Mortality-Associated Factors in a Traumatic Brain Injury Population in Mexico
Abstract
1. Introduction
2. Materials and Methods
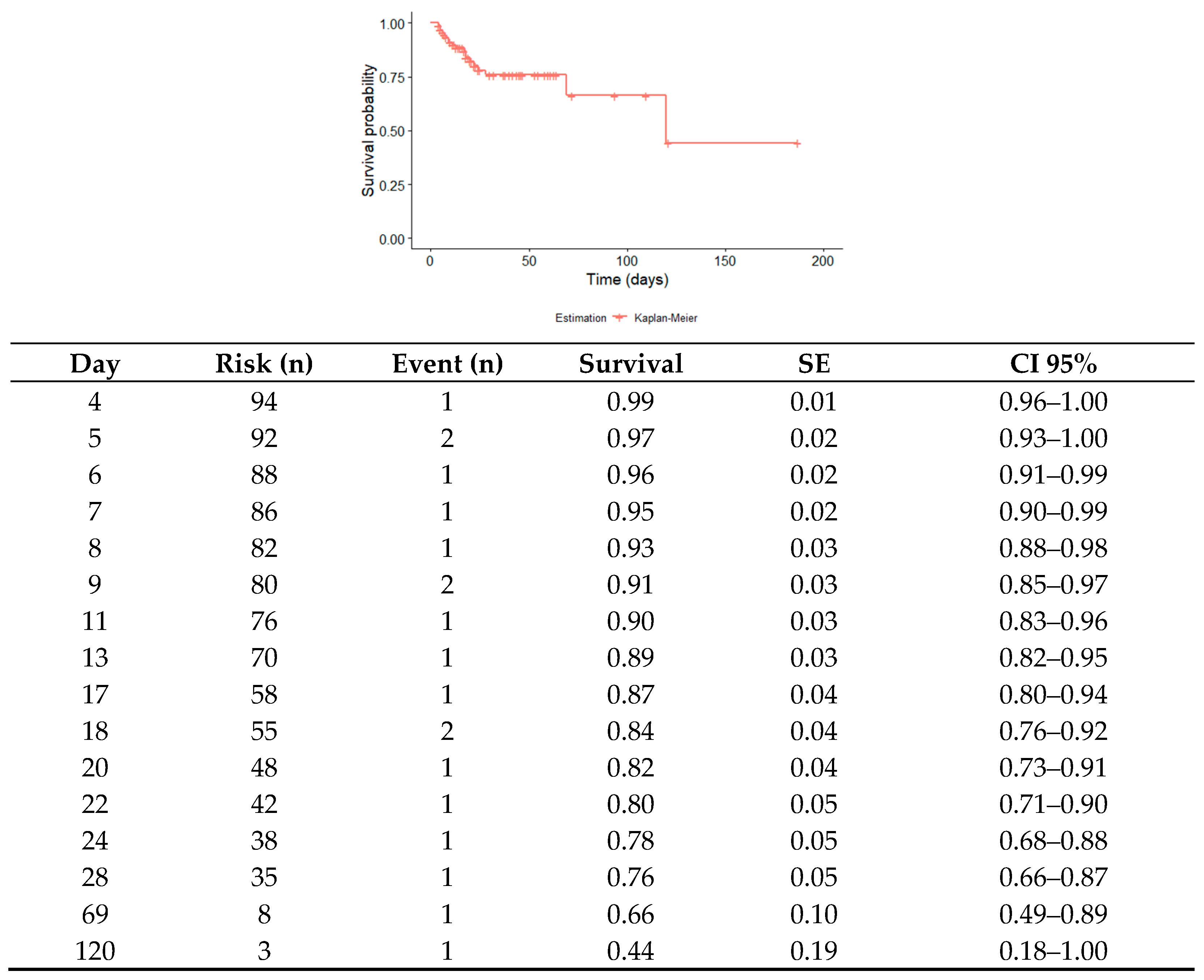
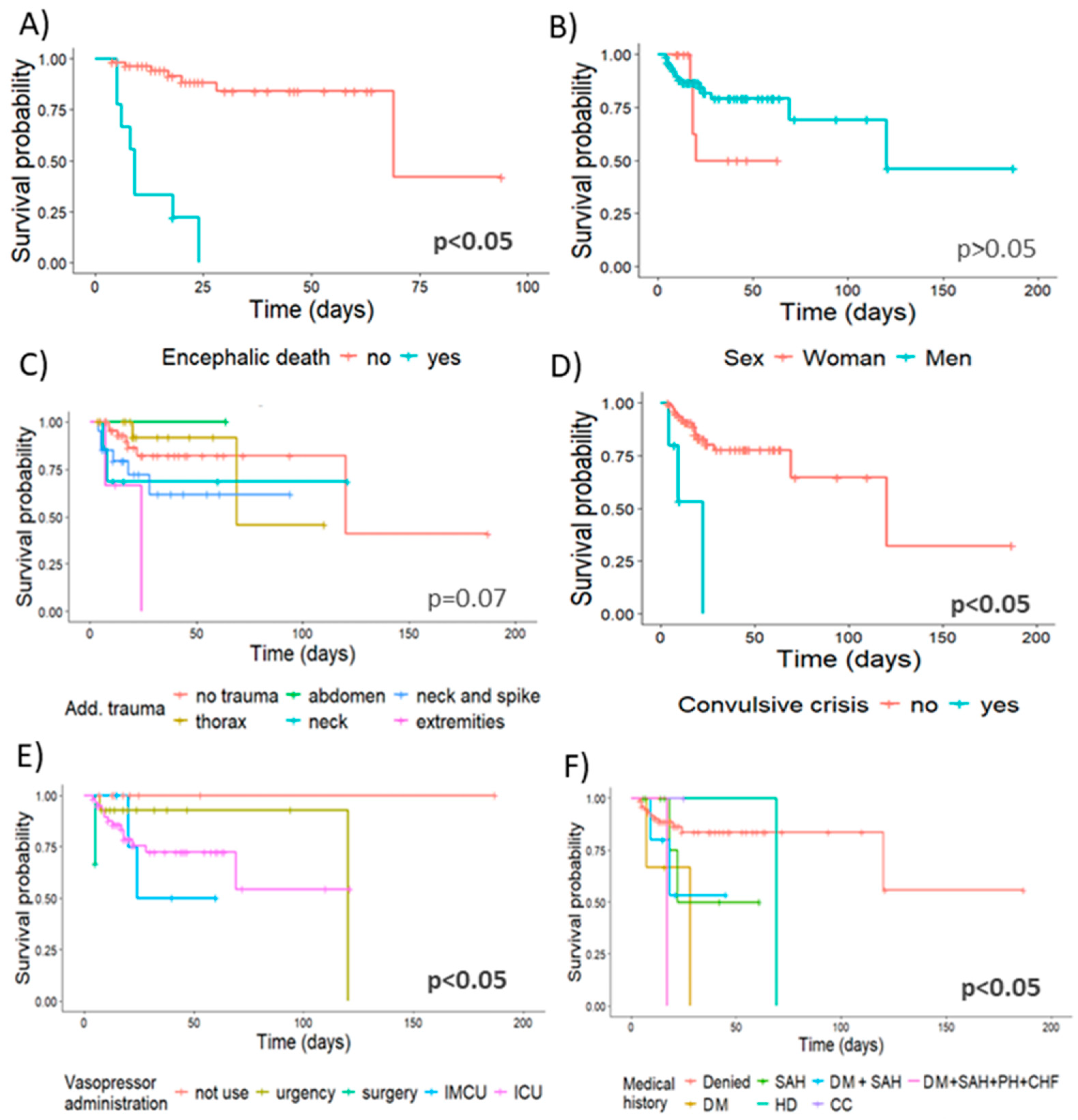
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hassett, L. Physiotherapy management of moderate-to-severe traumatic brain injury. J. Physiother. 2023, 69, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Menon, D.K.; Schwab, K.; Wright, D.W.; Maas, A.I. Position Statement: Definition of Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2010, 91, 1637–1640. [Google Scholar] [CrossRef] [PubMed]
- Pozzato, I.; Tate, R.L.; Rosenkoetter, U.; Cameron, I.D. Epidemiology of hospitalised traumatic brain injury in the state of New South Wales, Australia: A population-based study. Aust. N. Z. J. Public Health 2019, 43, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Soto-Páramo, D.G.; Pérez-Nieto, O.R.; Deloya-Tomás, E.; Rayo-Rodríguez, S.; Castillo-Gutiérrez, G.; Olvera-Ramos, M.G.; Carrión-Moya, J.; López-Fermín, J.; Zamarrón-López, E.I.; Guerrero-Gutiérrez, M.A.; et al. Pathophysiology, diagnosis and treatment of traumatic brain injury. Neurol. Neurocir. Psiquiatr. 2022, 50, 4–15. [Google Scholar]
- TCE—Traumatismo Craneoencefálico—RELACSIS. Available online: https://www3.paho.org/relacsis/index.php/es/foros-relacsis/foro-becker-fci-oms/61-foros/consultas-becker/938-tce-traumatismo-craneoencefalico/ (accessed on 26 August 2023).
