Evaluation of Stereopsis Performance, Gaze Direction and Pupil Diameter in Post-COVID Syndrome Using Machine Learning
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
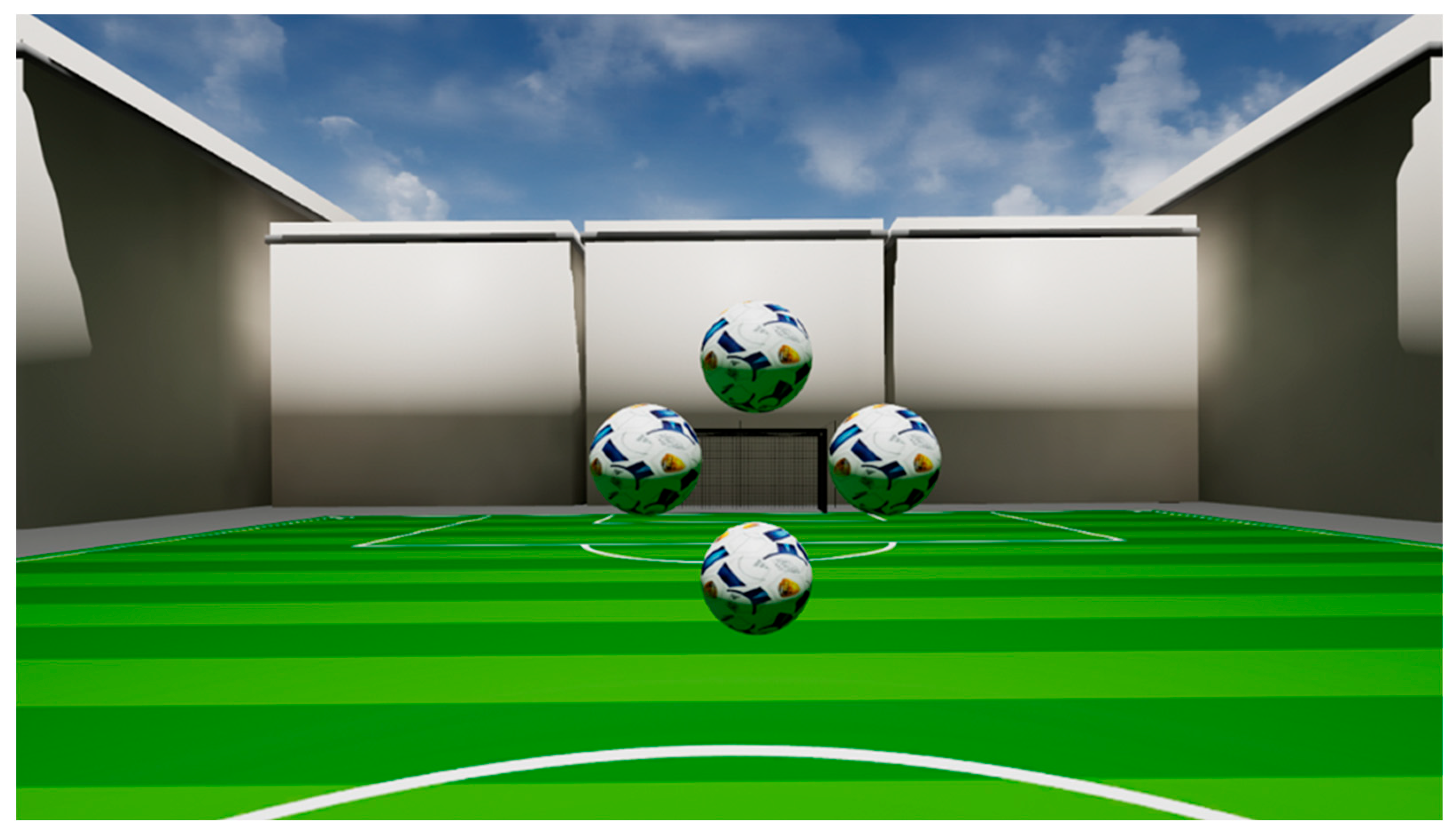
2.2. VR-OTS
2.2.1. Stereopsis Performance Features
2.2.2. Pupil Diameter Features
2.2.3. Gaze Behavior
2.2.4. Evaluation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| arcsec | arc-sec |
| AUROC | area under receiver operating characteristic |
| CNS | Central nervous system |
| IPA | Index of Pupillary Activity |
| LC | long COVID |
| LHIPA | Low/High Index of Pupillary Activity |
| PASC | post-acute sequelae of COVID-19 |
| PCS | Post-COVID-19-syndrome |
| PCR | Polymerase Chain Reaction |
| SARS-CoV-2 | severe acute respiratory syndrome coronavirus 2 |
| SVM | Support vector machines |
| VR-OTS | Virtual-Reality-oculomotor-test-system |
Appendix A
| Parameter | Difficulty | Mean AUROC ± Standard Deviation |
|---|---|---|
| Accuracy | 275 | 0.59 ± 0.10 |
| maximum (reaction time) | 275 | 0.63 ± 0.13 |
| minimum (reaction time) | 275 | 0.68 ± 0.10 |
| median (reaction time) | 275 | 0.68 ± 0.10 |
| mean (reaction time) | 275 | 0.68 ± 0.09 |
| standard deviation (reaction time) | 275 | 0.64 ± 0.10 |
| variance (reaction time) | 275 | 0.62 ± 0.11 |
| skewness (reaction time) | 275 | 0.62 ± 0.06 |
| kurtosis (reaction time) | 275 | 0.63 ± 0.09 |
| accuracy (reaction time) | 550 | 0.56 ± 0.07 |
| maximum (reaction time) | 550 | 0.68 ± 0.08 |
| minimum (reaction time) | 550 | 0.64 ± 0.09 |
| median (reaction time) | 550 | 0.68 ± 0.08 |
| mean (reaction time) | 550 | 0.67 ± 0.09 |
| standard deviation (reaction time) | 550 | 0.66 ± 0.08 |
| variance (reaction time) | 550 | 0.66 ± 0.07 |
| skewness (reaction time) | 550 | 0.54 ± 0.09 |
| kurtosis (reaction time) | 550 | 0.54 ± 0.12 |
| accuracy (reaction time) | 1100 | 0.53 ± 0.07 |
| maximum (reaction time) | 1100 | 0.64 ± 0.10 |
| minimum (reaction time) | 1100 | 0.65 ± 0.08 |
| median (reaction time) | 1100 | 0.66 ± 0.10 |
| mean (reaction time) | 1100 | 0.67 ± 0.10 |
