In Vitro Investigation of Statin Effects on Genes Associated with Severe COVID-19 in Cancerous and Non-Cancerous Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Whole-Transcriptome Analyses
2.2. Quantitative Real-Time PCR
2.3. Network Analysis
3. Results
3.1. Statins and Apolipoprotein E
3.2. Statins and Angiotensin-Converting Enzyme 2
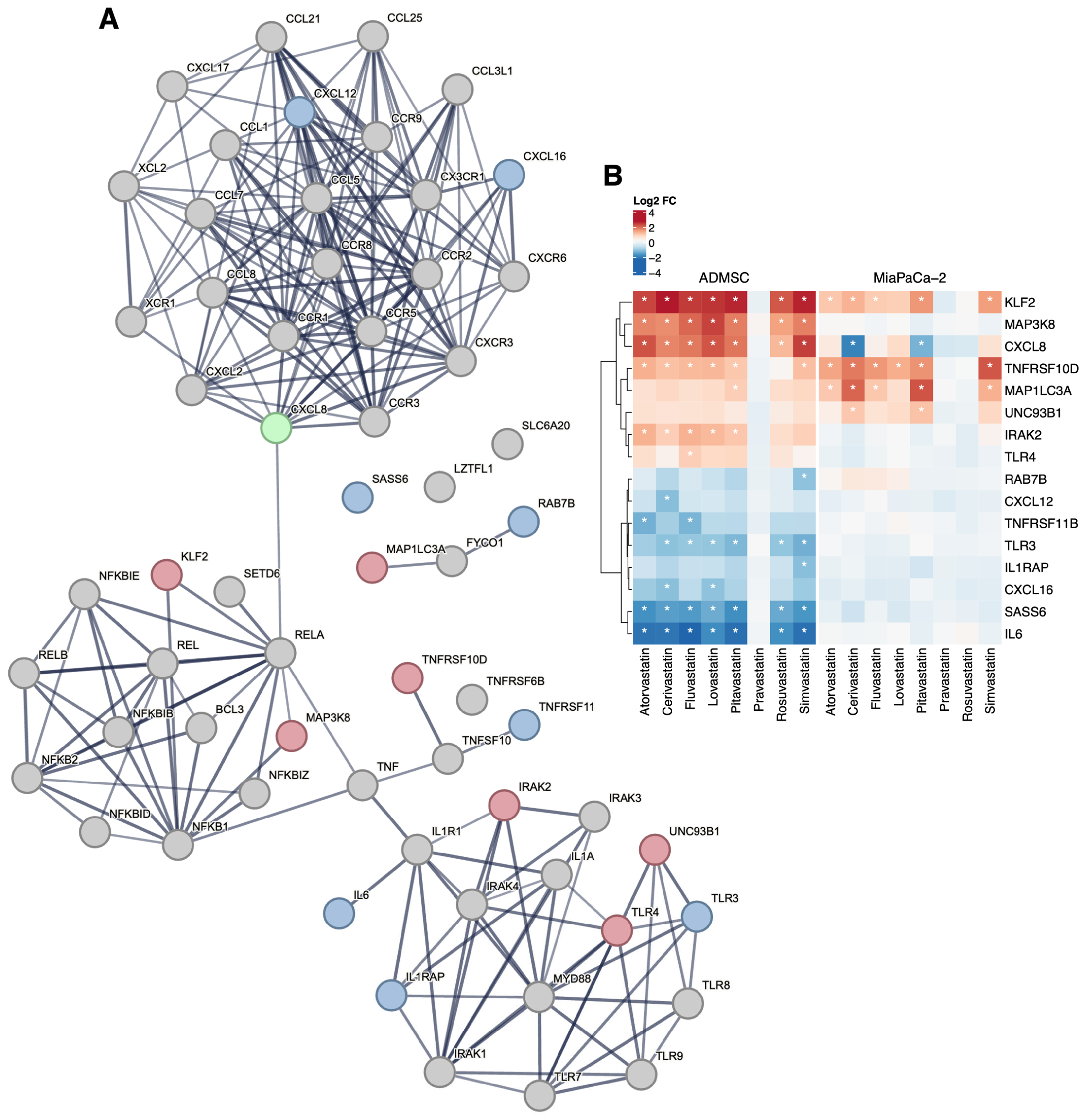
3.3. Statins and Immune System Genes
3.4. Statins and Respiratory Failure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACE2 | Angiotensin-converting enzyme 2 |
| AD-MSC | Adipose tissue-derived human mesenchymal stem cells |
| APOE | Apolipoprotein E |
| ARDS | Acute respiratory distress syndrome |
| CCR9 | C-C chemokine receptor type 9 |
| COVID-19 | Coronavirus disease 2019 |
| CXCR6 | C-X-C motif chemokine receptor 6 |
| CXCL12 | Chemokine (C-X-C motif) ligand 12 |
| CXCL16 | Chemokine (C-X-C motif) ligand 16 |
| ERK | Extracellular signal-regulated kinases |
| FC | Fold change |
| FYCO1 | FYVE and coiled-coil domain-containing protein 1 |
| GO | Gene ontology |
| GSEA | Gene set enrichment analysis |
| HDL | High-density lipoprotein |
| HMG-CoA reductase | 3-hydroxy-3-methylglutaryl-coenzyme A reductase |
| IL | Interleukin |
| IRAK2 | Interleukin-1 receptor-associated kinase-like 2 |
| KEGG | Kyoto encyclopedia of genes and genomes |
| LDL | Low-density lipoprotein |
| LDL-R | Low-density lipoprotein receptor |
| LZTFL1 | Leucine zipper transcription factor-like protein 1 |
| MAP1LC3A | Microtubule-associated protein 1 light chain 3α |