- Nguyen, R.; Fiest, K.M.; McChesney, J.; Kwon, C.S.; Jette, N.; Frolkis, A.D.; Atta, C.; Mah, S.; Dhaliwal, H.; Reid, A.; et al. The international incidence of traumatic brain injury: A systematic review and meta-analysis. Can. J. Neurol. Sci. 2016, 43, 774–785. [Google Scholar] [CrossRef]
- World Health Organization. Traumatismos y Violencia: Datos. Organización Mundial de la Salud. 2010. Available online: https://iris.who.int/handle/10665/44335 (accessed on 26 August 2023).
- Instituto Nacional de Estadística y Geografía. Comunicado de Prensa. Estadística de Defunciones Registradas de Enero a Junio de 2022 (Preliminar). 2023. Available online: https://www.inegi.org.mx/contenidos/saladeprensa/boletines/2023/EDR/EDR2022.pdf (accessed on 26 August 2023).
- Alberdi, F.; García, I.; Atutxa, L.; Zabarte, M. Epidemiology of severe trauma. Med. Intensiv. 2014, 38, 580–588. [Google Scholar] [CrossRef]
- Gordillo-Escobar, E.; Egea-Guerrero, J.J.; Rodríguez-Rodríguez, A.; Murillo-Cabezas, F. Utilidad de los biomarcadores en el pronóstico del traumatismo craneoencefálico grave. Med. Intensiv. 2016, 40, 105–112. [Google Scholar] [CrossRef]
- Soler, M.C.; León, P.D.; Larrondo, M.H.; Agustín, G.D. Respuesta bioquímica y molecular ante el daño cerebral agudo. Rev. Cuba. Med. 2014, 53, 76–90. [Google Scholar]
- Ortiz-Prado, E.; León, A.B.; Unigarro, L.; Santillan, P. Oxigenación y Flujo Sanguíneo Cerebral, Revisión Comprensiva de la Literatura. Rev. Ecuat. Neurol. 2018, 27, 80–89. [Google Scholar]
- Rodríguez-Boto, G.; Rivero-Garvía, M.; Gutiérrez-González, R.; Márquez-Rivas, J. Conceptos básicos sobre la fisiopatología cerebral y la monitorización de la presión intracraneal. Neurología 2015, 30, 16–22. [Google Scholar] [CrossRef]
- Cabrera, R.A.; Martínez, O.O.; Ibarra, G.A.; Morales, S.R.; Laguna, H.G.; Sánchez, P.H. Traumatismo craneoencefálico severo. Rev. Asoc. Mex. Med. Crit. Ter. Int. 2009, 24, 94–101. [Google Scholar]
- Werner, C.; Engelhard, K. Pathophysiology of traumatic brain injury. Br. J. Anaesth. 2007, 99, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Velásquez, H.A.; Cáñamo-Villafañe, P.A.; Fontalvo-Mendoza, M.F.; Florez Perdomo, W.A. Autorregulación cerebral: Fisiología y fisiopatología esenciales para el manejo neurocrítico. Rev. Arg. Med. 2020, 8, 305–310. [Google Scholar]
- McCredie, V.A.; Chavarría, J.; Baker, A.J. How do we identify the crashing traumatic brain injury patient—The intensivist’s view. Curr. Opin. Crit. Care 2021, 27, 320–327. [Google Scholar] [CrossRef]
- Meyfroidt, G.; Bouzat, P.; Casaer, M.P.; Chesnut, R.; Hamada, S.R.; Helbok, R.; Hutchinson, P.; Maas, A.I.; Manley, G.; Menon, D.K. Management of moderate to severe traumatic brain injury: An update for the intensivist. Intensive Care Med. 2022, 40, 649–666. [Google Scholar] [CrossRef]
- Hawryluk, G.W.; Aguilera, S.; Buki, A.; Bulger, E.; Citerio, G.; Cooper, D.J.; Arrastia, R.D.; Diringer, M.; Figaji, A.; Gao, G.; et al. A management algorithm for patients with intracranial pressure monitoring: The Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019, 45, 1783–1794. [Google Scholar] [CrossRef]