| standard deviation (reaction time) | 1100 | 0.62 ± 0.10 |
| variance (reaction time) | 1100 | 0.62 ± 0.10 |
| skewness (reaction time) | 1100 | 0.59 ± 0.09 |
| kurtosis (reaction time) | 1100 | 0.60 ± 0.09 |
| median gain Disp 275-1100 | 275-1100 | 0.60 ± 0.10 |
| median gain Disp 550-1100 | 550-1100 | 0.60 ± 0.07 |
| Parameter | Mean AUROC ± Standard Deviation |
|---|---|
| maximum (amplitude) | 0.54 ± 0.06 |
| median (amplitude) | 0.58 ± 0.17 |
| mean (amplitude) | 0.61 ± 0.11 |
| Standard deviation (amplitude) | 0.59 ± 0.10 |
| variance (amplitude) | 0.59 ± 0.10 |
| skewness (amplitude) | 0.65 ± 0.08 |
| kurtosis (amplitude) | 0.61 ± 0.11 |
| entropy (amplitude) | 0.61 ± 0.11 |
| maximum (angular velocity) | 0.52 ± 0.07 |
| median (angular velocity) | 0.58 ± 0.17 |
| mean (angular velocity) | 0.61 ± 0.12 |
| Standard deviation (angular velocity) | 0.60 ± 0.11 |
| variance (angular velocity) | 0.60 ± 0.11 |
| skewness (angular velocity) | 0.62 ± 0.09 |
| kurtosis (angular velocity) | 0.62 ± 0.10 |
| entropy (angular velocity) | 0.62 ± 0.09 |
| fixation duration | 0.70 ± 0.09 |
| fixation duration (background) | 0.67 ± 0.08 |
| fixation duration (ball up) | 0.61 ± 0.07 |
| fixation duration (ball down) | 0.64 ± 0.10 |
| fixation duration (ball left) | 0.62 ± 0.10 |
| fixation duration (ball right) | 0.65 ± 0.10 |
| ball transitions | 0.64 ± 0.10 |
| mean ball transitions per trial | 0.64 ± 0.10 |
| Parameter | Difficulty | Mean AUROC ± Standard Deviation |
|---|---|---|
| maximum (diameter) | 275-550-1100 | 0.60 ± 0.09 |
| minimum (diameter) | 275-550-1100 | 0.65 ± 0.09 |
| median (diameter) | 275-550-1100 | 0.63 ± 0.09 |
| mean (diameter) | 275-550-1100 | 0.63 ± 0.09 |
| standard deviation (diameter) | 275-550-1100 | 0.55 ± 0.09 |
| variance (diameter) | 275-550-1100 | 0.55 ± 0.10 |
| skewness (diameter) | 275-550-1100 | 0.48 ± 0.09 |
| kurtosis (diameter) | 275-550-1100 | 0.51 ± 0.10 |
| range (diameter) | 275-550-1100 | 0.51 ± 0.08 |
| mean IPA | 275-550-1100 | 0.53 ± 0.15 |
| mean LHIPA | 275-550-1100 | 0.55 ± 0.08 |
| mean IPA | 275 | 0.70 ± 0.09 |
