurons mediate the Bezold-Jarisch reflex and induce syncope. Nature 2023, 623, 387–396. [Google Scholar] [CrossRef]
- Abu-Ghazaleh, D.; Taylor, D.A.; Roberts, L.; Singh, I.; Cruzat, V.; Rose’Meyer, R.B. The pathophysiology of vasovagal syncope and new approaches to its pharmacological treatment. J. Cardiovasc. Pharmacol. Ther. 2025, 30, 10742484251351140. [Google Scholar] [CrossRef]
- Beinlich, F.R.M.; Asiminas, A.; Untiet, V.; Bojarowska, Z.; Plá, V.; Sigurdsson, B.; Timmel, V.; Gehrig, L.; Graber, M.H.; Hirase, H.; et al. Oxygen imaging of hypoxic pockets in the mouse cerebral cortex. Science 2024, 383, 1471–1478. [Google Scholar] [CrossRef]
- Kreydin, E.I.; Abedi, A.; Morales, L.; Montero, S.; Kohli, P.; Ha, N.; Chapman, D.; Abedi, A.; Ginsberg, D.; Jann, K.; et al. Neural mechanisms of poststroke urinary incontinence: Results from an fMRI Study. Stroke 2025, 56, 1516–1527. [Google Scholar] [CrossRef]
- Mattos, R.C.; Favorito, L.A. Neurophysiology of micturition: A narrative review on preventing mismanagement. Int. Braz. J. Urol. 2025, 51, e20259907. [Google Scholar] [CrossRef]
- Funayama, M.; Koreki, A.; Takata, T.; Nakagawa, Y.; Mimura, M. Post-stroke urinary incontinence is associated with behavior control deficits and overactive bladder. Neuropsychologia 2024, 201, 108942. [Google Scholar] [CrossRef] [PubMed]
- Vavilala, M.S.; Lee, L.A.; Lam, A.M. The lower limit of cerebral autoregulation in children during sevoflurane anesthesia. J. Neurosurg. Anesthesiol. 2003, 15, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Numan, M.; Alnajjar, R.; Lankford, J.; Gourishankar, A.; Butler, I. Cardiac asystole during head up tilt (HUTT) in children and adolescents: Is this benign physiology? Pediatr. Cardiol. 2015, 36, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Zou, R.; Wang, S.; Wen, W.; Cai, H.; Wang, Y.; Liu, P.; Li, F.; Lin, P.; Wang, C. Risk factors and prognostic follow-up of vasovagal syncope children with seizure-like activities during head-up tilt test induced-syncope. Front. Cardiovasc. Med. 2022, 9, 916542. [Google Scholar] [CrossRef]
