The Effects of Adipose Tissue Dysregulation on Type 2 Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
3. Overview of T2DM
3.1. Disease Description and Pathophysiology of T2DM
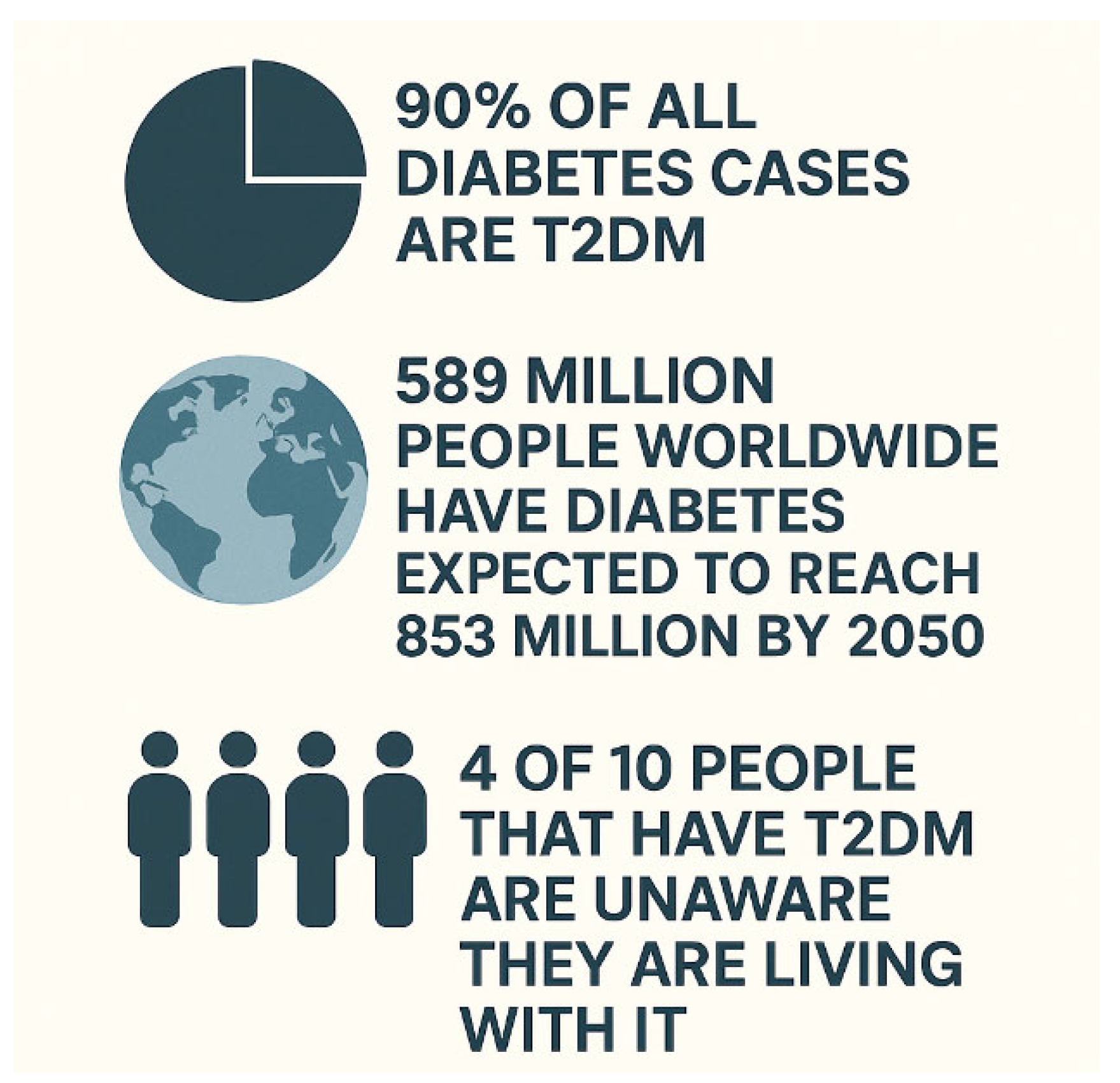
3.2. Prevalence and Influence on Public Health
4. Role of Adipose Tissue in Metabolic Regulation
4.1. Functions of Adipose Tissue
4.1.1. Normal Adipose Tissue Function
4.1.2. Dysregulation Mechanisms
4.1.3. Preventing ATD
5. Inflammatory Responses and Insulin Signaling Pathways
6. Clinical Implications of ATD in T2DM
7. Leptin in T2DM
7.1. Leptin Physiology—Normal Function
7.2. Leptin Pathophysiology—Dysregulation
7.3. Therapeutic Implications - Leptin
8. Adiponectin in T2DM
8.1. Adiponectin Physiology—Normal Function
8.2. Adiponectin Pathophysiology—Dysregulation
8.3. Therapeutic Implications - Adiponectin
9. Leptin-to-Adiponectin Ratio (LAR) in T2DM
9.1. Physiology—Normal Function
9.2. Pathophysiology—Dysregulation
9.3. Therapeutic Implications
10. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| T2DM | Type 2 Diabetes Mellitus |
| ATD | Adipose Tissue Dysregulation |
| T1DM | Type 1 Diabetes Mellitus |
| HbA1c | Glycated Hemoglobin |
| IDF | International Diabetes Federation |
| SDI | Sociodemographic Index |
| LAR | Leptin-to-Adiponectin Ratio |
| BMI | Body Mass Index |
| TNF | Tumor Necrosis Factor |
| IL | Interleukin |
| ATMs | Adipose Tissue Macrophages |
| ER | Endoplasmic Reticulum |
| FFA | Free Fatty Acids |
| HIF | Hypoxia-Inducible Factor |
| NF-KB | Nuclear Factor Kappa-light-chain-enhancer of activated B cell |
| JNK | c-Jun N-terminal Kinase |
| TLR | Toll-Like Receptor |
| SOCS | Suppressor Of Cytokine Signaling |
| AMPK | AMP-activated protein Kinase |
| PI3K/AKT | Phosphoinositide 3-kinese and protein kinase B |
| IRS | Insulin Receptor Substrate |
| TZDs | Thiazolidinediones |
| SGLT2 | Sodium-Glucose cotransporter-2s |
| GIPs | Gastric Inhibitory Polypeptides |
| GLP-1s | Glucagon-like Peptide 1s |
| ACE | Angiotensin-Converting Enzyme |
| ARB | Angiotensin Receptor Blocker |
References
- Muir, L.A.; Neeley, C.K.; Meyer, K.A.; Baker, N.A.; Brosius, A.M.; Washabaugh, A.R.; Varban, O.A.; Finks, J.F.; Zamarron, B.F.; Flesher, C.G.; et al. Adipose tissue fibrosis, hypertrophy, and hyperplasia: Correlations with diabetes in human obesity. Obesity 2016, 24, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Hajer, G.R.; Van Haeften, T.W.; Visseren, F.L. Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur. Heart J. 2008, 29, 2959–2971. [Google Scholar] [CrossRef] [PubMed]
- Björntorp, P. The Associations between Obesity, Adipose Tissue Distribution and Disease. J. Intern. Med. 1987, 222, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Björntorp, P. “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis 1990, 10, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Wozniak, S.E.; Gee, L.L.; Wachtel, M.S.; Frezza, E.E. Adipose Tissue: The New Endocrine Organ? A Review Article. Dig. Dis. Sci. 2009, 54, 1847–1856. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Vela, M.E.F.; Torres, N.; Tovar, A.R. White adipose tissue as endocrine organ and its role in obesity. Arch. Med. Res. 2008, 39, 715–728. [Google Scholar] [CrossRef] [PubMed]
- Kershaw, E.E.; Flier, J.S. Adipose tissue as an endocrine organ. J. Clin. Endocrinol. Metab. 2004, 89, 2548–2556. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Alaniz, M.H.; Takada, J.; Alonso-Vale, M.I.C.; Lima, F.B. Adipose tissue as an endocrine organ: From theory to practice. J. Pediatr. 2007, 83, S192–S203. [Google Scholar] [CrossRef]
- Papakonstantinou, E.; Oikonomou, C.; Nychas, G.; Dimitriadis, G.D. Effects of Diet, Lifestyle, Chrononutrition and Alternative Dietary Interventions on Postprandial Glycemia and Insulin Resistance. Nutrients 2022, 14, 823. [Google Scholar] [CrossRef] [PubMed]