- Dreier, J.P.; Fabricius, M.; Ayata, C.; Sakowitz, O.W.; William Shuttleworth, C.; Dohmen, C.; Graf, R.; Vajkoczy, P.; Helbok, R.; Suzuki, M.; et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: Review and recommendations of the COSBID research group. J. Cereb. Blood Flow. Metab. 2017, 37, 1595–1625. [Google Scholar] [CrossRef]
- Capizzi, A.; Woo, J.; Verduzco-Gutierrez, M. Traumatic Brain Injury: An Overview of Epidemiology, Pathophysiology, and Medical Management. Med. Clin. N. Am. 2020, 104, 213–238. [Google Scholar] [CrossRef] [PubMed]
- Mauritz, W.; Brazinova, A.; Majdan, M.; Leitgeb, J. Epidemiology of traumatic brain injury in Austria. Wien. Klin. Wochenschr. 2014, 126, 42–52. [Google Scholar] [CrossRef]
- Brazinova, A.; Rehorcikova, V.; Taylor, M.S.; Buckova, V.; Majdan, M.; Psota, M.; Peeters, W.; Feigin, V.; Theadom, A.; Holkovic, L. Epidemiology of Traumatic Brain Injury in Europe: A Living Systematic Review. J. Neurotrauma 2021, 38, 1411–1440. [Google Scholar] [CrossRef]
- Wu, X.; Hu, J.; Zhuo, L.; Fu, C.; Hui, G.; Wang, Y.; Yang, W.; Teng, L.; Lu, S.; Xu, G. Epidemiology of traumatic brain injury in eastern China, 2004: A prospective large case study. J. Trauma 2008, 64, 1313–1319. [Google Scholar] [CrossRef] [PubMed]
- Giner, J.; Galán, L.M.; Teruel, S.Y.; Espallargas, M.G.; López, C.P.; Guerrero, A.I.; Frade, J.R. Traumatic brain injury in the new millennium: New population and new management. Neurología 2022, 37, 383–389. [Google Scholar] [CrossRef]
- Styrke, J.; Stålnacke, B.M.; Sojka, P.; Björnstig, U. Traumatic brain injuries in a well-defined population: Epidemiological aspects and severity. J. Neurotrauma 2007, 24, 1425–1436. [Google Scholar] [CrossRef] [PubMed]
- Frohlich, S.; Johnson, P.; Moriarty, J. Prevalence, management and outcomes of traumatic brain injury patients admitted to an Irish intensive care unit. Ir. J. Med. Sci. 2011, 180, 423–427. [Google Scholar] [CrossRef]
- Ma, C.; Wu, X.; Shen, X.; Yang, Y.; Chen, Z.; Sun, X.; Wang, Z. Sex differences in traumatic brain injury: A multi-dimensional exploration in genes, hormones, cells, individuals, and society. Chin. Neurosurg. J. 2019, 5, 24. [Google Scholar] [CrossRef]
- Munivenkatappa, A.; Agrawal, A.; Shukla, D.P.; Kumaraswamy, D.; Devi, B.I. Traumatic brain injury: Does gender influence outcomes? Int. J. Crit. Illn. Inj. Sci. 2016, 6, 70–73. [Google Scholar] [CrossRef]
- Kalpakjian, C.Z.; Hanks, R.; Quint, E.H.; Millis, S.; Sander, A.M.; Lequerica, A.H.; Bushnik, T.; Brunner, R.; Rapport, L. Assessing menopause symptoms in women with traumatic brain injury: The development and initial testing of a new scale. Women Health 2023, 64, 51–64. [Google Scholar] [CrossRef]