| mean LHIPA | 275 | 0.67 ± 0.10 |
| mean slope | 275 | 0.58 ± 0.07 |
| mean slope 1 | 275 | 0.52 ± 0.11 |
| mean slope 2 | 275 | 0.52 ± 0.13 |
| mean IPA | 550 | 0.71 ± 0.14 |
| mean LHIPA | 550 | 0.67 ± 0.05 |
| mean slope | 550 | 0.57 ± 0.08 |
| mean slope 1 | 550 | 0.50 ± 0.10 |
| mean slope 2 | 550 | 0.48 ± 0.09 |
| mean IPA | 1100 | 0.66 ± 0.09 |
| mean LHIPA | 1100 | 0.65 ± 0.06 |
| mean slope | 1100 | 0.49 ± 0.09 |
| mean slope 1 | 1100 | 0.57 ± 0.10 |
| mean slope 2 | 1100 | 0.52 ± 0.12 |
References
- Singhal, T. A review of Coronavirus Disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- WHO. WHO COVID-19 Dashboard. 8 October 2025. Available online: https://data.who.int/dashboards/covid19 (accessed on 1 September 2025).
- Al-Aly, Z.; Davis, H.; McCorkell, L.; Soares, L.; Wulf-Hanson, S.; Iwasaki, A.; Topol, E.J. Long COVID science, research and policy. Nat. Med. 2024, 30, 2148–2164. [Google Scholar] [CrossRef]
- de Sire, A.; Moggio, L.; Marotta, N.; Agostini, F.; Tasselli, A.; Drago Ferrante, V.; Curci, C.; Calafiore, D.; Ferraro, F.; Bernetti, A.; et al. Impact of Rehabilitation on Fatigue in Post-COVID-19 Patients: A Systematic Review and Meta-Analysis. Appl. Sci. 2022, 12, 8593. [Google Scholar] [CrossRef]
- Chung, Y.S.; Lam, C.Y.; Tan, P.H.; Tsang, H.F.; Wong, S.C.C. Comprehensive Review of COVID-19: Epidemiology, Pathogenesis, Advancement in Diagnostic and Detection Techniques, and Post-Pandemic Treatment Strategies. Int. J. Mol. Sci. 2024, 25, 8155. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19; NICE Guideline; NICE: London, UK, 2024. [Google Scholar]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in international cohort: 7 months of symptoms and their impact. EClinical Med. 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Bundesärztekammer. Bekanntmachung “Post-COVID-Syndrom (PCS)”. Dtsch. Ärzteblatt 2022, 1–43. [Google Scholar] [CrossRef]
- WHO. Post COVID-19 Condition (Long COVID). 7 December 2022. Available online: https://www.who.int/europe/news-room/fact-sheets/item/post-COVID-19-condition (accessed on 20 June 2025).