| MAP3K8 | Mitogen-activated protein kinase kinase kinase 8 |
| MIAME | Minimum information about a microarray experiment |
| MiaPaCa-2 | Human cells from pancreatic carcinoma |
| MME | Membrane metalloendopeptidase |
| NF-κB | Nuclear factor kappa-light-chain-enhancer of activated B cells |
| RAB7B | Ras-related protein Rab-7b |
| RIN | RNA integrity number |
| SASS6 | Spindle assembly 6 homolog (C. elegans) |
| SLC6A20 | Sodium-dependent imino acid transporter 1 |
| TLR | Toll-like receptors |
| TNF | Tumor necrosis factor |
| TNFRSF10D | Tumor necrosis factor receptor superfamily member 10D |
| TNFRSF11B | Tumor necrosis factor receptor superfamily member 11B |
| UNC93B1 | Unc93 (C. elegans) homolog B1 |
| VLDL | Very low-density lipoprotein |
| XCR1 | Chemokine XC receptor 1 |
References
- Severe COVID-19 GWAS Group; Ellinghaus, D. Genomewide Association Study of Severe Covid-19 with Respiratory Failure. N. Engl. J. Med. 2020, 383, 1522–1534. [Google Scholar] [CrossRef]
- Noureddine, F.Y.; Chakkour, M. The Emergence of SARS-CoV-2 Variant(s) and Its Impact on the Prevalence of COVID-19 Cases in the Nabatieh Region, Lebanon. Med. Sci. 2021, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Šúri, T.; Pfeiferová, L. Developing molecular surveillance of SARS-CoV-2 in the Czech Republic (2021–2022). Sci. Rep. 2025, 15, 19690. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19). 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19 (accessed on 12 November 2020).