- Remesar, X.; Alemany, M. Dietary Energy Partition: The Central Role of Glucose. Int. J. Mol. Sci. 2020, 21, 7729. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.L.; Gong, Y.; Qi, Y.J.; Shao, Z.M.; Jiang, Y.Z. Effects of dietary intervention on human diseases: Molecular mechanisms and therapeutic potential. Signal Transduct. Target. Ther. 2024, 9, 59. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Jiang, W.; Guo, S. Regulation of Macronutrients in Insulin Resistance and Glucose Homeostasis during Type 2 Diabetes Mellitus. Nutrients 2023, 15, 4671. [Google Scholar] [CrossRef] [PubMed]
- Soo, J.; Raman, A.; Lawler, N.G.; Goods, P.S.R.; Deldicque, L.; Girard, O.; Fairchild, T.J. The role of exercise and hypoxia on glucose transport and regulation. Eur. J. Appl. Physiol. 2023, 123, 1147–1165. [Google Scholar] [CrossRef] [PubMed]
- Tucker, J.A.L.; Bornath, D.P.D.; McCarthy, S.F.; Hazell, T.J. Leptin and energy balance: Exploring Leptin’s role in the regulation of energy intake and energy expenditure. Nutr. Neurosci. 2024, 27, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Obradovic, M.; Sudar-Milovanovic, E.; Soskic, S.; Essack, M.; Arya, S.; Stewart, A.J.; Gojobori, T.; Isenovic, E.R. Leptin and Obesity: Role and Clinical Implication. Front. Endocrinol. 2021, 12, 585887. [Google Scholar] [CrossRef] [PubMed]
- Martelli, D.; Brooks, V.L. Leptin Increases: Physiological Roles in the Control of Sympathetic Nerve Activity, Energy Balance, and the Hypothalamic–Pituitary–Thyroid Axis. Int. J. Mol. Sci. 2023, 24, 2684. [Google Scholar] [CrossRef] [PubMed]
- Grannell, A.; Kokkinos, A.; le Roux, C.W. Myokines in Appetite Control and Energy Balance. Muscles 2022, 1, 26–47. [Google Scholar] [CrossRef]
- Hatami Marbini, M.; Amiri, F.; Sajadi Hezaveh, Z. Dietary glycemic index, glycemic load, insulin index, insulin load and risk of diabetes-related cancers: A systematic review of cohort studies. Clin. Nutr. ESPEN 2021, 42, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Kirichenko, T.V.; Markina, Y.V.; Bogatyreva, A.I.; Tolstik, T.V.; Varaeva, Y.R.; Starodubova, A.V. The role of adipokines in inflammatory mechanisms of obesity. Int. J. Mol. Sci. 2022, 23, 14982. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.N.; Jung, C.H. The role of anti-inflammatory adipokines in cardiometabolic disorders: Moving beyond adiponectin. Int. J. Mol. Sci. 2021, 22, 13529. [Google Scholar] [CrossRef] [PubMed]
- Begum, M.; Choubey, M.; Tirumalasetty, M.B.; Arbee, S.; Mohib, M.M.; Wahiduzzaman; Mamun, M.A.; Uddin, M.B.; Mohiuddin, M.S. Adiponectin: A promising target for the treatment of diabetes and its complications. Life 2023, 13, 2213. [Google Scholar] [CrossRef] [PubMed]
- Engin, A. (Ed.) Adiponectin Resistance in Obesity: Adiponectin Leptin/Insulin Interaction. In Advances in Experimental Medicine and Biology; Springer International Publishing: Berlin/Heidelberg, Germany, 2024; pp. 431–462. [Google Scholar]
- Ozkan, E.A.; Sadigov, A.; Oztürk, O. Evaluation of serum omentin-1, vaspin, leptin, adiponectin levels in obese/overweight children and their relationship with non-alcoholic fatty liver disease. Clin. Nutr. Res. 2022, 11, 194. [Google Scholar] [CrossRef] [PubMed]
- Kunz, H.E.; Hart, C.R.; Gries, K.J.; Parvizi, M.; Laurenti, M.; Man, C.D.; Moore, N.; Zhang, X.; Ryan, Z.; Polley, E.C.; et al. Adipose tissue macrophage populations and inflammation are associated with systemic inflammation and insulin resistance in obesity. Am. J. Physiol.-Endocrinol. Metab. 2021, 321, E105–E121. [Google Scholar] [CrossRef] [PubMed]
- Lipke, K.; Kubis-Kubiak, A.; Piwowar, A. Molecular mechanism of lipotoxicity as an interesting aspect in the development of pathological states—Current view of knowledge. Cells 2022, 11, 844. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.; Wanasinghe, A.I.; Brunori, P.; Santosa, S. Is Adipose Tissue Inflammation the Culprit of Obesity-Associated Comorbidities? Obes. Rev. 2025, e13956. [Google Scholar] [CrossRef] [PubMed]
- Savova, M.S.; Mihaylova, L.V.; Tews, D.; Wabitsch, M.; Georgiev, M.I. Targeting PI3K/AKT signaling pathway in obesity. Biomed. Pharmacother. 2023, 159, 114244. [Google Scholar] [CrossRef] [PubMed]
- Engin, A. Adipose Tissue Hypoxia in Obesity: Clinical Reappraisal of Hypoxia Hypothesis. In Obesity and Lipotoxicity; Engin, A.B., Engin, A., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2024; pp. 329–356. [Google Scholar]