- Ranganathan, P.; Kumar, R.G.; Davis, K.; McCullough, E.H.; Berga, S.L.; Wagner, A.K. Longitudinal sex and stress hormone profiles among reproductive age and post-menopausal women after severe TBI: A case series analysis. Brain Inj. 2016, 30, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Biscardi, M.; Shafi, R.; Cullen, N.; Einstein, G.; Colantonio, A. Menopause, anti-Müllerian hormone and cognition in a cohort of women with persistent symptoms following TBI: A case for future research. Brain Inj. 2021, 35, 934–942. [Google Scholar] [CrossRef]
- Yue, J.K.; Krishnan, N.; Chyall, L.; Vega, P.; Hamidi, S.; Etemad, L.; Tracey, J.X.; Tarapore, P.E.; Huang, M.C.; Manley, G.T.; et al. Socioeconomic and clinical factors associated with prolonged hospital length of stay after traumatic brain injury. Injury 2023, 54, 110815. [Google Scholar] [CrossRef]
- Haines, K.L.; Nguyen, B.P.; Vatsaas, C.; Alger, A.; Brooks, K.; Agarwal, S.K. Socioeconomic Status Affects Outcomes After Severity-Stratified Traumatic Brain Injury. J. Surg. Res. 2019, 235, 131–140. [Google Scholar] [CrossRef]
- Meo, N.; Liao, J.M.; Reddy, A. Hospitalized After Medical Readiness for Discharge: A Multidisciplinary Quality Improvement Initiative to Identify Discharge Barriers in General Medicine Patients. Am. J. Med. Qual. 2020, 35, 23–28. [Google Scholar] [CrossRef]
- McQuistion, K.; Zens, T.; Jung, H.S.; Beems, M.; Leverson, G.; Liepert, A.; Scarborough, J.; Agarwal, S. Insurance status and race affect treatment and outcome of traumatic brain injury. J. Surg. Res. 2016, 205, 261–271. [Google Scholar] [CrossRef]
- Rauch, S.; Marzolo, M.; Cappello, T.D.; Ströhle, M.; Mair, P.; Pietsch, U.; Brugger, H.; Strapazzon, G. Severe traumatic brain injury and hypotension is a frequent and lethal combination in multiple trauma patients in mountain areas—An analysis of the prospective international Alpine Trauma Registry. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 61. [Google Scholar] [CrossRef]
- Lafta, G.; Sbahi, H. Factors associated with the severity of traumatic brain injury. Med. Pharm. Rep. 2023, 96, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Tolonen, A.; Turkka, J.; Salonen, O.; Ahoniemi, E.; Alaranta, H. Traumatic brain injury is under-diagnosed in patients with spinal cord injury. J. Rehabil. Med. 2007, 39, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Macciocchi, S.; Seel, R.T.; Thompson, N.; Byams, R.; Bowman, B. Spinal Cord Injury and Co-Occurring Traumatic Brain Injury: Assessment and Incidence. Arch. Phys. Med. Rehabil. 2008, 89, 1350–1357. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.E. Alcohol and trauma: The perfect storm. J. Trauma 2005, 59, S53–S56. [Google Scholar] [CrossRef]
- VanderVeen, J.D. TBI as a Risk Factor for Substance Use Behaviors: A Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 1198–1209. [Google Scholar] [CrossRef] [PubMed]
- Leijdesdorff, H.A.; Legué, J.; Krijnen, P.; Rhemrev, S.; Kleinveld, S.; Schipper, I.B. Traumatic brain injury and alcohol intoxication: Effects on injury patterns and short-term outcome. Eur. J. Trauma Emerg. Surg. 2021, 47, 2065–2072. [Google Scholar] [CrossRef]