- Toth, P.P.; Banach, M. Statins: Then and now. Methodist DeBakey Cardiovasc. J. 2019, 15, 23–31. [Google Scholar] [CrossRef]
- De Spiegeleer, A.; Bronselaer, A. The effects of ARBs, ACEis, and statins on clinical outcomes of COVID-19 infection among nursing home residents. J. Am. Med. Dir. Assoc. 2020, 21, 909–914. [Google Scholar] [CrossRef] [PubMed]
- Daniels, L.B.; Sitapati, A.M. Relation of statin use prior to admission to severity and recovery among COVID-19 inpatients. Am. J. Cardiol. 2020, 136, 149–155. [Google Scholar] [CrossRef]
- Zhang, X.J.; Qin, J.J. In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metab. 2020, 32, 176–187. [Google Scholar] [CrossRef]
- Kow, C.S.; Hasan, S.S. Meta-analysis of effect of statins in patients with COVID-19. Am. J. Cardiol. 2020, 134, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Arocutipa, C.; Melgar-Talavera, B. Statins reduce mortality in patients with COVID-19: An updated meta-analysis of 147,824 patients. Int. J. Infect. Dis. 2021, 110, 374–381. [Google Scholar] [CrossRef]
- Kow, C.S.; Hasan, S.S. The association between the use of statins and clinical outcomes in patients with COVID-19: A systematic review and meta-analysis. Am. J. Cardiovasc. Drugs. 2022, 22, 295–304. [Google Scholar] [CrossRef]
- Florêncio de Mesquita, C.; Rivera, A. Adjunctive Statin Therapy in Patients with Covid-19: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Med. 2024, 137, 697–705. [Google Scholar] [CrossRef]
- Ayeh, S.K.; Abbey, E.J. Statins use and COVID-19 outcomes in hospitalized patients. PLoS ONE 2021, 16, e0256899. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S. Statin drug therapy may increase COVID-19 infection. NMJ 2020, 3, 326–327. [Google Scholar] [CrossRef][Green Version]
- Peymani, P.; Dehesh, T. Statins in patients with COVID-19: A retrospective cohort study in Iranian COVID-19 patients. Transl. Med. Commun. 2021, 6, 3. [Google Scholar] [CrossRef]
- Focosi, D.; Franchini, M. COVID-19 therapeutics. Clin. Microbiol. Rev. 2024, 37, e0011923. [Google Scholar] [CrossRef] [PubMed]
- Dashti-Khavidaki, S.; Khalili, H. Considerations for statin therapy in patients with COVID-19. Pharmacotherapy 2020, 40, 484–486. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Conti, P.; Ronconi, G. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVID-19 or SARS-CoV-2): Anti-inflammatory strategies. J. Biol. Regul. Homeost. Agents 2020, 34, 327–331. [Google Scholar]
- Gorabi, A.M.; Kiaie, N. Antiviral effects of statins. Pharmacol. Res. 2020. [CrossRef]
- Superti, F.; Seganti, L. SA-11 rotavirus binding to human serum lipoproteins. Med. Microbiol. Immunol. 1992, 181, 77–86. [Google Scholar] [CrossRef]
- Wang, H.; Yang, P. SARS coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway. Cell Res. 2008, 18, 290–301. [Google Scholar] [CrossRef]
- Moeller, R.; Zapatero-Belinchón, F. Effect of statins on SARS-CoV-2 infection. J. medRxiv 2020, 13, 20152272. [Google Scholar] [CrossRef]
- Shang, J.; Wan, Y. Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA 2020, 117, 11727–11734. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.B.; Farzan, M.; Chen, B.; Choe, H. Mechanisms of SARS-CoV-2 entry into cells. Nat. Rev. Mol. Cell Biol. 2022, 23, 3–20. [Google Scholar] [CrossRef] [PubMed]
- DeDiego, M.L.; Nieto-Torres, J.L. Inhibition of NF-κB-mediated inflammation in severe acute respiratory syndrome coronavirus-infected mice increases survival. J. Virol. 2014, 88, 913–924. [Google Scholar] [CrossRef]
