The Heart of Transformation: Exploring Artificial Intelligence in Cardiovascular Disease
Abstract
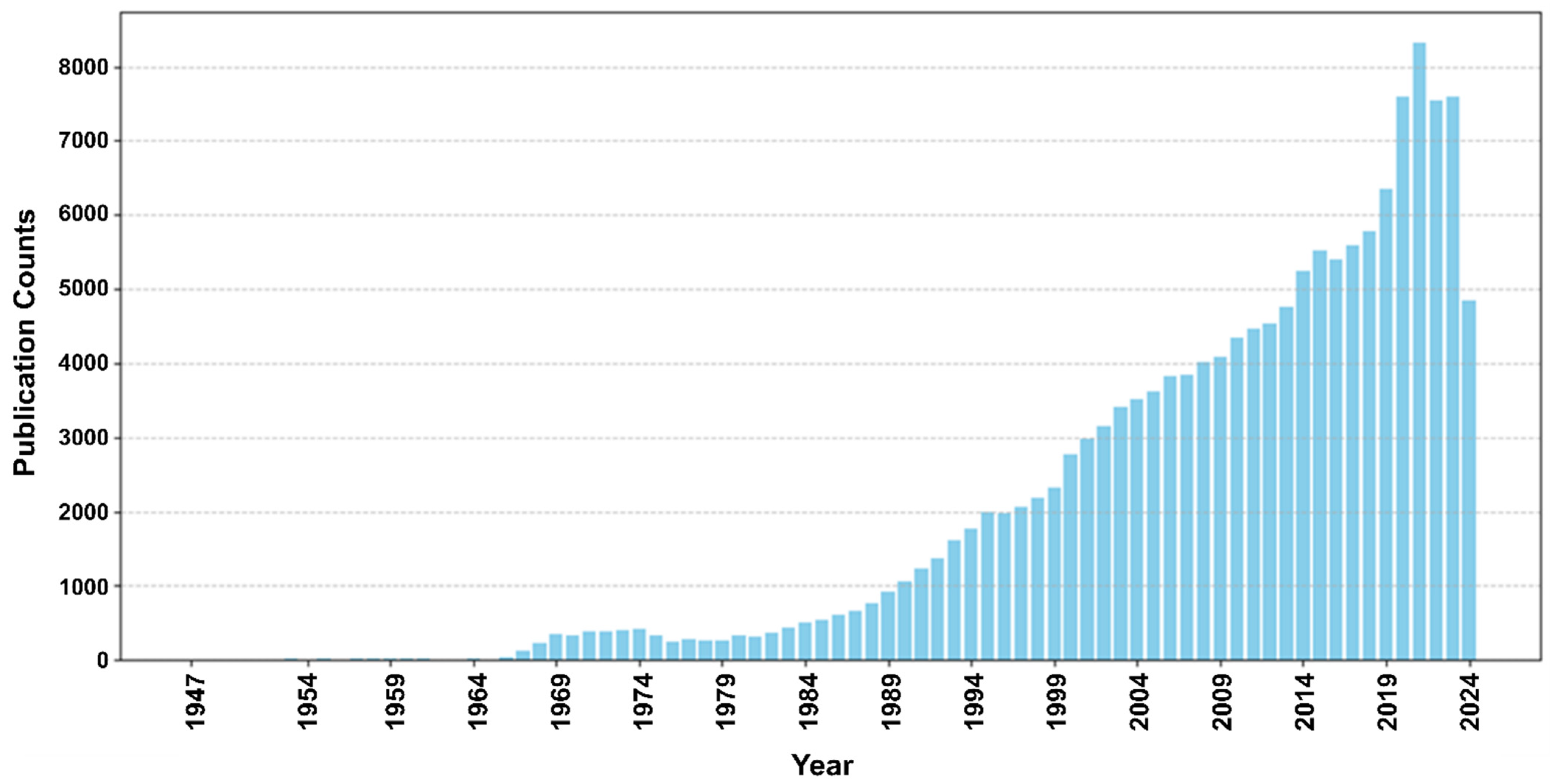
1. Introduction
- (1)
- Summarizing the recent progress of AI/ML applications in cardiovascular disease, particularly between 2022 and 2024.
- (2)
- Exploring commonly used AI/ML models and approaches in many different frontiers of cardiovascular care and health management.
- (3)
- Discussing the challenges, limitations, and potential solutions of AI/ML applications in cardiovascular disease.
- (4)
- Introducing policy and ethical considerations of AI/ML applications in cardiovascular disease.
- (5)
- Highlighting the promise of AI/ML applications and their future utility.
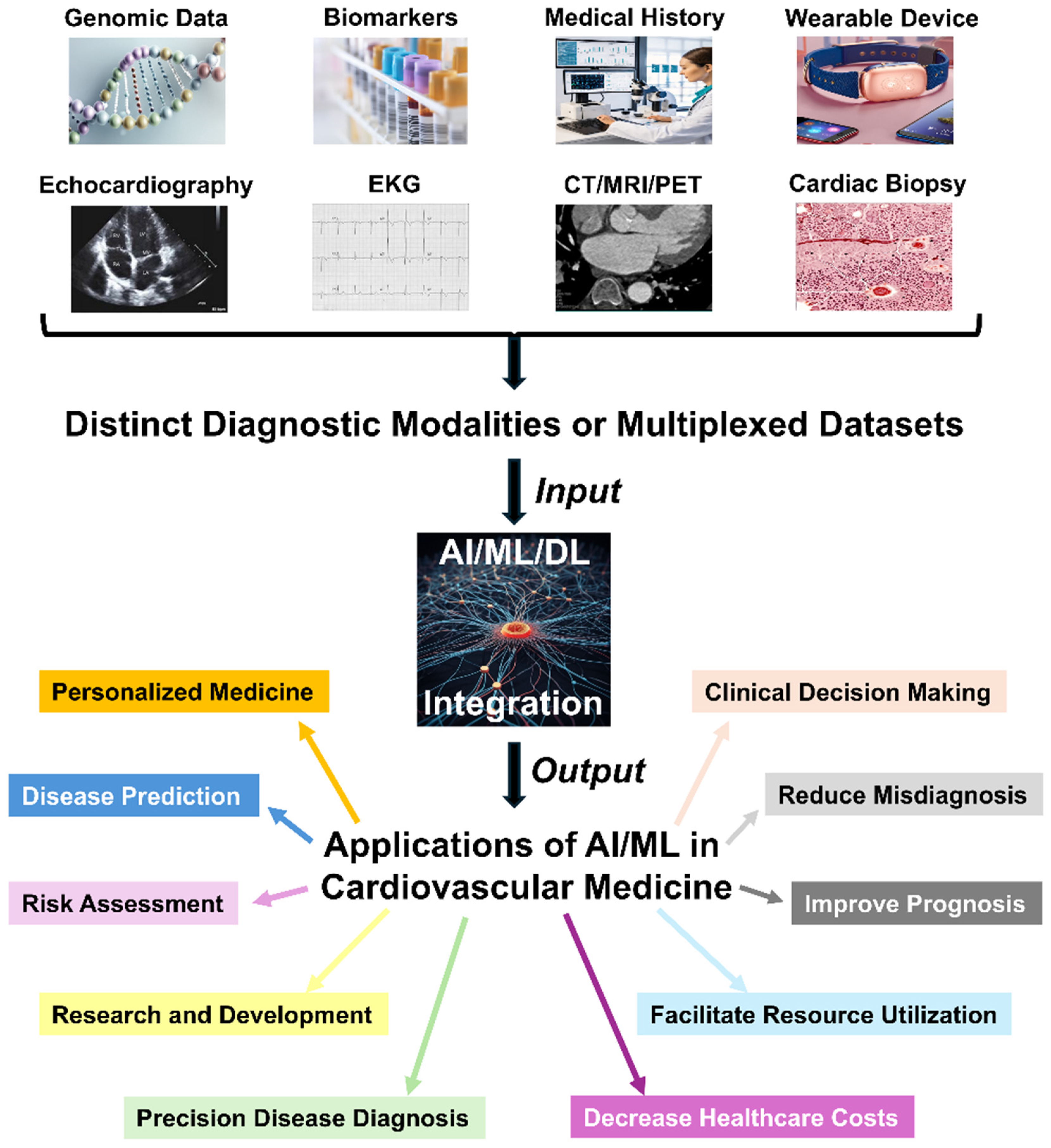
2. The Utility of AI in Cardiovascular Disease
2.1. Disease Diagnosis
2.1.1. AI Utility in Electrocardiograms (EKGs)
2.1.2. AI Utility in Echocardiograms
2.1.3. AI Utility in Cardiac CT and MRI
2.1.4. AI Utility in Other Aspects of Diagnostic Imaging
2.1.5. Future AI Utility for Cardiovascular Disease Diagnosis
2.2. Disease Prediction
2.3. Federated Learning for Cardiovascular Disease
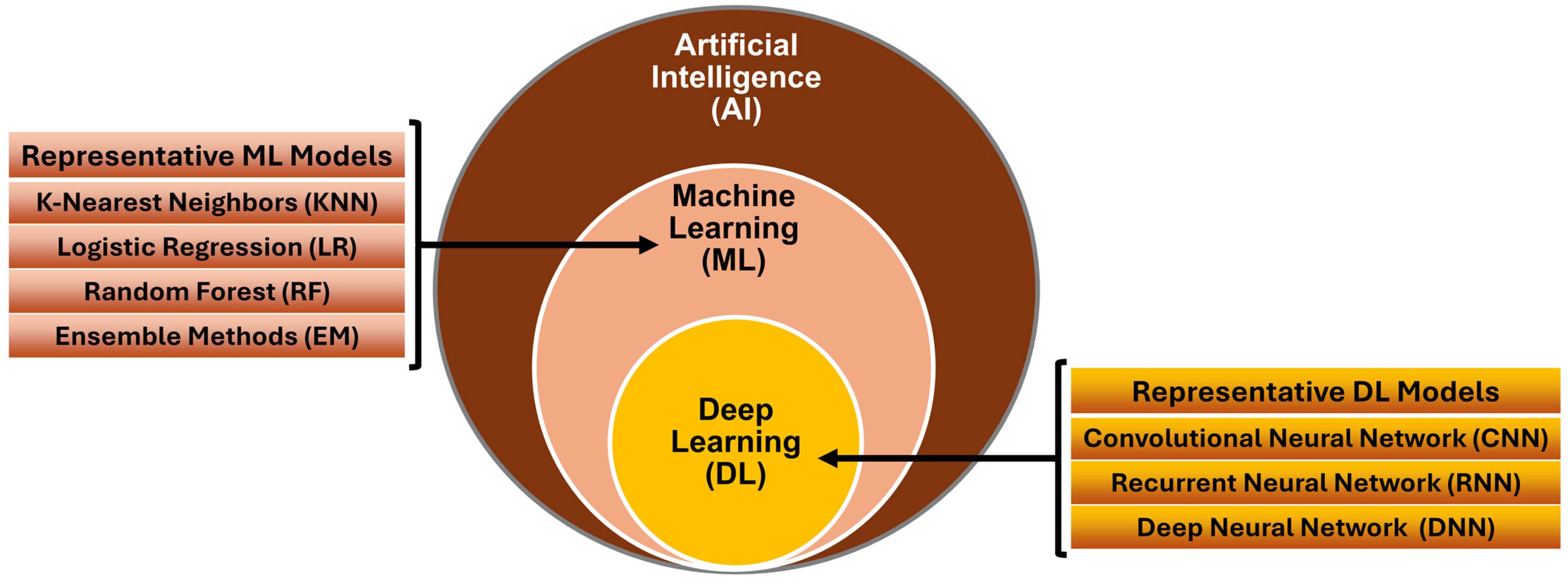
3. Current AI Models for Cardiovascular Disease
3.1. Machine Learning Models
- (1)
- K-nearest neighbors (KNN): KNN is a simple yet effective algorithm that classifies data points based on their proximity to other data points. KNN has been used to identify similar patients based on clinical features such as age, cholesterol level, and blood pressure [82].
