Sialic Acid and Colchicine Functionalized Silica Nanoparticles: A Novel Approach to Leishmanicidal Selective Treatments
Abstract
1. Introduction
2. Materials and Methods
2.1. Synthesis and Characterization of Functionalized Silica Nanoparticles
2.1.1. TEM
2.1.2. BET
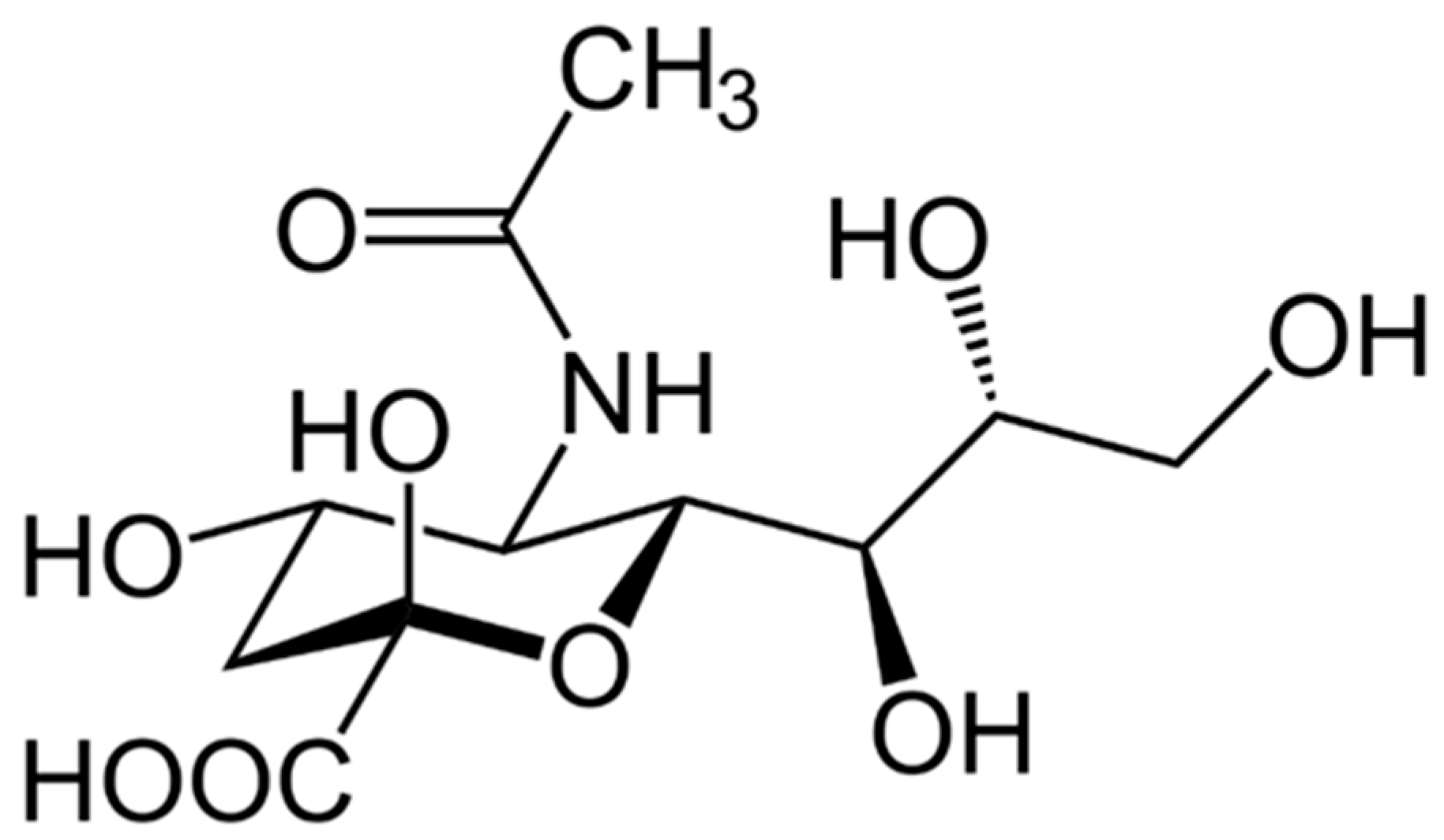
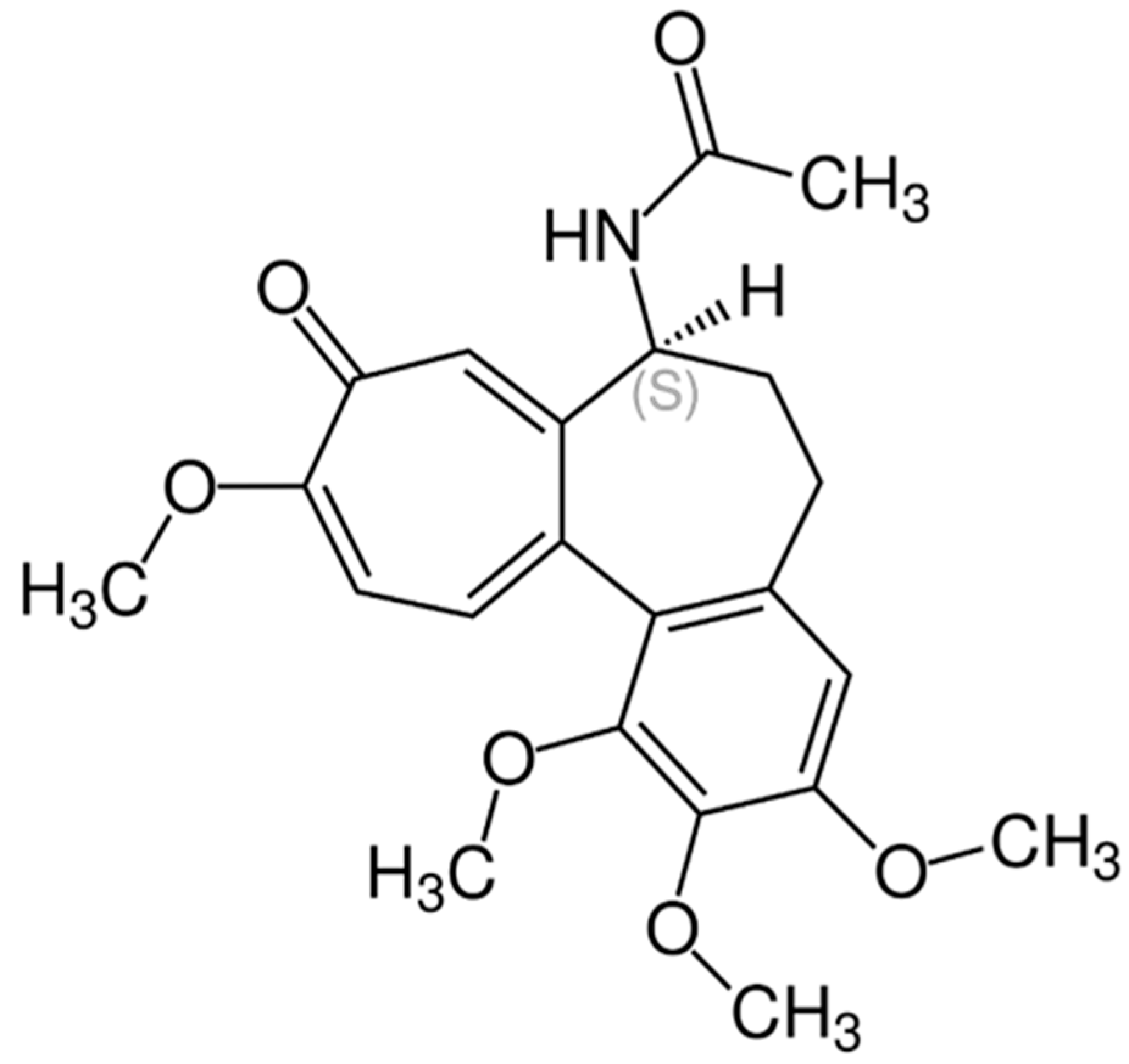
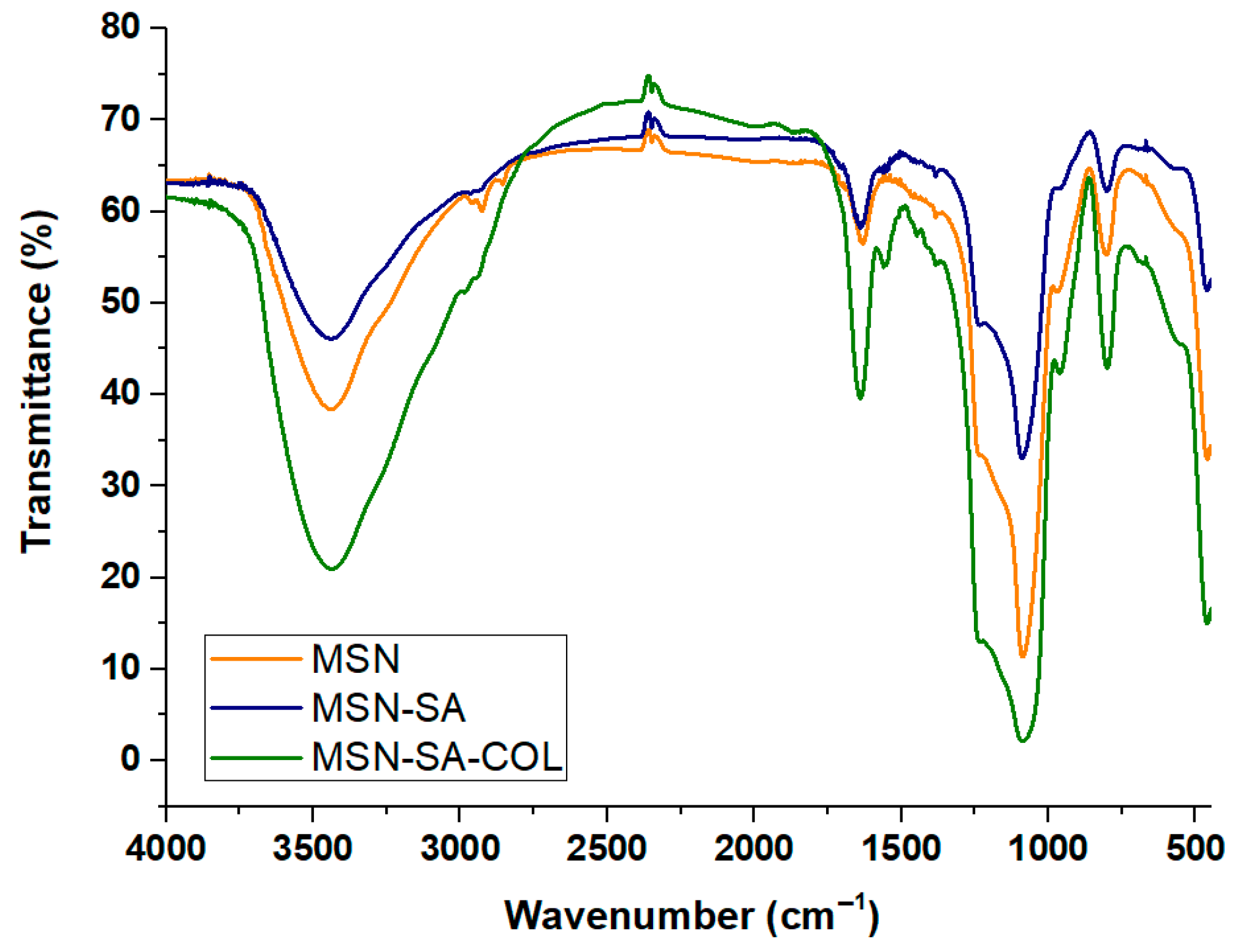
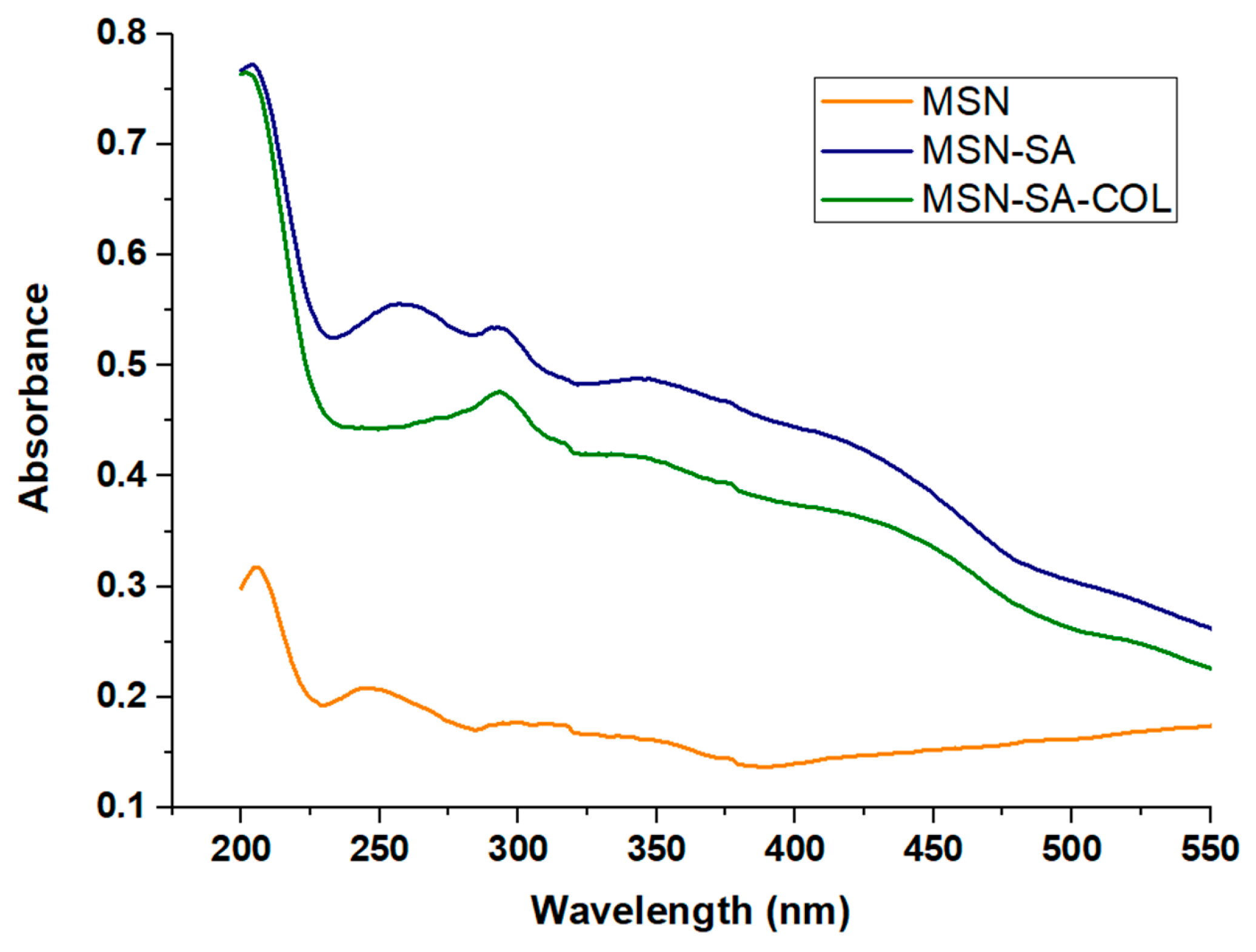
2.1.3. Spectroscopic Properties
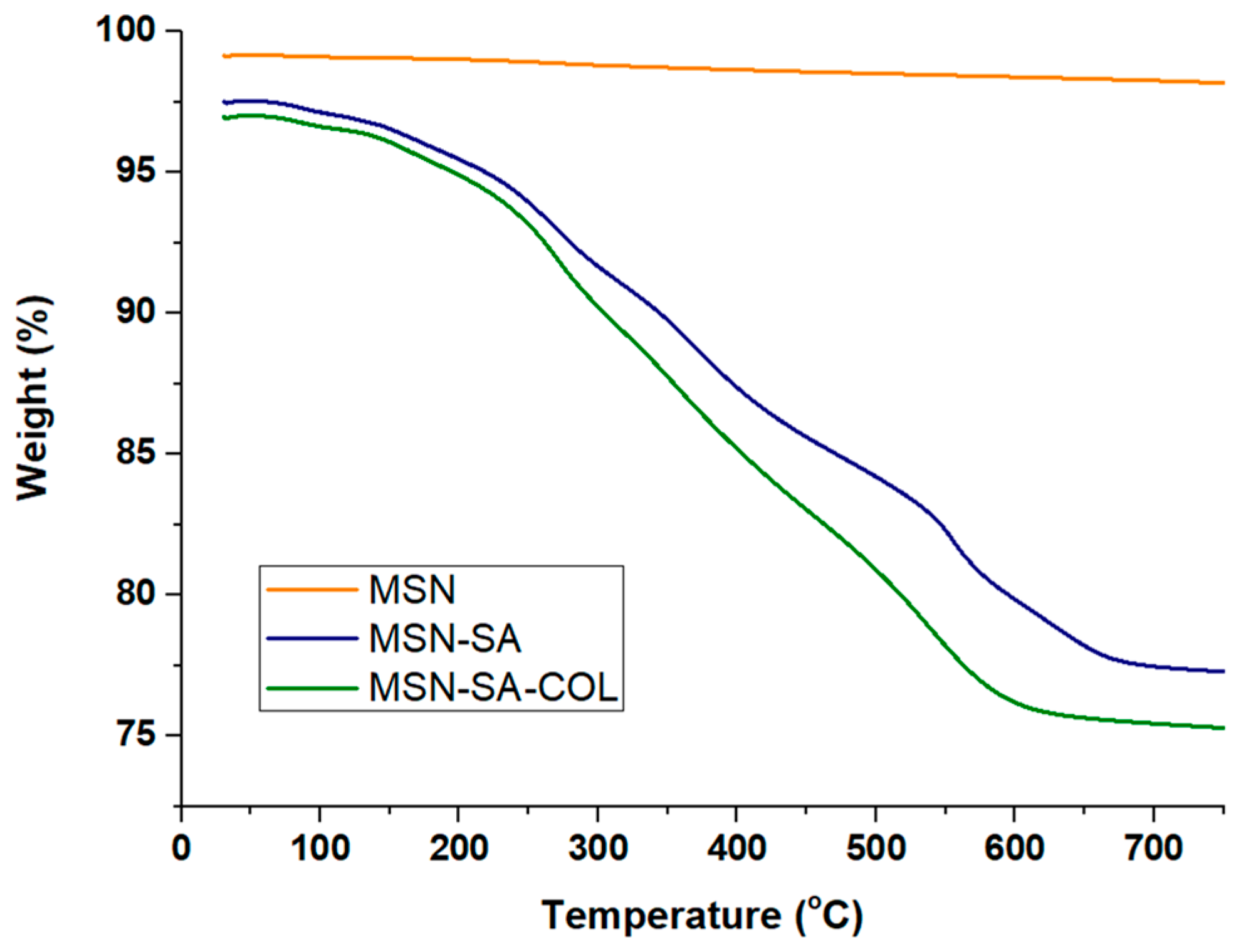
2.1.4. Thermogravimetry
2.2. Biological Assays
3. Results
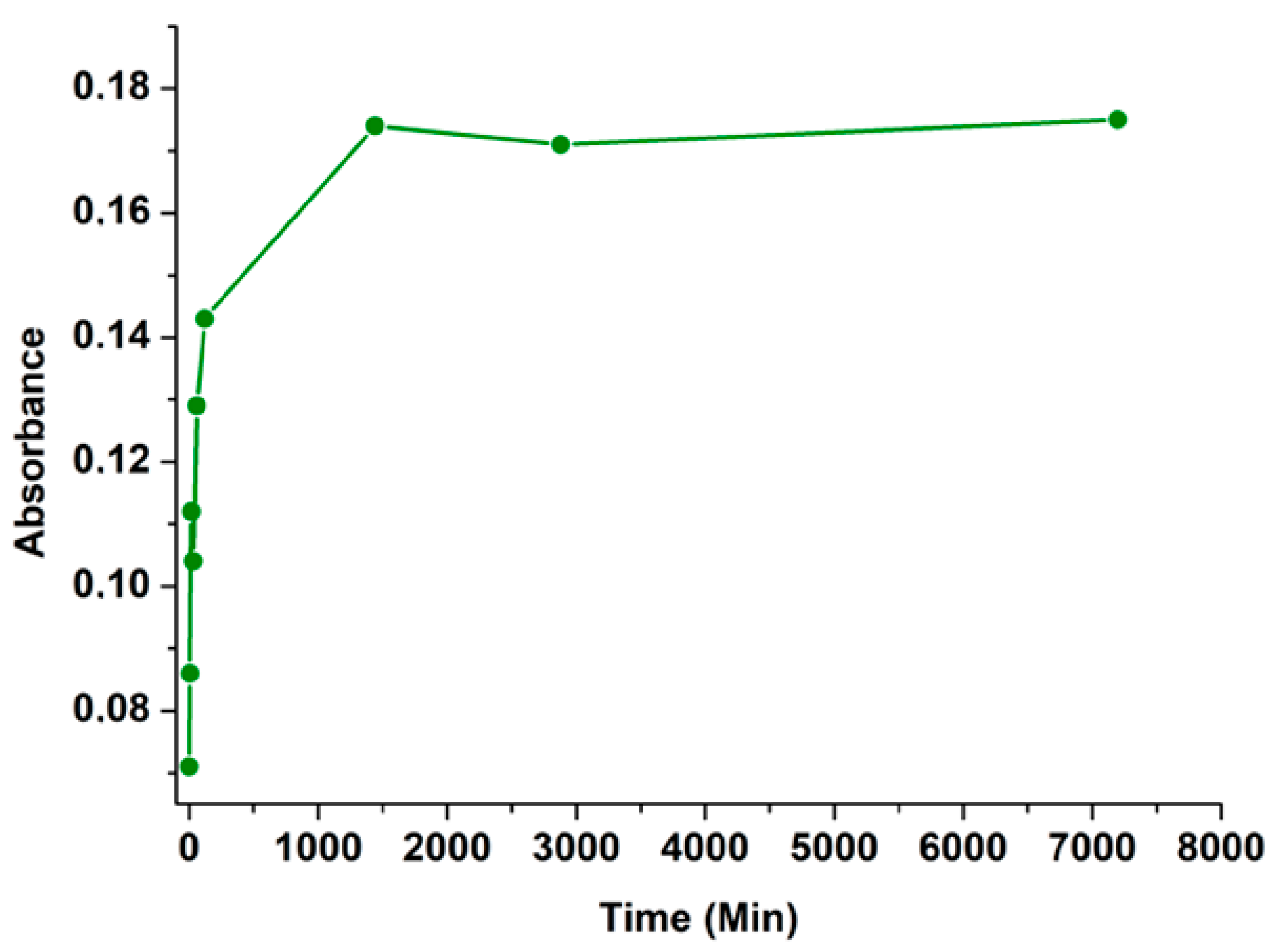
3.1. Release Studies
3.2. In Vitro Antiparasitic Activity and Toxicity
4. Discussion
5. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oryan, A. Plant-Derived Compounds in Treatment of Leishmaniasis. Iran. J. Vet. Res. 2015, 16, 1–19. [Google Scholar] [CrossRef]
- Steverding, D. The History of Leishmaniasis. Parasites Vectors 2017, 10, 82. [Google Scholar] [CrossRef]
- Croft, S.L.; Coombs, G.H. Leishmaniasis—Current Chemotherapy and Recent Advances in the Search for Novel Drugs. Trends Parasitol. 2003, 19, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Uliana, S.R.B.; Trinconi, C.T.; Coelho, A.C. Chemotherapy of Leishmaniasis: Present Challenges. Parasitology 2018, 145, 464–480. [Google Scholar] [CrossRef] [PubMed]
- Alpizar-Sosa, E.A.; Ithnin, N.R.B.; Wei, W.; Pountain, A.W.; Weidt, S.K.; Donachie, A.M.; Ritchie, R.; Dickie, E.A.; Burchmore, R.J.S.; Denny, P.W.; et al. Amphotericin B Resistance in Leishmania mexicana: Alterations to Sterol Metabolism and Oxidative Stress Response. PLoS Negl. Trop. Dis. 2022, 16, e0010779. [Google Scholar] [CrossRef]
- Pradhan, S.; Schwartz, R.A.; Patil, A.; Grabbe, S.; Goldust, M. Treatment Options for Leishmaniasis. Clin. Exp. Dermatol. 2022, 47, 516–521. [Google Scholar] [CrossRef]
- Zhang, H.; Yan, R.; Liu, Y.; Yu, M.; He, Z.; Xiao, J.; Li, K.; Liu, G.; Ning, Q.; Li, Y. Progress in Antileishmanial Drugs: Mechanisms, Challenges, and Prospects. PLoS Negl. Trop. Dis. 2025, 19, e0012735. [Google Scholar] [CrossRef] [PubMed]
- Mohammadzadeh, M.; Behnaz, F.; Golshan, Z. Efficacy of Glucantime for Treatment of Cutaneous Leishmaniasis in Central Iran. J. Infect. Public Health 2013, 6, 120–124. [Google Scholar] [CrossRef]
