Systemic Neurodegeneration and Brain Aging: Multi-Omics Disintegration, Proteostatic Collapse, and Network Failure Across the CNS
Abstract
1. Molecular Collapse in Context: From Complexity to Catastrophe
2. Disintegration of Signaling Networks in Neurodegeneration
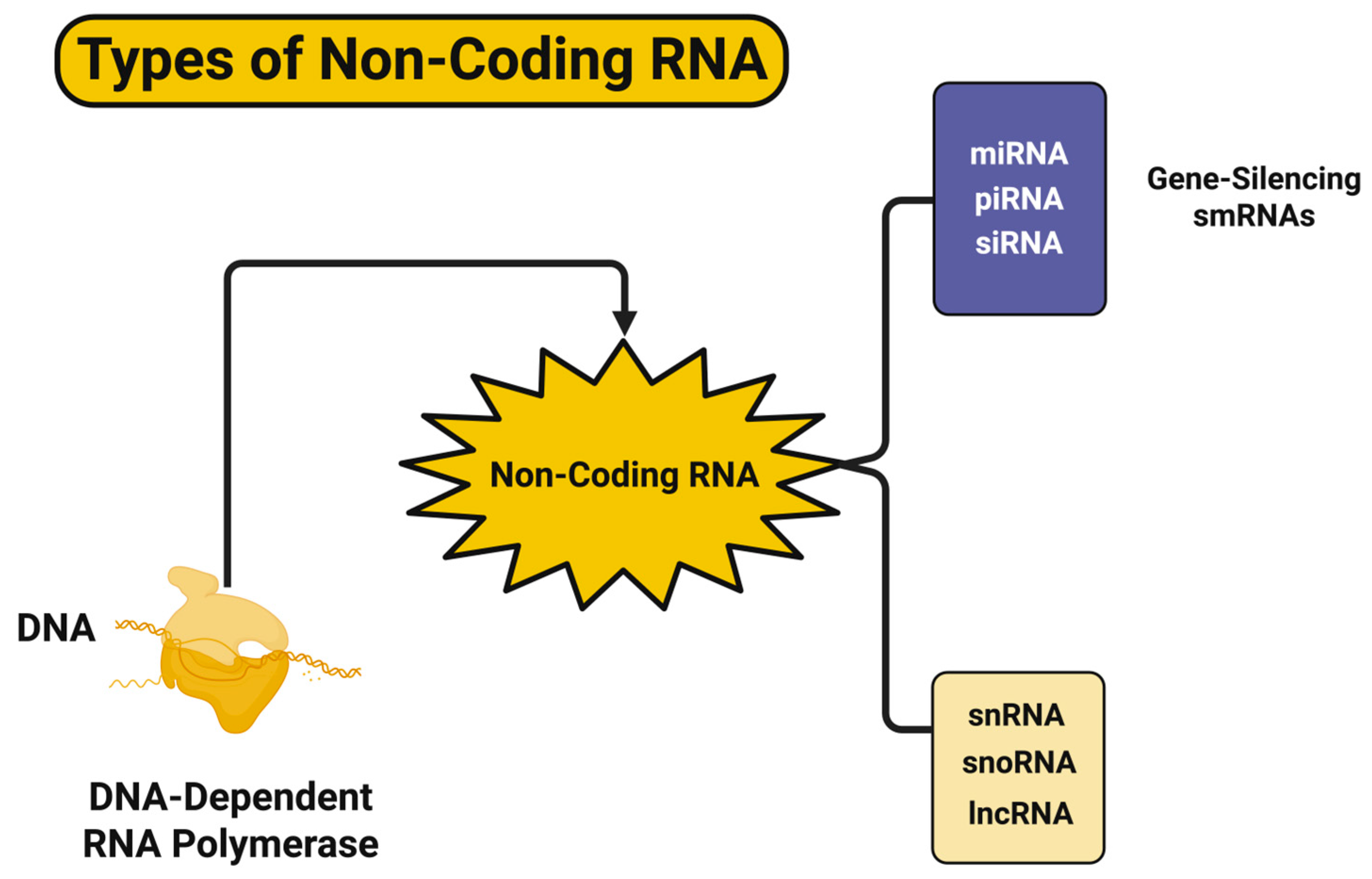
3. Epigenetic Drift and Transcriptional Entropy in Neurodegeneration
4. Proteostatic Collapse and Organelle Overload in Neurodegeneration
5. Network Disintegration and Functional Disconnectivity in Neurodegeneration
6. Neurovascular Uncoupling and Blood–Brain Interface Failure
7. Glymphatic–Venous Collapse and Perivascular Clearance Breakdown
8. Synaptic Disassembly and Excitatory–Inhibitory Circuit Breakdown
9. Metabolic Collapse and Mitochondrial Circuitry Failure
10. Gut–Brain Axis as a Modulator of Neurodegenerative Cascades
11. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gao, J.; Ding, M.; Qin, S.; Shukla, D.; Vicuna, L.; Liang, J.; Wang, X. The mechanisms underlying TDP-43-associated neurodegeneration in Alzheimer’s disease and related dementias. Mol. Psychiatry 2025. [Google Scholar] [CrossRef]
- Su, J.; Song, Y.; Zhu, Z.; Huang, X.; Fan, J.; Qiao, J.; Mao, F. Cell–cell communication: New insights and clinical implications. Signal Transduct. Target. Ther. 2024, 9, 196. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X.; Zhang, C.; Gao, S. Multi-scale neural homeostasis mechanisms: Insights into neurodegenerative diseases and therapeutic approaches, including exercise. Adv. Exerc. Health Sci. 2025, 2, 1–15. [Google Scholar] [CrossRef]
- Casartelli, L.; Maronati, C.; Cavallo, A. From neural noise to co-adaptability: Rethinking the multifaceted architecture of motor variability. Phys. Life Rev. 2023, 47, 245–263. [Google Scholar] [CrossRef]
- Foret, M.K.; Orciani, C.; Welikovitch, L.A.; Huang, C.; Cuello, A.C.; Do Carmo, S. Early oxidative stress and DNA damage in Aβ-burdened hippocampal neurons in an Alzheimer’s-like transgenic rat model. Commun. Biol. 2024, 7, 861. [Google Scholar] [CrossRef]
- Huang, Y.; Sun, L.; Zhu, S.; Xu, L.; Liu, S.; Yuan, C.; Guo, Y.; Wang, X. Neuroprotection Against Parkinson’s Disease Through the Activation of Akt/GSK3β Signaling Pathway by Tovophyllin A. Front. Neurosci. 2020, 14, 00723. [Google Scholar] [CrossRef] [PubMed]
- Marbach, D.; Lamparter, D.; Quon, G.; Kellis, M.; Kutalik, Z.; Bergmann, S. Tissue-specific regulatory circuits reveal variable modular perturbations across complex diseases. Nat. Methods 2016, 13, 366–370. [Google Scholar] [CrossRef] [PubMed]
- Grandi, F.C.; Modi, H.; Kampman, L.; Corces, M.R. Chromatin accessibility profiling by ATAC-seq. Nat. Protoc. 2022, 17, 1518–1552. [Google Scholar] [CrossRef] [PubMed]
- Zheng, K.; Lyu, Z.; Chen, J.; Chen, G. 5-Hydroxymethylcytosine: Far Beyond the Intermediate of DNA Demethylation. Int. J. Mol. Sci. 2024, 25, 11780. [Google Scholar] [CrossRef] [PubMed]
- Honig, F.; Murrell, A. Cell identity and 5-hydroxymethylcytosine. Epigenetics Chromatin 2025, 18, 36. [Google Scholar] [CrossRef]
- Derevyanko, A.; Tao, T.; Allen, N.J. Common alterations to astrocytes across neurodegenerative disorders. Curr. Opin. Neurobiol. 2025, 90, 102970. [Google Scholar] [CrossRef]
- Limone, F.; Mordes, D.A.; Couto, A.; Joseph, B.J.; Mitchell, J.M.; Therrien, M.; Ghosh, S.D.; Meyer, D.; Zhang, Y.; Goldman, M.; et al. Single-nucleus sequencing reveals enriched expression of genetic risk factors in extratelencephalic neurons sensitive to degeneration in ALS. Nat. Aging 2024, 4, 984–997. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; Wu, C.; Parker, E.; Liu, T.C.-Y.; Duan, R.; Yang, L. Microglia and Astrocytes in Alzheimer’s Disease: Significance and Summary of Recent Advances. Aging Dis. 2024, 15, 1537–1564. [Google Scholar] [CrossRef] [PubMed]
- Tedesco, B.; Ferrari, V.; Cozzi, M.; Chierichetti, M.; Casarotto, E.; Pramaggiore, P.; Mina, F.; Galbiati, M.; Rusmini, P.; Crippa, V.; et al. The Role of Small Heat Shock Proteins in Protein Misfolding Associated Motoneuron Diseases. Int. J. Mol. Sci. 2022, 23, 11759. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Oliveira, T.; Montezinho, L.; Simões, R.F.; Carvalho, M.; Ferreiro, E.; Silva, F.S.G. Mitochondria: A Promising Convergent Target for the Treatment of Amyotrophic Lateral Sclerosis. Cells 2024, 13, 248. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chu, J.-M.-T.; Wong, G.-T.-C. Cerebral Glutamate Regulation and Receptor Changes in Perioperative Neuroinflammation and Cognitive Dysfunction. Biomolecules 2022, 12, 597. [Google Scholar] [CrossRef]
- Pradeepa, M.M. Causal role of histone acetylations in enhancer function. Transcription 2017, 8, 40–47. [Google Scholar] [CrossRef]
- Bojarskaite, L.; Nafari, S.; Ravnanger, A.K.; Frey, M.M.; Skauli, N.; Åbjørsbråten, K.S.; Roth, L.C.; Amiry-Moghaddam, M.; Nagelhus, E.A.; Ottersen, O.P.; et al. Role of aquaporin-4 polarization in extracellular solute clearance. Fluids Barriers CNS 2024, 21, 28. [Google Scholar] [CrossRef]
- Bhat, G.R.; Sethi, I.; Sadida, H.Q.; Rah, B.; Mir, R.; Algehainy, N.; Albalawi, I.A.; Masoodi, T.; Subbaraj, G.K.; Jamal, F.; et al. Cancer cell plasticity: From cellular, molecular, and genetic mechanisms to tumor heterogeneity and drug resistance. Cancer Metastasis Rev. 2024, 43, 197–228. [Google Scholar] [CrossRef]
- Csermely, P.; Korcsmáros, T.; Kiss, H.J.M.; London, G.; Nussinov, R. Structure and dynamics of molecular networks: A novel paradigm of drug discovery: A comprehensive review. Pharmacol. Ther. 2013, 138, 333–408. [Google Scholar] [CrossRef]
- Picard, M.; Shirihai, O.S. Mitochondrial signal transduction. Cell Metab. 2022, 34, 1620–1653. [Google Scholar] [CrossRef]
- Toader, C.; Tataru, C.P.; Munteanu, O.; Serban, M.; Covache-Busuioc, R.-A.; Ciurea, A.V.; Enyedi, M. Decoding Neurodegeneration: A Review of Molecular Mechanisms and Therapeutic Advances in Alzheimer’s, Parkinson’s, and ALS. Int. J. Mol. Sci. 2024, 25, 12613. [Google Scholar] [CrossRef]
- Zhang, W.; Xiao, D.; Mao, Q.; Xia, H. Role of neuroinflammation in neurodegeneration development. Signal Transduct. Target. Ther. 2023, 8, 267. [Google Scholar] [CrossRef]
- Martínez Báez, A.; Ayala, G.; Pedroza-Saavedra, A.; González-Sánchez, H.M.; Chihu Amparan, L. Phosphorylation Codes in IRS-1 and IRS-2 Are Associated with the Activation/Inhibition of Insulin Canonical Signaling Pathways. Curr. Issues Mol. Biol. 2024, 46, 634–649. [Google Scholar] [CrossRef]
- Rad, S.K.; Arya, A.; Karimian, H.; Madhavan, P.; Rizwan, F.; Koshy, S.; Prabhu, G. Mechanism involved in insulin resistance via accumulation of β-amyloid and neurofibrillary tangles: Link between type 2 diabetes and Alzheimer’s disease. Drug Des. Devel. Ther. 2018, 12, 3999–4021. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.-C.; Wu, M.-Y.; Lim, P.S. Alterations in Autophagic Function and Endoplasmic Reticulum Stress Markers in the Peripheral Blood Mononuclear Cells of Patients on Hemodialysis. Int. J. Mol. Sci. 2025, 26, 447. [Google Scholar] [CrossRef]
- Verma, A.; Ravindranath, V. CaV1.3 L-Type Calcium Channels Increase the Vulnerability of Substantia Nigra Dopaminergic Neurons in MPTP Mouse Model of Parkinson’s Disease. Front. Aging Neurosci. 2020, 11, 382. [Google Scholar] [CrossRef] [PubMed]
- Trinh, V.H.; Nguyen Huu, T.; Sah, D.K.; Choi, J.M.; Yoon, H.J.; Park, S.C.; Jung, Y.S.; Lee, S.-R. Redox Regulation of PTEN by Reactive Oxygen Species: Its Role in Physiological Processes. Antioxidants 2024, 13, 199. [Google Scholar] [CrossRef]
- Wei, B.; Wei, M.; Huang, H.; Fan, T.; Zhang, Z.; Song, X. Mesenchymal Stem Cell-Derived Exosomes: A Promising Therapeutic Strategy for Age-Related Diseases. Cell Prolif. 2024, 58, e13795. [Google Scholar] [CrossRef]
- Scorza, C.; Goncalves, V.; Finsterer, J.; Scorza, F.; Fonseca, F. Exploring the Prospective Role of Propolis in Modifying Aging Hallmarks. Cells 2024, 13, 390. [Google Scholar] [CrossRef]
- Claiborne, N.; Anisimova, M.; Zito, K. Activity-Dependent Stabilization of Nascent Dendritic Spines Requires Nonenzymatic CaMKIIα Function. J. Neurosci. Off. J. Soc. Neurosci. 2024, 44, e1393222023. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, P.M.; Bender, K.J. Axon Initial Segment Structure and Function in Health and Disease. Physiol. Rev. 2025, 105, 765–801. [Google Scholar] [CrossRef]
- Marin Zapata, P.A.; Beese, C.J.; Jünger, A.; Dalmasso, G.; Brady, N.R.; Hamacher-Brady, A. Time course decomposition of cell heterogeneity in TFEB signaling states reveals homeostatic mechanisms restricting the magnitude and duration of TFEB responses to mTOR activity modulation. BMC Cancer 2016, 16, 355. [Google Scholar] [CrossRef] [PubMed]
- Green, C.D.; Maceyka, M.; Cowart, L.A.; Spiegel, S. Sphingolipids in Metabolic Disease: The Good, the Bad, and the Unknown. Cell Metab. 2021, 33, 1293–1306. [Google Scholar] [CrossRef]
- Ramos-Molina, B.; Rossell, J.; Pérez-Montes de Oca, A.; Pardina, E.; Genua, I.; Rojo-López, M.I.; Julián, M.T.; Alonso, N.; Julve, J.; Mauricio, D. Therapeutic implications for sphingolipid metabolism in metabolic dysfunction-associated steatohepatitis. Front. Endocrinol. 2024, 15, 1400961. [Google Scholar] [CrossRef]
- Warda, M.; Tekin, S.; Gamal, M.; Khafaga, N.; Çelebi, F.; Tarantino, G. Lipid rafts: Novel therapeutic targets for metabolic, neurodegenerative, oncological, and cardiovascular diseases. Lipids Health Dis. 2025, 24, 147. [Google Scholar] [CrossRef]
- van Weperen, V.Y.H.; Vaseghi, M. Cardiac vagal afferent neurotransmission in health and disease: Review and knowledge gaps. Front. Neurosci. 2023, 17, 1192188. [Google Scholar] [CrossRef]