- Totura, A.L.; Whitmore, A. Toll-like receptor 3 signaling via TRIF contributes to a protective innate immune response to severe acute respiratory syndrome coronavirus infection. Mbio 2015, 6, 10–1128. [Google Scholar] [CrossRef]
- Totura, A.L.; Baric, R.S. Reply to “Statins may decrease the fatality rate of MERS infection”. Mbio 2015, 6, 10–1128. [Google Scholar] [CrossRef]
- Tudorache, I.F.; Trusca, V.G. Apolipoprotein E–A multifunctional protein with implications in various pathologies as a result of its structural features. Comput. Struct. Biotechnol. J. 2017, 15, 359–365. [Google Scholar] [CrossRef]
- Kuo, C.L.; Pilling, L.C. APOE e4 genotype predicts severe COVID-19 in the UK Biobank community cohort. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 2231–2232. [Google Scholar] [CrossRef]
- Gbelcová, H.; Rimpelová, S. Variability in statin-induced changes in gene expression profiles of pancreatic cancer. Sci. Rep. 2017, 7, 44219. [Google Scholar] [CrossRef]
- Gbelcová, H.; Rimpelová, S. Highly variable biological effects of statins on cancer, non-cancer, and stem cells in vitro. Sci. Rep. 2024, 14, 11830. [Google Scholar] [CrossRef] [PubMed]
- Brábek, J.; Jakubek, M. Interleukin-6: Molecule in the intersection of cancer, ageing and COVID-19. Int. J. Mol. Sci. 2020, 21, 7937. [Google Scholar] [CrossRef] [PubMed]
- Katopodis, P.; Anikin, V. Pan-cancer analysis of transmembrane protease serine 2 and cathepsin L that mediate cellular SARS CoV 2 infection leading to COVID-19. Int. J. Oncol. 2020, 57, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, L. The SARS-CoV-2 host cell receptor ACE2 correlates positively with immunotherapy response and is a potential protective factor for cancer progression. Comput. Struct. Biotechnol. J. 2020, 18, 2438–2444. [Google Scholar] [CrossRef]
- Sánchez-Guijo, F.; García-Arranz, M. Adipose-derived mesenchymal stromal cells for the treatment of patients with severe SARS-CoV-2 pneumonia requiring mechanical ventilation: A proof of concept study. eClinicalMedicine 2020, 25, 100454. [Google Scholar] [CrossRef]
- Gbelcová, H.; Lenícek, M. Differences in antitumor effects of various statins on human pancreatic cancer. Int. J. Cancer. 2008, 122, 1214–1221. [Google Scholar] [CrossRef]
- Durinck, S.; Moreau, Y. BioMart and Bioconductor: A powerful link between biological databases and microarray data analysis. Bioinformatics 2005, 21, 3439–3440. [Google Scholar] [CrossRef]
- Hubbard, T.J.; Aken, B.L. Ensembl 2007. Nucleic Acids Res. 2007, 35, D610–D617. [Google Scholar] [CrossRef]
- Carvalho, B.S.; Irizarry, R.A. A framework for oligonucleotide microarray preprocessing. Bioinformatics 2010, 26, 2363–2367. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing. 2021. Available online: https://www.R-project.org/ (accessed on 20 February 2021).
- Ritchie, M.E.; Phipson, B. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015, 43, e47. [Google Scholar] [CrossRef]
- Storey, J.D.; Tibshirani, R. Statistical significance for genomewide studies. Proc. Natl. Acad. Sci. USA. 2003, 100, 9440–9445. [Google Scholar] [CrossRef]
- Bustin, S.A.; Benes, V.; Garson, J.A.; Hellemans, J.; Huggett, J.; Kubista, M.; Mueller, R.; Nolan, T.; Pfaffl, M.W.; Shipley, G.L.; et al. The MIQE Guidelines: M inimum I nformation for Publication of Q uantitative Real-Time PCR E xperiments. Clin. Chem. 2009, 55, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Jensen, L.J.; Kuhn, M. STRING 8–a global view on proteins and their functional interactions in 630 organisms. Nucleic Acids Res. 2009, 37, D412–D416. [Google Scholar] [CrossRef]