- Guo, Q.; Jin, Y.; Chen, X.; Ye, X.; Shen, X.; Lin, M.; Zeng, C.; Zhou, T.; Zhang, J. NF-κB in biology and targeted therapy: New insights and translational implications. Signal Transduct. Target. Ther. 2024, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; An, X.; Yang, C.; Sun, W.; Ji, H.; Lian, F. The crucial role and mechanism of insulin resistance in metabolic disease. Front. Endocrinol. 2023, 14, 1149239. [Google Scholar] [CrossRef] [PubMed]
- Berbudi, A.; Khairani, S.; Tjahjadi, A.I. Interplay Between Insulin Resistance and Immune Dysregulation in Type 2 Diabetes Mellitus: Implications for Therapeutic Interventions. Immunotargets Ther. 2025, 14, 359–382. [Google Scholar] [CrossRef] [PubMed]
- García-Macedo, R.; de los Ángeles Fortis, M. The Immune System and Inflammation in Type 2 Diabetes. In The Diabetes Textbook: Clinical Principles, Patient Management and Public Health Issues; Rodriguez-Saldana, J., Ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2023; pp. 171–196. [Google Scholar]
- Wang, K.; Wang, Y.-Y.; Wu, L.-L.; Jiang, L.-Y.; Hu, Y.; Xiao, X.-H.; Wang, Y.-D. Paracrine Regulation of Adipose Tissue Macrophages by Their Neighbors in the Microenvironment of Obese Adipose Tissue. Endocrinology 2022, 163, bqac062. [Google Scholar] [CrossRef] [PubMed]
- Engin, A. The Mechanism of Leptin Resistance in Obesity and Therapeutic Perspective. In Obesity and Lipotoxicity; Engin, A.B., Engin, A., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Berlin/Heidelberg, Germany, 2024; Volume 1460, pp. 463–487. [Google Scholar]
- Pan, D.; Li, G.; Jiang, C.; Hu, J.; Hu, X. Regulatory mechanisms of macrophage polarization in adipose tissue. Front. Immunol. 2023, 14, 1149366. [Google Scholar] [CrossRef] [PubMed]
- da Silva Rosa, S.C.; Nayak, N.; Caymo, A.M.; Gordon, J.W. Mechanisms of muscle insulin resistance and the cross-talk with liver and adipose tissue. Physiol. Rep. 2020, 8, e14607. [Google Scholar] [CrossRef] [PubMed]
- Hemat Jouy, S.; Mohan, S.; Scichilone, G.; Mostafa, A.; Mahmoud, A.M. Adipokines in the Crosstalk between Adipose Tissues and Other Organs: Implications in Cardiometabolic Diseases. Biomedicines 2024, 12, 2129. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef] [PubMed]
- Chait, A.; Den Hartigh, L.J. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front. Cardiovasc. Med. 2020, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Burhans, M.S.; Hagman, D.K.; Kuzma, J.N.; Schmidt, K.A.; Kratz, M. Contribution of Adipose Tissue Inflammation to the Development of Type 2 Diabetes Mellitus. Compr. Physiol. 2018, 9, 1–58. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Qi, Y.; Yi, H.; Mao, C.; Meng, Q.; Wang, H.; Zheng, C. The Roles of Adipose Tissue Macrophages in Human Disease. Front. Immunol. 2022, 13, 908749. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Redondo-Flórez, L.; Beltrán-Velasco, A.I.; Martín-Rodríguez, A.; Martínez-Guardado, I.; Navarro-Jiménez, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Role of Adipokines in Health and Disease. Biomedicines 2023, 11, 1290. [Google Scholar] [CrossRef] [PubMed]
- Waddell, T.; Bagur, A.; Cunha, D.; Thomaides-Brears, H.; Banerjee, R.; Cuthbertson, D.J.; Brown, E.; Cusi, K.; Després, J.; Brady, M. Greater ectopic fat deposition and liver fibroinflammation and lower skeletal muscle mass in people with type 2 diabetes. Obesity 2022, 30, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Verhaegen, A.; Van Gaal, L.F. (Eds.) Obesity, Ectopic Fat and Type 2 Diabetes. In Clinical Obesity in Adults and Children, 1st ed.; Wiley: Hoboken, NJ, USA, 2022; pp. 129–147. [Google Scholar]
- Edin, C.; Ekstedt, M.; Scheffel, T.; Karlsson, M.; Swahn, E.; Östgren, C.J.; Engvall, J.; Ebbers, T.; Leinhard, O.D.; Lundberg, P.; et al. Ectopic fat is associated with cardiac remodeling—A comprehensive assessment of regional fat depots in type 2 diabetes using multi-parametric, M.R.I. Front. Cardiovasc. Med. 2022, 9, 813427. [Google Scholar] [CrossRef] [PubMed]