- Park, J.Y.; Han, S.; Ka, H.I.; Joo, H.J.; Soh, S.J.; Yoo, K.H.; Yang, Y. Silent mating-type information regulation 2 homolog 1 overexpression is an important strategy for the survival of adapted suspension tumor cells. Cancer Sci. 2019, 110, 2773–2782. [Google Scholar] [CrossRef] [PubMed]
- Sidoryk-Węgrzynowicz, M.; Adamiak, K.; Strużyńska, L. Astrocyte–Neuron Interaction via the Glutamate–Glutamine Cycle and Its Dysfunction in Tau-Dependent Neurodegeneration. Int. J. Mol. Sci. 2024, 25, 3050. [Google Scholar] [CrossRef]
- Lia, A.; Di Spiezio, A.; Vitalini, L.; Tore, M.; Puja, G.; Losi, G. Ion Channels and Ionotropic Receptors in Astrocytes: Physiological Functions and Alterations in Alzheimer’s Disease and Glioblastoma. Life 2023, 13, 2038. [Google Scholar] [CrossRef]
- Sabit, H.; Arneth, B.; Pawlik, T.M.; Abdel-Ghany, S.; Ghazy, A.; Abdelazeem, R.M.; Alqosaibi, A.; Al-Dhuayan, I.S.; Almulhim, J.; Alrabiah, N.A.; et al. Leveraging Single-Cell Multi-Omics to Decode Tumor Microenvironment Diversity and Therapeutic Resistance. Pharmaceuticals 2025, 18, 75. [Google Scholar] [CrossRef]
- Armanville, S.; Tocco, C.; Haj Mohamad, Z.; Clarke, D.; Robitaille, R.; Drouin-Ouellet, J. Chemically Induced Senescence Prompts Functional Changes in Human Microglia-Like Cells. J. Immunol. Res. 2025, 2025, 3214633. [Google Scholar] [CrossRef]
- Mierke, C.T. Viscoelasticity, Like Forces, Plays a Role in Mechanotransduction. Front. Cell Dev. Biol. 2022, 10, 789841. [Google Scholar] [CrossRef]
- Ma, P.; Li, Y.; Wang, H.; Mao, B. Haploinsufficiency of the TDP43 ubiquitin E3 ligase RNF220 leads to ALS-like motor neuron defects in the mouse. J. Mol. Cell Biol. 2021, 13, 374–382. [Google Scholar] [CrossRef]
- Kofler, M.; Kapus, A. Nuclear Import and Export of YAP and TAZ. Cancers 2023, 15, 4956. [Google Scholar] [CrossRef]
- Guo, S.; Wang, H.; Yin, Y. Microglia Polarization From M1 to M2 in Neurodegenerative Diseases. Front. Aging Neurosci. 2022, 14, 815347. [Google Scholar] [CrossRef]
- Tufail, M.; Jiang, C.-H.; Li, N. Wnt signaling in cancer: From biomarkers to targeted therapies and clinical translation. Mol. Cancer 2025, 24, 107. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, X.; Vikash, V.; Ye, Q.; Wu, D.; Liu, Y.; Dong, W. ROS and ROS-Mediated Cellular Signaling. Oxid. Med. Cell. Longev. 2016, 2016, 4350965. [Google Scholar] [CrossRef] [PubMed]
- Toader, C.; Tataru, C.P.; Munteanu, O.; Covache-Busuioc, R.-A.; Serban, M.; Ciurea, A.V.; Enyedi, M. Revolutionizing Neuroimmunology: Unraveling Immune Dynamics and Therapeutic Innovations in CNS Disorders. Int. J. Mol. Sci. 2024, 25, 13614. [Google Scholar] [CrossRef]
- Csizmok, V.; Follis, A.V.; Kriwacki, R.W.; Forman-Kay, J.D. Dynamic protein interaction networks and new structural paradigms in signaling. Chem. Rev. 2016, 116, 6424–6462. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zuo, X.; Becker, A.; Mobley, W.C. Hyperactivation of RAB5 disrupts the endosomal Rab cascade leading to endolysosomal dysregulation in Down syndrome: A necessary role for increased APP gene dose. Alzheimer’s Dement. 2025, 21, e70046. [Google Scholar] [CrossRef] [PubMed]
- Siri, S.O.; Rozés-Salvador, V.; de la Villarmois, E.A.; Ghersi, M.S.; Quassollo, G.; Pérez, M.F.; Conde, C. Decrease of Rab11 prevents the correct dendritic arborization, synaptic plasticity and spatial memory formation. Biochim. Biophys. Acta Mol. Cell Res. 2020, 1867, 118735. [Google Scholar] [CrossRef]
- Ahn, G.; Banik, S.M.; Bertozzi, C.R. Degradation from the outside-in: Targeting extracellular and membrane proteins for degradation through the endo-lysosomal pathway. Cell Chem. Biol. 2021, 28, 1072–1080. [Google Scholar] [CrossRef]
- Stoliker, D.; Egan, G.F.; Friston, K.J.; Razi, A. Neural Mechanisms and Psychology of Psychedelic Ego Dissolution. Pharmacol. Rev. 2022, 74, 876–917. [Google Scholar] [CrossRef]
- Wason, T.D. A model integrating multiple processes of synchronization and coherence for information instantiation within a cortical area. Biosystems 2021, 205, 104403. [Google Scholar] [CrossRef]
- Giri, P.M.; Banerjee, A.; Ghosal, A.; Layek, B. Neuroinflammation in Neurodegenerative Disorders: Current Knowledge and Therapeutic Implications. Int. J. Mol. Sci. 2024, 25, 3995. [Google Scholar] [CrossRef] [PubMed]
- Ling, N.X.Y.; Kaczmarek, A.; Hoque, A.; Davie, E.; Ngoei, K.R.W.; Morrison, K.R.; Smiles, W.J.; Forte, G.M.; Wang, T.; Lie, S.; et al. mTORC1 directly inhibits AMPK to promote cell proliferation under nutrient stress. Nat. Metab. 2020, 2, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Jurca, C.M.; Kozma, K.; Petchesi, C.D.; Zaha, D.C.; Magyar, I.; Munteanu, M.; Faur, L.; Jurca, A.; Bembea, D.; Severin, E.; et al. Tuberous Sclerosis, Type II Diabetes Mellitus and the PI3K/AKT/mTOR Signaling Pathways—Case Report and Literature Review. Genes 2023, 14, 433. [Google Scholar] [CrossRef]
- Martínez-González, L.; Gonzalo-Consuegra, C.; Gómez-Almería, M.; Porras, G.; de Lago, E.; Martín-Requero, Á.; Martínez, A. Tideglusib, a Non-ATP Competitive Inhibitor of GSK-3β as a Drug Candidate for the Treatment of Amyotrophic Lateral Sclerosis. Int. J. Mol. Sci. 2021, 22, 8975. [Google Scholar] [CrossRef]
- Low, B.S.H.; Asimaki, A. Targeting Canonical Wnt-signaling Through GSK-3β in Arrhythmogenic Cardiomyopathy: Conservative or Progressive? J. Cardiovasc. Transl. Res. 2025, 18, 121–132. [Google Scholar] [CrossRef]
- Gottlieb, S.; van der Vaart, A.; Hassan, A.; Bledsoe, D.; Morgan, A.; O’Rourke, B.; Rogers, W.D.; Wolstenholme, J.T.; Miles, M.F. A Selective GSK3β Inhibitor, Tideglusib, Decreases Intermittent Access and Binge Ethanol Self-Administration in C57BL/6J Mice. Addict. Biol. 2025, 30, e70044. [Google Scholar] [CrossRef]
- Tzeplaeff, L.; Seguin, J.; Le Gras, S.; Megat, S.; Cosquer, B.; Plassard, D.; Dieterlé, S.; Paiva, I.; Picchiarelli, G.; Decraene, C.; et al. Mutant FUS induces chromatin reorganization in the hippocampus and alters memory processes. Prog. Neurobiol. 2023, 227, 102483. [Google Scholar] [CrossRef]
- Esvald, E.-E.; Tuvikene, J.; Sirp, A.; Patil, S.; Bramham, C.R.; Timmusk, T. CREB Family Transcription Factors Are Major Mediators of BDNF Transcriptional Autoregulation in Cortical Neurons. J. Neurosci. Off. J. Soc. Neurosci. 2020, 40, 1405–1426. [Google Scholar] [CrossRef]
- Zhang, S.; Meng, Y.; Zhou, L.; Qiu, L.; Wang, H.; Su, D.; Zhang, B.; Chan, K.; Han, J. Targeting epigenetic regulators for inflammation: Mechanisms and intervention therapy. MedComm 2022, 3, e173. [Google Scholar] [CrossRef]
- Kamel, M.M.; Robinson, N.; Kutyna, M.; Lim, K.; Thompson-Peach, C.; Lane, S.W.; Yeung, D.T.; Yong, A.S.M.; Ross, D.M.; Hiwase, D.; et al. High Dose Ascorbate Reduces Interleukin-1 Beta Secretion in TET2 Mutant Monocytes and Demonstrates Excellent Safety and Tolerability in CMML Patients in Combination with Azacitidine. Blood 2024, 144, 1817. [Google Scholar] [CrossRef]
- Guan, Y.; Hasipek, M.; Tiwari, A.D.; Maciejewski, J.P.; Jha, B.K. TET-dioxygenase deficiency in oncogenesis and its targeting for tumor-selective therapeutics. Semin. Hematol. 2021, 58, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.; Yao, H.; Shah, S.Z.A.; Wu, W.; Wang, D.; Zhao, Y.; Wang, L.; Zhou, X.; Zhao, D.; Yang, L. The NLRP3-Caspase 1 Inflammasome Negatively Regulates Autophagy via TLR4-TRIF in Prion Peptide-Infected Microglia. Front. Aging Neurosci. 2018, 10, 00116. [Google Scholar] [CrossRef] [PubMed]
- Olcum, M.; Tufekci, K.U.; Durur, D.Y.; Tastan, B.; Gokbayrak, I.N.; Genc, K.; Genc, S. Ethyl Pyruvate Attenuates Microglial NLRP3 Inflammasome Activation via Inhibition of HMGB1/NF-κB/miR-223 Signaling. Antioxidants 2021, 10, 745. [Google Scholar] [CrossRef]
- Yoshizaki, K.; Kimura, R.; Kobayashi, H.; Oki, S.; Kikkawa, T.; Mai, L.; Koike, K.; Mochizuki, K.; Inada, H.; Matsui, Y.; et al. Paternal age affects offspring via an epigenetic mechanism involving REST/NRSF. EMBO Rep. 2021, 22, e51524. [Google Scholar] [CrossRef]
- Wang, C.; Wang, F.; Li, Z.; Cao, Q.; Huang, L.; Chen, S. MeCP2-mediated epigenetic regulation in senescent endothelial progenitor cells. Stem Cell Res. Ther. 2018, 9, 87. [Google Scholar] [CrossRef]
- Periyasamy, P.; Thangaraj, A.; Guo, M.-L.; Hu, G.; Callen, S.; Buch, S. Epigenetic Promoter DNA Methylation of miR-124 Promotes HIV-1 Tat-Mediated Microglial Activation via MECP2-STAT3 Axis. J. Neurosci. Off. J. Soc. Neurosci. 2018, 38, 5367–5383. [Google Scholar] [CrossRef]
- Lidón, L.; Llaó-Hierro, L.; Nuvolone, M.; Aguzzi, A.; Ávila, J.; Ferrer, I.; del Río, J.A.; Gavín, R. Tau Exon 10 Inclusion by PrPC through Downregulating GSK3β Activity. Int. J. Mol. Sci. 2021, 22, 5370. [Google Scholar] [CrossRef]
- Baltissen, D.; Bold, C.S.; Rehra, L.; Banićević, M.; Fricke, J.; Just, J.; Ludewig, S.; Buchholz, C.J.; Korte, M.; Müller, U.C. APPsα rescues CDK5 and GSK3β dysregulation and restores normal spine density in Tau transgenic mice. Front. Cell. Neurosci. 2023, 17, 1106176. [Google Scholar] [CrossRef]
- Good, K.V.; Vincent, J.B.; Ausió, J. MeCP2: The Genetic Driver of Rett Syndrome Epigenetics. Front. Genet. 2021, 12, 620859. [Google Scholar] [CrossRef]
- Vuu, Y.M.; Roberts, C.-T.; Rastegar, M. MeCP2 Is an Epigenetic Factor That Links DNA Methylation with Brain Metabolism. Int. J. Mol. Sci. 2023, 24, 4218. [Google Scholar] [CrossRef]
- Allison, K.; Maletic-Savatic, M.; Pehlivan, D. MECP2-related disorders while gene-based therapies are on the horizon. Front. Genet. 2024, 15, 1332469. [Google Scholar] [CrossRef]