- Alborzi, A.; Pouladfar, G.; Attar, A.; Falahi, F.; Jafarpour, Z.; Karimi, A.; Kadivar, M.R. Effectiveness of Short-Course Meglumine Antimoniate (Glucantime®) for Treatment of Visceral Leishmaniasis: A 13-Year, Multistage, Non-Inferiority Study in Iran. Am. J. Trop. Med. Hyg. 2017, 96, 182–189. [Google Scholar] [CrossRef][Green Version]
- Frézard, F.; Demicheli, C.; Ribeiro, R.R. Pentavalent Antimonials: New Perspectives for Old Drugs. Molecules 2009, 14, 2317–2336. [Google Scholar] [CrossRef]
- Marques, S.A.; Merlotto, M.R.; Ramos, P.M.; Marques, M.E.A. American Tegumentary Leishmaniasis: Severe Side Effects of Pentavalent Antimonial in a Patient with Chronic Renal Failure. Bras. Dermatol. 2019, 94, 355–357. [Google Scholar] [CrossRef]
- An, I.; Harman, M.; Esen, M.; Çelik, H. The Effect of Pentavalent Antimonial Compounds Used in the Treatment of Cutaneous Leishmaniasis on Hemogram and Biochemical Parameters. Cutan. Ocul. Toxicol. 2019, 38, 294–297. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, E. Current Treatment for Cutaneous Leishmaniasis: A Review. Am. J. Ther. 2009, 16, 178. [Google Scholar] [CrossRef] [PubMed]
- Natera, S.; Machuca, C.; Padrón-Nieves, M.; Romero, A.; Díaz, E.; Ponte-Sucre, A. Leishmania spp.: Proficiency of Drug-Resistant Parasites. Int. J. Antimicrob. Agents 2007, 29, 637–642. [Google Scholar] [CrossRef] [PubMed]
- Wijnant, G.-J.; Dumetz, F.; Dirkx, L.; Bulté, D.; Cuypers, B.; Van Bocxlaer, K.; Hendrickx, S. Tackling Drug Resistance and Other Causes of Treatment Failure in Leishmaniasis. Front. Trop. Dis. 2022, 3, 837460. [Google Scholar] [CrossRef]
- Mollo, M.C.; Cambiaso, M.L.; Ferreira, L.L.G.; Kilimciler, N.B.; Bisceglia, J.A.; Andricopulo, A.D.; Orelli, L.R. Synthesis and in Vitro Leishmanicidal Activity of Novel N-Arylspermidine Derivatives. Bioorganic Chem. 2025, 154, 108083. [Google Scholar] [CrossRef]
- Jomori, T.; Higa, N.; Hokama, S.; Tyas, T.A.; Matsuura, N.; Ueda, Y.; Kimura, R.; Arizono, S.; de Voogd, N.J.; Hayashi, Y.; et al. A Novel Sesterterpenoid, Petrosaspongin and γ-Lactone Sesterterpenoids with Leishmanicidal Activity from Okinawan Marine Invertebrates. Mar. Drugs 2025, 23, 16. [Google Scholar] [CrossRef]
- Pyne, N.; Ray, R.; Paul, S. Computational and Experimental Approaches Manifest the Leishmanicidal Potential of α-Mangostin Resourced from Garcinia Cowa. Acta Trop. 2024, 257, 107291. [Google Scholar] [CrossRef]
- Herman, J.D.; Gallalee, J.V.; Best, J.M. Sodium Stibogluconate (Pentostam) Inhibition of Glucose Catabolism via the Glycolytic Pathway, and Fatty Acid β-Oxidation in leishmania mexicana Amastigotes. Biochem. Pharmacol. 1987, 36, 197–201. [Google Scholar] [CrossRef]