- Mokdad, A.H.; Ford, E.S.; Bowman, B.A.; Dietz, W.H.; Vinicor, F.; Bales, V.S.; Marks, J.S. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003, 289, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.S.; Armstrong, S.C.; Michalsky, M.P.; Fox, C.K. Obesity in adolescents: A review. J. Am. Med. Assoc. 2024, 332, 738–748. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Diabetes Basics. U.S. Centers for Disease Control and Prevention. 2024. Available online: https://www.cdc.gov/diabetes/about/index.html (accessed on 24 September 2024).
- Xourafa, G.; Korbmacher, M.; Roden, M. Inter-organ crosstalk during development and progression of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2024, 20, 27–49. [Google Scholar] [CrossRef] [PubMed]
- Tokhirovna, E.G. Study of clinical characteristics of patients with type 2 diabetes mellitus in middle and old age. J. Sci. Med. Life 2023, 1, 16–19. [Google Scholar]
- Su, J.; Luo, Y.; Hu, S.; Tang, L.; Ouyang, S. Advances in research on type 2 diabetes mellitus targets and therapeutic agents. Int. J. Mol. Sci. 2023, 24, 13381. [Google Scholar] [CrossRef] [PubMed]
- Ruze, R.; Liu, T.; Zou, X.; Song, J.; Chen, Y.; Xu, R.; Yin, X.; Xu, Q. Obesity and type 2 diabetes mellitus: Connections in epidemiology, pathogenesis, and treatments. Front. Endocrinol. 2023, 14, 1161521. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, P.; Weiskirchen, R. The role of obesity in type 2 diabetes mellitus—An overview. Int. J. Mol. Sci. 2024, 25, 1882. [Google Scholar] [CrossRef] [PubMed]
- Yen, H.Y.; Lee, S.C.; Lin, C.F.; Lee, T.I.; Yamaguchi, Y.; Lee, P.H. Complications and comorbidities as influencing factors of health outcomes in older adults with type 2 diabetes mellitus. Collegian 2023, 30, 230–235. [Google Scholar] [CrossRef]
- Shuvo, S.D.; Hossen, M.T.; Riazuddin, M.; Hossain, M.S.; Mazumdar, S.; Parvin, R.; Elahi, M.T. Prevalence of comorbidities and its associated factors among type-2 diabetes patients: A hospital-based study in Jashore District, Bangladesh. BMJ Open 2023, 13, e076261. [Google Scholar] [CrossRef] [PubMed]
- Cao, F.; Yang, M.; Cheng, Y.; Zhang, X.; Shi, L.; Li, N. Correlation analysis of monocyte chemoattractant protein-1 and clinical characteristics and cognitive impairment in type 2 diabetes mellitus comorbid major depressive disorder. Front. Aging Neurosci. 2023, 15, 1081393. [Google Scholar] [CrossRef] [PubMed]
- Salama, M.; Biggs, B.K.; Creo, A.; Prissel, R.; Al Nofal, A.; Kumar, S. Adolescents with Type 2 Diabetes: Overcoming Barriers to Effective Weight Management. Diabetes Metab. Syndr. Obes. 2023, 16, 693–711. [Google Scholar] [CrossRef] [PubMed]
- Mazrouei, S.; Petry, S.F.; Sharifpanah, F.; Javanmard, S.H.; Kelishadi, R.; Schulze, P.C.; Franz, M.; Jung, C. Pathophysiological correlation of arginase-1 in development of type 2 diabetes from obesity in adolescents. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2023, 1867, 130263. [Google Scholar] [CrossRef] [PubMed]
- Skrypnik, K.; Suliburska, J.; Skrypnik, D.; Pilarski, Ł.; Reguła, J.; Bogdański, P. The genetic basis of obesity complications. Acta Sci. Pol. Technol. Aliment. 2017, 16, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shi, J.; Ma, Y.; Yu, N.; Zheng, P.; Chen, Z.; Wang, T.; Jia, G. Association between Air Pollution and Lipid Profiles. Toxics 2023, 11, 894. [Google Scholar] [CrossRef] [PubMed]
- Beulens, J.W.J.; Pinho, M.G.M.; Abreu, T.C.; Braver, N.R.D.; Lam, T.M.; Huss, A.; Vlaanderen, J.; Sonnenschein, T.; Siddiqui, N.Z.; Yuan, Z.; et al. Environmental risk factors of type 2 diabetes-an exposome approach. Diabetologia 2022, 65, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; Wu, Y.; Yang, S.; Zhu, D.; Chen, F.; Chen, J.; Ji, X.; Hou, K. The global, regional and national burden of Type 2 Diabetes Mellitus in the past, present and future: A systematic analysis of the Global Burden of Disease Study 2019. Front. Endocrinol. 2023, 14, 1192629. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2021, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. Facts & Figures. 2025. Available online: https://idf.org/about-diabetes/diabetes-facts-figures/ (accessed on 23 June 2025).