- Ge, P.; Dawson, V.L.; Dawson, T.M. PINK1 and Parkin mitochondrial quality control: A source of regional vulnerability in Parkinson’s disease. Mol. Neurodegener. 2020, 15, 20. [Google Scholar] [CrossRef]
- Quinn, P.M.J.; Moreira, P.I.; Ambrósio, A.F.; Alves, C.H. PINK1/PARKIN signalling in neurodegeneration and neuroinflammation. Acta Neuropathol. Commun. 2020, 8, 189. [Google Scholar] [CrossRef]
- Carey, J.L.; Guo, L. Liquid-Liquid Phase Separation of TDP-43 and FUS in Physiology and Pathology of Neurodegenerative Diseases. Front. Mol. Biosci. 2022, 9, 826719. [Google Scholar] [CrossRef]
- Fang, M.; Deibler, S.K.; Nana, A.L.; Vatsavayai, S.C.; Banday, S.; Zhou, Y.; Almeida, S.; Weiss, A.; Brown, R.H.; Seeley, W.W.; et al. Loss of TDP-43 function contributes to genomic instability in amyotrophic lateral sclerosis. Front. Neurosci. 2023, 17, 1251228. [Google Scholar] [CrossRef]
- Pao, P.-C.; Tsai, L.-H. Three decades of Cdk5. J. Biomed. Sci. 2021, 28, 79. [Google Scholar] [CrossRef]
- Park, K.H.J.; Franciosi, S.; Parrant, K.; Lu, G.; Leavitt, B.R. p35 hemizygosity activates Akt but does not improve motor function in the YAC128 mouse model of Huntington’s disease. Neuroscience 2017, 352, 79–87. [Google Scholar] [CrossRef]
- Guo, W.-T.; Wang, Y. Dgcr8 knockout approaches to understand microRNA functions in vitro and in vivo. Cell. Mol. Life Sci. CMLS 2019, 76, 1697–1711. [Google Scholar] [CrossRef]
- Jouravleva, K.; Golovenko, D.; Demo, G.; Dutcher, R.C.; Tanaka Hall, T.M.; Zamore, P.D.; Korostelev, A.A. Structural Basis of MicroRNA Biogenesis by Dicer-1 and Its Partner Protein Loqs-PB. Mol. Cell 2022, 82, 4049–4063.e6. [Google Scholar] [CrossRef]
- Kristiani, L.; Kim, Y. The Interplay between Oxidative Stress and the Nuclear Lamina Contributes to Laminopathies and Age-Related Diseases. Cells 2023, 12, 1234. [Google Scholar] [CrossRef]
- Kaneshiro, J.M.; Capitanio, J.S.; Hetzer, M.W. Lamin B1 overexpression alters chromatin organization and gene expression. Nucl. Austin Tex. 2023, 14, 2202548. [Google Scholar] [CrossRef]
- Zhao, L.; Schepp, C.L.; Iskandar, M.; Tao, Y.; Dey, M. Epigenetic regulation of immune cells in central nervous system: From steady state to pathology. Neurochem. Int. 2025, 188, 106005. [Google Scholar] [CrossRef]
- Mangiavacchi, A.; Morelli, G.; Orlando, V. Behind the scenes: How RNA orchestrates the epigenetic regulation of gene expression. Front. Cell Dev. Biol. 2023, 11, 1123975. [Google Scholar] [CrossRef]
- Ibrahim, J.; Op de Beeck, K.; Fransen, E.; Peeters, M.; Van Camp, G. Genome-wide DNA methylation profiling and identification of potential pan-cancer and tumor-specific biomarkers. Mol. Oncol. 2022, 16, 2432–2447. [Google Scholar] [CrossRef]
- Edrei, Y.; Levy, R.; Kaye, D.; Marom, A.; Radlwimmer, B.; Hellman, A. Methylation-directed regulatory networks determine enhancing and silencing of mutation disease driver genes and explain inter-patient expression variation. Genome Biol. 2023, 24, 264. [Google Scholar] [CrossRef]
- McCartney, D.L.; Min, J.L.; Richmond, R.C.; Lu, A.T.; Sobczyk, M.K.; Davies, G.; Broer, L.; Guo, X.; Jeong, A.; Jung, J.; et al. Genome-wide association studies identify 137 genetic loci for DNA methylation biomarkers of aging. Genome Biol. 2021, 22, 194. [Google Scholar] [CrossRef]
- Marei, H.E. Epigenetic regulators in cancer therapy and progression. Npj Precis. Oncol. 2025, 9, 206. [Google Scholar] [CrossRef]
- Rabaneda-Bueno, R.; Mena-Montes, B.; Torres-Castro, S.; Torres-Carrillo, N.; Torres-Carrillo, N.M. Advances in Genetics and Epigenetic Alterations in Alzheimer’s Disease: A Notion for Therapeutic Treatment. Genes 2021, 12, 1959. [Google Scholar] [CrossRef]
- van Ruiten, M.S.; van Gent, D.; Sedeño Cacciatore, Á.; Fauster, A.; Willems, L.; Hekkelman, M.L.; Hoekman, L.; Altelaar, M.; Haarhuis, J.H.I.; Brummelkamp, T.R.; et al. The cohesin acetylation cycle controls chromatin loop length through a PDS5A brake mechanism. Nat. Struct. Mol. Biol. 2022, 29, 586–591. [Google Scholar] [CrossRef]
- Khan, T.; Seetharam, A.S.; Zhou, J.; Bivens, N.J.; Schust, D.J.; Ezashi, T.; Tuteja, G.; Roberts, R.M. Single Nucleus RNA Sequence (snRNAseq) Analysis of the Spectrum of Trophoblast Lineages Generated From Human Pluripotent Stem Cells in vitro. Front. Cell Dev. Biol. 2021, 9, 695248. [Google Scholar] [CrossRef]
- Catta-Preta, R.; Lindtner, S.; Ypsilanti, A.; Seban, N.; Price, J.D.; Abnousi, A.; Su-Feher, L.; Wang, Y.; Cichewicz, K.; Boerma, S.A.; et al. Combinatorial transcription factor binding encodes cis-regulatory wiring of mouse forebrain GABAergic neurogenesis. Dev. Cell 2025, 60, 288–304.e6. [Google Scholar] [CrossRef]
- Avarlaid, A.; Falkenberg, K.; Lehe, K.; Mudò, G.; Belluardo, N.; Di Liberto, V.; Frinchi, M.; Tuvikene, J.; Timmusk, T. An upstream enhancer and MEF2 transcription factors fine-tune the regulation of the Bdnf gene in cortical and hippocampal neurons. J. Biol. Chem. 2024, 300, 107411. [Google Scholar] [CrossRef]
- Kolson, D.R.; Wan, J.; Wu, J.; Dehoff, M.; Brandebura, A.N.; Qian, J.; Mathers, P.H.; Spirou, G.A. Temporal patterns of gene expression during calyx of held development. Dev. Neurobiol. 2016, 76, 166–189. [Google Scholar] [CrossRef]
- Toader, C.; Serban, M.; Munteanu, O.; Covache-Busuioc, R.-A.; Enyedi, M.; Ciurea, A.V.; Tataru, C.P. From Synaptic Plasticity to Neurodegeneration: BDNF as a Transformative Target in Medicine. Int. J. Mol. Sci. 2025, 26, 4271. [Google Scholar] [CrossRef]
- Jin, Q.; Zuo, C.; Cui, H.; Li, L.; Yang, Y.; Dai, H.; Chen, L. Single-cell entropy network detects the activity of immune cells based on ribosomal protein genes. Comput. Struct. Biotechnol. J. 2022, 20, 3556–3566. [Google Scholar] [CrossRef]
- Dérian, N.; Pham, H.-P.; Nehar-Belaid, D.; Tchitchek, N.; Klatzmann, D.; Eric, V.; Six, A. The Tsallis generalized entropy enhances the interpretation of transcriptomics datasets. PLoS ONE 2022, 17, e0266618. [Google Scholar] [CrossRef]
- Afanasyev, A.Y.; Kim, Y.; Tolokh, I.S.; Sharakhov, I.V.; Onufriev, A.V. The probability of chromatin to be at the nuclear lamina has no systematic effect on its transcription level in fruit flies. Epigenetics Chromatin 2024, 17, 13. [Google Scholar] [CrossRef]
- Tolokh, I.S.; Kinney, N.A.; Sharakhov, I.V.; Onufriev, A.V. Strong interactions between highly dynamic lamina-associated domains and the nuclear envelope stabilize the 3D architecture of Drosophila interphase chromatin. Epigenetics Chromatin 2023, 16, 21. [Google Scholar] [CrossRef]
- McGoldrick, P.; Robertson, J. Unraveling the impact of disrupted nucleocytoplasmic transport systems in C9orf72-associated ALS. Front. Cell. Neurosci. 2023, 17, 1247297. [Google Scholar] [CrossRef]
- Feric, M.; Misteli, T. Function moves biomolecular condensates in phase space. BioEssays News Rev. Mol. Cell. Dev. Biol. 2022, 44, e2200001. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, Z.; Chen, Y.; Chen, D. Reading the m6A-encoded epitranscriptomic information in development and diseases. Cell Biosci. 2024, 14, 124. [Google Scholar] [CrossRef]
- Humphrey, J.; Emmett, W.; Fratta, P.; Isaacs, A.M.; Plagnol, V. Quantitative analysis of cryptic splicing associated with TDP-43 depletion. BMC Med. Genom. 2017, 10, 38. [Google Scholar] [CrossRef]
- Costa, S.; La Rocca, G.; Cavalieri, V. Epigenetic Regulation of Chromatin Functions by MicroRNAs and Long Noncoding RNAs and Implications in Human Diseases. Biomedicines 2025, 13, 725. [Google Scholar] [CrossRef]
- Mukamel, E.A.; Ngai, J. Perspectives on defining cell types in the brain. Curr. Opin. Neurobiol. 2019, 56, 61–68. [Google Scholar] [CrossRef]
- Chawla, A.; Nagy, C.; Turecki, G. Chromatin Profiling Techniques: Exploring the Chromatin Environment and Its Contributions to Complex Traits. Int. J. Mol. Sci. 2021, 22, 7612. [Google Scholar] [CrossRef]
- Maddhesiya, P.; Lepko, T.; Steiner-Mezzardi, A.; Schneider, J.; Schwarz, V.; Merl-Pham, J.; Berger, F.; Hauck, S.M.; Ronfani, L.; Bianchi, M.; et al. Hmgb2 improves astrocyte to neuron conversion by increasing the chromatin accessibility of genes associated with neuronal maturation in a proneuronal factor-dependent manner. Genome Biol. 2025, 26, 100. [Google Scholar] [CrossRef]
- Sun, X.; Liu, Z. Engineering CRISPR for emerging therapeutic applications. EngMedicine 2024, 1, 100035. [Google Scholar] [CrossRef]
- Azeez, S.S.; Hamad, R.S.; Hamad, B.K.; Shekha, M.S.; Bergsten, P. Advances in CRISPR-Cas technology and its applications: Revolutionising precision medicine. Front. Genome Ed. 2024, 6, 1509924. [Google Scholar] [CrossRef]
- Liang, Y. Emerging Concepts and Functions of Autophagy as a Regulator of Synaptic Components and Plasticity. Cells 2019, 8, 34. [Google Scholar] [CrossRef]
- Hipp, M.S.; Kasturi, P.; Hartl, F.U. The proteostasis network and its decline in ageing. Nat. Rev. Mol. Cell Biol. 2019, 20, 421–435. [Google Scholar] [CrossRef] [PubMed]
- Verma, K.; Verma, M.; Chaphalkar, A.; Chakraborty, K. Recent advances in understanding the role of proteostasis. Fac. Rev. 2021, 10, 72. [Google Scholar] [CrossRef]
- Marinko, J.T.; Huang, H.; Penn, W.D.; Capra, J.A.; Schlebach, J.P.; Sanders, C.R. Folding and Misfolding of Human Membrane Proteins in Health and Disease: From Single Molecules to Cellular Proteostasis. Chem. Rev. 2019, 119, 5537–5606. [Google Scholar] [CrossRef]
- Cliff, O.M.; Prokopenko, M.; Fitch, R. Minimising the Kullback–Leibler Divergence for Model Selection in Distributed Nonlinear Systems. Entropy 2018, 20, 51. [Google Scholar] [CrossRef]