- WHO. Post COVID-19 Condition (Long COVID). 26 February 2025. Available online: https://www.who.int/news-room/fact-sheets/detail/post-covid-19-condition-(long-covid) (accessed on 20 June 2025).
- Mehringer, W.; Stoeve, M.; Krauss, D.; Ring, M.; Steussloff, F.; Güttes, M.; Zott, J.; Hohberger, B.; Michelson, G.; Eskofier, B. Virtual reality for assessing stereopsis performance and eye characteristics in Post-COVID. Sci. Rep. 2023, 13, 13167. [Google Scholar] [CrossRef] [PubMed]
- Güttes, M.; Lucio, M.; Skornia, A.; Rühl, E.; Steußloff, F.; Zott, J.; Mardin, C.; Mehringer, W.; Ganslmayer, M.; Michelson, G.; et al. A case-control study of reaction time deficits in a 3D virtual reality in patients with Post-COVID syndrome. Sci. Rep. 2024, 14, 27204. [Google Scholar] [CrossRef]
- Schmidt, L.M.; Klingner, C.; Petersen, I.; Volkmer, A.; Schreiber, M.; Schmidt, A.; Reuken, P.; Besteher, B.; Geis, C.; Ullsperger, M.; et al. Cognitive impairment and associated neurobehavioral dysfunction in post-COVID syndrome. Psychiatry Res. 2025, 349, 116522. [Google Scholar] [CrossRef] [PubMed]
- Bitirgen, S. Abnormal quantitative pupillary light responses in patients with COVID-19. Int. Ophthalmol. 2022, 42, 2847–2854. [Google Scholar] [CrossRef]
- Yurttaser Ocak, S.; Ozturan, S.G.; Bas, E. Pupil responses in patients with COVID-19. Int. Ophthalmol. 2022, 42, 385–391. [Google Scholar] [CrossRef] [PubMed]
- García Cena, C.; Costa, M.C.; Saltarén Pazmiño, R.; Santos, C.P.; Gómez-Andrés, D.; Benito-León, J. Eye movement alterations in Post-COVID-19 condition: A proof-of-concept study. Sensors 2022, 22, 1481. [Google Scholar] [CrossRef] [PubMed]
- Michelson, G. Europäische Patentanmeldung. Europe Patent EP 3 287 074 A1, 28 February 2018. [Google Scholar]
- Duchowski, A.T.; Krejtz, K.; Gehrer, N.A.; Bafna, T.; Bækgaard, P. The low/high index of pupillary activity. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020. [Google Scholar]
- Duchowski, A.T.; Krejtz, K.; Krejtz, I.; Biele, C.; Niedzielska, A.; Kiefer, P.; Raubal, M.; Giannopoulos, I. The index of pupillary activity: Measuring cognitive load vis-á-vis task difficulty with pupil oscillation. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, Montreal, QC, Canada, 21–26 April 2018. [Google Scholar]
- Baltaci, S.; Gokcay, D. Stress detection in human-computer detection: Fusion of pupillary activity and facial temperature features. Int. J. Hum. Comput. Interact. 2016, 32, 956–966. [Google Scholar] [CrossRef]
- Duchowski, A.T.; Medlin, E.; Cournia, N.; Gramopadhye, A.; Melloy, B.; Nair, S. 3D eye movement analysis for VR visual inspection training. In Proceedings of the 2002 Symposium on Eye Tracking Research & Applications, New Orleans, LA, USA, 25–27 March 2002. [Google Scholar]
- Ladek, A.M.; Lucio, M.; Weiß, A.; Knauer, T.; Sarmiento, H.; Ilgner, M.; Jakobi, M.; Barteczko, L.; Ganslmayer, M.; Rech, J.; et al. Deoxygenation Trends and Their Multivariate Association with Self-Reported Fatigue in Post-COVID Syndrome. Biomedicines 2025, 13, 1371. [Google Scholar] [CrossRef]