- (2)
- Logistic regression (LR): LR is widely used for binary classification tasks. It has been used to estimate the probability of an individual developing cardiovascular disease based on risk factors. It is interpretable and valuable for understanding the impact of different features [82].
- (3)
- Random forest (RF): RFs combine multiple decision trees to improve predictive accuracy. They handle complex interactions between features and are robust against overfitting. RFs perform well due to their ensemble nature [82].
3.2. Deep Learning Models
- (1)
- Convolutional neural network (CNN): CNNs excel at processing image data. For cardiovascular medicine, CNNs can perform specific tasks to aid clinical diagnosis and treatment planning, such as segmenting and classifying heart images [82].
- (2)
- Recurrent neural network (RNN): RNNs are useful for time-series data, such as monitoring patients’ vital signs over time. RNNs can be used to predict disease progression or to detect anomalies [82].
- (3)
- Deep neural network (DNN): With their multiple hidden layers, DNNs can learn complex representations from diverse patient data. DNNs are valuable for risk prediction and personalized treatment recommendations [82].
- (4)
- Ensemble methods (EMs): EMs combine multiple ML/DL models to enhance performance. For example, XGBoost, a gradient-boosting algorithm and a widely used EM approach, has been successful in various medical applications, including cardiovascular disease prediction [83].
3.3. Other Models and Use Cases
4. AI in Cardiovascular Disease Diagnosis, Management, and Prognostication
4.1. Cardiovascular Research
4.2. Myocardial Infarction (MI)
4.3. Cardiac Arrhythmia
4.4. Heart Failure (HF)
4.5. Right Ventricular Failure (RVF)
4.6. Cardiogenic Shock (CS)
4.7. Mechanical Circulatory Support (MCS)
4.8. Cardiac Transplantation
4.9. Inherited and Rare Cardiovascular Diseases
4.10. Pulmonary Hypertension (PH)
4.11. Cardiac Amyloidosis (CA)
4.12. Cardio-Oncology
4.13. Implantable and Wearable Medical Devices
4.14. Improving Healthcare Resource Utilization
4.15. Reducing Healthcare Disparities
4.16. Knowledge Gaps Between Modeled and Real Clinical Practice
5. Challenges of AI in Cardiovascular Disease
6. Policy and Ethical Considerations of AI in Cardiovascular Disease
7. The Future of AI in Cardiovascular Disease
Author Contributions
Funding
Conflicts of Interest
References
- Vaduganathan, M.; Mensah, G.A.; Turco, J.V.; Fuster, V.; Roth, G.A. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J. Am. Coll. Cardiol. 2022, 80, 2361–2371. [Google Scholar] [CrossRef]
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar] [CrossRef]
- Joynt Maddox, K.E.; Elkind, M.S.V.; Aparicio, H.J.; Commodore-Mensah, Y.; de Ferranti, S.D.; Dowd, W.N.; Hernandez, A.F.; Khavjou, O.; Michos, E.D.; Palaniappan, L.; et al. Forecasting the Burden of Cardiovascular Disease and Stroke in the United States Through 2050—Prevalence of Risk Factors and Disease: A Presidential Advisory From the American Heart Association. Circulation 2024, 150, e65–e88. [Google Scholar] [CrossRef] [PubMed]
- Kazi, D.S.; Elkind, M.S.V.; Deutsch, A.; Dowd, W.N.; Heidenreich, P.; Khavjou, O.; Mark, D.; Mussolino, M.E.; Ovbiagele, B.; Patel, S.S.; et al. Forecasting the Economic Burden of Cardiovascular Disease and Stroke in the United States Through 2050: A Presidential Advisory From the American Heart Association. Circulation 2024, 150, e89–e101. [Google Scholar] [CrossRef]
- Fairweather, D.; Beetler, D.J.; Di Florio, D.N.; Musigk, N.; Heidecker, B.; Cooper, L.T., Jr. COVID-19, Myocarditis and Pericarditis. Circ. Res. 2023, 132, 1302–1319. [Google Scholar] [CrossRef] [PubMed]
- Knight, R.; Walker, V.; Ip, S.; Cooper, J.A.; Bolton, T.; Keene, S.; Denholm, R.; Akbari, A.; Abbasizanjani, H.; Torabi, F.; et al. Association of COVID-19 With Major Arterial and Venous Thrombotic Diseases: A Population-Wide Cohort Study of 48 Million Adults in England and Wales. Circulation 2022, 146, 892–906. [Google Scholar] [CrossRef] [PubMed]
- Gruetzemacher, R.; Whittlestone, J. The transformative potential of artificial intelligence. Futures 2022, 135, 102884. [Google Scholar] [CrossRef]
- Rahman, A.; Debnath, T.; Kundu, D.; Khan, M.S.I.; Aishi, A.A.; Sazzad, S.; Sayduzzaman, M.; Band, S.S. Machine learning and deep learning-based approach in smart healthcare: Recent advances, applications, challenges and opportunities. AIMS Public Health 2024, 11, 58–109. [Google Scholar] [CrossRef] [PubMed]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef]
- Clark, T.; Caufield, H.; Parker, J.A.; Al Manir, S.; Amorim, E.; Eddy, J.; Gim, N.; Gow, B.; Goar, W.; Haendel, M.; et al. AI-readiness for Biomedical Data: Bridge2AI Recommendations. bioRxiv 2024. [Google Scholar] [CrossRef]
- Wang, J.; Jiang, J.; Zhang, D.; Zhang, Y.Z.; Guo, L.; Jiang, Y.; Du, S.; Zhou, Q. An integrated AI model to improve diagnostic accuracy of ultrasound and output known risk features in suspicious thyroid nodules. Eur. Radiol. 2022, 32, 2120–2129. [Google Scholar] [CrossRef]
- Parekh, A.E.; Shaikh, O.A.; Simran; Manan, S.; Hasibuzzaman, M.A. Artificial intelligence (AI) in personalized medicine: AI-generated personalized therapy regimens based on genetic and medical history: Short communication. Ann. Med. Surg. 2023, 85, 5831–5833. [Google Scholar] [CrossRef]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Filipp, F.V. Opportunities for Artificial Intelligence in Advancing Precision Medicine. Curr. Genet. Med. Rep. 2019, 7, 208–213. [Google Scholar] [CrossRef]
- Vatansever, S.; Schlessinger, A.; Wacker, D.; Kaniskan, H.; Jin, J.; Zhou, M.M.; Zhang, B. Artificial intelligence and machine learning-aided drug discovery in central nervous system diseases: State-of-the-arts and future directions. Med. Res. Rev. 2021, 41, 1427–1473. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. npj Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef]
- Niazi, S.K. The Coming of Age of AI/ML in Drug Discovery, Development, Clinical Testing, and Manufacturing: The FDA Perspectives. Drug Des. Dev. Ther. 2023, 17, 2691–2725. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.Q.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision Medicine, AI, and the Future of Personalized Health Care. Clin. Transl. Sci. 2021, 14, 86–93. [Google Scholar] [CrossRef]
- Kourou, K.; Exarchos, K.P.; Papaloukas, C.; Sakaloglou, P.; Exarchos, T.; Fotiadis, D.I. Applied machine learning in cancer research: A systematic review for patient diagnosis, classification and prognosis. Comput. Struct. Biotechnol. J. 2021, 19, 5546–5555. [Google Scholar] [CrossRef]
- Khera, R.; Oikonomou, E.K.; Nadkarni, G.N.; Morley, J.R.; Wiens, J.; Butte, A.J.; Topol, E.J. Transforming Cardiovascular Care with Artificial Intelligence: From Discovery to Practice: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2024, 84, 97–114. [Google Scholar] [CrossRef]
- Singh, M.; Kumar, A.; Khanna, N.N.; Laird, J.R.; Nicolaides, A.; Faa, G.; Johri, A.M.; Mantella, L.E.; Fernandes, J.F.E.; Teji, J.S.; et al. Artificial intelligence for cardiovascular disease risk assessment in personalised framework: A scoping review. eClinicalMedicine 2024, 73, 102660. [Google Scholar] [CrossRef] [PubMed]
- Shu, S.; Ren, J.; Song, J. Clinical Application of Machine Learning-Based Artificial Intelligence in the Diagnosis, Prediction, and Classification of Cardiovascular Diseases. Circ. J. 2021, 85, 1416–1425. [Google Scholar] [CrossRef]
- Dixon, D.; Sattar, H.; Moros, N.; Kesireddy, S.R.; Ahsan, H.; Lakkimsetti, M.; Fatima, M.; Doshi, D.; Sadhu, K.; Junaid Hassan, M. Unveiling the Influence of AI Predictive Analytics on Patient Outcomes: A Comprehensive Narrative Review. Cureus 2024, 16, e59954. [Google Scholar] [CrossRef]