- Yarbro, J.M.; Han, X.; Dasgupta, A.; Yang, K.; Liu, D.; Shrestha, H.K.; Zaman, M.; Wang, Z.; Yu, K.; Lee, D.G.; et al. Human and mouse proteomics reveals the shared pathways in Alzheimer’s disease and delayed protein turnover in the amyloidome. Nat. Commun. 2025, 16, 1533. [Google Scholar] [CrossRef]
- Anastasaki, C.; Wegscheid, M.L.; Hartigan, K.; Papke, J.B.; Kopp, N.D.; Chen, J.; Cobb, O.; Dougherty, J.D.; Gutmann, D.H. Human iPSC-Derived Neurons and Cerebral Organoids Establish Differential Effects of Germline NF1 Gene Mutations. Stem Cell Rep. 2020, 14, 541–550. [Google Scholar] [CrossRef]
- Folci, A.; Mirabella, F.; Fossati, M. Ubiquitin and Ubiquitin-Like Proteins in the Critical Equilibrium between Synapse Physiology and Intellectual Disability. eNeuro 2020, 7, ENEURO.0137-20.2020. [Google Scholar] [CrossRef] [PubMed]
- Callan, K.; Prince, C.R.; Feaga, H.A. The ribosome-associated quality control pathway supports survival in the absence of non-stop ribosome rescue factors. mBio 2024, 15, e0232224. [Google Scholar] [CrossRef]
- Kamzeeva, P.N.; Alferova, V.A.; Korshun, V.A.; Varizhuk, A.M.; Aralov, A.V. 5′-UTR G-Quadruplex-Mediated Translation Regulation in Eukaryotes: Current Understanding and Methodological Challenges. Int. J. Mol. Sci. 2025, 26, 1187. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Torraca, V.; Lyu, H.; Xiao, S.; Guo, D.; Zhou, C.; Tang, J. RUNDC1 negatively mediates the fusion of autophagosomes with lysosomes via regulating SNARE complex assembly. Autophagy 2024, 20, 454–456. [Google Scholar] [CrossRef]
- Qi, R.; Chen, X.; Li, Z.; Wang, Z.; Xiao, Z.; Li, X.; Han, Y.; Zheng, H.; Wu, Y.; Xu, Y. Tracking Chaperone-Mediated Autophagy Flux with a pH-Resistant Fluorescent Reporter. Int. J. Mol. Sci. 2025, 26, 17. [Google Scholar] [CrossRef]
- Sassano, M.L.; Felipe-Abrio, B.; Agostinis, P. ER-mitochondria contact sites; a multifaceted factory for Ca2+ signaling and lipid transport. Front. Cell Dev. Biol. 2022, 10, 988014. [Google Scholar] [CrossRef]
- Steinberger, A.E.; Tecos, M.E.; Phelps, H.M.; Rubin, D.C.; Davidson, N.O.; Guo, J.; Warner, B.W. A novel maladaptive unfolded protein response as a mechanism for small bowel resection-induced liver injury. Am. J. Physiol. Gastrointest. Liver Physiol. 2022, 323, G165–G176. [Google Scholar] [CrossRef]
- Omar, I.; Lapenna, A.; Cohen-Daniel, L.; Tirosh, B.; Berger, M. Schlafen2 mutation unravels a role for chronic ER stress in the loss of T cell quiescence. Oncotarget 2016, 7, 39396–39407. [Google Scholar] [CrossRef]
- Hanif Sayyed, U.M.; Mahalakshmi, R. Mitochondrial protein translocation machinery: From TOM structural biogenesis to functional regulation. J. Biol. Chem. 2022, 298, 101870. [Google Scholar] [CrossRef]
- Song, M.; Bai, Y.; Song, F. High-fat diet and neuroinflammation: The role of mitochondria. Pharmacol. Res. 2025, 212, 107615. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.A.; Smikle, R.; Reid, M.J.; Mizielinska, S. Altered Phase Separation and Cellular Impact in C9orf72-Linked ALS/FTD. Front. Cell. Neurosci. 2021, 15, 664151. [Google Scholar] [CrossRef]
- Yuan, L.; Mao, L.-H.; Huang, Y.-Y.; Outeiro, T.F.; Li, W.; Vieira, T.C.R.G.; Li, J.-Y. Stress granules: Emerging players in neurodegenerative diseases. Transl. Neurodegener. 2025, 14, 22. [Google Scholar] [CrossRef]
- Gan, Q.; Fan, C. Orthogonal Translation for Site-Specific Installation of Post-translational Modifications. Chem. Rev. 2024, 124, 2805–2838. [Google Scholar] [CrossRef]
- Rosdah, A.A.; Smiles, W.J.; Oakhill, J.S.; Scott, J.W.; Langendorf, C.G.; Delbridge, L.M.D.; Holien, J.K.; Lim, S.Y. New perspectives on the role of Drp1 isoforms in regulating mitochondrial pathophysiology. Pharmacol. Ther. 2020, 213, 107594. [Google Scholar] [CrossRef]
- Kim, H.; Hwang, J.; Park, C.; Park, R. Redox system and ROS-related disorders in peroxisomes. Free Radic. Res. 2024, 58, 662–675. [Google Scholar] [CrossRef]
- Adamu, A.; Li, S.; Gao, F.; Xue, G. The role of neuroinflammation in neurodegenerative diseases: Current understanding and future therapeutic targets. Front. Aging Neurosci. 2024, 16, 1347987. [Google Scholar] [CrossRef]
- Mukherjee, S. Immune gene network of neurological diseases: Multiple sclerosis (MS), Alzheimer’s disease (AD), Parkinson’s disease (PD) and Huntington’s disease (HD). Heliyon 2021, 7, e08518. [Google Scholar] [CrossRef]
- Bravo-Jimenez, M.A.; Sharma, S.; Karimi-Abdolrezaee, S. The integrated stress response in neurodegenerative diseases. Mol. Neurodegener. 2025, 20, 20. [Google Scholar] [CrossRef]
- Kunoh, S.; Nakashima, H.; Nakashima, K. Epigenetic Regulation of Neural Stem Cells in Developmental and Adult Stages. Epigenomes 2024, 8, 22. [Google Scholar] [CrossRef]
- Gupta, S.; Hui, S.P. Epigenetic Cross-Talk Between Sirt1 and Dnmt1 Promotes Axonal Regeneration After Spinal Cord Injury in Zebrafish. Mol. Neurobiol. 2025, 62, 2396–2419. [Google Scholar] [CrossRef]
- Wendimu, M.Y.; Hooks, S.B. Microglia Phenotypes in Aging and Neurodegenerative Diseases. Cells 2022, 11, 2091. [Google Scholar] [CrossRef]
- Noh, M.-Y.; Kwon, H.S.; Kwon, M.-S.; Nahm, M.; Jin, H.K.; Bae, J.; Kim, S.H. Biomarkers and therapeutic strategies targeting microglia in neurodegenerative diseases: Current status and future directions. Mol. Neurodegener. 2025, 20, 82. [Google Scholar] [CrossRef] [PubMed]
- Gędek, A.; Koziorowski, D.; Szlufik, S. Assessment of factors influencing glymphatic activity and implications for clinical medicine. Front. Neurol. 2023, 14, 1232304. [Google Scholar] [CrossRef]
- Gomolka, R.S.; Hablitz, L.M.; Mestre, H.; Giannetto, M.; Du, T.; Hauglund, N.L.; Xie, L.; Peng, W.; Martinez, P.M.; Nedergaard, M.; et al. Loss of aquaporin-4 results in glymphatic system dysfunction via brain-wide interstitial fluid stagnation. eLife 2023, 12, e82232. [Google Scholar] [CrossRef]
- Chen, S.; Wang, H.; Zhang, L.; Xi, Y.; Lu, Y.; Yu, K.; Zhu, Y.; Regina, I.; Bi, Y.; Tong, F. Glymphatic system: A self-purification circulation in brain. Front. Cell. Neurosci. 2025, 19, 1528995. [Google Scholar] [CrossRef]
- Stevanovic, M.; Drakulic, D.; Lazic, A.; Ninkovic, D.S.; Schwirtlich, M.; Mojsin, M. SOX Transcription Factors as Important Regulators of Neuronal and Glial Differentiation During Nervous System Development and Adult Neurogenesis. Front. Mol. Neurosci. 2021, 14, 654031. [Google Scholar] [CrossRef]
- Lee, D.G.; Kim, Y.-K.; Baek, K.-H. The bHLH Transcription Factors in Neural Development and Therapeutic Applications for Neurodegenerative Diseases. Int. J. Mol. Sci. 2022, 23, 13936. [Google Scholar] [CrossRef]
- Liang, S.; Zhou, J.; Yu, X.; Lu, S.; Liu, R. Neuronal conversion from glia to replenish the lost neurons. Neural Regen. Res. 2023, 19, 1446–1453. [Google Scholar] [CrossRef] [PubMed]
- Soll, L.G.; Eisen, J.N.; Vargas, K.J.; Medeiros, A.T.; Hammar, K.M.; Morgan, J.R. α-Synuclein-112 Impairs Synaptic Vesicle Recycling Consistent With Its Enhanced Membrane Binding Properties. Front. Cell Dev. Biol. 2020, 8, 00405. [Google Scholar] [CrossRef]
- Sharma, M.; Burré, J. α-Synuclein in synaptic function and dysfunction. Trends Neurosci. 2023, 46, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.-I.; Lee, G.-H.; Woo, J.-H.; Jun, I.; Kim, E.K. Reduced OPA1, Mitochondrial Fragmentation and Increased Susceptibility to Apoptosis in Granular Corneal Dystrophy Type 2 Corneal Fibroblasts. Genes 2023, 14, 566. [Google Scholar] [CrossRef]
- Wojtyniak, P.; Boratynska-Jasinska, A.; Serwach, K.; Gruszczynska-Biegala, J.; Zablocka, B.; Jaworski, J.; Kawalec, M. Mitofusin 2 Integrates Mitochondrial Network Remodelling, Mitophagy and Renewal of Respiratory Chain Proteins in Neurons after Oxygen and Glucose Deprivation. Mol. Neurobiol. 2022, 59, 6502–6518. [Google Scholar] [CrossRef]
- Liu, Q.; Lin, W.-J.; Tang, Y. New Insights into the Dysfunctions of Pericytes and Neurovascular Units in Neurodegenerative Diseases. Neurosci. Bull. 2020, 36, 1570–1572. [Google Scholar] [CrossRef]
- Roth, M.; Carlsson, R.; Buizza, C.; Enström, A.; Paul, G. Pericyte response to ischemic stroke precedes endothelial cell death and blood-brain barrier breakdown. J. Cereb. Blood Flow Metab. 2024, 45, 617–629. [Google Scholar] [CrossRef]
- Kim, J.W.; Lee, J.-Y.; Oh, M.; Lee, E.-W. An integrated view of lipid metabolism in ferroptosis revisited via lipidomic analysis. Exp. Mol. Med. 2023, 55, 1620–1631. [Google Scholar] [CrossRef]
- Ma, C.; Hu, H.; Liu, H.; Zhong, C.; Wu, B.; Lv, C.; Tian, Y. Lipotoxicity, lipid peroxidation and ferroptosis: A dilemma in cancer therapy. Cell Biol. Toxicol. 2025, 41, 75. [Google Scholar] [CrossRef]
- Khitun, A.; Slavoff, S.A. Proteomic detection and validation of translated small open reading frames. Curr. Protoc. Chem. Biol. 2019, 11, e77. [Google Scholar] [CrossRef]
- Khandia, R.; Sharma, A.; Alqahtani, T.; Alqahtani, A.M.; Asiri, Y.I.; Alqahtani, S.; Alharbi, A.M.; Kamal, M.A. Strong Selectional Forces Fine-Tune CpG Content in Genes Involved in Neurological Disorders as Revealed by Codon Usage Patterns. Front. Neurosci. 2022, 16, 887929. [Google Scholar] [CrossRef]
- Mowat, C.; Schiller, D.; Baker, K. NLRP3 activation promotes cGAS/STING signaling and antitumor immunity by colorectal cancer cells. Cancer Immunol. Immunother. CII 2025, 74, 238. [Google Scholar] [CrossRef]
- Singh, D. Astrocytic and microglial cells as the modulators of neuroinflammation in Alzheimer’s disease. J. Neuroinflamm. 2022, 19, 206. [Google Scholar] [CrossRef]
- Rothman, A.M.K.; Florentin, A.; Zink, F.; Quigley, C.; Bonneau, O.; Hemmig, R.; Hachey, A.; Rejtar, T.; Thaker, M.; Jain, R.; et al. Therapeutic potential of allosteric HECT E3 ligase inhibition. Cell 2025, 188, 2603–2620.e18. [Google Scholar] [CrossRef]