- Baneth, G.; Shaw, S.E. Chemotherapy of Canine Leishmaniosis. Vet. Parasitol. 2002, 106, 315–324. [Google Scholar] [CrossRef]
- Machado, G.U.; Prates, F.V.; Machado, P.R.L. Disseminated Leishmaniasis: Clinical, Pathogenic, and Therapeutic Aspects. An. Bras. Dermatol. 2019, 94, 9–16. [Google Scholar] [CrossRef]
- Fernández, M.; Arce, E.R.; Sarniguet, C.; Morais, T.S.; Tomaz, A.I.; Azar, C.O.; Figueroa, R.; Diego Maya, J.; Medeiros, A.; Comini, M.; et al. Novel Ruthenium(II) Cyclopentadienyl Thiosemicarbazone Compounds with Antiproliferative Activity on Pathogenic Trypanosomatid Parasites. J. Inorg. Biochem. 2015, 153, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Fandzloch, M.; Arriaga, J.M.M.; Sánchez-Moreno, M.; Wojtczak, A.; Jezierska, J.; Sitkowski, J.; Wiśniewska, J.; Salas, J.M.; Łakomska, I. Strategies for Overcoming Tropical Disease by Ruthenium Complexes with Purine Analog: Application against Leishmania spp. and Trypanosoma cruzi. J. Inorg. Biochem. 2017, 176, 144–155. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Arce, E.; Machado, I.; Rodríguez, B.; Lapier, M.; Zúñiga, M.C.; Maya, J.D.; Olea Azar, C.; Otero, L.; Gambino, D. Rhenium(I) Tricarbonyl Compounds of Bioactive Thiosemicarbazones: Synthesis, Characterization and Activity against Trypanosoma cruzi. J. Inorg. Biochem. 2017, 170, 125–133. [Google Scholar] [CrossRef]
- Nascimento, N.R.F.d.; Aguiar, F.L.N.d.; Santos, C.F.; Costa, A.M.L.; Hardoim, D. de J.; Calabrese, K. da S.; Almeida-Souza, F.; Sousa, E.H.S. de; Lopes, L.G. de F.; Teixeira, M.J.; et al. In Vitro and in Vivo Leishmanicidal Activity of a Ruthenium Nitrosyl Complex against Leishmania (Viannia) braziliensis. Acta Trop. 2019, 192, 61–65. [Google Scholar] [CrossRef]
- Braga, S.S. Ruthenium Complexes, an Emerging Class of Leishmanicidal Drug Candidates. Appl. Biosci. 2022, 1, 129–142. [Google Scholar] [CrossRef]
- Łakomska, I.; Fandzloch, M. Application of 1,2,4-Triazolo[1,5-a]pyrimidines for the Design of Coordination Compounds with Interesting Structures and New Biological Properties. Coord. Chem. Rev. 2016, 327–328, 221–241. [Google Scholar] [CrossRef]
- Salas, J.M.; Caballero, A.B.; Esteban-Parra, G.M.; Méndez-Arriaga, J.M. Leishmanicidal and Trypanocidal Activity of Metal Complexes with 1,2,4-Triazolo[1,5-a]pyrimidines: Insights on Their Therapeutic Potential against Leishmaniasis and Chagas Disease. Curr. Med. Chem. 2017, 24, 2796–2806. [Google Scholar] [CrossRef]
