SGLT2 Inhibitors Are Associated with Left Ventricular Reverse Remodeling in Patients with Non-Compaction Cardiomyopathy—A Prospective Observational Cohort Trial
Abstract
1. Introduction
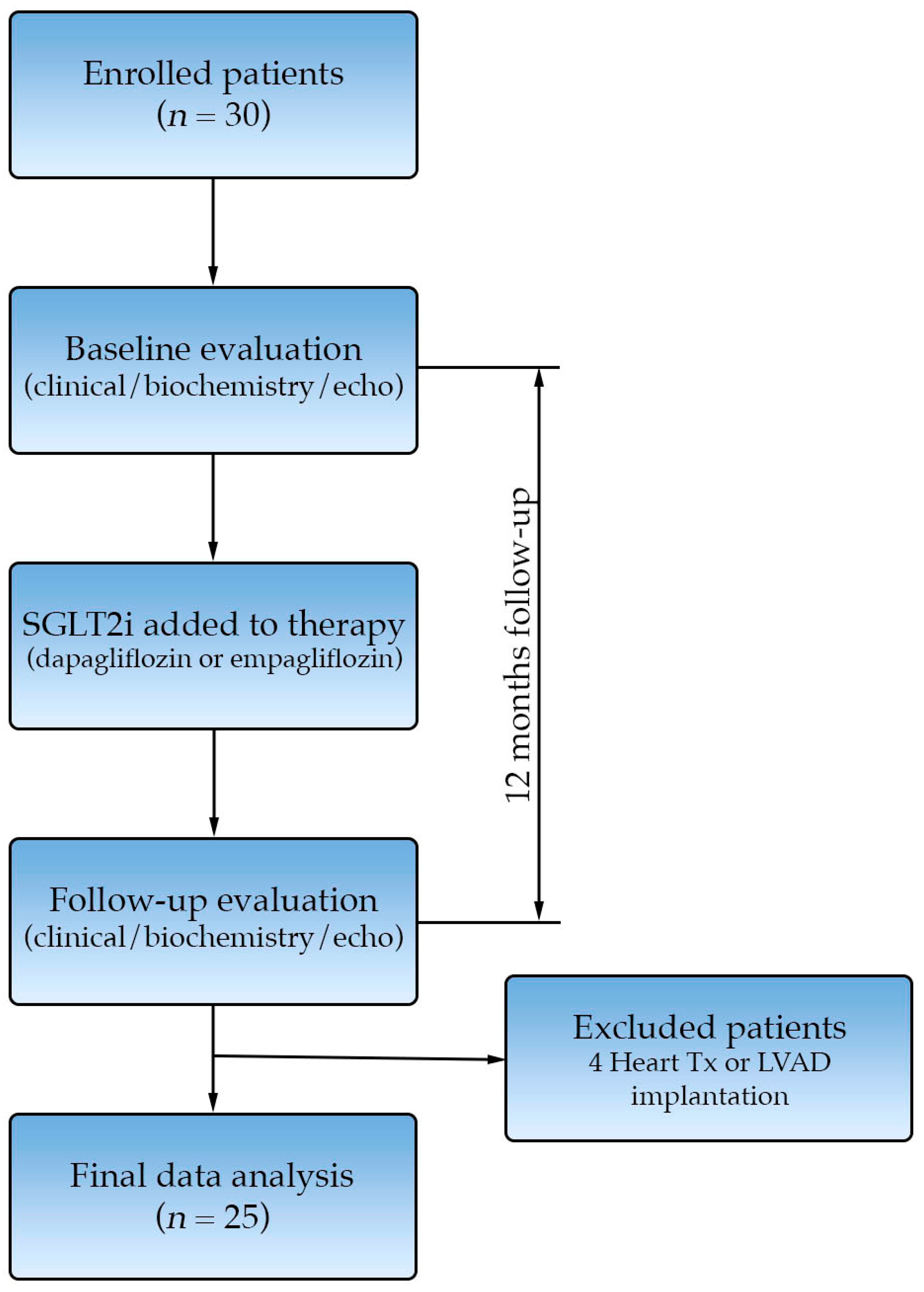
2. Methods
2.1. Patient Population
2.2. Patient and Public Involvement
2.3. Study Design
2.4. Echocardiography
2.5. NT-proBNP Measurements
2.6. Statistical Methods
3. Results
3.1. Patient Characteristics
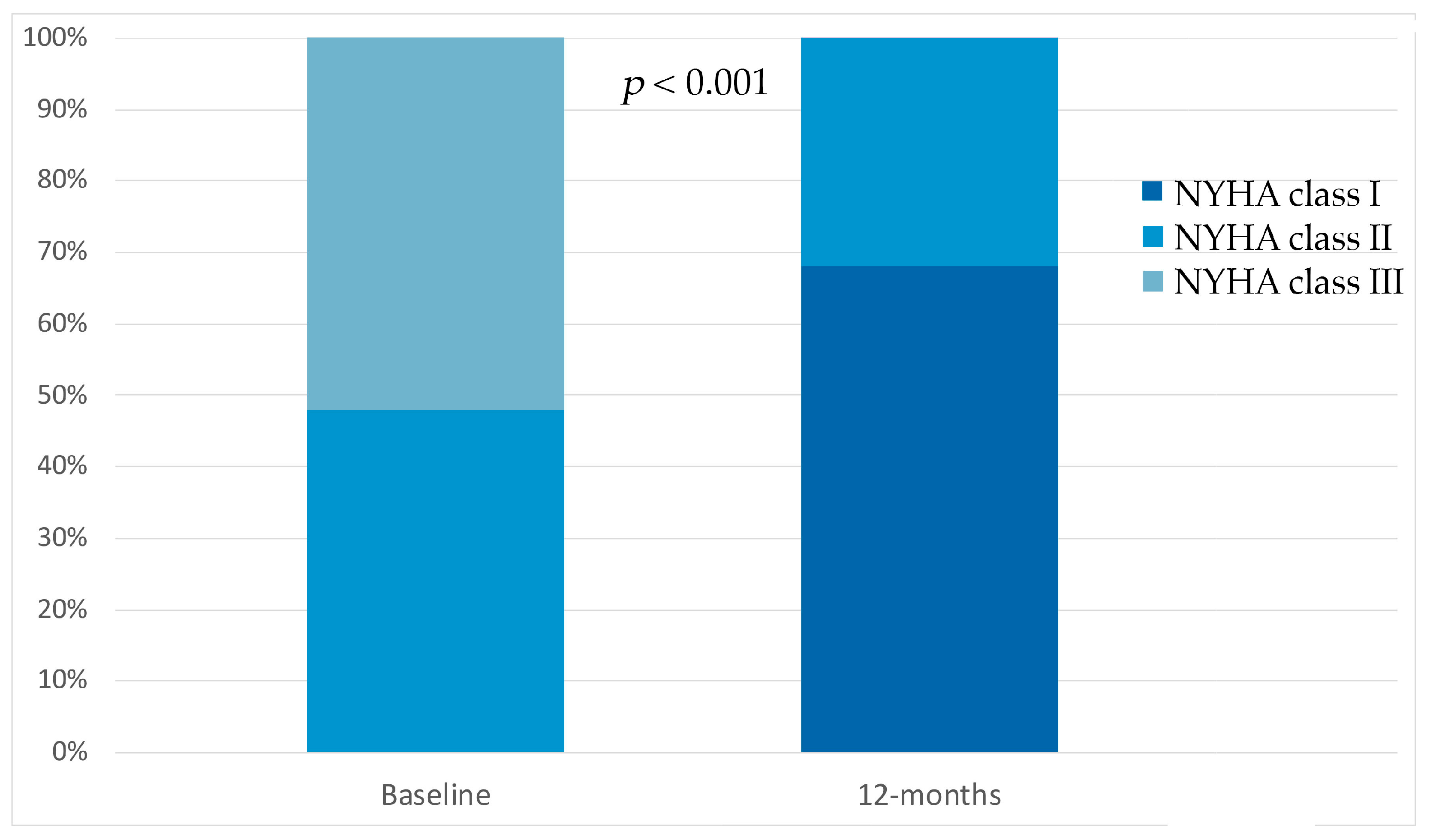
3.2. Effect of SGLT2i on NYHA Class
3.3. Effects of SGLT2i on Reverse Remodeling and Neurohormonal Modulation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ritter, M.; Oechslin, E.; Sütsch, G.; Attenhofer, C.; Schneider, J.; Jenni, R. Isolated Noncompaction of the Myocardium in Adults. Mayo Clin. Proc. 1997, 72, 26–31. [Google Scholar] [CrossRef]
- Towbin, J.A.; Lorts, A.; Jefferies, J.L. Left Ventricular Non-Compaction Cardiomyopathy. Lancet 2015, 386, 813–825. [Google Scholar] [CrossRef]
- van Waning, J.I.; Caliskan, K.; Hoedemaekers, Y.M.; van Spaendonck-Zwarts, K.Y.; Baas, A.F.; Boekholdt, S.M.; Van Melle, J.P.; Teske, A.J.; Asselbergs, F.W.; Backx, P.C.M.; et al. Genetics, Clinical Features, and Long-Term Outcome of Noncompaction Cardiomyopathy. J. Am. Coll. Cardiol. 2018, 71, 711–722. [Google Scholar] [CrossRef] [PubMed]
- Oechslin, E.; Jenni, R. Left Ventricular Noncompaction: From Physiologic Remodeling to Noncompaction Cardiomyopathy. J. Am. Coll. Cardiol. 2018, 71, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Jenni, R.; Oechslin, E.; Schneider, J.; Attenhofer Jost, C.; Kaufmann, P.A. Echocardiographic and Pathoanatomical Characteristics of Isolated Left Ventricular Non-Compaction: A Step towards Classification as a Distinct Cardiomyopathy. Heart 2001, 86, 666–671. [Google Scholar] [CrossRef]