- Mendonca Filho, V.C.M.; de Oliveira, A.G.; Maia, I.D.F.V.C.; de Falcone, A.C.M.; Betini, B.G.; Rezende, L.B.; Alves, F.H.M. COVID-19 in the nervous system: Physiopathology and neurological manifestations. Arq. Neuro-Psiquiatr. 2023, 81, 756–763. [Google Scholar] [CrossRef]
- Voruz, P.; Allali, G.; Benzakour, L.; Nuber-Champier, A.; Thomasson, M.; Jacot de Alcântara, I.; Pierce, J.; Lalive, P.H.; Lövblad, K.O.; Braillard, O.; et al. Long COVID neuropsychological deficits after severe, moderate, or mild infection. Clin. Transl. Neurosci. 2022, 6, 9. [Google Scholar] [CrossRef]
- Wu, Y.; Xu, X.; Chen, Z.; Duan, J.; Hashimoto, K.; Yang, L.; Liu, C.; Yang, C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020, 97, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Wennmo, C.; Hindfelt, B. Eye movements in brainstem lesions. Acta Oto-Laryngol. 1980, 90, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Kara, D.D.; Ring, M.; Hennig, F.F.; Michelson, G. Effects of mild traumatic brain injury on stereopsis detected by a virtual reality system: Attempt to develop a screening test. J. Med. Biol. Eng. 2020, 40, 639–647. [Google Scholar] [CrossRef]
- Duan, X.; Huang, Z.; Zhang, S.; Zhu, G.; Wang, R.; Wang, Z. Duan. SARS-CoV-2 infection impairs oculomotor functions: A longitudinal eye-tracking study. J. Eye Mov. Res. 2024, 17, 10–16910. [Google Scholar] [CrossRef] [PubMed]
- Vinuela-Navarro, V.; Goset, J.; Aldaba, M.; Mestre, C.; Rovira-Gay, C.; Cano, N.; Ariza, M.; Delàs, B.; Garolera, M.; Vilaseca, M. Eye movements in patients with post-COVID condition. Biomed. Opt. Express 2023, 14, 3936–3949. [Google Scholar] [CrossRef] [PubMed]
- Carbone, F.; Zamarian, L.; Rass, V.; Bair, S.; Ritter, M.; Beer, R.; Mahlknecht, P.; Heim, B.; Limmert, V.; Peball, M.; et al. Cognitive dysfunction 1 year after COVID-19: Evidence from eye tracking. Ann. Clin. Transl. Neurol. 2022, 9, 1826–1831. [Google Scholar] [CrossRef]
- Maiorana, N.V.; Aiello, E.N.; Poletti, B.; Carusi, F.; De Sandi, A.; Guidetti, M.; Prandin, R.; Marceglia, S.; Ticozzi, N.; Silani, V.; et al. Relationship between Reaction Times and Post-COVID-19. Healthcare 2023, 11, 284. [Google Scholar] [CrossRef] [PubMed]
- Santoyo-Mora, M.; Villaseñor-Mora, C.; Cardona-Torres, L.M.; Martínez-Nolasco, J.J.; Barranco-Gutiérrez, A.I.; Padilla-Medina, J.A.; Bravo-Sánchez, M.G. COVID-19 Long-Term Effects: Is There an Impact on the Simple Reaction Time and Alternative-Forced Choice on Recovered Patients? Brain Sci. 2022, 12, 1258. [Google Scholar] [CrossRef]
- Martinez-Cedillo, A.P.; Gavrila, N.; Mishra, A.; Geangu, E.; Foulsham, T. Cognitive load affects gaze dynamics during real-world tasks. Exp. Brain Res. 2025, 243, 82. [Google Scholar] [CrossRef] [PubMed]
- Çorbacıoğlu, Ş.K.; Aksel, G. Receiver operating characteristic curve analysis in diagnostic accuracy studies: A guide to interpreting the area under the curve value. Turk. J. Emerg. Med. 2023, 23, 195–198. [Google Scholar] [CrossRef]