- Wang, C.; Li, W.; Wu, L.; Lin, P.; Li, F.; Luo, H.; Xu, Y.; Xie, Z. Clinical characteristics and treatment of 89 patients with head-up tilt table test induced syncope with convulsion. J. Cent. South Univ. (Med. Sci.) 2013, 38, 70–73. [Google Scholar] [CrossRef]
- Jorge, J.G.; Pournazari, P.; Raj, S.R.; Maxey, C.; Sheldon, R.S. Frequency of injuries associated with syncope in the prevention of syncope trials. Europace 2020, 22, 1896–1903. [Google Scholar] [CrossRef]
- Tajdini, M.; Tavolinejad, H.; Aminorroaya, A.; Aryan, Z.; Jalali, A.; Alaeddini, F.; Sadeghian, S.; Yadangi, S.; Vasheghani-Farahani, A.; Kalhor, P.; et al. Clinical associations of injuries caused by vasovagal syncope: A cohort study from a tertiary syncope unit. J. Am. Heart Assoc. 2023, 12, e027272. [Google Scholar] [CrossRef]
- Jorge, J.G.; Raj, S.R.; Teixeira, P.S.; Teixeira, J.A.C.; Sheldon, R.S. Likelihood of injury due to vasovagal syncope: A systematic review and meta-analysis. Europace 2021, 23, 1092–1099. [Google Scholar] [CrossRef]
- Grinevich, A.A.; Chemeris, N.K. Age-related changes in heart rate variability from the neonatal period to adulthood. Dokl Biochem. Biophys. 2024, 519, 477–481. [Google Scholar] [CrossRef]
- Helánová, K.; Šišáková, M.; Hnatkova, K.; Novotný, T.; Andršová, I.; Malik, M. Development of autonomic heart rate modulations during childhood and adolescence. Pflugers Arch. 2024, 476, 1187–1207. [Google Scholar] [CrossRef]
| Atypical VVS Group (N = 68) | Control Group (N = 325) | t/Z/χ2 Value | p-Value | |
|---|---|---|---|---|
| Age, year | 12.0 (9.0, 14.0) | 12.0 (11.0, 14.0) | 1.248 | 0.209 a |
| Gender | 0.608 | 0.436 b | ||
| Male, n (%) | 30 (44.1) | 124 (38.2) | - | - |
| Female, n (%) | 38 (55.9) | 201 (61.8) | - | - |
| Height, cm | 160.0 (150.0, 167.0) | 160.0 (140.8, 167.5) | 0.497 | 0.619 a |
| Body weight, kg | 48.4 (38.5, 57.2) | 45.9 (31.4, 54.6) | 1.501 | 0.1335 a |
| BMI, kg/cm2 | 17.5 (15.4, 19.9) | 18.7 (16.6, 21.4) | 2.116 | 0.034 a |
| Baseline SBP, mmHg | 112.0 (106.0, 120.0) | 112.0 (105.3, 117.3) | 0.930 | 0.353 a |
| Baseline DBP, mmHg | 67.5 ± 8.3 | 65.9 ± 8.3 | 1.469 | 0.142 c |