- Institute for Health Metrics and Evaluation. Global Burden of Disease (GBD). 2021. Available online: https://www.healthdata.org/research-analysis/about-gbd (accessed on 14 November 2024).
- Monteiro, C.A.; Moubarac, J.-C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Yao, Y.; Yang, G.; Wang, X.; Vejre, H. Strong contribution of rapid urbanization and urban agglomeration development to regional thermal environment dynamics and evolution. For. Ecol. Manag. 2019, 446, 214–225. [Google Scholar] [CrossRef]
- Xiong, Y.; Huang, S.; Chen, F.; Ye, H.; Wang, C.; Zhu, C. The impacts of rapid urbanization on the thermal environment: A remote sensing study of Guangzhou, South China. Remote Sens. 2012, 4, 2033–2056. [Google Scholar] [CrossRef]
- Khan, M.A.B.; Hashim, M.J.; King, J.K.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Richard, A.J.; White, U.; Elks, C.M.; Stephens, J.M. Adipose Tissue: Physiology to Metabolic Dysfunction. Endotext [Internet]. Published Online 2020. Available online: https://www.ncbi.nlm.nih.gov/sites/books/NBK555602/ (accessed on 3 December 2024).
- Koenen, M.; Hill, M.A.; Cohen, P.; Sowers, J.R. Obesity, Adipose Tissue and Vascular Dysfunction. Circ. Res. 2021, 128, 951–968. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol. Cell Physiol. 2021, 320, C375–C391. [Google Scholar] [CrossRef] [PubMed]
- Antuna-Puente, B.; Feve, B.; Fellahi, S.; Bastard, J.P. Adipokines: The missing link between insulin resistance and obesity. Diabetes Metab. 2008, 34, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Harvey, I.; Boudreau, A.; Stephens, J.M. Adipose tissue in health and disease. Open Biol. 2020, 10, 200291. [Google Scholar] [CrossRef] [PubMed]
- Cleveland Clinic. What Is Leptin? Cleveland Clinic. 2025. Available online: https://my.clevelandclinic.org/health/body/22446-leptin (accessed on 13 May 2025).
- Cleveland Clinic. What Is Adiponectin? Cleveland Clinic. 2025. Available online: https://my.clevelandclinic.org/health/articles/22439-adiponectin (accessed on 13 May 2025).
- Otero, M.; Lago, R.; Gómez, R.; Lago, F.; Gómez-Reino, J.J.; Gualillo, O. Leptin: A metabolic hormone that functions like a proinflammatory adipokine. Drug News Perspect. 2006, 19, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Fantuzzi, G. Adiponectin and inflammation: Consensus and controversy. J. Allergy Clin. Immunol. 2008, 121, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, T.; Galiero, R.; Caturano, A.; Vetrano, E.; Rinaldi, L.; Coviello, F.; Di Martino, A.; Albanese, G.; Colantuoni, S.; Medicamento, G.; et al. Dysregulated Epicardial Adipose Tissue as a Risk Factor and Potential Therapeutic Target of Heart Failure with Preserved Ejection Fraction in Diabetes. Biomolecules 2022, 12, 176. [Google Scholar] [CrossRef] [PubMed]
- Menendez, A.; Wanczyk, H.; Walker, J.; Zhou, B.; Santos, M.; Finck, C. Obesity and adipose tissue dysfunction: From pediatrics to adults. Genes 2022, 13, 1866. [Google Scholar] [CrossRef] [PubMed]
- Atakan, M.M.; Koşar, Ş.N.; Güzel, Y.; Tin, H.T.; Yan, X. The role of exercise, diet, and cytokines in preventing obesity and improving adipose tissue. Nutrients 2021, 13, 1459. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xu, M.; Li, Y. Adipose tissue aging and metabolic disorder, and the impact of nutritional interventions. Nutrients 2022, 14, 3134. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Verduci, E.; Ghezzi, M.; Cena, H.; Pascuzzi, M.C.; Regalbuto, C.; Lamberti, R.; Rossi, V.; Manuelli, M.; Bosetti, A.; et al. Pediatric obesity-related asthma: The role of nutrition and nutrients in prevention and treatment. Nutrients 2021, 13, 3708. [Google Scholar] [CrossRef] [PubMed]
- Meister, B.M.; Hong, S.G.; Shin, J.; Rath, M.; Sayoc, J.; Park, J.Y. Healthy versus unhealthy adipose tissue expansion: The role of exercise. J. Obes. Metab. Syndr. 2022, 31, 37. [Google Scholar] [CrossRef] [PubMed]
- Abedpoor, N.; Taghian, F.; Hajibabaie, F. Physical activity ameliorates the function of organs via adipose tissue in metabolic diseases. Acta Histochem. 2022, 124, 151844. [Google Scholar] [CrossRef] [PubMed]
- Babaei, Z.; Moslemi, D.; Parsian, H.; Khafri, S.; Pouramir, M.; Mosapour, A. Relationship of obesity with serum concentrations of leptin, CRP and IL-6 in breast cancer survivors. J. Egypt. Natl. Cancer Inst. 2015, 27, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Winn, N.C.; Cottam, M.A.; Wasserman, D.H.; Hasty, A.H. Exercise and Adipose Tissue Immunity: Outrunning Inflammation. Obesity 2021, 29, 790–801. [Google Scholar] [CrossRef] [PubMed]