- Daniore, P.; Nittas, V.; Haag, C.; Bernard, J.; Gonzenbach, R.; von Wyl, V. From wearable sensor data to digital biomarker development: Ten lessons learned and a framework proposal. npj Digit. Med. 2024, 7, 161. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Cai, Y.-Q.; Tang, L.-Y.; Wang, Y.-H.; Gong, M.; Jing, T.-C.; Li, H.-J.; Li-Ling, J.; Hu, W.; Yin, Z.; et al. Artificial intelligence in the risk prediction models of cardiovascular disease and development of an independent validation screening tool: A systematic review. BMC Med. 2024, 22, 56. [Google Scholar] [CrossRef] [PubMed]
- Benjamins, J.W.; Hendriks, T.; Knuuti, J.; Juarez-Orozco, L.E.; van der Harst, P. A primer in artificial intelligence in cardiovascular medicine. Neth. Heart J. 2019, 27, 392–402. [Google Scholar] [CrossRef]
- Karatzia, L.; Aung, N.; Aksentijevic, D. Artificial intelligence in cardiology: Hope for the future and power for the present. Front. Cardiovasc. Med. 2022, 9, 945726. [Google Scholar] [CrossRef]
- Chaudhary, I.; Anwar, H. The Impact of Artificial Intelligence on Cardiovascular Disease Diagnosis: A Review. Pak. J. Med. Health Sci. 2024, 17, 8. [Google Scholar] [CrossRef]
- Quinn, G.R.; Ranum, D.; Song, E.; Linets, M.; Keohane, C.; Riah, H.; Greenberg, P. Missed Diagnosis of Cardiovascular Disease in Outpatient General Medicine: Insights from Malpractice Claims Data. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 508–516. [Google Scholar] [CrossRef] [PubMed]
- El Naqa, I.; Das, S. The role of machine and deep learning in modern medical physics. Med. Phys. 2020, 47, e125–e126. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, G.; Xu, Y.; Tang, X. Application of Artificial Intelligence in the MRI Classification Task of Human Brain Neurological and Psychiatric Diseases: A Scoping Review. Diagnostics 2021, 11, 1402. [Google Scholar] [CrossRef] [PubMed]
- Hannun, A.Y.; Rajpurkar, P.; Haghpanahi, M.; Tison, G.H.; Bourn, C.; Turakhia, M.P.; Ng, A.Y. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat. Med. 2019, 25, 65–69. [Google Scholar] [CrossRef]
- Siontis, K.C.; Noseworthy, P.A.; Attia, Z.I.; Friedman, P.A. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat. Rev. Cardiol. 2021, 18, 465–478. [Google Scholar] [CrossRef]
- Vaid, A.; Johnson, K.W.; Badgeley, M.A.; Somani, S.S.; Bicak, M.; Landi, I.; Russak, A.; Zhao, S.; Levin, M.A.; Freeman, R.S.; et al. Using Deep-Learning Algorithms to Simultaneously Identify Right and Left Ventricular Dysfunction From the Electrocardiogram. JACC Cardiovasc. Imaging 2022, 15, 395–410. [Google Scholar] [CrossRef]
- Zhou, J.; Du, M.; Chang, S.; Chen, Z. Artificial intelligence in echocardiography: Detection, functional evaluation, and disease diagnosis. Cardiovasc. Ultrasound 2021, 19, 29. [Google Scholar] [CrossRef]
- Zhang, J.; Gajjala, S.; Agrawal, P.; Tison, G.H.; Hallock, L.A.; Beussink-Nelson, L.; Lassen, M.H.; Fan, E.; Aras, M.A.; Jordan, C.; et al. Fully Automated Echocardiogram Interpretation in Clinical Practice. Circulation 2018, 138, 1623–1635. [Google Scholar] [CrossRef]
- Narula, S.; Shameer, K.; Salem Omar, A.M.; Dudley, J.T.; Sengupta, P.P. Machine-Learning Algorithms to Automate Morphological and Functional Assessments in 2D Echocardiography. J. Am. Coll. Cardiol. 2016, 68, 2287–2295. [Google Scholar] [CrossRef] [PubMed]
- Kelkar, A.A.; Schultz, W.M.; Khosa, F.; Schulman-Marcus, J.; O’Hartaigh, B.W.J.; Gransar, H.; Blaha, M.J.; Knapper, J.T.; Berman, D.S.; Quyyumi, A.; et al. Long-Term Prognosis After Coronary Artery Calcium Scoring Among Low-Intermediate Risk Women and Men. Circ. Cardiovasc. Imaging 2016, 9, e003742. [Google Scholar] [CrossRef]
- Wolterink, J.M.; Leiner, T.; de Vos, B.D.; van Hamersvelt, R.W.; Viergever, M.A.; Išgum, I. Automatic coronary artery calcium scoring in cardiac CT angiography using paired convolutional neural networks. Med. Image Anal. 2016, 34, 123–136. [Google Scholar] [CrossRef]
- Wang, X.; Yang, B.; Moody, J.B.; Tang, J. Improved myocardial perfusion PET imaging using artificial neural networks. Phys. Med. Biol. 2020, 65, 145010. [Google Scholar] [CrossRef] [PubMed]
- Kwiecinski, J.; Tzolos, E.; Meah, M.N.; Cadet, S.; Adamson, P.D.; Grodecki, K.; Joshi, N.V.; Moss, A.J.; Williams, M.C.; van Beek, E.J.R.; et al. Machine Learning with 18F-Sodium Fluoride PET and Quantitative Plaque Analysis on CT Angiography for the Future Risk of Myocardial Infarction. J. Nucl. Med. 2022, 63, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Yang, G.; Gao, Z.; Xu, C.; Zhang, Y.; Shi, R.; Keegan, J.; Xu, L.; Zhang, H.; Fan, Z.; et al. Deep Learning for Diagnosis of Chronic Myocardial Infarction on Nonenhanced Cardiac Cine MRI. Radiology 2019, 291, 606–617. [Google Scholar] [CrossRef]
- Chong, L.R.; Tsai, K.T.; Lee, L.L.; Foo, S.G.; Chang, P.C. Artificial Intelligence Predictive Analytics in the Management of Outpatient MRI Appointment No-Shows. AJR. Am. J. Roentgenol. 2020, 215, 1155–1162. [Google Scholar] [CrossRef]
- Ritchie, A.J.; Sanghera, C.; Jacobs, C.; Zhang, W.; Mayo, J.; Schmidt, H.; Gingras, M.; Pasian, S.; Stewart, L.; Tsai, S.; et al. Computer Vision Tool and Technician as First Reader of Lung Cancer Screening CT Scans. J. Thorac. Oncol. 2016, 11, 709–717. [Google Scholar] [CrossRef]
- Rodríguez-Ruiz, A.; Krupinski, E.; Mordang, J.J.; Schilling, K.; Heywang-Köbrunner, S.H.; Sechopoulos, I.; Mann, R.M. Detection of Breast Cancer with Mammography: Effect of an Artificial Intelligence Support System. Radiology 2019, 290, 305–314. [Google Scholar] [CrossRef]
- Wolterink, J.M.; Leiner, T.; Viergever, M.A.; Išgum, I. Generative Adversarial Networks for Noise Reduction in Low-Dose CT. IEEE Trans. Med. Imaging 2017, 36, 2536–2545. [Google Scholar] [CrossRef]
- van Leeuwen, K.G.; de Rooij, M.; Schalekamp, S.; van Ginneken, B.; Rutten, M. How does artificial intelligence in radiology improve efficiency and health outcomes? Pediatr. Radiol. 2022, 52, 2087–2093. [Google Scholar] [CrossRef]
- Chen, H.; Ouyang, D.; Baykaner, T.; Jamal, F.; Cheng, P.; Rhee, J.W. Artificial intelligence applications in cardio-oncology: Leveraging high dimensional cardiovascular data. Front. Cardiovasc. Med. 2022, 9, 941148. [Google Scholar] [CrossRef]
- Muehlematter, U.J.; Bluethgen, C.; Vokinger, K.N. FDA-cleared artificial intelligence and machine learning-based medical devices and their 510(k) predicate networks. Lancet Digit. Health 2023, 5, e618–e626. [Google Scholar] [CrossRef]
- Chiarito, M.; Luceri, L.; Oliva, A.; Stefanini, G.; Condorelli, G. Artificial Intelligence and Cardiovascular Risk Prediction: All That Glitters is not Gold. Eur. Cardiol. 2022, 17, e29. [Google Scholar] [CrossRef]
- Pettit, R.W.; Fullem, R.; Cheng, C.; Amos, C.I. Artificial intelligence, machine learning, and deep learning for clinical outcome prediction. Emerg. Top. Life Sci. 2021, 5, 729–745. [Google Scholar] [CrossRef]
- Pinton, P. Impact of artificial intelligence on prognosis, shared decision-making, and precision medicine for patients with inflammatory bowel disease: A perspective and expert opinion. Ann. Med. 2023, 55, 2300670. [Google Scholar] [CrossRef]
- Doudesis, D.; Lee, K.K.; Boeddinghaus, J.; Bularga, A.; Ferry, A.V.; Tuck, C.; Lowry, M.T.H.; Lopez-Ayala, P.; Nestelberger, T.; Koechlin, L.; et al. Machine learning for diagnosis of myocardial infarction using cardiac troponin concentrations. Nat. Med. 2023, 29, 1201–1210. [Google Scholar] [CrossRef]
- Boeddinghaus, J.; Doudesis, D.; Lopez-Ayala, P.; Lee, K.K.; Koechlin, L.; Wildi, K.; Nestelberger, T.; Borer, R.; Miró, Ò.; Martin-Sanchez, F.J.; et al. Machine Learning for Myocardial Infarction Compared With Guideline-Recommended Diagnostic Pathways. Circulation 2024, 149, 1090–1101. [Google Scholar] [CrossRef]