- Scalese, G.; Kostenkova, K.; Crans, D.C.; Gambino, D. Metallomics and Other Omics Approaches in Antiparasitic Metal-Based Drug Research. Curr. Opin. Chem. Biol. 2022, 67, 102127. [Google Scholar] [CrossRef]
- Rice, D.R.; Vacchina, P.; Norris-Mullins, B.; Morales, M.A.; Smith, B.D. Zinc(II)-Dipicolylamine Coordination Complexes as Targeting and Chemotherapeutic Agents for Leishmania Major. Antimicrob. Agents Chemother. 2016, 60, 2932–2940. [Google Scholar] [CrossRef]
- Soldera, P. de F.; Chagas, A.F. da S.; Brasil, A.M.V.; Comandolli-Wyrepkowski, C.D.; Porchia, M.; Pereira, A.M.R.F. In Vitro and in Vivo Anti-Leishmanial Potential of [Ag(PTA)4]BF4 and [Ag(HBPz3)(PPh3)] Silver Complexes. Rev. Soc. Bras. Med. Trop. 2022, 55, e0478. [Google Scholar] [CrossRef] [PubMed]
- Caballero, A.B.; Rodríguez-Diéguez, A.; Vidal, I.; Dobado, J.A.; Castillo, Ó.; Lezama, L.; Salas, J.M. Insights on the Binding Ability of a New Adenine Analog: 7-Amine-1,2,4-triazolo[1,5-a]pyrimidine. Synthesis and Magnetic Study of the First Copper(II) Complexes. Dalton Trans. 2012, 41, 1755–1764. [Google Scholar] [CrossRef]
- Caballero, A.B.; Rodríguez-Diéguez, A.; Salas, J.M.; Sánchez-Moreno, M.; Marín, C.; Ramírez-Macías, I.; Santamaría-Díaz, N.; Gutiérrez-Sánchez, R. Lanthanide Complexes Containing 5-Methyl-1,2,4-triazolo[1,5-a]pyrimidin-7(4H)-One and Their Therapeutic Potential to Fight Leishmaniasis and Chagas Disease. J. Inorg. Biochem. 2014, 138, 39–46. [Google Scholar] [CrossRef]
- Esteban-Parra, G.M.; Méndez-Arriaga, J.M.; Rodríguez-Diéguez, A.; Quirós, M.; Salas, J.M.; Sánchez-Moreno, M. High Antiparasitic Activity of Silver Complexes of 5,7-Dimethyl-1,2,4-triazolo[1,5-a]pyrimidine. J. Inorg. Biochem. 2019, 201, 110810. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Arriaga, J.M.; Oyarzabal, I.; Martín-Montes, Á.; García-Rodríguez, J.; Quirós, M.; Sánchez-Moreno, M. First Example of Antiparasitic Activity Influenced by Thermochromism: Leishmanicidal Evaluation of 5,7-Dimethyl-1,2,4-triazolo[1,5-a]pyrimidine Metal Complexes. Med. Chem. 2020, 16, 422–430. [Google Scholar] [CrossRef]
- García-García, A.; Méndez-Arriaga, J.M.; Martín-Escolano, R.; Cepeda, J.; Gómez-Ruiz, S.; Salinas-Castillo, A.; Seco, J.M.; Sánchez-Moreno, M.; Choquesillo-Lazarte, D.; Ruiz-Muelle, A.B.; et al. In Vitro Evaluation of Leishmanicidal Properties of a New Family of Monodimensional Coordination Polymers Based on Diclofenac Ligand. Polyhedron 2020, 184, 114570. [Google Scholar] [CrossRef]