| Baseline HR, beats/min | 82.5 (78.8, 91.3) | 88.0 (79.0, 94.0) | 1.152 | 0.249 a |
| Atypical VVS Group (N = 68) | Control Group (N = 325) | Z/χ2 Value | p Value | |
|---|---|---|---|---|
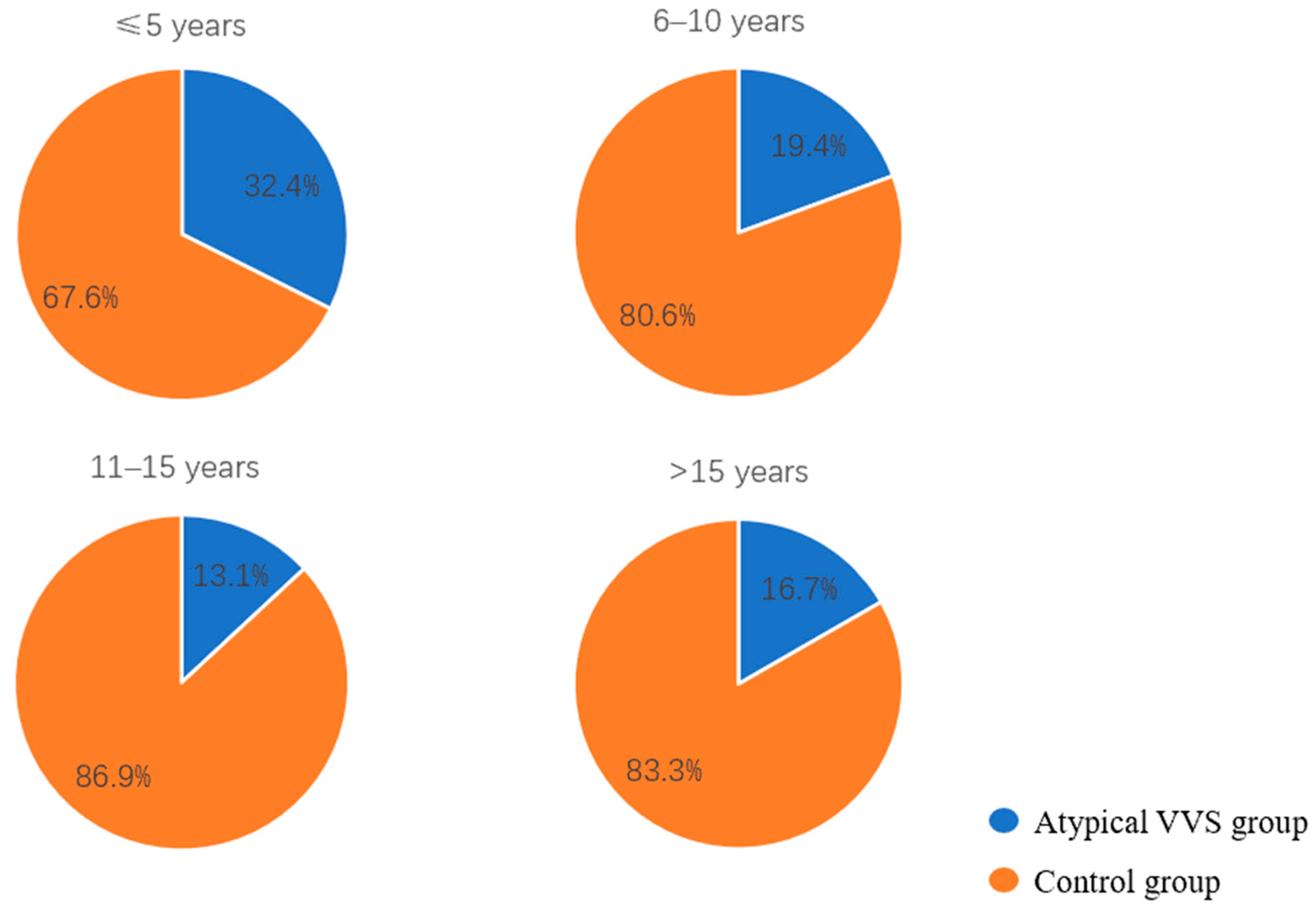
| Age at first syncopal episode, year | 9.5 (7.0, 12.0) | 11.0 (8.0, 13.0) | 2.227 | 0.025 a |
| Age groups by first-episode age | 0.027 b | |||
| ≤5 years, n (%) | 12 (17.6) | 25 (7.7) | 6.534 | 0.011 c |
| 6–10 years, n (%) | 28 (43.1) | 116 (35.7) | 0.729 | 0.393 c |
| 11–15 years, n (%) | 27 (39.7) | 179 (55.1) | 5.327 | 0.021 c |
| >15 years, n (%) | 1 (1.5) | 5 (1.5) | 1.000 b | |
| Course of disease, months | 12.0 (1.9, 36.3) | 8.0 (1.0, 24.0) | −1.397 | 0.162 a |
| Number of episodes | 3 (2, 4) | 3 (2, 5) | 0.039 | 0.969 a |
| Syncope-related trauma, n (%) | 15 (22.1) | 30 (9.2) | 7.905 | 0.005 c |
| Positive family history, n (%) | 24 (35.3) | 74 (22.8) | −4.067 | 0.044 c |
| Predisposing factors | ||||
| Peripheral triggers, n (%) | 58 (85.3) | 300 (92.3) | 2.600 | 0.107 c |
| Prolonged standing, n (%) | 44 (64.7) | 202 (74.8) | 0.066 | 0.797 c |
| Postural change, n (%) | 26 (38.2) | 138 (42.5) | 0.258 | 0.612 c |
| Rest after exercise, n (%) | 7 (10.3) | 46 (14.2) | 0.425 | 0.514 c |
| Central triggers, n (%) | 23 (33.8) | 64 (19.7) | 5.721 | 0.017 c |
| Intramuscular injection or venipuncture, n (%) | 8 (11.8) | 23 (7.1) | 1.117 | 0.291 c |
| Emotion, n (%) | 9 (13.2) | 29 (8.9) | 0.754 | 0.385 c |
| Pain, n (%) | 13 (19.1) | 20 (6.2) | 10.659 | 0.001 c |
| Premonitory symptom | ||||
| Dizziness, n (%) | 35 (51.5) | 219 (67.4) | 5.553 | 0.018 c |
| Amaurosis fugax, n (%) | 28 (41.2) | 190 (58.5) | 6.120 | 0.013 c |
| Blurred vision, n (%) | 20 (29.4) | 70 (21.5) | 1.554 | 0.213 c |
| Tinnitus, n (%) | 4 (5.9) | 30 (9.2) | 0.430 | 0.512 c |
| Gastrointestinal symptoms, n (%) | 19 (27.9) | 86 (26.5) | 0.010 | 0.920 c |
| Palpation, n (%) | 5 (7.4) | 50 (15.4) | 2.383 | 0.123 c |
| Absent, n (%) | 8 (11.8) | 19 (5.8) | 0.109 b |
| Atypical VVS Group (N = 68) | Control Group (N = 325) | t/Z/χ2 Value | p-Value | |
|---|---|---|---|---|