- Rice, G.I.; Thomas, D.A. Evaluation of angiotensin-converting enzyme (ACE), its homologue ACE2, and neprilysin in angiotensin peptide metabolism. Biochem. J. 2004, 383, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Velazquez-Salinas, L.; Verdugo-Rodriguez, A. The role of interleukin 6 during viral infections. Front. Microbiol. 2019, 10, 1057. [Google Scholar] [CrossRef]
- Lee, J.H.; Sergi, C.; Kast, R.E. Basic implications on three pathways associated with SARS-CoV-2. Biomed. J. 2024, 47, 100766. [Google Scholar] [CrossRef]
- Zou, M.; Su, X. The molecular mechanism of multiple organ dysfunction and targeted intervention of COVID-19 based on time-order transcriptomic analysis. Front. Immunol. 2021, 12, 729776. [Google Scholar] [CrossRef] [PubMed]
- Rimpelová, S.; Kolář, M. Comparison of transcriptomic profiles of MiaPaCa-2 pancreatic cancer cells treated with different statins. Molecules 2021, 26, 3528. [Google Scholar] [CrossRef]
- Nguyen, T.B.; Sakata-Yanagimoto, M. Dasatinib is an effective treatment for angioimmunoblastic T-cell lymphoma. Cancer Res. 2020, 80, 1875–1884. [Google Scholar] [CrossRef]
- Tanaka, K.; Matsumoto, Y. Impact of RhoA overexpression on clinical outcomes in cervical squamous cell carcinoma treated with concurrent chemoradiotherapy. J. Radiat. Res. 2020, 61, 221–230. [Google Scholar] [CrossRef]
- Bros, M.; Haas, K. RhoA as a key regulator of innate and adaptive immunity. Cells 2019, 8, 733. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Mei, X. RhoA inhibits apoptosis and increases proliferation of cultured SPCA1 lung cancer cells. J. Mol. Med. 2017, 15, 3963–3968. [Google Scholar] [CrossRef]
- Ozkan, S.; Cakmak, F. Efficacy of serum angiotensin II levels in prognosis of patients with coronavirus disease 2019. Crit. Care Med. 2021, 49, e613–e623. [Google Scholar] [CrossRef]
- Eleuteri, D.; Montini, L. Renin-angiotensin system dysregulation in critically ill patients with acute respiratory distress syndrome due to COVID-19: A preliminary report. Crit. Care 2021, 25, 91. [Google Scholar] [CrossRef] [PubMed]
- Miesbach, W. Pathological Role of Angiotensin II in Severe COVID-19. TH Open 2020, 4, e138–e144. [Google Scholar] [CrossRef]
- Zoufaly, A.; Poglitsch, M. Human recombinant soluble ACE2 in severe COVID-19. Lancet Respir. Med. 2020, 8, 1154–1158. [Google Scholar] [CrossRef]
- Abd El-Aziz, T.M.; Al-Sabi, A. Human recombinant soluble ACE2 (hrsACE2) shows promise for treating severe COVID-19. Signal Transduct. Target. Ther. 2020, 5, 258. [Google Scholar] [CrossRef]
- Li, Y.H.; Wang, Q.X. Effects of rosuvastatin on expression of angiotensin-converting enzyme 2 after vascular balloon injury in rats. J. Geriatr. Cardiol. 2013, 10, 151–158. [Google Scholar] [PubMed]
- Minz, M.; Bansal, M. Statins and SARS-CoV-2 disease: Current concepts and possible benefits. Diabetes Metab. Syndr. 2020, 14, 2063–2067. [Google Scholar] [CrossRef]
- Wang, H.; Yuan, Z. Cholesterol and COVID-19 lethality in elderly. bioRxiv 2020. [Google Scholar] [CrossRef]
- Fuior, E.V.; Gafencu, A.V. Apolipoprotein C1: Its pleiotropic effects in lipid metabolism and beyond. Int. J. Mol. Sci. 2019, 20, 5939. [Google Scholar] [CrossRef] [PubMed]
- Subir, R.; Jagat, J.M. Pros and cons for use of statins in people with coronavirus disease-19 (COVID-19). Diabetes Metab. Syndr. 2020, 14, 1225–1229. [Google Scholar] [CrossRef]