- Sumithaa, C.; Ganeshpandian, M. Half-Sandwich Ruthenium Arene Complexes Bearing Clinically Approved Drugs as Ligands: The Importance of Metal–Drug Synergism in Metallodrug Design. Mol. Pharm. 2023, 20, 1453–1479. [Google Scholar] [CrossRef] [PubMed]
- de Souza, C.C.; de Azevedo-França, J.A.; Barrias, E.; Cavalcante, S.C.F.; Vieira, E.G.; Ferreira, A.M.D.C.; de Souza, W.; Navarro, M. Silver and Copper-Benznidazole Derivatives as Potential Antiparasitic Metallodrugs: Synthesis, Characterization, and Biological Evaluation. J. Inorg. Biochem. 2023, 239, 112047. [Google Scholar] [CrossRef]
- Damodharan, J. Nanomaterials in Medicine—An Overview. Mater. Today: Proc. 2021, 37, 383–385. [Google Scholar] [CrossRef]
- Yusuf, A.; Almotairy, A.R.Z.; Henidi, H.; Alshehri, O.Y.; Aldughaim, M.S. Nanoparticles as Drug Delivery Systems: A Review of the Implication of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers 2023, 15, 1596. [Google Scholar] [CrossRef]
- Díaz-García, D.; Fischer-Fodor, E.; Vlad, C.I.; Méndez-Arriaga, J.M.; Prashar, S.; Gómez-Ruiz, S. Study of Cancer Cell Cytotoxicity, Internalization and Modulation of Growth Factors Induced by Transferrin-Conjugated Formulations of Metallodrug-Functionalized Mesoporous Silica Nanoparticles. Microporous Mesoporous Mater. 2021, 323, 111238. [Google Scholar] [CrossRef]
- Jimenez-Falcao, S.; Torres, D.; Martínez-Ruiz, P.; Vilela, D.; Martínez-Máñez, R.; Villalonga, R. Sucrose-Responsive Intercommunicated Janus Nanoparticles Network. Nanomaterials 2021, 11, 2492. [Google Scholar] [CrossRef]
- Mitchell, M.J.; Billingsley, M.M.; Haley, R.M.; Wechsler, M.E.; Peppas, N.A.; Langer, R. Engineering Precision Nanoparticles for Drug Delivery. Nat. Rev. Drug Discov. 2021, 20, 101–124. [Google Scholar] [CrossRef] [PubMed]
- Hierro, I.d.; Pérez, Y.; Fajardo, M. Supported Choline Hydroxide (Ionic Liquid) on Mesoporous Silica as Heterogeneous Catalyst for Knoevenagel Condensation Reactions. Microporous Mesoporous Mater. 2018, 263, 173–180. [Google Scholar] [CrossRef]
- Carvalho, G.C.; Sábio, R.M.; de Cássia Ribeiro, T.; Monteiro, A.S.; Pereira, D.V.; Ribeiro, S.J.L.; Chorilli, M. Highlights in Mesoporous Silica Nanoparticles as a Multifunctional Controlled Drug Delivery Nanoplatform for Infectious Diseases Treatment. Pharm. Res. 2020, 37, 191. [Google Scholar] [CrossRef]