- Petersen, S.E.; Selvanayagam, J.B.; Wiesmann, F.; Robson, M.D.; Francis, J.M.; Anderson, R.H.; Watkins, H.; Neubauer, S. Left Ventricular Non-Compaction: Insights from Cardiovascular Magnetic Resonance Imaging. J. Am. Coll. Cardiol. 2005, 46, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Arbelo, E.; Protonotarios, A.; Gimeno, J.R.; Arbustini, E.; Barriales-Villa, R.; Basso, C.; Bezzina, C.R.; Biagini, E.; Blom, N.A.; de Boer, R.A.; et al. 2023 ESC Guidelines for the Management of Cardiomyopathies. Eur. Heart J. 2023, 44, 3503–3526. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. Circulation 2022, 145, e895–e1032, Erratum in Circulation 2023, 147, e674. https://doi.org/10.1161/CIR.0000000000001142. [Google Scholar] [CrossRef]
- Stöllberger, C.; Finsterer, J.; Blazek, G. Left Ventricular Hypertrabeculation/Noncompaction and Association with Additional Cardiac Abnormalities and Neuromuscular Disorders. Am. J. Cardiol. 2002, 90, 899–902. [Google Scholar] [CrossRef]
- Ichida, F.; Hamamichi, Y.; Miyawaki, T.; Ono, Y.; Kamiya, T.; Akagi, T.; Hamada, H.; Hirose, O.; Isobe, T.; Yamada, K.; et al. Clinical Features of Isolated Noncompaction of the Ventricular Myocardium. J. Am. Coll. Cardiol. 1999, 34, 233–240. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 4901–4989. [Google Scholar] [CrossRef]
- Bustea, C.; Bungau, A.F.; Tit, D.M.; Iovanovici, D.C.; Toma, M.M.; Bungau, S.G.; Radu, A.-F.; Behl, T.; Cote, A.; Babes, E.E. The Rare Condition of Left Ventricular Non-Compaction and Reverse Remodeling. Life 2023, 13, 1318. [Google Scholar] [CrossRef]
- Cerar, A.; Kšela, J.; Poglajen, G.; Vrtovec, B.; Kneževič, I. LVAD as a Bridge to Heart Transplantation in a Patient with Left Ventricular Noncompaction Cardiomyopathy and Advanced Heart Failure. Heart Surg. Forum 2016, 19, E128–E130. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.W.; Yuan, J.; Xing, J.F.; Fan, M. Sacubitril-Valsartan Therapy in a Patient with Heart Failure Due to Isolated Left Ventricular Noncompaction: A Case Report and Literature Review. Cardiol. Plus 2022, 7, 56–59, Erratum in Cardiol. Plus 2022, 7, 148–149. [Google Scholar] [CrossRef]
- Bonatto, M.G.; Albanez, R.; Salemi, V.M.C.; Moura, L.Z. Use of Sacubitril/Valsartan in Non-Compaction Cardiomyopathy: A Case Report. ESC Heart Fail. 2020, 7, 1186–1189. [Google Scholar] [CrossRef] [PubMed]