- Al’Aref, S.J.; Anchouche, K.; Singh, G.; Slomka, P.J.; Kolli, K.K.; Kumar, A.; Pandey, M.; Maliakal, G.; van Rosendael, A.R.; Beecy, A.N.; et al. Clinical applications of machine learning in cardiovascular disease and its relevance to cardiac imaging. Eur. Heart J. 2019, 40, 1975–1986. [Google Scholar] [CrossRef]
- Li, X.; Liu, X.; Deng, X.; Fan, Y. Interplay between Artificial Intelligence and Biomechanics Modeling in the Cardiovascular Disease Prediction. Biomedicines 2022, 10, 2157. [Google Scholar] [CrossRef]
- Wessler, B.S.; Lai YH, L.; Kramer, W.; Cangelosi, M.; Raman, G.; Lutz, J.S.; Kent, D.M. Clinical Prediction Models for Cardiovascular Disease. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 368–375. [Google Scholar] [CrossRef]
- Mallya, S.; Overhage, M.; Srivastava, N.; Arai, T.; Erdman, C. Effectiveness of lstms in predicting congestive heart failure onset. arXiv 2019, arXiv:1902.02443. [Google Scholar]
- Motwani, M.; Dey, D.; Berman, D.S.; Germano, G.; Achenbach, S.; Al-Mallah, M.H.; Andreini, D.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; et al. Machine learning for prediction of all-cause mortality in patients with suspected coronary artery disease: A 5-year multicentre prospective registry analysis. Eur. Heart J. 2017, 38, 500–507. [Google Scholar] [CrossRef]
- Mathur, P.; Srivastava, S.; Xu, X.; Mehta, J.L. Artificial Intelligence, Machine Learning, and Cardiovascular Disease. Clin. Med. Insights Cardiol. 2020, 14, 1179546820927404. [Google Scholar] [CrossRef] [PubMed]
- Kampaktsis, P.N.; Emfietzoglou, M.; Al Shehhi, A.; Fasoula, N.A.; Bakogiannis, C.; Mouselimis, D.; Tsarouchas, A.; Vassilikos, V.P.; Kallmayer, M.; Eckstein, H.H.; et al. Artificial intelligence in atherosclerotic disease: Applications and trends. Front. Cardiovasc. Med. 2022, 9, 949454. [Google Scholar] [CrossRef]
- Mohsen, F.; Al-Saadi, B.; Abdi, N.; Khan, S.; Shah, Z. Artificial Intelligence-Based Methods for Precision Cardiovascular Medicine. J. Pers. Med. 2023, 13, 1268. [Google Scholar] [CrossRef]
- Xu, J.; Glicksberg, B.S.; Su, C.; Walker, P.B.; Bian, J.; Wang, F. Federated Learning for Healthcare Informatics. J. Healthc. Inform. Res. 2019, 5, 1–19. [Google Scholar] [CrossRef]
- Upreti, D.; Yang, E.; Kim, H.; Seo, C. A Comprehensive Survey on Federated Learning in the Healthcare Area: Concept and Applications. Comput. Model. Eng. Sci. 2024, 140, 2239. [Google Scholar] [CrossRef]
- Rieke, N.; Hancox, J.; Li, W.; Milletarì, F.; Roth, H.R.; Albarqouni, S.; Bakas, S.; Galtier, M.; Landman, B.A.; Maier-Hein, K.H.; et al. The future of digital health with federated learning. npj Digit. Med. 2020, 3, 119. [Google Scholar] [CrossRef]
- Aouedi, O.; Sacco, A.; Piamrat, K.; Marchetto, G. Handling Privacy-Sensitive Medical Data With Federated Learning: Challenges and Future Directions. IEEE J. Biomed. Health Inform. 2022, 27, 790–803. [Google Scholar] [CrossRef]
- Gu, X.; Sabrina, F.; Fan, Z.; Sohail, S. A Review of Privacy Enhancement Methods for Federated Learning in Healthcare Systems. Int. J. Environ. Res. Public Health 2023, 20, 6539. [Google Scholar] [CrossRef]
- Islam, T.U.; Ghasemi, R.; Mohammed, N. Privacy-Preserving Federated Learning Model for Healthcare Data. In Proceedings of the 2022 IEEE 12th Annual Computing and Communication Workshop and Conference (CCWC), Las Vegas, NV, USA, 26–29 January 2022; pp. 0281–0287. [Google Scholar]
- Loftus, T.J.; Ruppert, M.M.; Shickel, B.; Ozrazgat-Baslanti, T.; Balch, J.A.; Efron, P.A.; Upchurch, G.R.; Rashidi, P.; Tignanelli, C.J.; Bian, J.; et al. Federated learning for preserving data privacy in collaborative healthcare research. Digit. Health 2022, 8, 20552076221134455. [Google Scholar] [CrossRef]
- Kolobkov, D.; Sharma, S.M.; Medvedev, A.; Lebedev, M.; Kosaretskiy, E.; Vakhitov, R. Efficacy of federated learning on genomic data: A study on the UK Biobank and the 1000 Genomes Project. Front. Big Data 2023, 7, 1266031. [Google Scholar] [CrossRef]
- Huang, L.; Liu, D. Patient Clustering Improves Efficiency of Federated Machine Learning to predict mortality and hospital stay time using distributed Electronic Medical Records. J. Biomed. Inform. 2019, 99, 103291. [Google Scholar] [CrossRef]
- Si, W.; Liu, C. Privacy Preservation Learning with Deep Cooperative Method for Multimedia Data Analysis. Secur. Commun. Netw. 2022, 2022, 8449987. [Google Scholar] [CrossRef]
- Islam, T.U.; Mohammed, N.; Alhadidi, D. Privacy preserving vertical distributed learning for health data. J. Surveill. Secur. Saf. 2024, 5, 1–18. [Google Scholar] [CrossRef]
- Omran, A.H.; Mohammed, S.Y.; Aljanabi, M.; Aljanabi, M. Detecting Data Poisoning Attacks in Federated Learning for Healthcare Applications Using Deep Learning. Iraqi J. Comput. Sci. Math. 2023, 4, 225–237. [Google Scholar]
- Dritsas, E.; Trigka, M. Efficient Data-Driven Machine Learning Models for Cardiovascular Diseases Risk Prediction. Sensors 2023, 23, 1161. [Google Scholar] [CrossRef]
- Bhatt, C.; Patel, P.; Ghetia, T.; Mazzeo, P.L. Effective Heart Disease Prediction Using Machine Learning Techniques. Algorithms 2023, 16, 88. [Google Scholar] [CrossRef]
- Baashar, Y.; Alkawsi, G.; Alhussian, H.; Capretz, L.F.; Alwadain, A.; Alkahtani, A.A.; Almomani, M. Effectiveness of Artificial Intelligence Models for Cardiovascular Disease Prediction: Network Meta-Analysis. Comput. Intell. Neurosci. 2022, 2022, 5849995. [Google Scholar] [CrossRef]
- Lee, S.; Chu, Y.; Ryu, J.; Park, Y.J.; Yang, S.; Koh, S.B. Artificial Intelligence for Detection of Cardiovascular-Related Diseases from Wearable Devices: A Systematic Review and Meta-Analysis. Yonsei Med. J. 2022, 63, S93–S107. [Google Scholar] [CrossRef]
- Krittanawong, C.; Virk, H.U.H.; Bangalore, S.; Wang, Z.; Johnson, K.W.; Pinotti, R.; Zhang, H.; Kaplin, S.; Narasimhan, B.; Kitai, T.; et al. Machine learning prediction in cardiovascular diseases: A meta-analysis. Sci. Rep. 2020, 10, 16057. [Google Scholar] [CrossRef]
- Mohan, S.; Thirumalai, C.; Srivastava, G. Effective Heart Disease Prediction Using Hybrid Machine Learning Techniques. IEEE Access 2019, 7, 81542–81554. [Google Scholar] [CrossRef]
- Abdar, M.; Książek, W.; Acharya, U.R.; Tan, R.S.; Makarenkov, V.; Pławiak, P. A new machine learning technique for an accurate diagnosis of coronary artery disease. Comput. Methods Programs Biomed. 2019, 179, 104992. [Google Scholar] [CrossRef]
- Sun, X.; Yin, Y.; Yang, Q.; Huo, T. Artificial intelligence in cardiovascular diseases: Diagnostic and therapeutic perspectives. Eur. J. Med. Res. 2023, 28, 242. [Google Scholar] [CrossRef]
- Bernand, C.; Mirand, E.; Aryun, M. Coronary heart disease prediction models using machine learning and deep learning algorithms. In Proceedings of the 8th International Conference on Engineering, Technology, and Industrial Applications 2021 (8th Icetia 2021): Engineering, Environment, and Health: Exploring the Opportunities for the Future, Surakarta, Indonesia, 15–16 December 2021. [Google Scholar]
- Srinivasan, S.; Gunasekaran, S.; Mathivanan, S.K.; Benjula Anbu Malar, M.B.; Jayagopal, P.; Dalu, G.T. An active learning machine technique based prediction of cardiovascular heart disease from UCI-repository database. Sci. Rep. 2023, 13, 13588. [Google Scholar] [CrossRef]
- Khera, R.; Haimovich, J.; Hurley, N.C.; McNamara, R.; Spertus, J.A.; Desai, N.; Rumsfeld, J.S.; Masoudi, F.A.; Huang, C.; Normand, S.-L.; et al. Use of Machine Learning Models to Predict Death After Acute Myocardial Infarction. JAMA Cardiol. 2021, 6, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Stewart, W.F.; Sun, J.; Ng, K.; Yan, X. Recurrent Neural Networks for Early Detection of Heart Failure From Longitudinal Electronic Health Record Data. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005114. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Schuetz, A.; Stewart, W.F.; Sun, J. Using recurrent neural network models for early detection of heart failure onset. J. Am. Med. Inform. Assoc. 2016, 24, 361–370. [Google Scholar] [CrossRef]