| 24 h urinary sodium excretion, mmol/24 h | 115.1 (91.6, 152.0) | 119.5 (84.0, 158.4) | 0.259 | 0.796 a |
| 24 h urinary volume, mL | 1350.0 (1033.8, 1831.3) | 1350.0 (1000.0, 1810.0) | −0.558 | 0.577 a |
| FMD, % | 10.7 (9.8, 12.7) | 11.5 (10.0, 13.7) | 1.256 | 0.208 a |
| 24 h total heartbeats, beats | 113,250.7 ± 12,857.9 | 115,112.4 ± 12,210.1 | 1.133 | 0.258 b |
| Minimum heart rate, beats/min | 48.0 (44.8, 52.0) | 50.0 (47.0, 54.0) | 2.668 | 0.008 a |
| Maximum heart rate, beats/min | 151.5 (143.5, 159.0) | 151.0 (141.0, 159.0) | −0.046 | 0.964 a |
| Average heart rate, beats/min | 79.0 (73.0, 85.3) | 82.0 (75.0, 86.0) | 1.290 | 0.197 a |
| SDNN, ms | 150.5 (135.0, 179.0) | 151.0 (129.0, 171.0) | −1.088 | 0.277 a |
| SDANN, ms | 133.0 (114.8, 157.3) | 132.0 (113.0, 151.0) | −0.849 | 0.396 a |
| rMSSD, ms | 47.5 (41.0, 64.0) | 45.0 (36.0, 56.0) | −2.074 | 0.038 a |
| pNN50, % | 23.4 (16.6, 34.2) | 20.1 (13.1, 28.4) | −2.318 | 0.021 a |
| HF, ms | 26.1 (20.5, 36.7) | 24.7 (18.5, 34.2) | −1.739 | 0.082 a |
| LF, ms | 31.3 (25.1, 40.6) | 29.4 (24.4, 35.0) | −1.747 | 0.081 a |
| LF/HF | 1.14 (0.97, 1.29) | 1.18 (0.99, 1.37) | 1.337 | 0.181 a |
| Cardioinhibitory or mixed type, n (%) | 10 (14.7) | 25 (7.7) | 2.600 | 0.107 c |
| Malignant VVS, n (%) | 5 (7.4) | 2 (0.6) | 0.002 d |
| Parameter | F | B | p (Gender) | p (Age) | p (Group) |
|---|---|---|---|---|---|
| 24 h total heartbeats | 3.081 | −2546.439 | 0.002 | 0.000 | 0.080 |
| Minimum heart rate | 11.570 | −2.620 | 0.000 | 0.000 | 0.001 |
| Maximum heart rate | 0.066 | −0.467 | 0.006 | 0.000 | 0.797 |
| Average heart rate | 5.093 | −2.403 | 0.014 | 0.000 | 0.025 |
| SDNN | 3.153 | 7.699 | 0.001 | 0.000 | 0.077 |
| SDANN | 1.818 | 5.628 | 0.004 | 0.000 | 0.178 |
| rMSSD | 6.339 | 5.858 | 0.033 | 0.964 | 0.012 |
| pNN50 | 5.802 | 3.451 | 0.017 | 0.207 | 0.016 |
| HF | 4.750 | 3.796 | 0.401 | 0.254 | 0.030 |
| LF | 3.977 | 2.406 | 0.000 | 0.095 | 0.047 |
| LF/HF | 1.953 | −0.054 | 0.010 | 0.000 | 0.163 |
| Variable | OR | 95% CI | p-Value | False Discovery Rate-Adjusted p-Value |
|---|---|---|---|---|