- Rodrigues-Diez, R.R.; Tejera-Muñoz, A. Statins: Could an old friend help in the fight against COVID-19? Br. J. Pharmacol. 2020, 177, 4873–4886. [Google Scholar] [CrossRef] [PubMed]
- Chansrichavala, P.; Chantharaksri, U. Atorvastatin attenuates TLR4-mediated NF-κB activation in a MyD88-dependent pathway. Asian Pac. J. Allergy Immunol. 2009, 27, 49–57. [Google Scholar]
- Gubernatorova, E.; Gorshkova, E. IL-6: Relevance for immunopathology of SARS-CoV-2. Cytokine Growth Factor. Rev. 2020, 53, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Coomes, E.A.; Haghbayan, H. Interleukin-6 in COVID-19: A systematic review and meta-analysis. Rev. Med. Virol. 2020, 30, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Toniati, P.; Piva, S. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single-center study of 100 patients in Brescia, Italy. Autoimmun. Rev. 2020, 19, 102568. [Google Scholar] [CrossRef]
- Salvarani, C.; Dolci, G. Effect of Tocilizumab vs Standard Care on Clinical Worsening in Patients Hospitalized With COVID-19 Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021, 181, 24–31. [Google Scholar] [CrossRef]
- Veiga, V.C.; Prats, J.A.G.G. Effect of tocilizumab on clinical outcomes at 15 days in patients with severe or critical coronavirus disease 2019: Randomised controlled trial. BMJ 2021, 372, n84. [Google Scholar] [CrossRef]
- Hermine, O.; Mariette, X. Effect of Tocilizumab vs Usual Care in Adults Hospitalized With COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021, 181, 32–40. [Google Scholar] [CrossRef]
- Stone, J.H.; Frigault, M.J. Efficacy of Tocilizumab in Patients Hospitalized with Covid-19. N. Engl. J. Med. 2020, 383, 2333–2344. [Google Scholar] [CrossRef] [PubMed]
- Campbell, G.R.; To, R.K. SARS-CoV-2, SARS-CoV-1, and HIV-1 derived ssRNA sequences activate the NLRP3 inflammasome in human macrophages through a non-classical pathway. iScience 2021, 24, 102295. [Google Scholar] [CrossRef] [PubMed]
- Onodi, F.; Bonnet-Madin, L. SARS-CoV-2 induces human plasmacytoid predendritic cell diversification via UNC93B and IRAK4. J. Exp. Med. 2021, 218, e20201387. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kapustová, A.; Macášek, P.; Baďurová, B.; Melegová, J.; Rimpelová, S.; Kubovčiak, J.; Šáchová, J.; Hradilová, M.; Kolář, M.; Vítek, L.; et al. In Vitro Investigation of Statin Effects on Genes Associated with Severe COVID-19 in Cancerous and Non-Cancerous Cells. Biomedicines 2025, 13, 1714. https://doi.org/10.3390/biomedicines13071714
Kapustová A, Macášek P, Baďurová B, Melegová J, Rimpelová S, Kubovčiak J, Šáchová J, Hradilová M, Kolář M, Vítek L, et al. In Vitro Investigation of Statin Effects on Genes Associated with Severe COVID-19 in Cancerous and Non-Cancerous Cells. Biomedicines. 2025; 13(7):1714. https://doi.org/10.3390/biomedicines13071714
Chicago/Turabian StyleKapustová, Adriana, Patrik Macášek, Bibiána Baďurová, Jana Melegová, Silvie Rimpelová, Jan Kubovčiak, Jana Šáchová, Miluše Hradilová, Michal Kolář, Libor Vítek, and et al. 2025. "In Vitro Investigation of Statin Effects on Genes Associated with Severe COVID-19 in Cancerous and Non-Cancerous Cells" Biomedicines 13, no. 7: 1714. https://doi.org/10.3390/biomedicines13071714
APA StyleKapustová, A., Macášek, P., Baďurová, B., Melegová, J., Rimpelová, S., Kubovčiak, J., Šáchová, J., Hradilová, M., Kolář, M., Vítek, L., Ruml, T., & Gbelcová, H. (2025). In Vitro Investigation of Statin Effects on Genes Associated with Severe COVID-19 in Cancerous and Non-Cancerous Cells. Biomedicines, 13(7), 1714. https://doi.org/10.3390/biomedicines13071714