- Wang, H.; Fu, T.; Du, Y.; Gao, W.; Huang, K.; Liu, Z.; Chandak, P.; Liu, S.; Van Katwyk, P.; Deac, A.; et al. Scientific discovery in the age of artificial intelligence. Nature 2023, 620, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Jajcay, N.; Bezak, B.; Segev, A.; Matetzky, S.; Jankova, J.; Spartalis, M.; El Tahlawi, M.; Guerra, F.; Friebel, J.; Thevathasan, T.; et al. Data processing pipeline for cardiogenic shock prediction using machine learning. Front. Cardiovasc. Med. 2023, 10, 1132680. [Google Scholar] [CrossRef]
- Cunningham, J.W.; Singh, P.; Reeder, C.; Claggett, B.; Marti-Castellote, P.M.; Lau, E.S.; Khurshid, S.; Batra, P.; Lubitz, S.A.; Maddah, M.; et al. Natural Language Processing for Adjudication of Heart Failure Hospitalizations in a Multi-Center Clinical Trial. medRxiv 2023. [Google Scholar] [CrossRef]
- Khurshid, S.; Reeder, C.; Harrington, L.X.; Singh, P.; Sarma, G.; Friedman, S.F.; Di Achille, P.; Diamant, N.; Cunningham, J.W.; Turner, A.C.; et al. Cohort design and natural language processing to reduce bias in electronic health records research. npj Digit. Med. 2022, 5, 47. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, M.A.; Olesen, K.K.W.; Koul, S.; Gale, C.P.; Rylance, R.; Jernberg, T.; Baron, T.; Spaak, J.; James, S.; Lindahl, B.; et al. Development and validation of an artificial neural network algorithm to predict mortality and admission to hospital for heart failure after myocardial infarction: A nationwide population-based study. Lancet Digit. Health 2022, 4, e37–e45. [Google Scholar] [CrossRef]
- Frampton, J.; Ortengren, A.R.; Zeitler, E.P. Arrhythmias After Acute Myocardial Infarction. Yale J. Biol. Med. 2023, 96, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Dillon, S.M.; Allessie, M.A.; Ursell, P.C.; Wit, A.L. Influences of anisotropic tissue structure on reentrant circuits in the epicardial border zone of subacute canine infarcts. Circ. Res. 1988, 63, 182–206. [Google Scholar] [CrossRef]
- De Bakker, J.; Van Capelle, F.; Janse, M.J.; Tasseron, S.; Vermeulen, J.T.; de Jonge, N.; Lahpor, J.R. Slow conduction in the infarcted human heart. ‘Zigzag’course of activation. Circulation 1993, 88, 915–926. [Google Scholar] [CrossRef]
- Arevalo, H.J.; Vadakkumpadan, F.; Guallar, E.; Jebb, A.; Malamas, P.; Wu, K.C.; Trayanova, N.A. Arrhythmia risk stratification of patients after myocardial infarction using personalized heart models. Nat. Commun. 2016, 7, 11437. [Google Scholar] [CrossRef]
- Stevenson, W.G.; Friedman, P.L.; Kocovic, D.; Sager, P.T.; Saxon, L.A.; Pavri, B. Radiofrequency catheter ablation of ventricular tachycardia after myocardial infarction. Circulation 1998, 98, 308–314. [Google Scholar] [CrossRef]
- Prakosa, A.; Arevalo, H.J.; Deng, D.; Boyle, P.M.; Nikolov, P.P.; Ashikaga, H.; Blauer, J.J.E.; Ghafoori, E.; Park, C.J.; Blake, R.C., III; et al. Personalized virtual-heart technology for guiding the ablation of infarct-related ventricular tachycardia. Nat. Biomed. Eng. 2018, 2, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Kornej, J.; Börschel, C.S.; Benjamin, E.J.; Schnabel, R.B. Epidemiology of Atrial Fibrillation in the 21st Century: Novel Methods and New Insights. Circ. Res. 2020, 127, 4–20. [Google Scholar] [CrossRef]
- Tang, S.; Razeghi, O.; Kapoor, R.; Alhusseini, M.I.; Fazal, M.; Rogers, A.J.; Rodrigo Bort, M.; Clopton, P.; Wang, P.J.; Rubin, D.L.; et al. Machine Learning–Enabled Multimodal Fusion of Intra-Atrial and Body Surface Signals in Prediction of Atrial Fibrillation Ablation Outcomes. Circ. Arrhythmia Electrophysiol. 2022, 15, e010850. [Google Scholar] [CrossRef] [PubMed]
- Deisenhofer, I.; Albenque, J.-P.; Busch, S.; Gitenay, E.; Mountantonakis, S.; Roux, A.; Horvilleur, J.; Bakouboula, B.; Oza, S.R.; Abbey, S.; et al. LB-469805-01 Tailored Cardiac Ablation Procedure for Persistent Atrial Fibrillation Guided by Artificial Intelligence: The Tailored-AF Randomized Clinical Trial. Heart Rhythm 2024, 21, 1199. [Google Scholar] [CrossRef]
- Mehra, M.R.; Canter, C.E.; Hannan, M.M.; Semigran, M.J.; Uber, P.A.; Baran, D.A.; Danziger-Isakov, L.; Kirklin, J.K.; Kirk, R.; Kushwaha, S.S.; et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: A 10-year update. J. Heart Lung Transplant. 2016, 35, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Hearn, J.; Ross, H.J.; Mueller, B.; Fan, C.-P.; Crowdy, E.; Duhamel, J.; Walker, M.; Alba, A.C.; Manlhiot, C. Neural Networks for Prognostication of Patients With Heart Failure. Circ. Heart Fail. 2018, 11, e005193. [Google Scholar] [CrossRef] [PubMed]
- Adler, E.D.; Voors, A.A.; Klein, L.; Macheret, F.; Braun, O.O.; Urey, M.A.; Zhu, W.; Sama, I.; Tadel, M.; Campagnari, C.; et al. Improving risk prediction in heart failure using machine learning. Eur. J. Heart Fail. 2020, 22, 139–147. [Google Scholar] [CrossRef]
- Konstam, M.A.; Kiernan, M.S.; Bernstein, D.; Bozkurt, B.; Jacob, M.; Kapur, N.K.; Kociol, R.D.; Lewis, E.F.; Mehra, M.R.; Pagani, F.D.; et al. Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e578–e622. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, M.A.; Cook, J.M.; Moukarbel, G.V.; Ashtiani, S.; Schwann, T.A.; Bonnell, M.R.; Cooper, C.J.; Khouri, S.J. Pre-operative right ventricular echocardiographic parameters associated with short-term outcomes and long-term mortality after CABG. Echo Res. Prac. 2018, 5, 155–166. [Google Scholar] [CrossRef]
- Hameed, A.; Condliffe, R.; Swift, A.J.; Alabed, S.; Kiely, D.G.; Charalampopoulos, A. Assessment of Right Ventricular Function—A State of the Art. Curr. Heart Fail. Rep. 2023, 20, 194–207. [Google Scholar] [CrossRef] [PubMed]
- Shad, R.; Quach, N.; Fong, R.; Kasinpila, P.; Bowles, C.; Castro, M.; Guha, A.; Suarez, E.E.; Jovinge, S.; Lee, S.; et al. Predicting post-operative right ventricular failure using video-based deep learning. Nat. Commun. 2021, 12, 5192. [Google Scholar] [CrossRef]
- Van Diepen, S.; Katz, J.N.; Albert, N.M.; Henry, T.D.; Jacobs, A.K.; Kapur, N.K.; Kilic, A.; Menon, V.; Ohman, E.M.; Sweitzer, N.K. Contemporary management of cardiogenic shock: A scientific statement from the American Heart Association. Circulation 2017, 136, e232–e268. [Google Scholar] [CrossRef]
- Vahdatpour, C.; Collins, D.; Goldberg, S. Cardiogenic Shock. J. Am. Heart Assoc. 2019, 8, e011991. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, Y.; Yao, R.; Chen, K.; Xu, Q.; Huang, R.; Mao, Z.; Yu, Y. Identification of distinct clinical phenotypes of cardiogenic shock using machine learning consensus clustering approach. BMC Cardiovasc. Disord. 2023, 23, 426. [Google Scholar] [CrossRef]
- Rahman, F.; Finkelstein, N.; Alyakin, A.; Gilotra, N.A.; Trost, J.; Schulman, S.P.; Saria, S. Using Machine Learning for Early Prediction of Cardiogenic Shock in Patients With Acute Heart Failure. J. Soc. Cardiovasc. Angiogr. Interv. 2022, 1, 100308. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Antonescu, C.; Ravindranath, S.; Dong, J.; Lu, M.; Vicario, F.; Wondrely, L.; Thompson, P.; Swearingen, D.; Acharya, D. Early Prediction of Cardiogenic Shock Using Machine Learning. Front. Cardiovasc. Med. 2022, 9, 862424. [Google Scholar] [CrossRef] [PubMed]
- Stephens, A.F.; Šeman, M.; Diehl, A.; Pilcher, D.; Barbaro, R.P.; Brodie, D.; Pellegrino, V.; Kaye, D.M.; Gregory, S.D.; Hodgson, C.; et al. ECMO PAL: Using deep neural networks for survival prediction in venoarterial extracorporeal membrane oxygenation. Intensive Care Med. 2023, 49, 1090–1099. [Google Scholar] [CrossRef]