- Rafey, M.F.; Abdalgwad, R.; O’Shea, P.M.; Foy, S.; Claffey, B.; Davenport, C.; O’Keeffe, D.T.; Finucane, F.M. Changes in the Leptin to Adiponectin Ratio Are Proportional to Weight Loss After Meal Replacement in Adults with Severe Obesity. Front. Nutr. 2022, 9, 845574. [Google Scholar] [CrossRef] [PubMed]
- Samovski, D.; Smith, G.I.; Palacios, H.; Pietka, T.; Fuchs, A.; Patti, G.J.; Nawaz, A.; Kahn, C.R.; Klein, S. Effect of Marked Weight Loss on Adipose Tissue Biology in People with Obesity and Type 2 Diabetes. Diabetes Care 2025, dc242739. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Chen, Y.; Upender, R.P. Sleep disturbance and metabolic dysfunction: The roles of adipokines. Int. J. Mol. Sci. 2022, 23, 1706. [Google Scholar] [CrossRef] [PubMed]
- Stich, F.M.; Huwiler, S.; D’Hulst, G.; Lustenberger, C. The potential role of sleep in promoting a healthy body composition: Underlying mechanisms determining muscle, fat, and bone mass and their association with sleep. Neuroendocrinology 2022, 112, 673–701. [Google Scholar] [CrossRef] [PubMed]
- Civelek, E.; Ozturk Civelek, D.; Akyel, Y.K.; Kaleli Durman, D.; Okyar, A. Circadian dysfunction in adipose tissue: Chronotherapy in metabolic diseases. Biology 2023, 12, 1077. [Google Scholar] [CrossRef] [PubMed]
- Kappes, C.; Stein, R.; Körner, A.; Merkenschlager, A.; Kiess, W. Stress, Stress Reduction and Obesity in Childhood and Adolescence. Horm. Res. Paediatr. 2023, 96, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Moreira, S.M.B.P.; Bachi, A.L.L.; Jirjos, E.I.; Malheiros, C.A.; Vencio, S.; Alves, V.L.S.; Sousa, A.R.T.; Felipe, L.A.; Perez, E.A.; Lino, M.E.M.; et al. Roux-en-Y Gastric Bypass Improves Adiponectin to Leptin Ratio and Inflammatory Profile in Severely Obese Women with and without Metabolic Syndrome: A Randomized Controlled Trial. Nutrients 2023, 15, 3312. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, R.A.; Maiya, G.A.; Hombali, A.; Umakanth, S.; Shivashankar, K.N. Effect of physical activity promotion on adiponectin, leptin and other inflammatory markers in prediabetes: A systematic review and meta-analysis of randomized controlled trials. Acta Diabetol. 2021, 58, 419–429. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Ramírez-Vélez, R.; Díez, J.; González, A.; Izquierdo, M. Exercise training-induced changes in exerkine concentrations may be relevant to the metabolic control of type 2 diabetes mellitus patients: A systematic review and meta-analysis of randomized controlled trials. J. Sport. Health Sci. 2023, 12, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Boutens, L.; Stienstra, R. Adipose tissue macrophages: Going off track during obesity. Diabetologia 2016, 59, 879–894. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.; Liang, Y.; Ma, Y.; Wu, J.; Luo, H.; Yi, B. The Variation and Correlation of Serum Adiponectin, Nesfatin-1, IL-6, and TNF-α Levels in Prediabetes. Front. Endocrinol. 2022, 13, 774272. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Li, H.; Xia, N. The Interplay Between Adipose Tissue and Vasculature: Role of Oxidative Stress in Obesity. Front. Cardiovasc. Med. 2021, 8, 650214. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Zhao, F.; Cheng, H.; Su, M.; Wang, Y. Macrophage polarization: An important role in inflammatory diseases. Front. Immunol. 2024, 15, 1352946. [Google Scholar] [CrossRef] [PubMed]
- Hou, L.; Wang, X.; Li, P.; Zhang, H.; Yao, Y.; Liu, Z.; Wang, J.; Liu, W. Adiposity modifies the association between heart failure risk and glucose metabolic disorder in older individuals: A community-based prospective cohort study. Cardiovasc. Diabetol. 2024, 23, 318. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Park, S.Y.; Choi, C.S. Insulin resistance: From mechanisms to therapeutic strategies. Diabetes Metab. J. 2021, 46, 15–37. [Google Scholar] [CrossRef] [PubMed]
- John, A.; Raza, H. Alterations in inflammatory cytokines and redox homeostasis in LPS-induced pancreatic beta-cell toxicity and mitochondrial stress: Protection by azadirachtin. Front. Cell Dev. Biol. 2022, 10, 867608. [Google Scholar] [CrossRef] [PubMed]
- Faro, D.C.; Di Pino, F.L.; Monte, I.P. Inflammation, oxidative stress, and endothelial dysfunction in the pathogenesis of vascular damage: Unraveling novel cardiovascular risk factors in Fabry disease. Int. J. Mol. Sci. 2024, 25, 8273. [Google Scholar] [CrossRef] [PubMed]