- Kramer, D.G.; Trikalinos, T.A.; Kent, D.M.; Antonopoulos, G.V.; Konstam, M.A.; Udelson, J.E. Quantitative Evaluation of Drug or Device Effects on Ventricular Remodeling as Predictors of Therapeutic Effects on Mortality in Patients with Heart Failure and Reduced Ejection Fraction. J. Am. Coll. Cardiol. 2010, 56, 392–406. [Google Scholar] [CrossRef]
- Li, J.; Franke, J.; Pribe-Wolferts, R.; Meder, B.; Ehlermann, P.; Mereles, D.; Andre, F.; Abdelrazek, M.A.; Merten, C.; Schweizer, P.A.; et al. Effects of β-Blocker Therapy on Electrocardiographic and Echocardiographic Characteristics of Left Ventricular Noncompaction. Clin. Res. Cardiol. 2015, 104, 241–249. [Google Scholar] [CrossRef]
- Carluccio, E.; Biagioli, P.; Reboldi, G.; Mengoni, A.; Lauciello, R.; Zuchi, C.; D’aDdario, S.; Bardelli, G.; Ambrosio, G. Left Ventricular Remodeling Response to SGLT2 Inhibitors in Heart Failure: An Updated Meta-Analysis of Randomized Controlled Studies. Cardiovasc. Diabetol. 2023, 22, 235. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- Dhingra, N.K.; Mistry, N.; Puar, P.; Verma, R.; Anker, S.; Mazer, C.D.; Verma, S. SGLT2 Inhibitors and Cardiac Remodelling: A Systematic Review and Meta-Analysis of Randomized Cardiac Magnetic Resonance Imaging Trials. ESC Heart Fail. 2021, 8, 4693–4700. [Google Scholar] [CrossRef] [PubMed]
- Theofilis, P.; Sagris, M.; Oikonomou, E.; Antonopoulos, A.S.; Siasos, G.; Tsioufis, K.; Tousoulis, D. Pleiotropic effects of SGLT2 inhibitors and heart failure outcomes. Diabetes Res. Clin. Pract. 2022, 188, 109927. [Google Scholar] [CrossRef]
- Matteucci, A.; Pandozi, C.; Bonanni, M.; Mariani, M.V.; Sgarra, L.; Nesti, L.; Pierucci, N.; La Fazia, V.M.; Lavalle, C.; Nardi, F.; et al. Impact of empagliflozin and dapagliflozin on sudden cardiac death: A systematic review and meta-analysis of adjudicated randomized evidence. Heart Rhythm 2025, in press. [Google Scholar] [CrossRef]