- Matta, S.K.; Kumar, A.; D’Silva, P. Mgr2 regulates mitochondrial preprotein import by associating with channel-forming Tim23 subunit. Mol. Biol. Cell 2020, 31, 1112–1123. [Google Scholar] [CrossRef]
- Jiang, Q.; Liu, J.; Huang, S.; Wang, X.-Y.; Chen, X.; Liu, G.-H.; Ye, K.; Song, W.; Masters, C.L.; Wang, J.; et al. Antiageing strategy for neurodegenerative diseases: From mechanisms to clinical advances. Signal Transduct. Target. Ther. 2025, 10, 76. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, S.; Luo, W.; Tang, J. Analysis of Cascading Failures and Recovery in Freeway Network Under the Impact of Incidents. Appl. Sci. 2025, 15, 7276. [Google Scholar] [CrossRef]
- Jhun, B.; Choi, H.; Lee, Y.; Lee, J.; Kim, C.H.; Kahng, B. Prediction and mitigation of nonlocal cascading failures using graph neural networks. Chaos Interdiscip. J. Nonlinear Sci. 2023, 33, 013115. [Google Scholar] [CrossRef]
- Schimmelpfennig, J.; Topczewski, J.; Zajkowski, W.; Jankowiak-Siuda, K. The role of the salience network in cognitive and affective deficits. Front. Hum. Neurosci. 2023, 17, 1133367. [Google Scholar] [CrossRef]
- Stocks, J.; Popuri, K.; Heywood, A.; Tosun, D.; Alpert, K.; Beg, M.F.; Rosen, H.; Wang, L. Network-wise concordance of multimodal neuroimaging features across the Alzheimer’s disease continuum. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2022, 14, e12304. [Google Scholar] [CrossRef]
- Mahfouz, A.; Huisman, S.M.H.; Lelieveldt, B.P.F.; Reinders, M.J.T. Brain transcriptome atlases: A computational perspective. Brain Struct. Funct. 2017, 222, 1557–1580. [Google Scholar] [CrossRef]
- Yang, S.; Park, J.H.; Lu, H.-C. Axonal energy metabolism, and the effects in aging and neurodegenerative diseases. Mol. Neurodegener. 2023, 18, 49. [Google Scholar] [CrossRef]
- Perdaens, O.; van Pesch, V. Should We Consider Neurodegeneration by Itself or in a Triangulation with Neuroinflammation and Demyelination? The Example of Multiple Sclerosis and Beyond. Int. J. Mol. Sci. 2024, 25, 12637. [Google Scholar] [CrossRef]
- Makarov, M.; Papa, M.; Korkotian, E. Computational Modeling of Extrasynaptic NMDA Receptors: Insights into Dendritic Signal Amplification Mechanisms. Int. J. Mol. Sci. 2024, 25, 4235. [Google Scholar] [CrossRef]
- Perez, J.D.; Dieck, S.t.; Alvarez-Castelao, B.; Tushev, G.; Chan, I.C.; Schuman, E.M. Subcellular sequencing of single neurons reveals the dendritic transcriptome of GABAergic interneurons. eLife 2021, 10, e63092. [Google Scholar] [CrossRef]
- Lu, H.; Diaz-Pier, S.; Lenz, M.; Vlachos, A. The interplay between homeostatic synaptic scaling and homeostatic structural plasticity maintains the robust firing rate of neural networks. eLife 2025, 12, RP88376. [Google Scholar] [CrossRef]
- Suárez-Ántola, R. An analytical approach to bifurcations and stability in simplified mathematical models of nuclear reactors. Prog. Nucl. Energy 2019, 114, 171–190. [Google Scholar] [CrossRef]
- Akinlaja, Y.O.; Nishiyama, A. Glial modulation of synapse development and plasticity: Oligodendrocyte precursor cells as a new player in the synaptic quintet. Front. Cell Dev. Biol. 2024, 12, 1418100. [Google Scholar] [CrossRef]
- Rangel-Gomez, M.; Alberini, C.M.; Deneen, B.; Drummond, G.T.; Manninen, T.; Sur, M.; Vicentic, A. Neuron–Glial Interactions: Implications for Plasticity, Behavior, and Cognition. J. Neurosci. 2024, 44, e1231242024. [Google Scholar] [CrossRef]
- Wu, X.; Li, L.; Zhou, B.; Wang, J.; Shao, W. Connexin 43 regulates astrocyte dysfunction and cognitive deficits in early life stress-treated mice. Exp. Brain Res. 2023, 241, 1207–1214. [Google Scholar] [CrossRef]
- Liu, W.; Zuo, C.; Chen, L.; Lan, H.; Luo, C.; Li, X.; Kemp, G.J.; Lui, S.; Suo, X.; Gong, Q. The whole-brain structural and functional connectome in Alzheimer’s disease spectrum: A multimodal Bayesian meta-analysis of graph theoretical characteristics. Neurosci. Biobehav. Rev. 2025, 174, 106174. [Google Scholar] [CrossRef]
- Orso, B.; Lorenzini, L.; Arnaldi, D.; Girtler, N.; Brugnolo, A.; Doglione, E.; Mattioli, P.; Biassoni, E.; Massa, F.; Peira, E.; et al. The Role of Hub and Spoke Regions in Theory of Mind in Early Alzheimer’s Disease and Frontotemporal Dementia. Biomedicines 2022, 10, 544. [Google Scholar] [CrossRef]
- Andrade-Talavera, Y.; Fisahn, A.; Rodríguez-Moreno, A. Timing to be precise? An overview of spike timing-dependent plasticity, brain rhythmicity, and glial cells interplay within neuronal circuits. Mol. Psychiatry 2023, 28, 2177–2188. [Google Scholar] [CrossRef]
- Mueller, B.D.; Merrill, S.A.; Watanabe, S.; Liu, P.; Niu, L.; Singh, A.; Maldonado-Catala, P.; Cherry, A.; Rich, M.S.; Silva, M.; et al. CaV1 and CaV2 calcium channels mediate the release of distinct pools of synaptic vesicles. eLife 2023, 12, e81407. [Google Scholar] [CrossRef]
- Chen, L.; Li, X.; Tjia, M.; Thapliyal, S. Homeostatic plasticity and excitation-inhibition balance: The good, the bad, and the ugly. Curr. Opin. Neurobiol. 2022, 75, 102553. [Google Scholar] [CrossRef]
- Madrazo, N.; Khattar, Z.; Powers, E.T.; Rosarda, J.D.; Wiseman, R.L. Mapping stress-responsive signaling pathways induced by mitochondrial proteostasis perturbations. Mol. Biol. Cell 2024, 35, ar74. [Google Scholar] [CrossRef]
- Bauer, R.; Gharabaghi, A. Constraints and Adaptation of Closed-Loop Neuroprosthetics for Functional Restoration. Front. Neurosci. 2017, 11, 111. [Google Scholar] [CrossRef]
- Bendahman, N.; Lotfi, D. Unveiling Influence in Networks: A Novel Centrality Metric and Comparative Analysis through Graph-Based Models. Entropy 2024, 26, 486. [Google Scholar] [CrossRef]
- van Dinther, M.; Voorter, P.H.M.; Zhang, E.; van Kuijk, S.M.J.; Jansen, J.F.A.; van Oostenbrugge, R.J.; Backes, W.H.; Staals, J. The neurovascular unit and its correlation with cognitive performance in patients with cerebral small vessel disease: A canonical correlation analysis approach. GeroScience 2024, 46, 5061–5073. [Google Scholar] [CrossRef]
- Zhong, J.; Li, G.; Lv, Z.; Chen, J.; Wang, C.; Shao, A.; Gong, Z.; Wang, J.; Liu, S.; Luo, J.; et al. Neuromodulation of Cerebral Blood Flow: A Physiological Mechanism and Methodological Review of Neurovascular Coupling. Bioengineering 2025, 12, 442. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.; Fang, L. Spatially resolved transcriptomics provide a new method for cancer research. J. Exp. Clin. Cancer Res. CR 2022, 41, 179. [Google Scholar] [CrossRef]
- Gwynne, K.; Jiang, S.; Venema, R.; Christie, V.; Boughtwood, T.; Ritha, M.; Skinner, J.; Ali, N.; Rambaldini, B.; Calma, T. Genomics and inclusion of Indigenous peoples in high income countries. Hum. Genet. 2023, 142, 1407–1416. [Google Scholar] [CrossRef]
- Hillmer, L.; Erhardt, E.B.; Caprihan, A.; Adair, J.C.; Knoefel, J.E.; Prestopnik, J.; Thompson, J.; Hobson, S.; Rosenberg, G.A. Blood-brain barrier disruption measured by albumin index correlates with inflammatory fluid biomarkers. J. Cereb. Blood Flow Metab. 2023, 43, 712–721. [Google Scholar] [CrossRef]
- Belkozhayev, A.M.; Al-Yozbaki, M.; George, A.; Niyazova, R.Y.; Sharipov, K.O.; Byrne, L.J.; Wilson, C.M. Extracellular Vesicles, Stem Cells and the Role of miRNAs in Neurodegeneration. Curr. Neuropharmacol. 2022, 20, 1450–1478. [Google Scholar] [CrossRef]
- Velmurugan, G.V.; Vekaria, H.J.; Patel, S.P.; Sullivan, P.G.; Hubbard, W.B. Astrocytic mitochondrial transfer to brain endothelial cells and pericytes in vivo increases with aging. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2024, 271678X241306054. [Google Scholar] [CrossRef]
- Palazzo, C.; Buccoliero, C.; Mola, M.G.; Abbrescia, P.; Nicchia, G.P.; Trojano, M.; Frigeri, A. AQP4ex is crucial for the anchoring of AQP4 at the astrocyte end-feet and for neuromyelitis optica antibody binding. Acta Neuropathol. Commun. 2019, 7, 51. [Google Scholar] [CrossRef]
- Sun, H.; Cao, Q.; He, X.; Du, X.; Jiang, X.; Wu, T.; Xiao, M. Melatonin Mitigates Sleep Restriction-Induced Cognitive and Glymphatic Dysfunction Via Aquaporin-4 Polarization. Mol. Neurobiol. 2025. [Google Scholar] [CrossRef]
- Yang, L.; Zhao, W.; Kan, Y.; Ren, C.; Ji, X. From Mechanisms to Medicine: Neurovascular Coupling in the Diagnosis and Treatment of Cerebrovascular Disorders: A Narrative Review. Cells 2025, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Toader, C.; Dumitru, A.V.; Eva, L.; Serban, M.; Covache-Busuioc, R.-A.; Ciurea, A.V. Nanoparticle Strategies for Treating CNS Disorders: A Comprehensive Review of Drug Delivery and Theranostic Applications. Int. J. Mol. Sci. 2024, 25, 13302. [Google Scholar] [CrossRef]
- Penna, C.; Pagliaro, P. Endothelial Dysfunction: Redox Imbalance, NLRP3 Inflammasome, and Inflammatory Responses in Cardiovascular Diseases. Antioxidants 2025, 14, 256. [Google Scholar] [CrossRef] [PubMed]
- Kral-Pointner, J.B.; Haider, P.; Szabo, P.L.; Salzmann, M.; Brekalo, M.; Schneider, K.H.; Schrottmaier, W.C.; Kaun, C.; Bleichert, S.; Kiss, A.; et al. Reduced Monocyte and Neutrophil Infiltration and Activation by P-Selectin/CD62P Inhibition Enhances Thrombus Resolution in Mice. Arterioscler. Thromb. Vasc. Biol. 2024, 44, 954–968. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Zou, Q.; Ding, X.; Shi, D.; Zhu, X.; Hu, W.; Liu, L.; Zhou, H. Complement component C3a plays a critical role in endothelial activation and leukocyte recruitment into the brain. J. Neuroinflammation 2016, 13, 23. [Google Scholar] [CrossRef]
- Behnam, V.; Rong, J.; Larson, M.G.; Gotal, J.D.; Benjamin, E.J.; Hamburg, N.M.; Vasan, R.S.; Mitchell, G.F. Windkessel Measures Derived From Pressure Waveforms Only: The Framingham Heart Study. J. Am. Heart Assoc. 2019, 8, e012300. [Google Scholar] [CrossRef]