- Młynarska, E.; Czarnik, W.; Fularski, P.; Hajdys, J.; Majchrowicz, G.; Stabrawa, M.; Rysz, J.; Franczyk, B. From atherosclerotic plaque to myocardial infarction—The leading cause of coronary artery occlusion. Int. J. Mol. Sci. 2024, 25, 7295. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.; Farb, M.G.; Gokce, N. Cardiometabolic implications of adipose tissue aging. Obes. Rev. 2024, 25, e13806. [Google Scholar] [CrossRef] [PubMed]
- Khalid, M.; Alkaabi, J.; Khan, M.A.B.; Adem, A. Insulin Signal Transduction Perturbations in Insulin Resistance. Int. J. Mol. Sci. 2021, 22, 8590. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Chi, X.; Wang, Y.; Setrerrahmane, S.; Xie, W.; Xu, H. Trends in insulin resistance: Insights into mechanisms and therapeutic strategy. Signal Transduct. Target. Ther. 2022, 7, 216. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Yin, L.; Wang, X. Central and peripheral leptin resistance in obesity and improvements of exercise. Horm. Behav. 2021, 133, 105006. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Lai, F.; Hou, Y.; Zheng, R. Leptin signaling and leptin resistance. Med. Rev. 2022, 2, 363–384. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Liu, G.; Guo, J.; Su, Z. The PI3K/AKT pathway in obesity and type 2 diabetes. Int. J. Biol. Sci. 2018, 14, 1483–1496. [Google Scholar] [CrossRef] [PubMed]
- da Silva Rosa, S.C.; Liu, M.; Sweeney, G. Adiponectin Synthesis, Secretion and Extravasation from Circulation to Interstitial Space. Physiology 2021, 36, 134–149. [Google Scholar] [CrossRef] [PubMed]
- Munzberg, H.; Heymsfield, S.B.; Berthoud, H.R.; Morrison, C.D. History and future of leptin: Discovery, regulation and signaling. Metabolism 2024, 161, 156026. [Google Scholar] [CrossRef] [PubMed]
- Roy, P.K.; Islam, J.; Lalhlenmawia, H. Prospects of potential adipokines as therapeutic agents in obesity-linked atherogenic dyslipidemia and insulin resistance. Egypt. Heart J. 2023, 75, 24. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Li, N.; Xiong, W.; Li, G.; He, S.; Zhang, Z.; Zhu, Q.; Jiang, N.; Ikejiofor, C.; Zhu, Y.; et al. Leptin reduction as a required component for weight loss. Diabetes 2024, 73, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Wulff, B.S.; Kuhre, R.E.; Selvaraj, M.; Rehfeld, J.F.; Niss, K.; Fels, J.J.; Anna, S.; Raun, K.; Gerstenberg, M.K. Improved leptin sensitivity and increased soluble leptin receptor concentrations may underlie the additive effects of combining PYY [1–34] and exendin-4 on body weight lowering in diet-induced obese mice. Heliyon 2024, 10, e32009. [Google Scholar] [CrossRef] [PubMed]
- Erichsen, J.M.; Fadel, J.R.; Reagan, L.P. Peripheral versus central insulin and leptin resistance: Role in metabolic disorders, cognition, and neuropsychiatric diseases. Neuropharmacology 2022, 203, 108877. [Google Scholar] [CrossRef] [PubMed]
- Gunturiz Albarracín, M.L.; Forero Torres, A.Y. Adiponectin and Leptin Adipocytokines in Metabolic Syndrome: What Is Its Importance? Dubai Diabetes Endocrinol. J. 2020, 26, 93–102. [Google Scholar] [CrossRef]
- Li, S.; Han, X.; Song, J.; Dong, M.; Xie, T. Mechanism of Action and Risk Prediction of Adiponectin in Cardiovascular Diseases. Front. Biosci. -Landmark 2024, 29, 286. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Kusminski, C.M.; Scherer, P.E. Adiponectin, Leptin and Cardiovascular Disorders. Circ. Res. 2021, 128, 136–149. [Google Scholar] [CrossRef] [PubMed]
- Rausch, J.; Gillespie, S.; Orchard, T.; Tan, A.; McDaniel, J.C. Systematic review of marine-derived omega-3 fatty acid supplementation effects on leptin, adiponectin, and the leptin-to-adiponectin ratio. Nutr. Res. 2021, 85, 135–152. [Google Scholar] [CrossRef] [PubMed]
- Laurindo, L.F.; Rodrigues, V.D.; Catharin, V.M.C.S.; Simili, O.A.G.; Barboza, G.O.; Sloan, K.P.; Barbalho, S.M. Unraveling the rationale and conducting a comprehensive assessment of AdipoRon (adiponectin receptor agonist) as a candidate drug for diabetic nephropathy and cardiomyopathy prevention and intervention—A systematic review. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2025, 398, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, M.M.I. Therapeutic potential of adiponectin in prediabetes: Strategies, challenges, and future directions. Ther. Adv. Endocrinol. 2024, 15, 20420188231222371. [Google Scholar] [CrossRef] [PubMed]
- Liao, P.J.; Ting, M.K.; Wu, I.W.; Chen, S.W.; Yang, N.I.; Hsu, K.H. Higher Leptin-to-Adiponectin Ratio Strengthens the Association Between Body Measurements and Occurrence of Type 2 Diabetes Mellitus. Front. Public. Health 2021, 9, 678681. [Google Scholar] [CrossRef] [PubMed]