- Ayers, B.; Wood, K.; Gosev, I.; Prasad, S. Predicting Survival After Extracorporeal Membrane Oxygenation by Using Machine Learning. Ann. Thorac. Surg. 2020, 110, 1193–1200. [Google Scholar] [CrossRef]
- Kourou, K.; Rigas, G.; Exarchos, K.P.; Goletsis, Y.; Exarchos, T.P.; Jacobs, S.; Meyns, B.; Trivella, M.-G.; Fotiadis, D.I. Prediction of time dependent survival in HF patients after VAD implantation using pre- and post-operative data. Comput. Biol. Med. 2016, 70, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kilic, A.; Macickova, J.; Duan, L.; Movahedi, F.; Seese, L.; Zhang, Y.; Jacoski, M.V.; Padman, R. Machine Learning Approaches to Analyzing Adverse Events Following Durable LVAD Implantation. Ann. Thorac. Surg. 2021, 112, 770–777. [Google Scholar] [CrossRef] [PubMed]
- Kilic, A.; Dochtermann, D.; Padman, R.; Miller, J.K.; Dubrawski, A. Using machine learning to improve risk prediction in durable left ventricular assist devices. PLoS ONE 2021, 16, e0247866. [Google Scholar] [CrossRef]
- Bellavia, D.; Iacovoni, A.; Agnese, V.; Falletta, C.; Coronnello, C.; Pasta, S.; Novo, G.; di Gesaro, G.; Senni, M.; Maalouf, J.; et al. Usefulness of regional right ventricular and right atrial strain for prediction of early and late right ventricular failure following a left ventricular assist device implant: A machine learning approach. Int. J. Artif. Organs 2020, 43, 297–314. [Google Scholar] [CrossRef]
- Misumi, Y.; Miyagawa, S.; Yoshioka, D.; Kainuma, S.; Kawamura, T.; Kawamura, A.; Maruyama, Y.; Ueno, T.; Toda, K.; Asanoi, H.; et al. Prediction of aortic valve regurgitation after continuous-flow left ventricular assist device implantation using artificial intelligence trained on acoustic spectra. J. Artif. Organs 2021, 24, 164–172. [Google Scholar] [CrossRef]
- Topkara, V.K.; Elias, P.; Jain, R.; Sayer, G.; Burkhoff, D.; Uriel, N. Machine Learning-Based Prediction of Myocardial Recovery in Patients With Left Ventricular Assist Device Support. Circ. Heart Fail. 2022, 15, e008711. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, A.M.; Schlöglhofer, T.; Lauenroth, V.; Mueller, F.; Mueller, M.; Schoede, A.; Klopsch, C. Prevention and early treatment of driveline infections in ventricular assist device patients—The DESTINE staging proposal and the first standard of care protocol. J. Crit. Care 2020, 56, 106–112. [Google Scholar] [CrossRef]
- Skaria, R.; Aras, S.; Johnson, T.; Johnson, K.; Szep, J.; Gniady, C.; Hariri, S.; Khalpey, Z.I. Artificial Intelligence Improves Left Ventricular Assist Device Driveline Infections. J. Am. Coll. Surg. 2018, 227, e85. [Google Scholar] [CrossRef]
- Bhagra, S.K.; Pettit, S.; Parameshwar, J. Cardiac transplantation: Indications, eligibility and current outcomes. Heart 2019, 105, 252–260. [Google Scholar] [CrossRef]
- Medved, D.; Ohlsson, M.; Höglund, P.; Andersson, B.; Nugues, P.; Nilsson, J. Improving prediction of heart transplantation outcome using deep learning techniques. Sci. Rep. 2018, 8, 3613. [Google Scholar] [CrossRef]
- Medved, D.; Nugues, P.; Nilsson, J. Simulating the Outcome of Heart Allocation Policies Using Deep Neural Networks. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 6141–6144. [Google Scholar] [CrossRef]
- Yoon, J.; Zame, W.R.; Banerjee, A.; Cadeiras, M.; Alaa, A.M.; van der Schaar, M. Personalized survival predictions via Trees of Predictors: An application to cardiac transplantation. PLoS ONE 2018, 13, e0194985. [Google Scholar] [CrossRef]
- Miller, P.E.; Pawar, S.; Vaccaro, B.; McCullough, M.; Rao, P.; Ghosh, R.; Warier, P.; Desai, N.R.; Ahmad, T. Predictive Abilities of Machine Learning Techniques May Be Limited by Dataset Characteristics: Insights From the UNOS Database. J. Card. Fail. 2019, 25, 479–483. [Google Scholar] [CrossRef]
- Parkes, M.D.; Aliabadi, A.Z.; Cadeiras, M.; Crespo-Leiro, M.G.; Deng, M.; Depasquale, E.C.; Goekler, J.; Kim, D.H.; Kobashigawa, J.; Loupy, A.; et al. An integrated molecular diagnostic report for heart transplant biopsies using an ensemble of diagnostic algorithms. J. Heart Lung Transplant. 2019, 38, 636–646. [Google Scholar] [CrossRef]
- Nilsson, J.; Ohlsson, M.; Höglund, P.; Ekmehag, B.; Koul, B.; Andersson, B. The International Heart Transplant Survival Algorithm (IHTSA): A new model to improve organ sharing and survival. PLoS ONE 2015, 10, e0118644. [Google Scholar] [CrossRef]
- Gotlieb, N.; Azhie, A.; Sharma, D.; Spann, A.; Suo, N.-J.; Tran, J.; Orchanian-Cheff, A.; Wang, B.; Goldenberg, A.; Chassé, M.; et al. The promise of machine learning applications in solid organ transplantation. npj Digit. Med. 2022, 5, 89. [Google Scholar] [CrossRef]
- Adedinsewo, D.; Hardway, H.D.; Morales-Lara, A.C.; Wieczorek, M.A.; Johnson, P.W.; Douglass, E.J.; Dangott, B.J.; Nakhleh, R.E.; Narula, T.; Patel, P.C.; et al. Non-invasive detection of cardiac allograft rejection among heart transplant recipients using an electrocardiogram based deep learning model. Eur. Heart J. Digit. Health 2023, 4, 71–80. [Google Scholar] [CrossRef]
- Seraphin, T.P.; Luedde, M.; Roderburg, C.; van Treeck, M.; Scheider, P.; Buelow, R.D.; Boor, P.; Loosen, S.H.; Provaznik, Z.; Mendelsohn, D.; et al. Prediction of heart transplant rejection from routine pathology slides with self-supervised deep learning. Eur. Heart J. Digit. Health 2023, 4, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Hoda, M.R.; Grimm, M.; Laufer, G. Prediction of cyclosporine blood levels in heart transplantation patients using a pharmacokinetic model identified by evolutionary algorithms. J. Heart Lung Transpl. 2005, 24, 1855–1862. [Google Scholar] [CrossRef]
- Woillard, J.-B.; Labriffe, M.; Debord, J.; Marquet, P. Tacrolimus Exposure Prediction Using Machine Learning. Clin. Pharmacol. Ther. 2021, 110, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Musunuru, K.; Hershberger, R.E.; Day, S.M.; Klinedinst, N.J.; Landstrom, A.P.; Parikh, V.N.; Prakash, S.; Semsarian, C.; Sturm, A.C.; American Heart Association Council on Genomic and Precision Medicine; et al. Genetic Testing for Inherited Cardiovascular Diseases: A Scientific Statement From the American Heart Association. Circ. Genom. Precis. Med. 2020, 13, e000067. [Google Scholar] [CrossRef] [PubMed]
- Mao, D.; Liu, C.; Wang, L.; AI-Ouran, R.; Deisseroth, C.; Pasupuleti, S.; Kim, S.Y.; Li, L.; Rosenfeld, J.A.; Meng, L.; et al. AI-MARRVEL—A Knowledge-Driven AI System for Diagnosing Mendelian Disorders. NEJM AI 2024, 1, AIoa2300009. [Google Scholar] [CrossRef] [PubMed]
- Rich, J.D.; Rich, S. Clinical Diagnosis of Pulmonary Hypertension. Circulation 2014, 130, 1820–1830. [Google Scholar] [CrossRef]
- Tchuente Foguem, G.; Teguede Keleko, A. Artificial intelligence applied in pulmonary hypertension: A bibliometric analysis. AI Ethics 2023, 3, 1063–1093. [Google Scholar] [CrossRef]
- Hyde, B.; Paoli, C.J.; Panjabi, S.; Bettencourt, K.C.; Bell Lynum, K.S.; Selej, M. A claims-based, machine-learning algorithm to identify patients with pulmonary arterial hypertension. Pulm. Circ. 2023, 13, e12237. [Google Scholar] [CrossRef]
- Anand, V.; Weston, A.D.; Scott, C.G.; Kane, G.C.; Pellikka, P.A.; Carter, R.E. Machine Learning for Diagnosis of Pulmonary Hypertension by Echocardiography. Mayo Clin. Proc. 2024, 99, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Swinnen, K.; Verstraete, K.; Baratto, C.; Hardy, L.; De Vos, M.; Topalovic, M.; Claessen, G.; Quarck, R.; Belge, C.; Vachiery, J.L.; et al. Machine learning to differentiate pulmonary hypertension due to left heart disease from pulmonary arterial hypertension. ERJ Open Res. 2023, 9, 00229-2023. [Google Scholar] [CrossRef]
- Maurer, M.S.; Bokhari, S.; Damy, T.; Dorbala, S.; Drachman, B.M.; Fontana, M.; Grogan, M.; Kristen, A.V.; Lousada, I.; Nativi-Nicolau, J.; et al. Expert Consensus Recommendations for the Suspicion and Diagnosis of Transthyretin Cardiac Amyloidosis. Circ. Heart Fail. 2019, 12, e006075. [Google Scholar] [CrossRef]