- Alcidi, G.; Pugliese, R.; Ioannoni, S.; Romano, M.; Palmieri, G.; Tabella, E.; Correale, M.; Di Biase, M.; Brunetti, N.D.; Iacoviello, M. Improvement in Left and Right Ventricular Function after Introduction of SGLT2 Inhibitors in Heart Failure Outpatients with Reduced Ejection Fraction. Clin. Pract. 2023, 13, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Jiang, C.; Guo, M.; Zeng, Y.; Jiang, Z.; Zhang, D.; Tu, M.; Tan, X.; Yan, P.; Xu, X.; et al. Effects of SGLT2 Inhibitors on Cardiac Function and Health Status in Chronic Heart Failure: A Systematic Review and Meta-Analysis. Cardiovasc. Diabetol. 2024, 23, 2. [Google Scholar] [CrossRef]

| All | Group A (n = 18) | Group B (n = 7) | p | |
|---|---|---|---|---|
| Age (years) | 49 ± 16 | 50 ± 15 | 46 ± 15 | 0.282 |
| Male gender | 17 (68%) | 12 (67%) | 5 (71%) | 0.538 |
| NYHA class | ||||
| II | 12 (48%) | 9 (50%) | 3 (43%) | 0.645 |
| III | 13 (52%) | 9 (50%) | 4 (67%) | |
| Medical history | ||||
| Arterial hypertension | 2 (8%) | 2 (11%) | 0 | 0.352 |
| Diabetes | 0 | 0 | 0 | / |
| Atrial fibrillation | 6 (24%) | 2 (11%) | 4 (57%) | 0.135 |
| ICD | 12 (48%) | 6 (33%) | 6 (86%) | 0.097 |
| CRT | 5 (20%) | 3 (17%) | 2 (29%) | 0.696 |
| Laboratory values | ||||
| Sodium (mmol/L) | 139 ± 2.7 | 140.6 ± 2.6 | 138.2 ± 2.0 | 0.011 |
| Potassium (mmol/L) | 4.4 ± 0.5 | 4.5 ± 0.5 | 4.3 ± 0.4 | 0.352 |
| Creatinine (μmol/L) | 86 ± 25 | 83 ± 27 | 89 ± 21 | 0.527 |
| Bilirubine (μmol/L) | 19 ± 14 | 21 ± 15 | 17 ± 12 | 0.558 |
| γGT (μkat/L) | 1.0 ± 0.8 | 0.7 ± 0.5 | 1.4 ± 1.1 | 0.017 |
| AST (μkat/L) | 0.7 ± 0.7 | 0.5 ± 0.4 | 0.9 ± 0.9 | 0.208 |
| ALT (μkat/L) | 0.9 ± 1.1 | 0.5 ± 0.3 | 1.4 ± 1.7 | 0.052 |
| hs-TnI (pg/mL) | 13.8 ± 11.7 | 11.4 ± 5.7 | 19.9 ± 20.0 | 0.31 |
| NT-proBNP (pg/mL) | 2026 ± 2198 | 1720 ± 1661 | 4527 ± 4369 | 0.020 |
| Medical therapy | ||||
| ACEI/ARB | 1 (4%) | 0 | 1 (14%) | / |
| ramipril 1.25 mg qid | 1 (4%) | 0 | 1 (14%) | / |
| ARNI | 24 (96%) | 18 (100%) | 6 (86%) | / |
| sac/val 24/26 mg bid | 2 (8%) | 0 | 2 (29%) | / |
| sac/val 49/51 mg bid | 11 (44%) | 9 (50%) | 2 (29%) | / |
| sac/val 103/97 mg bid | 11 (44%) | 9 (50%) | 2 (29%) | / |
| Beta blockers | 25 (100%) | 18 (100%) | 7 (100%) | / |
| bisoprolol 2.5 mg qid | 5 (20%) | 3 (17%) | 2 (29%) | / |