- Rammuana, H.L.; Hijam, D.; Ngangbam, N.; Devi, M.P.; Devi, M.J.; Ashem, F. Serum Leptin-adiponectin Ratio in Patients with and Without Metabolic Syndrome: A Cross-sectional Study. J. Clin. Diagn. Res. 2024, 18, 10. [Google Scholar] [CrossRef]
- Senkus, K.E.; Crowe-White, K.M.; Bolland, A.C.; Locher, J.L.; Ard, J.D. Changes in adiponectin:leptin ratio among older adults with obesity following a 12-month exercise and diet intervention. Nutr. Diabetes 2022, 12, 30. [Google Scholar] [CrossRef] [PubMed]


| Category | Factor | Relationship to T2DM | Connection to Adipose Tissue |
|---|---|---|---|
| Physiological | Insulin resistance [24] | Central mechanism to T2DM development | Increased visceral fat impairs insulin signaling |
| β-cell dysfunction [25] | Leads to reduced insulin secretion | Inflammation from adipose tissue can damage β-cells | |
| Hormonal | Leptin [26,27,28,29,30,31,32,33,34,35] | Often elevated in obesity but with resistance | Secreted by adipocytes; dysregulation linked to insulin resistance |
| Adiponectin [26,28,30,31,32,35] | Decreased levels associated with T2DM | Produced by adipose tissue; enhances insulin sensitivity | |
| Inflammatory | TNF-α, IL-6 [36] | Increased inflammation and insulin resistance | Secreted by adipose tissue macrophages during obesity |
| Morphological | Visceral adiposity [37,38,39,40,41] | Strong predictor of metabolic dysfunction | Excess intra-abdominal fat is metabolically active and pro-inflammatory |
| Adipocyte hypertrophy [42] | Enlarged fat cells impair glucose metabolism | Associated with increased inflammatory cytokine secretion | |
| Ectopic fat deposition [43,44,45] | Fat in liver, muscle, or pancreas impairs function | Occurs when adipose tissue is unable to store excess energy | |
| Lifestyle and Environmental | High-calorie diet [46] | Promotes weight gain and insulin resistance | Increases adipose tissue mass and dysregulation |
| Physical inactivity [46] | Reduces glucose uptake and promotes insulin resistance | Limits adipose tissue lipolysis and increases fat storage | |
| Genetic | Family history of T2DM [47] | Increases individual risk | Some gene variants affect adipose tissue development and function |
| Sex/BMI | Leptin (ng/mL) | Adiponectin (mcg/mL) |
|---|---|---|
| =22 | 0.5–12.5 | |
| <25 | 5–37 | |
| 25–30 | 5–28 | |
| >30 | 2–20 | |
| =22 | 0.5–15.2 | |
| <25 | 5–37 | |
| 25–30 | 4–20 | |
| >30 | 4–22 |
| Aspect | Leptin [26,27,28,30,31,32,33,34,35] | Adiponectin [26,28,30,31,32,35] | LAR [94,119,120,121,124,125,126] |
|---|---|---|---|
| Source | Primarily adipose tissue | Primarily adipose tissue | Derived ratio (leptin/adiponectin) |
| Normal Role | Regulates appetite and energy expenditure, and enhances insulin sensitivity | Enhances insulin sensitivity, is anti-inflammatory, and promotes lipid oxidation | Reflects balance between pro- and anti-diabetic/inflammatory adipokines |
| Levels in T2DM | Increased—due to adiposity and leptin resistance | Decreased—due to increased adiposity | Increased |
| Effect on Insulin | Decreases—when resistance develops | Increases | High LAR correlates with greater insulin resistance |
| Inflammatory Role | Pro-inflammatory | Anti-inflammatory | High LAR = Pro-inflammatory state |
| Clinical Relevance | Marker of adiposity, leptin resistance, and inflammation | Marker of insulin sensitivity, metabolic health, and inflammation | Better predictor of T2DM risk than either alone |
| Therapeutic Targeting | Indirect: weight loss, others possible but not currently clear | Targeted by changes to diet, exercise, and pharmacological interventions | Lowered through lifestyle changes, insulin-sensitizing therapy, and modifications of leptin and/or adiponectin |
| Predictive Value | Moderate alone | Moderate alone | High predictive value for T2DM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rausch, J.; Horne, K.E.; Marquez, L. The Effects of Adipose Tissue Dysregulation on Type 2 Diabetes Mellitus. Biomedicines 2025, 13, 1770. https://doi.org/10.3390/biomedicines13071770
Rausch J, Horne KE, Marquez L. The Effects of Adipose Tissue Dysregulation on Type 2 Diabetes Mellitus. Biomedicines. 2025; 13(7):1770. https://doi.org/10.3390/biomedicines13071770
Chicago/Turabian StyleRausch, Jamie, Kaitlyn E. Horne, and Luis Marquez. 2025. "The Effects of Adipose Tissue Dysregulation on Type 2 Diabetes Mellitus" Biomedicines 13, no. 7: 1770. https://doi.org/10.3390/biomedicines13071770
APA StyleRausch, J., Horne, K. E., & Marquez, L. (2025). The Effects of Adipose Tissue Dysregulation on Type 2 Diabetes Mellitus. Biomedicines, 13(7), 1770. https://doi.org/10.3390/biomedicines13071770