- Opwonya, J.; Kim, K.; Lee, K.H.; Kim, J.I.; Kim, J.U. Task-evoked pupillary responses as potential biomarkers of mild cognitive impairment. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2024, 16, e70019. [Google Scholar] [CrossRef]
- El Haj, M.; Chapelet, G.; Moustafa, A.A.; Boutoleau-Bretonnière, C. Pupil size as an indicator of cognitive activity in mild Alzheimer’s disease. EXCLI J. 2022, 21, 307. [Google Scholar]
- Proal, A.D.; VanElzakker, M.B.; Aleman, S.; Bach, K.; Boribong, B.P.; Buggert, M.; Cherry, S.; Chertow, D.S.; Davies, H.E.; Dupont, C.L.; et al. SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC). Nat. Immunol. 2023, 24, 1616–1627. [Google Scholar] [CrossRef] [PubMed]
- Kell, D.B.; Laubscher, G.J.; Pretorius, E. A central role for amyloid fibrin microclots in long COVID/PASC: Origins and therapeutic implications. Biochem. J. 2022, 479, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Wallukat, G.; Hohberger, B.; Wenzel, K.; Fürst, J.; Schulze-Rothe, S.; Wallukat, A.; Hönicke, A.S.; Müller, J. Functional autoantibodies against G-protein coupled receptors in patients with persistent Long-COVID-19 symptoms. J. Transl. Autoimmun. 2021, 4, 100100. [Google Scholar] [CrossRef]
| PCS (n = 330) | Control (n = 99) | |
|---|---|---|
| Sex (male/female) | 137 (41.5%)/193 (58.5%) | 50 (50.5%)/49 (49.5%) |
| Age | 40.9 (±11.9) | 35.7 (±14.5) |
| Parameter Group | Mean AUROC ± Standard Deviation |
|---|---|
| pupil diameter | 0.73 ± 0.09 |
| gaze direction | 0.68 ± 0.07 |
| stereopsis performance | 0.66 ± 0.09 |
| all extracted VR-OTS | 0.71 ± 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knauer, T.S.; Mardin, C.Y.; Rech, J.; Michelson, G.; Stog, A.; Zott, J.; Steußloff, F.; Güttes, M.; Sarmiento, H.; Ilgner, M.; et al. Evaluation of Stereopsis Performance, Gaze Direction and Pupil Diameter in Post-COVID Syndrome Using Machine Learning. Biomedicines 2025, 13, 2828. https://doi.org/10.3390/biomedicines13112828
Knauer TS, Mardin CY, Rech J, Michelson G, Stog A, Zott J, Steußloff F, Güttes M, Sarmiento H, Ilgner M, et al. Evaluation of Stereopsis Performance, Gaze Direction and Pupil Diameter in Post-COVID Syndrome Using Machine Learning. Biomedicines. 2025; 13(11):2828. https://doi.org/10.3390/biomedicines13112828
Chicago/Turabian StyleKnauer, Thomas S., Christian Y. Mardin, Jürgen Rech, Georg Michelson, Andreas Stog, Julia Zott, Fritz Steußloff, Moritz Güttes, Helena Sarmiento, Miriam Ilgner, and et al. 2025. "Evaluation of Stereopsis Performance, Gaze Direction and Pupil Diameter in Post-COVID Syndrome Using Machine Learning" Biomedicines 13, no. 11: 2828. https://doi.org/10.3390/biomedicines13112828
APA StyleKnauer, T. S., Mardin, C. Y., Rech, J., Michelson, G., Stog, A., Zott, J., Steußloff, F., Güttes, M., Sarmiento, H., Ilgner, M., Jakobi, M., Hohberger, B., & Schottenhamml, J. (2025). Evaluation of Stereopsis Performance, Gaze Direction and Pupil Diameter in Post-COVID Syndrome Using Machine Learning. Biomedicines, 13(11), 2828. https://doi.org/10.3390/biomedicines13112828