| BMI | 0.944 | 0.873–1.014 | 0.127 | 0.127 |
| Age at first syncopal episode | 0.907 | 0.835–0.983 | 0.018 | 0.048 |
| Positive family history | 1.85 | 1.045–3.222 | 0.032 | 0.050 |
| Peripheral trigger | 0.483 | 0.226–1.104 | 0.070 | 0.080 |
| Central trigger | 2.084 | 1.163–3.668 | 0.012 | 0.047 |
| Minimum heart rate | 0.937 | 0.897–0.978 | 0.003 | 0.027 |
| HF | 1.021 | 1.002–1.04 | 0.024 | 0.066 |
| Cardioinhibitory or mixed type | 0.483 | 0.226–1.104 | 0.070 | 0.093 |
| Variable | Tolerance | VIF |
|---|---|---|
| Gender | 0.906 | 1.104 |
| Age | 0.383 | 2.613 |
| Age at first syncopal episode, years | 0.369 | 2.712 |
| Positive family history | 0.950 | 1.052 |
| Peripheral trigger | 0.890 | 1.124 |
| Central trigger | 0.822 | 1.216 |
| Minimum heart rate, beats/min | 0.677 | 1.477 |
| HF | 0.787 | 1.271 |
| Cardioinhibitory or mixed type | 0.962 | 1.040 |
| B | SE | Wald | p | OR (95% CI) | |
|---|---|---|---|---|---|
| Age at first syncopal episode | −0.135 | 0.044 | 9.566 | 0.002 | 0.874 (0.802, 0.952) |
| Minimum heart rate | −0.082 | 0.024 | 12.002 | 0.001 | 0.921 (0.879, 0.965) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Xu, W.; Zhang, C.; Du, J.; Jin, H.; Liao, Y. Analysis of Clinical Features in Children with Vasovagal Syncope Complicated by Convulsions or Incontinence. Biomedicines 2026, 14, 36. https://doi.org/10.3390/biomedicines14010036
Xu W, Zhang C, Du J, Jin H, Liao Y. Analysis of Clinical Features in Children with Vasovagal Syncope Complicated by Convulsions or Incontinence. Biomedicines. 2026; 14(1):36. https://doi.org/10.3390/biomedicines14010036
Chicago/Turabian StyleXu, Wenrui, Chunyu Zhang, Junbao Du, Hongfang Jin, and Ying Liao. 2026. "Analysis of Clinical Features in Children with Vasovagal Syncope Complicated by Convulsions or Incontinence" Biomedicines 14, no. 1: 36. https://doi.org/10.3390/biomedicines14010036
APA StyleXu, W., Zhang, C., Du, J., Jin, H., & Liao, Y. (2026). Analysis of Clinical Features in Children with Vasovagal Syncope Complicated by Convulsions or Incontinence. Biomedicines, 14(1), 36. https://doi.org/10.3390/biomedicines14010036