- Grogan, M.; Murphree, D.H.; Shelly, M.; Dispenzieri, A.; Attia, Z.I.; Abou-Ezzeddine, O.; Lin, G.; Kapa, S.; Borgeson, D.; Friedman, P.; et al. Artificial-intelligence enhanced screening for cardiac amyloidosis by electrocardiography. J. Am. Coll. Cardiol. 2021, 77, 527. [Google Scholar] [CrossRef]
- Harmon, D.M.; Mangold, K.; Suarez, A.B.; Scott, C.G.; Murphree, D.H.; Malik, A.; Attia, Z.I.; Lopez-Jimenez, F.; Friedman, P.A.; Dispenzieri, A.; et al. Postdevelopment Performance and Validation of the Artificial Intelligence-Enhanced Electrocardiogram for Detection of Cardiac Amyloidosis. JACC Adv. 2023, 2, 100612. [Google Scholar] [CrossRef] [PubMed]
- Martinez, D.S.; Noseworthy, P.A.; Akbilgic, O.; Herrmann, J.; Ruddy, K.J.; Hamid, A.; Maddula, R.; Singh, A.; Davis, R.; Gunturkun, F.; et al. Artificial intelligence opportunities in cardio-oncology: Overview with spotlight on electrocardiography. Am. Heart J. Plus 2022, 15, 100129. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Liu, W.-T.; Chang, C.-H.; Lee, C.-C.; Hsing, S.-C.; Fang, W.-H.; Tsai, D.-J.; Chen, K.-C.; Lee, C.-H.; Cheng, C.-C.; et al. Artificial Intelligence–Powered Rapid Identification of ST-Elevation Myocardial Infarction via Electrocardiogram (ARISE)—A Pragmatic Randomized Controlled Trial. NEJM AI 2024, 1, AIoa2400190. [Google Scholar] [CrossRef]
- Lin, C.-S.; Liu, W.-T.; Tsai, D.-J.; Lou, Y.-S.; Chang, C.-H.; Lee, C.-C.; Fang, W.-H.; Wang, C.-C.; Chen, Y.-Y.; Lin, W.-S.; et al. AI-enabled electrocardiography alert intervention and all-cause mortality: A pragmatic randomized clinical trial. Nat. Med. 2024, 30, 1461–1470. [Google Scholar] [CrossRef]
- Noseworthy, P.A.; Attia, Z.I.; Behnken, E.M.; Giblon, R.E.; Bews, K.A.; Liu, S.; Gosse, T.A.; Linn, Z.D.; Deng, Y.; Yin, J.; et al. Artificial intelligence-guided screening for atrial fibrillation using electrocardiogram during sinus rhythm: A prospective non-randomised interventional trial. Lancet 2022, 400, 1206–1212. [Google Scholar] [CrossRef]
- Perez, M.V.; Mahaffey, K.W.; Hedlin, H.; Rumsfeld, J.S.; Garcia, A.; Ferris, T.; Balasubramanian, V.; Russo, A.M.; Rajmane, A.; Cheung, L.; et al. Large-Scale Assessment of a Smartwatch to Identify Atrial Fibrillation. N. Engl. J. Med. 2019, 381, 1909–1917. [Google Scholar] [CrossRef]
- New AAMC Report Shows Continuing Projected Physician Shortage. Available online: https://www.aamc.org/news/press-releases/new-aamc-report-shows-continuing-projected-physician-shortage (accessed on 23 January 2025).
- Martin, B.; Kaminski-Ozturk, N.; O’Hara, C.; Smiley, R. Examining the Impact of the COVID-19 Pandemic on Burnout and Stress Among U.S. Nurses. J. Nurs. Regul. 2023, 14, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.K.; Friese, C.R. Policy Strategies for Addressing Current Threats to the U.S. Nursing Workforce. N. Engl. J. Med. 2022, 386, 2454–2456. [Google Scholar] [CrossRef]
- Kane, R.L.; Shamliyan, T.A.; Mueller, C.; Duval, S.; Wilt, T.J. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Med. Care 2007, 45, 1195–1204. [Google Scholar] [CrossRef]
- Birger, M.; Kaldjian, A.S.; Roth, G.A.; Moran, A.E.; Dieleman, J.L.; Bellows, B.K. Spending on Cardiovascular Disease and Cardiovascular Risk Factors in the United States: 1996 to 2016. Circulation 2021, 144, 271–282. [Google Scholar] [CrossRef]
- Clifton, D.A.; Wong, D.; Clifton, L.; Wilson, S.; Way, R.; Pullinger, R.; Tarassenko, L. A large-scale clinical validation of an integrated monitoring system in the emergency department. IEEE J. Biomed. Health Inform. 2012, 17, 835–842. [Google Scholar] [CrossRef]
- Guglin, M.E.; Thatai, D. Common errors in computer electrocardiogram interpretation. Int. J. Cardiol. 2006, 106, 232–237. [Google Scholar] [CrossRef]
- Gandhi, T.K.; Classen, D.; Sinsky, C.A.; Rhew, D.C.; Vande Garde, N.; Roberts, A.; Federico, F. How can artificial intelligence decrease cognitive and work burden for front line practitioners? JAMIA Open 2023, 6, ooad079. [Google Scholar] [CrossRef]
- Hazarika, I. Artificial intelligence: Opportunities and implications for the health workforce. Int. Health 2020, 12, 241–245. [Google Scholar] [CrossRef]
- How AI Is Helping Doctors Communicate with Patients. Available online: https://www.aamc.org/news/how-ai-helping-doctors-communicate-patients (accessed on 23 January 2025).
- Babel, A.; Taneja, R.; Mondello Malvestiti, F.; Monaco, A.; Donde, S. Artificial Intelligence Solutions to Increase Medication Adherence in Patients With Non-communicable Diseases. Front. Digit. Health 2021, 3, 669869. [Google Scholar] [CrossRef]
- Armoundas, A.A.; Narayan, S.M.; Arnett, D.K.; Spector-Bagdady, K.; Bennett, D.A.; Celi, L.A.; Friedman, P.A.; Gollob, M.H.; Hall, J.L.; Kwitek, A.E.; et al. Use of Artificial Intelligence in Improving Outcomes in Heart Disease: A Scientific Statement From the American Heart Association. Circulation 2024, 149, e1028–e1050. [Google Scholar] [CrossRef] [PubMed]
- Curtis, R.G.; Bartel, B.; Ferguson, T.; Blake, H.T.; Northcott, C.; Virgara, R.; Maher, C.A. Improving user experience of virtual health assistants: Scoping review. J. Med. Internet Res. 2021, 23, e31737. [Google Scholar] [CrossRef]
- Sachdeva, S.; Bhatia, S.; Al Harrasi, A.; Shah, Y.A.; Anwer, K.; Philip, A.K.; Shah, S.F.A.; Khan, A.; Ahsan Halim, S. Unraveling the role of cloud computing in health care system and biomedical sciences. Heliyon 2024, 10, e29044. [Google Scholar] [CrossRef]
- Johnvictor, A.C.; Poonkodi, M.; Prem Sankar, N.; Vs, T. TinyML-Based Lightweight AI Healthcare Mobile Chatbot Deployment. J. Multidiscip. Heal. 2024, 17, 5091–5104. [Google Scholar] [CrossRef]
- Figueroa, C.A.; Aguilera, A.; Chakraborty, B.; Modiri, A.; Aggarwal, J.; Deliu, N.; Sarkar, U.; Jay Williams, J.; Lyles, C.R. Adaptive learning algorithms to optimize mobile applications for behavioral health: Guidelines for design decisions. J. Am. Med. Inform. Assoc. 2021, 28, 1225–1234. [Google Scholar] [CrossRef]
- Zhou, Q.; Chen, Z.-h.; Cao, Y.-h.; Peng, S. Clinical impact and quality of randomized controlled trials involving interventions evaluating artificial intelligence prediction tools: A systematic review. npj Digit. Med. 2021, 4, 154. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Gupta, A. Dealing with Noise Problem in Machine Learning Data-sets: A Systematic Review. Procedia Comput. Sci. 2019, 161, 466–474. [Google Scholar] [CrossRef]
- Liang, W.; Tadesse, G.A.; Ho, D.; Fei-Fei, L.; Zaharia, M.; Zhang, C.; Zou, J. Advances, challenges and opportunities in creating data for trustworthy AI. Nat. Mach. Intell. 2022, 4, 669–677. [Google Scholar] [CrossRef]
- Torkzadehmahani, R.; Nasirigerdeh, R.; Blumenthal, D.B.; Kacprowski, T.; List, M.; Matschinske, J.; Spaeth, J.; Wenke, N.K.; Baumbach, J. Privacy-Preserving Artificial Intelligence Techniques in Biomedicine. Methods Inform. Med. 2022, 61, e12–e27. [Google Scholar] [CrossRef]
- Murdoch, B. Privacy and artificial intelligence: Challenges for protecting health information in a new era. BMC Med. Ethics 2021, 22, 122. [Google Scholar] [CrossRef]
- Goetz, L.; Seedat, N.; Vandersluis, R.; van der Schaar, M. Generalization—A key challenge for responsible AI in patient-facing clinical applications. npj Digit. Med. 2024, 7, 126. [Google Scholar] [CrossRef] [PubMed]
- Tat, E.; Bhatt, D.L.; Rabbat, M.G. Addressing bias: Artificial intelligence in cardiovascular medicine. Lancet Digit. Health 2020, 2, e635–e636. [Google Scholar] [CrossRef]
- Dinov, I.D. Model Performance Assessment, Validation, and Improvement. In Data Science and Predictive Analytics: Biomedical and Health Applications Using R; Springer International Publishing: Cham, Switherland, 2023; pp. 477–531. [Google Scholar] [CrossRef]