- Díaz-García, D.; Ferrer-Donato, Á.; Méndez-Arriaga, J.M.; Cabrera-Pinto, M.; Díaz-Sánchez, M.; Prashar, S.; Fernandez-Martos, C.M.; Gómez-Ruiz, S. Design of Mesoporous Silica Nanoparticles for the Treatment of Amyotrophic Lateral Sclerosis (ALS) with a Therapeutic Cocktail Based on Leptin and Pioglitazone. ACS Biomater. Sci. Eng. 2022, 8, 4838–4849. [Google Scholar] [CrossRef] [PubMed]
- Tessarolo, L.D.; Mello, C.P.; Lima, D.B.; Magalhães, E.P.; Bezerra, E.M.; Sales, F.A.M.; Neto, I.L.B.; de Fátima Oliveira, M.; Dos Santos, R.P.; Albuquerque, E.L.; et al. Nanoencapsulation of Benznidazole in Calcium Carbonate Increases Its Selectivity to Trypanosoma cruzi. Parasitology 2018, 145, 1191–1198. [Google Scholar] [CrossRef]
- Arrúa, E.C.; Seremeta, K.P.; Bedogni, G.R.; Okulik, N.B.; Salomon, C.J. Nanocarriers for Effective Delivery of Benznidazole and Nifurtimox in the Treatment of Chagas Disease: A Review. Acta Trop. 2019, 198, 105080. [Google Scholar] [CrossRef]
- Arrua, E.C.; Hartwig, O.; Loretz, B.; Goicoechea, H.; Murgia, X.; Lehr, C.-M.; Salomon, C.J. Improving the Oral Delivery of Benznidazole Nanoparticles by Optimizing the Formulation Parameters through a Design of Experiment and Optimization Strategy. Colloids Surf. B Biointerfaces 2022, 217, 112678. [Google Scholar] [CrossRef]
- Roy, S.; Mandal, C. Leishmania donovani Utilize Sialic Acids for Binding and Phagocytosis in the Macrophages through Selective Utilization of Siglecs and Impair the Innate Immune Arm. PLoS Negl. Trop. Dis. 2016, 10, e0004904. [Google Scholar] [CrossRef]
- Najer, A. Pathogen-Binding Nanoparticles to Inhibit Host Cell Infection by Heparan Sulfate and Sialic Acid Dependent Viruses and Protozoan Parasites. Smart Med. 2024, 3, e20230046. [Google Scholar] [CrossRef]
- Cavalcante, T.; Medeiros, M.M.; Mule, S.N.; Palmisano, G.; Stolf, B.S. The Role of Sialic Acids in the Establishment of Infections by Pathogens, with Special Focus on Leishmania. Front. Cell. Infect. Microbiol. 2021, 11, 671913. [Google Scholar] [CrossRef] [PubMed]
- Aguirre-Cruz, L.; Calderon, M.; Sotelo, J. Colchicine Decreases the Infection by Toxoplasma Gondii in Cultured Glial Cells. J. Parasitol. 1996, 82, 325–327. [Google Scholar] [CrossRef]