| bisoprolol 5 mg qid | 12 (48%) | 8 (44%) | 4 (57%) | / |
| bisoprolol 10 mg qid | 5 (20%) | 5 (28%) | 0 | / |
| carvedilol 6.25 mg bid | 1 (4%) | 1 (6%) | 0 | / |
| carvedilol 12.5 mg bid | 1 (4%) | 0 | 1 (14%) | / |
| carvedilol 25 mg bid | 1 (4%) | 1 (6%) | 0 | / |
| MRA | 25 (100%) | 18 (100%) | 7 (100%) | / |
| spironolactone 25 mg qid | 16 (64%) | 11 (61%) | 5 (71%) | / |
| eplerenone 25 mg qid | 9 (36%) | 7 (39%) | 2 (29%) | / |
| Aspirin | 7 (28%) | 6 (33%) | 1 (14%) | 0.336 |
| Warfarin | 9 (36%) | 5 (28%) | 4(57%) | 0.169 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerar, A.; Poglajen, G.; Zemljič, G.; Frljak, S.; Žorž, N.; Jaklič, M.; Okrajšek, R.; Šebeštjen, M.; Vrtovec, B. SGLT2 Inhibitors Are Associated with Left Ventricular Reverse Remodeling in Patients with Non-Compaction Cardiomyopathy—A Prospective Observational Cohort Trial. Biomedicines 2025, 13, 2773. https://doi.org/10.3390/biomedicines13112773
Cerar A, Poglajen G, Zemljič G, Frljak S, Žorž N, Jaklič M, Okrajšek R, Šebeštjen M, Vrtovec B. SGLT2 Inhibitors Are Associated with Left Ventricular Reverse Remodeling in Patients with Non-Compaction Cardiomyopathy—A Prospective Observational Cohort Trial. Biomedicines. 2025; 13(11):2773. https://doi.org/10.3390/biomedicines13112773
Chicago/Turabian StyleCerar, Andraž, Gregor Poglajen, Gregor Zemljič, Sabina Frljak, Neža Žorž, Martina Jaklič, Renata Okrajšek, Miran Šebeštjen, and Bojan Vrtovec. 2025. "SGLT2 Inhibitors Are Associated with Left Ventricular Reverse Remodeling in Patients with Non-Compaction Cardiomyopathy—A Prospective Observational Cohort Trial" Biomedicines 13, no. 11: 2773. https://doi.org/10.3390/biomedicines13112773
APA StyleCerar, A., Poglajen, G., Zemljič, G., Frljak, S., Žorž, N., Jaklič, M., Okrajšek, R., Šebeštjen, M., & Vrtovec, B. (2025). SGLT2 Inhibitors Are Associated with Left Ventricular Reverse Remodeling in Patients with Non-Compaction Cardiomyopathy—A Prospective Observational Cohort Trial. Biomedicines, 13(11), 2773. https://doi.org/10.3390/biomedicines13112773