- van Royen, F.S.; Asselbergs, F.W.; Alfonso, F.; Vardas, P.; van Smeden, M. Five critical quality criteria for artificial intelligence-based prediction models. Eur. Heart J. 2023, 44, 4831–4834. [Google Scholar] [CrossRef]
- Kwong, J.C.C.; Khondker, A.; Lajkosz, K.; McDermott, M.B.A.; Frigola, X.B.; McCradden, M.D.; Mamdani, M.; Kulkarni, G.S.; Johnson, A.E.W. APPRAISE-AI Tool for Quantitative Evaluation of AI Studies for Clinical Decision Support. JAMA Netw. Open 2023, 6, e2335377. [Google Scholar] [CrossRef]
- Vimbi, V.; Shaffi, N.; Mahmud, M. Interpreting artificial intelligence models: A systematic review on the application of LIME and SHAP in Alzheimer’s disease detection. Brain Inform. 2024, 11, 10. [Google Scholar] [CrossRef] [PubMed]
- Ponce-Bobadilla, A.V.; Schmitt, V.; Maier, C.S.; Mensing, S.; Stodtmann, S. Practical guide to SHAP analysis: Explaining supervised machine learning model predictions in drug development. Clin. Transl. Sci. 2024, 17, e70056. [Google Scholar] [CrossRef] [PubMed]
- Salih, A.M.; Raisi-Estabragh, Z.; Galazzo, I.B.; Radeva, P.; Petersen, S.E.; Lekadir, K.; Menegaz, G. A Perspective on Explainable Artificial Intelligence Methods: SHAP and LIME. Adv. Intell. Syst. 2024, 7, 2400304. [Google Scholar] [CrossRef]
- Riley, R.D.; Archer, L.; Snell, K.I.E.; Ensor, J.; Dhiman, P.; Martin, G.P.; Bonnett, L.J.; Collins, G.S. Evaluation of clinical prediction models (part 2): How to undertake an external validation study. BMJ 2024, 384, e074820. [Google Scholar] [CrossRef] [PubMed]
- Edafetanure-Ibeh, F. Advancing Predictive Insights in Cardiology: A Comparative Analysis of Machine Learning Models for Early Detection and Clinical Implications of Heart Disease. OSF Prepr. 2024. [Google Scholar] [CrossRef]
- Mooghali, M.; Stroud, A.M.; Yoo, D.W.; Barry, B.A.; Grimshaw, A.A.; Ross, J.S.; Zhu, X.; Miller, J.E. Barriers and Facilitators to Trustworthy and Ethical AI-enabled Medical Care From Patient’s and Healthcare Provider’s Perspectives: A Literature Review. medRxiv 2023. [Google Scholar] [CrossRef]
- Panjiyar, B.K.; Davydov, G.; Nashat, H.; Ghali, S.; Afifi, S.; Suryadevara, V.; Habab, Y.; Hutcheson, A.; Arcia Franchini, A.P. A Systematic Review: Do the Use of Machine Learning, Deep Learning, and Artificial Intelligence Improve Patient Outcomes in Acute Myocardial Ischemia Compared to Clinician-Only Approaches? Cureus 2023, 15, e43003. [Google Scholar] [CrossRef]
- Petrick, N.; Chen, W.; Delfino, J.G.; Gallas, B.D.; Kang, Y.; Krainak, D.; Sahiner, B.; Samala, R.K. Regulatory considerations for medical imaging AI/ML devices in the United States: Concepts and challenges. J. Med. Imaging 2023, 10, 051804. [Google Scholar] [CrossRef]
- Shipley, E.; Joddrell, M.; Lip, G.; Zheng, Y. Bridging the Gap Between Artificial Intelligence Research and Clinical Practice in Cardiovascular Science: What the Clinician Needs to Know. Arrhythmia Electrophysiol. Rev. 2022, 11, e03. [Google Scholar] [CrossRef]
- Farhud, D.D.; Zokaei, S. Ethical Issues of Artificial Intelligence in Medicine and Healthcare. Iran. J. Public Health 2021, 50, i–v. [Google Scholar] [CrossRef]
- Wang, C.; Zhang, J.; Lassi, N.; Zhang, X. Privacy Protection in Using Artificial Intelligence for Healthcare: Chinese Regulation in Comparative Perspective. Healthcare 2022, 10, 1878. [Google Scholar] [CrossRef]
- Khalid, N.; Qayyum, A.; Bilal, M.; Al-Fuqaha, A.; Qadir, J. Privacy-preserving artificial intelligence in healthcare: Techniques and applications. Comput. Biol. Med. 2023, 158, 106848. [Google Scholar] [CrossRef]
- Drabiak, K. Leveraging law and ethics to promote safe and reliable AI/ML in healthcare. Front. Nucl. Med. 2022, 2, 983340. [Google Scholar] [CrossRef]
- Arbelaez Ossa, L.; Milford, S.R.; Rost, M.; Leist, A.K.; Shaw, D.M.; Elger, B.S. AI Through Ethical Lenses: A Discourse Analysis of Guidelines for AI in Healthcare. Sci. Eng. Ethics 2024, 30, 24. [Google Scholar] [CrossRef] [PubMed]
- Papadakis, T.; Christou, I.T.; Ipektsidis, C.; Soldatos, J.; Amicone, A. Explainable and transparent artificial intelligence for public policymaking. Data Policy 2024, 6, e10. [Google Scholar] [CrossRef]
- Osasona, F.; Amoo, O.; Atadoga, A.; Abrahams, T.; Farayola, O.; Ayinla, B. REVIEWING THE ETHICAL IMPLICATIONS OF AI IN DECISION MAKING PROCESSES. Int. J. Manag. Entrep. Res. 2024, 6, 322–335. [Google Scholar] [CrossRef]
- Thoenes, M.; Agarwal, A.; Grundmann, D.; Ferrero, C.; McDonald, A.; Bramlage, P.; Steeds, R.P. Narrative review of the role of artificial intelligence to improve aortic valve disease management. J. Thorac. Dis. 2021, 13, 396–404. [Google Scholar] [CrossRef]
- Shiferaw, K.B.; Wali, P.; Waltemath, D.; Zeleke, A.A. Navigating the AI frontiers in cardiovascular research: A bibliometric exploration and topic modeling. Front. Cardiovasc. Med. 2023, 10, 1308668. [Google Scholar] [CrossRef]
- Stamate, E.; Piraianu, A.I.; Ciobotaru, O.R.; Crassas, R.; Duca, O.; Fulga, A.; Grigore, I.; Vintila, V.; Fulga, I.; Ciobotaru, O.C. Revolutionizing Cardiology through Artificial Intelligence-Big Data from Proactive Prevention to Precise Diagnostics and Cutting-Edge Treatment-A Comprehensive Review of the Past 5 Years. Diagnostics 2024, 14, 1103. [Google Scholar] [CrossRef] [PubMed]
- Doolub, G.; Mamalakis, M.; Alabed, S.; Van der Geest, R.J.; Swift, A.J.; Rodrigues, J.C.L.; Garg, P.; Joshi, N.V.; Dastidar, A. Artificial Intelligence as a Diagnostic Tool in Non-Invasive Imaging in the Assessment of Coronary Artery Disease. Med. Sci. 2023, 11, 20. [Google Scholar] [CrossRef] [PubMed]
| Study | Data | AI Model | Performance |
|---|---|---|---|
| Dritsas et al. [75] | Clinical | Stacking Ensemble Model with Synthetic Minority Oversampling TEchnique (SMOTE) | 87.8% accuracy, 88.3% recall, 88% precision, and 98.2% AUC |
| Bhat et al. [76] | Kaggle | Multi-Layer Perceptron (MLP) | 87.28% accuracy |
| Bashaar et al. [77] | Clinical | ANN, Gradient-Boosting Machine (GBM), SVM, RF | ANN: OR of 0.0905, CI of [0.0489; 0.1673]; GBM: average accuracy of 91.10%; SVM: OR of 25.0801, CI of [11.4824; 54.7803]; RF: OR of 10.8527, CI [4.7434; 24.8305] |
| Lee et al. [78] | Wearable Devices | DNN | AUROC of 0.981 |
| Krittanawong et al. [79] | SVM, Boosting Algorithms, CNN | SVM: AUC of 0.92; Boosting Algorithms: AUC of 0.91; CNN: AUC of 0.90 | |
| Mohan et al. [80] | Clinical | RF with a Linear Model | 88.7% accuracy |
| Abdar et al. [81] | Clinical | SVM | 93.08% accuracy, 91.51% F1-score |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chowdhury, M.A.; Rizk, R.; Chiu, C.; Zhang, J.J.; Scholl, J.L.; Bosch, T.J.; Singh, A.; Baugh, L.A.; McGough, J.S.; Santosh, K.; et al. The Heart of Transformation: Exploring Artificial Intelligence in Cardiovascular Disease. Biomedicines 2025, 13, 427. https://doi.org/10.3390/biomedicines13020427
Chowdhury MA, Rizk R, Chiu C, Zhang JJ, Scholl JL, Bosch TJ, Singh A, Baugh LA, McGough JS, Santosh K, et al. The Heart of Transformation: Exploring Artificial Intelligence in Cardiovascular Disease. Biomedicines. 2025; 13(2):427. https://doi.org/10.3390/biomedicines13020427
Chicago/Turabian StyleChowdhury, Mohammed A., Rodrigue Rizk, Conroy Chiu, Jing J. Zhang, Jamie L. Scholl, Taylor J. Bosch, Arun Singh, Lee A. Baugh, Jeffrey S. McGough, KC Santosh, and et al. 2025. "The Heart of Transformation: Exploring Artificial Intelligence in Cardiovascular Disease" Biomedicines 13, no. 2: 427. https://doi.org/10.3390/biomedicines13020427
APA StyleChowdhury, M. A., Rizk, R., Chiu, C., Zhang, J. J., Scholl, J. L., Bosch, T. J., Singh, A., Baugh, L. A., McGough, J. S., Santosh, K., & Chen, W. C. W. (2025). The Heart of Transformation: Exploring Artificial Intelligence in Cardiovascular Disease. Biomedicines, 13(2), 427. https://doi.org/10.3390/biomedicines13020427