- Schrader, L.A.; Ronnekleiv-Kelly, S.M.; Hogenesch, J.B.; Bradfield, C.A.; Malecki, K.M.C. Circadian disruption, clock genes, and metabolic health. J. Clin. Investig. 2024, 134, e170998. [Google Scholar] [CrossRef]
- Leleo, E.G.; Segev, I. Burst control: Synaptic conditions for burst generation in cortical layer 5 pyramidal neurons. PLoS Comput. Biol. 2021, 17, e1009558. [Google Scholar] [CrossRef]
- Parkin, G.M.; Udawela, M.; Gibbons, A.; Dean, B. Glutamate transporters, EAAT1 and EAAT2, are potentially important in the pathophysiology and treatment of schizophrenia and affective disorders. World J. Psychiatry 2018, 8, 51–63. [Google Scholar] [CrossRef]
- Shi, M.-Q.; Xu, Y.; Fu, X.; Pan, D.-S.; Lu, X.-P.; Xiao, Y.; Jiang, Y.-Z. Advances in targeting histone deacetylase for treatment of solid tumors. J. Hematol. Oncol. 2024, 17, 37. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.; Kuppuswamy, S.; Ledford, W.L.; Sukumari-Ramesh, S. The role of HDAC3 in inflammation: Mechanisms and therapeutic implications. Front. Immunol. 2024, 15, 1419685. [Google Scholar] [CrossRef] [PubMed]
- Yusri, K.; Jose, S.; Vermeulen, K.S.; Tan, T.C.M.; Sorrentino, V. The role of NAD+ metabolism and its modulation of mitochondria in aging and disease. Npj Metab. Health Dis. 2025, 3, 26. [Google Scholar] [CrossRef]
- Wagner, K.; Unger, L.; Salman, M.M.; Kitchen, P.; Bill, R.M.; Yool, A.J. Signaling Mechanisms and Pharmacological Modulators Governing Diverse Aquaporin Functions in Human Health and Disease. Int. J. Mol. Sci. 2022, 23, 1388. [Google Scholar] [CrossRef] [PubMed]
- Stein, R.M.; Kang, H.J.; McCorvy, J.D.; Glatfelter, G.C.; Jones, A.J.; Che, T.; Slocum, S.; Huang, X.-P.; Savych, O.; Moroz, Y.S.; et al. Virtual discovery of melatonin receptor ligands to modulate circadian rhythms. Nature 2020, 579, 609–614. [Google Scholar] [CrossRef]
- Ota, M.; Maki, H.; Takahashi, Y.; Shigemoto, Y.; Kimura, Y.; Matsuda, H.; Sato, N. Relationships between neuroimaging biomarkers and glymphatic-system activity in dementia with Lewy bodies. Neurosci. Lett. 2024, 842, 137995. [Google Scholar] [CrossRef]
- Kempuraj, D.; Dourvetakis, K.D.; Cohen, J.; Valladares, D.S.; Joshi, R.S.; Kothuru, S.P.; Anderson, T.; Chinnappan, B.; Cheema, A.K.; Klimas, N.G.; et al. Neurovascular unit, neuroinflammation and neurodegeneration markers in brain disorders. Front. Cell. Neurosci. 2024, 18, 1491952. [Google Scholar] [CrossRef]
- Iadecola, C. The neurovascular unit coming of age: A journey through neurovascular coupling in health and disease. Neuron 2017, 96, 17–42. [Google Scholar] [CrossRef]
- Xu, Y.; Yin, H.; Li, L.; Wang, X.; Hou, Q. Covert cerebrospinal fluid dynamics dysfunction: Evolution from conventional to innovative therapies. Front. Neurol. 2025, 16, 1554813. [Google Scholar] [CrossRef]
- Giannetto, M.J.; Gomolka, R.S.; Gahn-Martinez, D.; Newbold, E.J.; Bork, P.A.R.; Chang, E.; Gresser, M.; Thompson, T.; Mori, Y.; Nedergaard, M. Glymphatic fluid transport is suppressed by the AQP4 inhibitor AER-271. Glia 2024, 72, 982–998. [Google Scholar] [CrossRef]
- Arizono, M.; Nägerl, U.V. Deciphering the functional nano-anatomy of the tripartite synapse using stimulated emission depletion microscopy. Glia 2022, 70, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Daversin-Catty, C.; Vinje, V.; Mardal, K.-A.; Rognes, M.E. The mechanisms behind perivascular fluid flow. PLoS ONE 2020, 15, e0244442. [Google Scholar] [CrossRef]
- Martinac, A.D.; Bilston, L.E. Computational modelling of fluid and solute transport in the brain. Biomech. Model. Mechanobiol. 2020, 19, 781–800. [Google Scholar] [CrossRef] [PubMed]
- Hauglund, N.L.; Andersen, M.; Tokarska, K.; Radovanovic, T.; Kjaerby, C.; Sørensen, F.L.; Bojarowska, Z.; Untiet, V.; Ballestero, S.B.; Kolmos, M.G.; et al. Norepinephrine-mediated slow vasomotion drives glymphatic clearance during sleep. Cell 2025, 188, 606–622.e17. [Google Scholar] [CrossRef] [PubMed]
- Martín Jiménez, A.; Bermejo Gil, B.M.; Santos-Lozano, A.; Pinto-Fraga, F.J.; García Barroso, C.; Vittori, L.R.; Fraino, A.; Menéndez Alegre, H. Efficacy of complex decongestive therapy on venous flow, internal saphenous diameter, edema, fat mass of the limbs and quality of life in patients with chronic venous insufficiency: A randomized clinical trial. J. Vasc. Surg. Venous Lymphat. Disord. 2025, 13, 102005. [Google Scholar] [CrossRef]
- Picos, A.; Seoane, N.; Campos-Toimil, M.; Viña, D. Vascular senescence and aging: Mechanisms, clinical implications, and therapeutic prospects. Biogerontology 2025, 26, 118. [Google Scholar] [CrossRef]
- Rustenhoven, J.; Pavlou, G.; Storck, S.E.; Dykstra, T.; Du, S.; Wan, Z.; Quintero, D.; Scallan, J.P.; Smirnov, I.; Kamm, R.D.; et al. Age-related alterations in meningeal immunity drive impaired CNS lymphatic drainage. J. Exp. Med. 2023, 220, e20221929. [Google Scholar] [CrossRef]
- Denes, A.; Hansen, C.E.; Oezorhan, U.; Figuerola, S.; de Vries, H.E.; Sorokin, L.; Planas, A.M.; Engelhardt, B.; Schwaninger, M. Endothelial cells and macrophages as allies in the healthy and diseased brain. Acta Neuropathol. 2024, 147, 38. [Google Scholar] [CrossRef]
- Santiago-Balmaseda, A.; Aguirre-Orozco, A.; Valenzuela-Arzeta, I.E.; Villegas-Rojas, M.M.; Pérez-Segura, I.; Jiménez-Barrios, N.; Hurtado-Robles, E.; Rodríguez-Hernández, L.D.; Rivera-German, E.R.; Guerra-Crespo, M.; et al. Neurodegenerative Diseases: Unraveling the Heterogeneity of Astrocytes. Cells 2024, 13, 921. [Google Scholar] [CrossRef]
- Zhan, X.; Wang, S.; Bèchet, N.; Gouras, G.; Wen, G. Perivascular macrophages in the central nervous system: Insights into their roles in health and disease. Cell Death Dis. 2025, 16, 350. [Google Scholar] [CrossRef] [PubMed]
- Luz, Y.; Shamir, M. Oscillations via Spike-Timing Dependent Plasticity in a Feed-Forward Model. PLoS Comput. Biol. 2016, 12, e1004878. [Google Scholar] [CrossRef]
- Klostranec, J.M.; Vucevic, D.; Bhatia, K.D.; Kortman, H.G.J.; Krings, T.; Murphy, K.P.; terBrugge, K.G.; Mikulis, D.J. Current Concepts in Intracranial Interstitial Fluid Transport and the Glymphatic System: Part II-Imaging Techniques and Clinical Applications. Radiology 2021, 301, 516–532. [Google Scholar] [CrossRef] [PubMed]
- Taoufik, E.; Kouroupi, G.; Zygogianni, O.; Matsas, R. Synaptic dysfunction in neurodegenerative and neurodevelopmental diseases: An overview of induced pluripotent stem-cell-based disease models. Open Biol. 2018, 8, 180138. [Google Scholar] [CrossRef]
- Jiang, Y.; Li, L.; Pang, K.; Liu, J.; Chen, B.; Yuan, J.; Shen, L.; Chen, X.; Lu, B.; Han, H. Synaptic degeneration in the prefrontal cortex of a rat AD model revealed by volume electron microscopy. J. Mol. Cell Biol. 2022, 14, mjac012. [Google Scholar] [CrossRef]
- Stein, I.S.; Zito, K. Dendritic Spine Elimination: Molecular Mechanisms and Implications. Neurosci. Rev. J. Bringing Neurobiol. Neurol. Psychiatry 2019, 25, 27–47. [Google Scholar] [CrossRef]
- Youssef, H.; Weissmann, C.; Uruk, G.; Gatto, R.G. Looking into Abnormal Co-Expressions of Tau and TDP-43 in the Realm of Mixed Dementia Types: A Double-Punch Scenario. Brain Sci. 2025, 15, 716. [Google Scholar] [CrossRef]
- Han, J.; Zhang, Z.; Zhang, P.; Yu, Q.; Cheng, Q.; Lu, Z.; Zong, S. The roles of microglia and astrocytes in neuroinflammation of Alzheimer’s disease. Front. Neurosci. 2025, 19, 1575453. [Google Scholar] [CrossRef]
- Zhang, H.; Jin, Q.; Li, J.; Wang, J.; Li, M.; Yin, Q.; Li, Q.; Qi, Y.; Feng, L.; Shen, L.; et al. Astrocyte-derived complement C3 facilitated microglial phagocytosis of synapses in Staphylococcus aureus-associated neurocognitive deficits. PLoS Pathog. 2025, 21, e1013126. [Google Scholar] [CrossRef]
- Khoshkhoo, S.; Vogt, D.; Sohal, V.S. Dynamic, Cell-Type-Specific Roles for GABAergic Interneurons in a Mouse Model of Optogenetically Inducible Seizures. Neuron 2017, 93, 291–298. [Google Scholar] [CrossRef]
- Asgarian, Z.; Oliveira, M.G.; Stryjewska, A.; Maragkos, I.; Rubin, A.N.; Magno, L.; Pachnis, V.; Ghorbani, M.; Hiebert, S.W.; Denaxa, M.; et al. MTG8 interacts with LHX6 to specify cortical interneuron subtype identity. Nat. Commun. 2022, 13, 5217. [Google Scholar] [CrossRef]
- Han, S.; Cho, S.; Choi, W.; Eilbeck, K.; Coon, H.; Nho, K.; Lee, Y. Interaction of genetic variants and methylation in transcript-level expression regulation in Alzheimer’s disease by multi-omics data analysis. BMC Genom. 2025, 26, 170. [Google Scholar] [CrossRef]
- Bavarsad, M.S.; Grinberg, L.T. SV2A PET imaging in human neurodegenerative diseases. Front. Aging Neurosci. 2024, 16, 1380561. [Google Scholar] [CrossRef]
- Rozells, J.; Gavornik, J.P. Optogenetic manipulation of inhibitory interneurons can be used to validate a model of spatiotemporal sequence learning. Front. Comput. Neurosci. 2023, 17, 1198128. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Feng, L.; Wei, S.; Wang, Y.; Li, G.; Lu, Y.; Zhang, Y.; Chu, Y.; Wang, W.; Zhang, H. Antisense oligonucleotides targeting basal forebrain ATXN2 enhances spatial memory and ameliorates sleep deprivation-induced fear memory impairment in mice. Brain Behav. 2023, 13, e3013. [Google Scholar] [CrossRef]
- Pirscoveanu, D.F.V.; Olaru, D.G.; Hermann, D.M.; Doeppner, T.R.; Ghinea, F.S.; Popa-Wagner, A. Immune genes involved in synaptic plasticity during early postnatal brain development contribute to post-stroke damage in the aging male rat brain. Biogerontology 2025, 26, 60. [Google Scholar] [CrossRef] [PubMed]
- Andoh, M.; Koyama, R. Microglia regulate synaptic development and plasticity. Dev. Neurobiol. 2021, 81, 568–590. [Google Scholar] [CrossRef]