- Bhatia, S.; Hilsch, M.; Cuellar-Camacho, J.L.; Ludwig, K.; Nie, C.; Parshad, B.; Wallert, M.; Block, S.; Lauster, D.; Böttcher, C.; et al. Adaptive Flexible Sialylated Nanogels as Highly Potent Influenza A Virus Inhibitors. Angew. Chem. Int. Ed. 2020, 59, 12417–12422. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Trewyn, B.G.; Slowing, I.I.; Lin, V.S.-Y. Mesoporous Silica Nanoparticle-Based Double Drug Delivery System for Glucose-Responsive Controlled Release of Insulin and Cyclic AMP. J. Am. Chem. Soc. 2009, 131, 8398–8400. [Google Scholar] [CrossRef] [PubMed]
- Martín-Montes, Á.; Jimenez-Falcao, S.; Gómez-Ruiz, S.; Marín, C.; Mendez-Arriaga, J.M. First-Row Transition 7-Oxo-5-phenyl-1,2,4-triazolo[1,5-a]pyrimidine Metal Complexes: Antiparasitic Activity and Release Studies. Pharmaceuticals 2023, 16, 1380. [Google Scholar] [CrossRef]
- Iorhemba, M.A.; Álvarez-Conde, J.; Díaz-García, D.; Méndez-Arriaga, J.M.; García-Almodóvar, V.; Ovejero-Paredes, K.; Idris, S.O.; Shallangwa, G.A.; Abdulkadir, I.; Prashar, S.; et al. Vanadocene-Functionalized Mesoporous Silica Nanoparticles: Platforms for the Development of Theranostic Materials against Breast Cancer. Biomed. Mater. 2024, 19, 035005. [Google Scholar] [CrossRef]
- Iorhemba, M.A.; Ovejero-Paredes, K.; Díaz-García, D.; García-Almodóvar, V.; Idris, S.O.; Shallangwa, G.A.; Abdulkadir, I.; Méndez-Arriaga, J.M.; Prashar, S.; Filice, M.; et al. Amino Acid-Decorated Mesoporous Silica Nanoparticles Loaded with Titanocene Derivatives for Targeted Anticancer Studies. Appl. Organomet. Chem. 2024, 38, e7483. [Google Scholar] [CrossRef]
- Vallet-Regi, M.; Balas, F.; Colilla, M.; Manzano, M. Drug Confinement and Delivery in Ceramic Implants. Drug Metab. Lett. 2007, 1, 37–40. [Google Scholar] [CrossRef]
- Nastase, S.; Bajenaru, L.; Berger, D.; Matei, C.; Moisescu, M.; Constantin, D.; Savopol, T. Mesostructured Silica Matrix for Irinotecan Delivery Systems. Open Chem. 2014, 12, 813–820. [Google Scholar] [CrossRef]
- Moreno, D.; Plano, D.; Baquedano, Y.; Jiménez-Ruiz, A.; Antonio Palop, J.; Sanmartín, C. Antileishmanial Activity of Imidothiocarbamates and Imidoselenocarbamates. Parasitol. Res. 2011, 108, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, R.; Baker, H.; Seif, M.A.; Al-Qawasmeh, R.A.; Mataneh, A.-A.; Al-Gharabli, S.I. Photochemical Transformation of Colchicine: A Kinetic Study. J. Solut. Chem. 2010, 39, 441–456. [Google Scholar] [CrossRef]
- Nwaka, S.; Hudson, A. Innovative Lead Discovery Strategies for Tropical Diseases. Nat. Rev. Drug Discov. 2006, 5, 941–955. [Google Scholar] [CrossRef] [PubMed]