- Wang, C.; He, T.; Qin, J.; Jiao, J.; Ji, F. The roles of immune factors in neurodevelopment. Front. Cell. Neurosci. 2025, 19, 1451889. [Google Scholar] [CrossRef]
- Casanova, A.; Wevers, A.; Navarro-Ledesma, S.; Pruimboom, L. Mitochondria: It is all about energy. Front. Physiol. 2023, 14, 1114231. [Google Scholar] [CrossRef] [PubMed]
- Otero-Garcia, M.; Mahajani, S.U.; Wakhloo, D.; Tang, W.; Xue, Y.-Q.; Morabito, S.; Pan, J.; Oberhauser, J.; Madira, A.E.; Shakouri, T.; et al. Molecular signatures underlying neurofibrillary tangle susceptibility in Alzheimer’s disease. Neuron 2022, 110, 2929–2948.e8. [Google Scholar] [CrossRef]
- Zanfardino, P.; Amati, A.; Perrone, M.; Petruzzella, V. The Balance of MFN2 and OPA1 in Mitochondrial Dynamics, Cellular Homeostasis, and Disease. Biomolecules 2025, 15, 433. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, A.; Takeiwa, T.; Ikeda, K.; Inoue, S. Roles of Noncoding RNAs in Regulation of Mitochondrial Electron Transport Chain and Oxidative Phosphorylation. Int. J. Mol. Sci. 2023, 24, 9414. [Google Scholar] [CrossRef]
- Huang, M.L.-H.; Chiang, S.; Kalinowski, D.S.; Bae, D.-H.; Sahni, S.; Richardson, D.R. The Role of the Antioxidant Response in Mitochondrial Dysfunction in Degenerative Diseases: Cross-Talk between Antioxidant Defense, Autophagy, and Apoptosis. Oxid. Med. Cell. Longev. 2019, 2019, 6392763. [Google Scholar] [CrossRef]
- Lu, X.; Gong, Y.; Hu, W.; Mao, Y.; Wang, T.; Sun, Z.; Su, X.; Fu, G.; Wang, Y.; Lai, D. Ultrastructural and proteomic profiling of mitochondria-associated endoplasmic reticulum membranes reveal aging signatures in striated muscle. Cell Death Dis. 2022, 13, 296. [Google Scholar] [CrossRef]
- Roumes, H.; Pellerin, L.; Bouzier-Sore, A.-K. Astrocytes as metabolic suppliers to support neuronal activity and brain functions. Essays Biochem. 2023, 67, 27–37. [Google Scholar] [CrossRef]
- Canty, J.T.; Hensley, A.; Aslan, M.; Jack, A.; Yildiz, A. TRAK adaptors regulate the recruitment and activation of dynein and kinesin in mitochondrial transport. Nat. Commun. 2023, 14, 1376. [Google Scholar] [CrossRef]
- Zufferey, V.; Barve, A.; Parietti, E.; Belinga, L.; Bringaud, A.; Varisco, Y.; Fabbri, K.; Capotosti, F.; Bezzi, P.; Déglon, N.; et al. Extracellular PHF-tau modulates astrocyte mitochondrial dynamics and mediates neuronal connectivity. Transl. Neurodegener. 2025, 14, 13. [Google Scholar] [CrossRef]
- Lyu, Y.; Wang, T.; Huang, S.; Zhang, Z. Mitochondrial Damage-Associated Molecular Patterns and Metabolism in the Regulation of Innate Immunity. J. Innate Immun. 2023, 15, 665–679. [Google Scholar] [CrossRef]
- Poulaki, A.; Giannouli, S. Mitochondrial Lipids: From Membrane Organization to Apoptotic Facilitation. Int. J. Mol. Sci. 2022, 23, 3738. [Google Scholar] [CrossRef]
- Alshehri, B. Cytochrome c and cancer cell metabolism: A new perspective. Saudi Pharm. J. SPJ 2024, 32, 102194. [Google Scholar] [CrossRef]
- Lu, J.; Tan, M.; Cai, Q. The Warburg effect in tumor progression: Mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett. 2015, 356, 156–164. [Google Scholar] [CrossRef]
- Wang, X.; Shen, X.; Yan, Y.; Li, H. Pyruvate dehydrogenase kinases (PDKs): An overview toward clinical applications. Biosci. Rep. 2021, 41, BSR20204402. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Li, Y.; Zhao, H. Spatiotemporal metabolomic approaches to the cancer-immunity panorama: A methodological perspective. Mol. Cancer 2024, 23, 202. [Google Scholar] [CrossRef]
- Verma, M.; Lizama, B.N.; Chu, C.T. Excitotoxicity, calcium and mitochondria: A triad in synaptic neurodegeneration. Transl. Neurodegener. 2022, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Sander, P.; Gudermann, T.; Schredelseker, J. A Calcium Guard in the Outer Membrane: Is VDAC a Regulated Gatekeeper of Mitochondrial Calcium Uptake? Int. J. Mol. Sci. 2021, 22, 946. [Google Scholar] [CrossRef]
- Zhang, Y.; Qi, Y.; Gao, Y.; Chen, W.; Zhou, T.; Zang, Y.; Li, J. Astrocyte metabolism and signaling pathways in the CNS. Front. Neurosci. 2023, 17, 1217451. [Google Scholar] [CrossRef]
- Krasley, A.T.; Li, E.; Galeana, J.M.; Bulumulla, C.; Beyene, A.G.; Demirer, G.S. Carbon Nanomaterial Fluorescent Probes and Their Biological Applications. Chem. Rev. 2024, 124, 3085–3185. [Google Scholar] [CrossRef]
- Jurcau, A. Insights into the Pathogenesis of Neurodegenerative Diseases: Focus on Mitochondrial Dysfunction and Oxidative Stress. Int. J. Mol. Sci. 2021, 22, 11847. [Google Scholar] [CrossRef]
- Dave, K.M.; Dobbins, D.X.; Farinelli, M.N.; Sullivan, A.; Milosevic, J.; Stolz, D.B.; Kim, J.; Zheng, S.; Manickam, D.S. Engineering Extracellular Vesicles to Modulate Their Innate Mitochondrial Load. Cell. Mol. Bioeng. 2022, 15, 367–389. [Google Scholar] [CrossRef]
- Koumpouli, D.; Koumpouli, V.; Koutelidakis, A.E. The Gut–Brain Axis and Neurodegenerative Diseases: The Role of Nutritional Interventions Targeting the Gut Microbiome—A Systematic Review. Appl. Sci. 2025, 15, 5558. [Google Scholar] [CrossRef]
- Kadyan, S.; Park, G.; Singh, T.P.; Patoine, C.; Singar, S.; Heise, T.; Domeier, C.; Ray, C.; Kumar, M.; Behare, P.V.; et al. Microbiome-based therapeutics towards healthier aging and longevity. Genome Med. 2025, 17, 75. [Google Scholar] [CrossRef]
- Hein, Z.M.; Arbain, M.F.F.; Kumar, S.; Mehat, M.Z.; Hamid, H.A.; Che Ramli, M.D.; Che Mohd Nassir, C.M.N. Intermittent Fasting as a Neuroprotective Strategy: Gut–Brain Axis Modulation and Metabolic Reprogramming in Neurodegenerative Disorders. Nutrients 2025, 17, 2266. [Google Scholar] [CrossRef] [PubMed]
- Jagodic, A.; Krsek, A.; Schleicher, L.M.S.; Baticic, L. Microbiome Dysbiosis as a Driver of Neurodegeneration: Insights into Alzheimer’s and Parkinson’s Diseases. Gastrointest. Disord. 2025, 7, 28. [Google Scholar] [CrossRef]
- Stolfi, C.; Maresca, C.; Monteleone, G.; Laudisi, F. Implication of Intestinal Barrier Dysfunction in Gut Dysbiosis and Diseases. Biomedicines 2022, 10, 289. [Google Scholar] [CrossRef]
- Sharma, C.; Woo, H.; Kim, S.R. Addressing Blood–Brain Barrier Impairment in Alzheimer’s Disease. Biomedicines 2022, 10, 742. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez Lopez, D.E.; Lashinger, L.M.; Weinstock, G.M.; Bray, M.S. Circadian rhythms and the gut microbiome synchronize the host’s metabolic response to diet. Cell Metab. 2021, 33, 873–887. [Google Scholar] [CrossRef]
- Ren, F.; Wei, J.; Chen, Q.; Hu, M.; Yu, L.; Mi, J.; Zhou, X.; Qin, D.; Wu, J.; Wu, A. Artificial intelligence-driven multi-omics approaches in Alzheimer’s disease: Progress, challenges, and future directions. Acta Pharm. Sin. B 2025. [Google Scholar] [CrossRef]
- Temis-Cortina, J.A.; Prada-Ramírez, H.A.; Ríos-Guerra, H.; Espinosa-Raya, J.; Gómez-Pliego, R. Response of Akkermansia muciniphila to Bioactive Compounds: Effects on Its Abundance and Activity. Fermentation 2025, 11, 427. [Google Scholar] [CrossRef]
- Adil, N.A.; Omo-Erigbe, C.; Yadav, H.; Jain, S. The Oral–Gut Microbiome–Brain Axis in Cognition. Microorganisms 2025, 13, 814. [Google Scholar] [CrossRef]
- Czarnota-Łydka, K.; Kucwaj-Brysz, K.; Mordyl, B.; Głuch-Lutwin, M.; Karcz, T.; Jastrzębska-Więsek, M.; Partyka, A.; Dąbrowska, M.; Satała, G.; Sudoł-Tałaj, S.; et al. The first-in-class 1,3,5-triazine-derived dual 5-HT6R/FAAH modulators in search for potential drug against neurodegenerative diseases with cognitive impairment. Eur. J. Med. Chem. 2025, 298, 118026. [Google Scholar] [CrossRef]
- Mukerji, S.S.; Bachanová, P.; Park, H.; Rosen, L.V.; Kashlan, R.; Kivisäkk, P.; Anderson, A.M.; Chow, F.C.; Wu, K.; Dastgheyb, R.M.; et al. Plasma Neurofilament Light Chain and Glial Fibrillary Acidic Protein as Biomarkers of Cognitive Decline in People With Human Immunodeficiency Virus. J. Infect. Dis. 2025, 231, 946–956. [Google Scholar] [CrossRef]
- Axelsson, T.; Zetterberg, H.; Blennow, K.; Arslan, B.; Ashton, N.J.; Axelsson, M.; Svensson, M.K.; Saeed, A.; Guron, G. Plasma concentrations of neurofilament light, p-Tau231 and glial fibrillary acidic protein are elevated in patients with chronic kidney disease and correlate with measured glomerular filtration rate. BMC Nephrol. 2025, 26, 231. [Google Scholar] [CrossRef]
- Singh, S.; Dey, D.; Barik, D.; Mohapatra, I.; Kim, S.; Sharma, M.; Prasad, S.; Wang, P.; Singh, A.; Singh, G. Glioblastoma at the crossroads: Current understanding and future therapeutic horizons. Signal Transduct. Target. Ther. 2025, 10, 213. [Google Scholar] [CrossRef] [PubMed]
- Loushambam, B.; Yanglem, S.; Krishnaswami, V.; Kumar, M.; Vijayaraghavalu, S. Nanomedicine: Pioneering Advances in Neural Disease, Stroke and Spinal Cord Injury Treatment. Neuroglia 2025, 6, 9. [Google Scholar] [CrossRef]
- Guan, F.; Wang, R.; Yi, Z.; Luo, P.; Liu, W.; Xie, Y.; Liu, Z.; Xia, Z.; Zhang, H.; Cheng, Q. Tissue macrophages: Origin, heterogenity, biological functions, diseases and therapeutic targets. Signal Transduct. Target. Ther. 2025, 10, 93. [Google Scholar] [CrossRef] [PubMed]
- Zayani, Z.; Matinahmadi, A.; Tavakolpournegari, A.; Bidooki, S.H. Exploring Stressors: Impact on Cellular Organelles and Implications for Cellular Functions. Stresses 2025, 5, 26. [Google Scholar] [CrossRef]
- Li, C.; Yu, S.; Cui, Y. Parcellation of individual brains: From group level atlas to precise mapping. Neurosci. Biobehav. Rev. 2025, 174, 106172. [Google Scholar] [CrossRef]
- Chmiel, J.; Malinowska, A. The Influence of Circadian Rhythms on Transcranial Direct Current Stimulation (tDCS) Effects: Theoretical and Practical Considerations. Cells 2025, 14, 1152. [Google Scholar] [CrossRef]