- Don, R.; Ioset, J.-R. Screening Strategies to Identify New Chemical Diversity for Drug Development to Treat Kinetoplastid Infections. Parasitology 2014, 141, 140–146. [Google Scholar] [CrossRef]

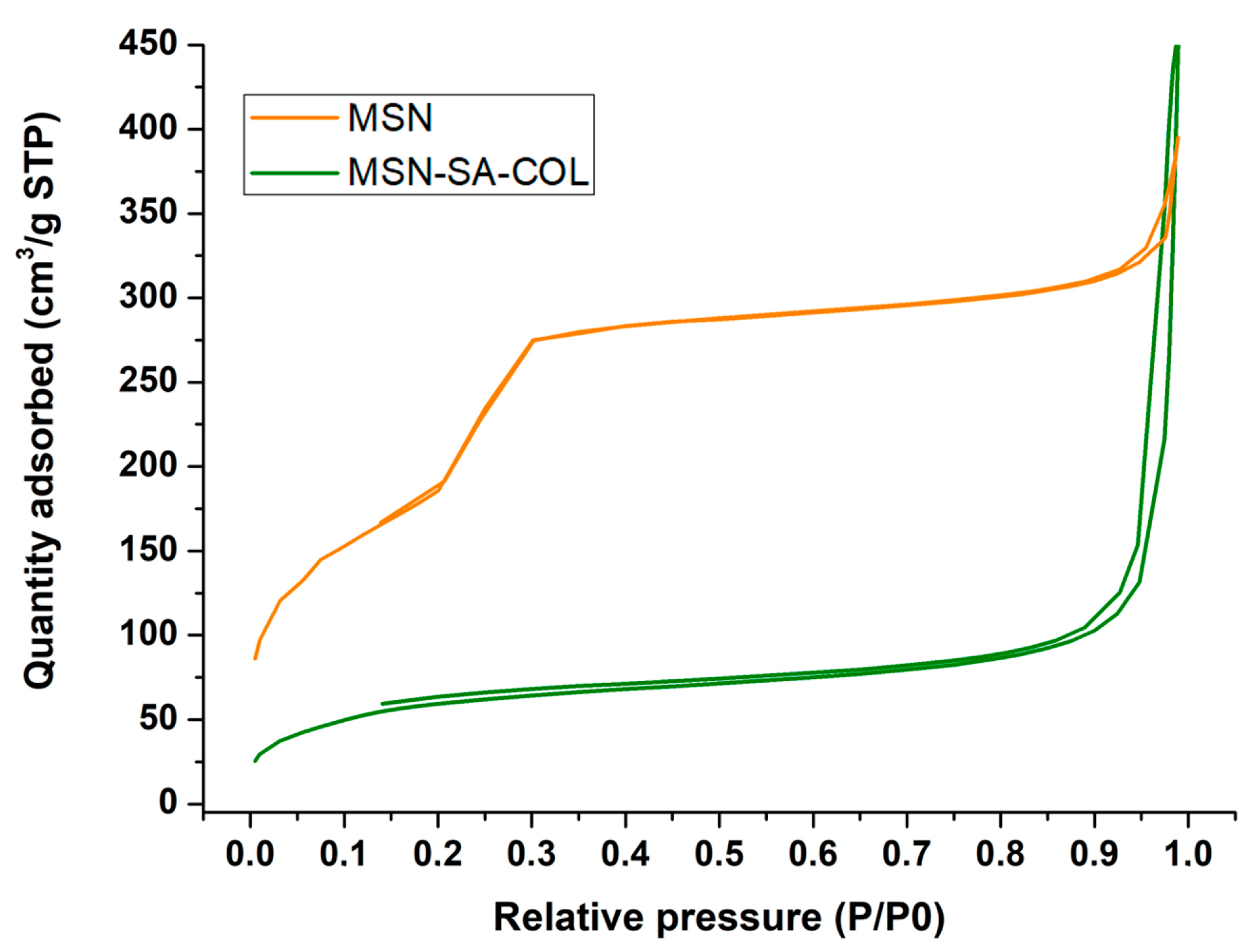
| Material | SBET (m2g−1) | Total Pore Volume (cm3g−1) |
| MSN | 682 | 0.52 |
| MSN-SA-COL | 222 | 0.33 |
| Products | IC50 a (Promastigote) | IC50 a (Vero Cells) | SI b | SI Corrected c |
|---|---|---|---|---|
| MSN | - | ≥0.5 mg/mL | - | - |
| MSN-AS | 0.08175 ± 12.46 mg/mL | ≥0.5 mg/mL | 6.12 | 7.58 (1) |
| MSN-AS-COL | 0.05529 ± 19.05 mg/mL | ≥0.5 mg/mL | 9.04 | 57.89 (9) |
| Glucantime | 64.88 ± 20.06 µM | ≥400 µM | 6.16 | - |
| AS | 149.9 ± 37.09 µM | ≥400 µM | 2.67 | - |
| COL | 19.68 ± 16.99 µM | ≥400 µM | 20.32 | - |
| Products | IC50 a (Amastigote) | SI b | SI Corrected c |
|---|---|---|---|
| MSN | - | - | - |
| MSN-AS | 0.06274 ± 13.93 mg/mL | 7.97 | 9.85 (0) |
| MSN-AS-COL | 0.03607 ± 10.08 mg/mL | 13.86 | 88.88 (4) |
| Glucantime | 17.26 ± 14.21 µM | 23.25 | - |
| AS | 130.30 ± 33.00 µM | 3.07 | - |
| COL | 9.51 ± 11.20 µM | 42.06 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galue-Parra, A.J.; Jimenez-Falcao, S.; Arribas-Yuste, E.; Marin, C.; Mendez-Arriaga, J.M. Sialic Acid and Colchicine Functionalized Silica Nanoparticles: A Novel Approach to Leishmanicidal Selective Treatments. Biomedicines 2025, 13, 1648. https://doi.org/10.3390/biomedicines13071648
Galue-Parra AJ, Jimenez-Falcao S, Arribas-Yuste E, Marin C, Mendez-Arriaga JM. Sialic Acid and Colchicine Functionalized Silica Nanoparticles: A Novel Approach to Leishmanicidal Selective Treatments. Biomedicines. 2025; 13(7):1648. https://doi.org/10.3390/biomedicines13071648
Chicago/Turabian StyleGalue-Parra, Adan Jesus, Sandra Jimenez-Falcao, Esther Arribas-Yuste, Clotilde Marin, and Jose Manuel Mendez-Arriaga. 2025. "Sialic Acid and Colchicine Functionalized Silica Nanoparticles: A Novel Approach to Leishmanicidal Selective Treatments" Biomedicines 13, no. 7: 1648. https://doi.org/10.3390/biomedicines13071648
APA StyleGalue-Parra, A. J., Jimenez-Falcao, S., Arribas-Yuste, E., Marin, C., & Mendez-Arriaga, J. M. (2025). Sialic Acid and Colchicine Functionalized Silica Nanoparticles: A Novel Approach to Leishmanicidal Selective Treatments. Biomedicines, 13(7), 1648. https://doi.org/10.3390/biomedicines13071648