| Decision Point Node | Converging Pathways | Upstream Stressors/Activators | Disease-Associated Genetic/Epigenetic Variants | Post-Translational Modulators | Subcellular Microdomain | Cell-Type Localization | Primary Experimental Models | Reversibility Potential | Targeting Tools/Strategies | References |
|---|---|---|---|---|---|---|---|---|---|---|
| mTORC1 Complex | PI3K/AKT, AMPK, lysosomal-autophagic loop | Hyperinsulinemia, nutrient flux, ER stress | TSC1/2, RHEB, Sestrin variants | Rag GTPases, S2448 phosphorylation, ULK1 repression | Lysosomal membrane | Neurons, astrocytes | Mouse Tsc1 cKO, 3xTg-AD, SH-SY5Y | High (context-sensitive) | Rapamycin, Sestrin mimetics, CRISPR-TFEB | [57,58] |
| GSK-3β | Wnt, insulin, neurotrophins | IRS1 inhibition, DKK1 upregulation | CTNNB1, MAPT (Tau), GSK3B methylation | Y216 phosphorylation, β-catenin degradation | Cytosol, dendritic cytoskeleton | Neurons, oligodendrocytes | APP/PS1, tau-P301L, human iPSC neurons | Intermediate | Tideglusib, Wnt agonists, lithium microdosing | [59,60,61] |
| CREB/CBP Axis | BDNF, MAPK, calcium influx | Glutamate excitotoxicity, oxidative burst | CREBBP mutations, BDNF promoter methylation | Ser133 phosphorylation, SUMOylation | Nucleoplasm, chromatin contact zones | Cortical pyramidal neurons | Aβ-treated hippocampal slices, CaMKIIα-Cre models | High | HDAC2 inhibitors, PGC1α activators | [62,63] |
| TET2 Complex | Oxidative base excision, microglial remodeling | ROS, IL-1β, DNA breaks | ALS-linked TET2 mutations, 5hmC loss | Dioxygenase oxidation, Fe2+/vitamin C dependence | Euchromatic nuclear foci | Microglia, neural progenitors | LPS microglial activation, human AD hippocampus | Moderate (early only) | TET activators, 5hmC-guided editing | [64,65,66] |
| NLRP3 Inflammasome | DAMP sensors, NF-κB, ROS | Aβ oligomers, gut-brain LPS, trauma | rs10754558 (NLRP3), miR-223 loss | ASC speck formation, Caspase-1 cleavage | Cytosol near mitochondria | Microglia, meningeal macrophages | NLRP3-GFP reporter mice, CX3CR1-CreERT2 lines | Low (post-priming) | MCC950, caspase-1 inhibitors | [67,68] |
| REST/NRSF Complex | Wnt, Notch, BDNF repression | Aging, inflammation, epigenetic drift | REST overexpression, CpG methylation, miR-124 loss | SUMOylation, MeCP2 binding | Perinucleolar chromatin domains | Hippocampal neurons, striatal interneurons | Aged mice, REST-GFP reporters, MeCP2 KO | High in early stages | REST siRNA, CoREST inhibitors | [69,70,71] |
| Tau Kinase Hub | GSK-3β, CDK5, MARK | Aβ exposure, insulin resistance | MAPT mutations, exon 10 splicing dysregulation | AT8 phospho-sites, acetylation K274 | Axoplasm, dendritic spines | Cortical layer V neurons | P301S tau mice, TBI models, CSF tau proteomics | Low | Anti-tau ASOs, pan-kinase inhibitors | [72,73] |
| MeCP2/MBD2 | Histone code–DNA methylation scaffold | ROS, metabolic instability | MECP2 duplication, Rett syndrome variants | HDAC3 tethering, phosphorylation-dependent dissociation | Nucleosome interface | Neurons, glial progenitors | MeCP2-null mice, iPSC-derived glia | Moderate | CRISPR-editing, MeCP2-stabilizing peptides | [74,75,76] |
| PINK1–Parkin Gate | Mitochondrial depolarization, calcium spikes | MPTP, ROS, dopaminergic stress | PARK2, PINK1 loss-of-function mutations | Ubiquitin phosphorylation, Mfn2 degradation | Outer mitochondrial membrane | SNpc dopaminergic neurons, astrocytes | Pink1/Parkin KO mice, iPSC-derived midbrain neurons | Moderate | Mitofusin agonists, autophagosome flux enhancers | [77,78] |
| FUS/TDP-43 Nucleocytoplasmic Shuttling | DNA damage, stress granule signaling | Oxidative DNA breaks, RNA instability | TARDBP, FUS mutations (ALS, FTD) | Phosphorylation, sumoylation, LLPS dynamics | Nucleoplasm ↔ cytosol, stress granules | Cortical and spinal motor neurons | ALS-FUS mice, iPSC neurons, C9ORF72-ALS lines | Low if LLPS already seeded | Phase separation inhibitors, nuclear transport correctors | [79,80] |
| CDK5–p25 Hyperactivation Axis | Ca2+ overload, NMDA excitotoxicity | ROS, Aβ, ischemia | p35 → p25 proteolytic shift, CDK5 mislocalization | Phosphorylation of tau, neurofilaments | Axon initial segment, perinuclear ER | Projection neurons, Purkinje cells | Ischemia models, AD postmortem cortex | Moderate | CDK5 inhibitors, calpain blockade | [81,82] |
| Dicer/miRNA Processing Node | miRNA biogenesis, synaptic plasticity | Inflammation, nuclear–cytoplasmic transport dysfunction | DICER1 loss in ALS, miRNA-132 repression | Phosphorylation, Dicer–TRBP interaction | Cytoplasmic P-bodies | Neurons, astrocytes, NSCs | Dicer KO models, Drosha-DGCR8 pathway studies | High (if early) | miRNA mimics, Dicer stabilization peptides | [83,84] |
| Lamin B1–Nuclear Scaffold Axis | Heterochromatin maintenance, nuclear integrity | Aging, oxidative damage, histone loss | LMNB1 overexpression in AD, epigenetic erosion | Phosphorylation, caspase cleavage | Nuclear lamina, chromatin contact zones | Neurons, OPCs, ependymal cells | Human AD tissue, lamin-deficient models | Low if fragmentation present | Lamin stabilizers, nuclear membrane chaperones | [85,86] |
| Regulatory Axis | Primary Failure Mode | Representative Disorders | Triggering Vulnerabilities | Biological Interface Affected | Omics-Derived Markers/Readouts | Regulatory Buffers/Adaptive Nodes | Precision Restoration Vectors | References |
|---|---|---|---|---|---|---|---|---|
| Signal Integration Collapse | Temporal desynchronization of intracellular pathways; feedback breakdown | AD, PD, ALS, HD | Oxidative stress, Aβ, cytokine storms | Neuron–glia axis | Phospho-proteomics; scRNA-seq signaling clusters | PTEN, IRS-1, phosphatases, CaMKII | CRISPR logic circuits; mTOR auto-tuners | [136,137,138] |
| Epigenetic Drift and Noise Amplification | Cell identity erosion; enhancer–promoter detachment | AD, ALS, FTD | Inflammation, chromatin erosion, tau | Transcriptional hubs | ATAC-seq entropy, MeCP2 loss, histone code shifts | DNMT1/3A, REST, SIRT1, CTCF | dCas9 editing, chromatin loop reweaving | [139,140] |
| Immune Regulation Failure | Chronic glial activation, failure of resolution pathways | AD, PD, ALS | Mito-DAMPs, APOE4, lipid imbalance | Microglia, astrocytes | scRNA-seq glial state trajectories; cytokine proteomics | TREM2, PPARγ, IL-10 | TREM2 agonists, NLRP3 inhibitors, CD33 modulation | [141,142] |
| Proteostasis–Glymphatic Collapse | Clearance pathway overload; AQP4 polarity loss | AD, ALS, CAA | Tauopathy, ER stress, venous outflow failure | Interstitial matrix, astrocytic endfeet | Spatial proteomics; AQP4 mislocalization maps | TFEB, LAMP2A, HSPs, AQP4/α-syntrophin | AAV-TFEB, sleep-timed drainage therapies | [143,144,145] |
| Degenerative Fate Lock-in | Terminal glial or hybrid cell states; loss of neurogenic potential | ALS, PD, MS | NF-κB loops, Notch dysregulation, chromatin closure | Spatially restricted glial niches | Pseudotime bifurcation (scRNA-seq); trajectory fate traps | REST, Sox2, bHLH TFs, lamins | Astrocyte-to-neuron reprogramming; spatial CRISPR tools | [146,147,148] |
| Synaptic Vesicle Regulation Failure | Loss of vesicle cycling, endocytosis; neurotransmission collapse | ALS, PD, FTD | SNARE dysfunction, vesicle acidification, α-synuclein | Pre-/post-synaptic terminals | Synaptic proteome decay; VGLUT misexpression | Synaptotagmin, dynamin, Rab3A, Munc18 | SV2A stabilizers, SNARE complex stabilizers | [149,150] |
| Mitochondrial Network Collapse | Fragmentation, fusion–fission imbalance, ROS overflow | ALS, PD, AD | PINK1/Parkin loss, calcium overload, mtDNA damage | Soma, axon terminals, astrocytes | Mito-tracker imaging; OXPHOS transcript depletion | MFN2, DRP1, SIRT3, OPA1 | Mitofusin activators, NAD+ boosters, mitochondrial editing | [151,152] |
| Neurovascular Uncoupling | BBB breakdown, endothelial de-differentiation | AD, MS, stroke | Pericyte loss, chronic inflammation, hypoxia | Endothelium, perivascular glia | Spatial transcriptomics (CLDN5 loss); leakage assays | ZO-1, claudins, PDGFRβ, VEGF-A | AAV-mediated BBB repair; zonulin inhibitors | [153,154] |
| Lipidomic Disintegration | Lipid raft destabilization, myelin loss, peroxidation cascades | AD, MS, ALS | Cholesterol efflux imbalance, ferroptosis | Membranes, myelin, ER | Lipidomics; ferroptosis transcriptomics | ApoE, ABCA1, GPX4, PLA2 | Ferroptosis inhibitors, lipidome modulators | [155,156] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voicu, V.; Toader, C.; Șerban, M.; Covache-Busuioc, R.-A.; Ciurea, A.V. Systemic Neurodegeneration and Brain Aging: Multi-Omics Disintegration, Proteostatic Collapse, and Network Failure Across the CNS. Biomedicines 2025, 13, 2025. https://doi.org/10.3390/biomedicines13082025
Voicu V, Toader C, Șerban M, Covache-Busuioc R-A, Ciurea AV. Systemic Neurodegeneration and Brain Aging: Multi-Omics Disintegration, Proteostatic Collapse, and Network Failure Across the CNS. Biomedicines. 2025; 13(8):2025. https://doi.org/10.3390/biomedicines13082025
Chicago/Turabian StyleVoicu, Victor, Corneliu Toader, Matei Șerban, Răzvan-Adrian Covache-Busuioc, and Alexandru Vlad Ciurea. 2025. "Systemic Neurodegeneration and Brain Aging: Multi-Omics Disintegration, Proteostatic Collapse, and Network Failure Across the CNS" Biomedicines 13, no. 8: 2025. https://doi.org/10.3390/biomedicines13082025
APA StyleVoicu, V., Toader, C., Șerban, M., Covache-Busuioc, R.-A., & Ciurea, A. V. (2025). Systemic Neurodegeneration and Brain Aging: Multi-Omics Disintegration, Proteostatic Collapse, and Network Failure Across the CNS. Biomedicines, 13(8), 2025. https://doi.org/10.3390/biomedicines13082025