- Madan, A.K.; Yu, K.; Beech, D.J.; Derrick, J. Alcohol and drug use in victims of life-threatening trauma. J. Trauma Acute Care Surg. 1999, 47, 568–571. [Google Scholar] [CrossRef]
- Dams-O’Connor, K.; Gibbons, L.E.; Landau, A.; Larson, E.B.; Crane, P.K. Health Problems Precede Traumatic Brain Injury in Older Adults. J. Am. Geriatr. Soc. 2016, 64, 844–848. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.F.; Stulc, J.L.; Skolarus, L.E.; Sears, E.D.; Zahuranec, D.B.; Morgenstern, L.B. Traumatic brain injury may be an independent risk factor for stroke. Neurology 2013, 81, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Hammond, F.M.; Corrigan, J.D.; Ketchum, J.M.; Malec, J.F.; Dams-O’Connor, K.; Hart, T.; Novack, T.A.; Bogner, J.; Dahdah, M.N.; Whiteneck, G.G. Prevalence of Medical and Psychiatric Comorbidities Following Traumatic Brain Injury. J. Head Trauma Rehabil. 2019, 34, E1–E10. [Google Scholar] [CrossRef]
- Tohme, S.; Delhumeau, C.; Zuercher, M.; Haller, G.; Walder, B. Prehospital risk factors of mortality and impaired consciousness after severe traumatic brain injury: An epidemiological study. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 1. [Google Scholar] [CrossRef]
- Berry, C.; Ley, E.J.; Bukur, M.; Malinoski, D.; Margulies, D.R.; Mirocha, J.; Salim, A. Redefining hypotension in traumatic brain injury. Injury 2012, 43, 1833–1837. [Google Scholar] [CrossRef] [PubMed]
- Barton, C.W.; Hemphill, J.C.; Morabito, D.; Manley, G. A novel method of evaluating the impact of secondary brain insults on functional outcomes in traumatic brain-injured patients. Acad. Emerg. Med. 2005, 12, 1–6. [Google Scholar] [CrossRef]
- Manley, G.; Knudson, M.M.; Morabito, D.; Damron, S.; Erickson, V.; Pitts, L. Hypotension, Hypoxia, and Head Injury Frequency, Duration, and Consequences. Arch. Surg. 2001, 136, 1118–1123. [Google Scholar] [CrossRef]
- Krishnamoorthy, V.; Vavilala, M.S.; Mills, B.; Rowhani-Rahbar, A. Demographic and clinical risk factors associated with hospital mortality after isolated severe traumatic brain injury: A cohort study. J. Intensive Care 2015, 10, 46. [Google Scholar] [CrossRef]
- Hosomi, S.; Sobue, T.; Kitamura, T.; Hirayama, A.; Ogura, H.; Shimazu, T. Association between vasopressor use and mortality in patients with severe traumatic brain injury: A nationwide retrospective cohort study in Japan. Acute Med. Surg. 2021, 8, e695. [Google Scholar] [CrossRef]
- Toro, C.; Temkin, N.; Barber, J.; Manley, G.; Jain, S.; Ohnuma, T.; Komisarow, J.; Foreman, B.; Korley, F.K.; Vavilala, M.S.; et al. Association of Vasopressor Choice with Clinical and Functional Outcomes Following Moderate to Severe Traumatic Brain Injury: A TRACK-TBI Study. Neurocrit. Care 2022, 36, 180–191. [Google Scholar] [CrossRef]
- Brassard, P.; Seifert, T.; Secher, N.H. Is cerebral oxygenation negatively affected by infusion of norepinephrine in healthy subjects? Br. J. Anaesth. 2009, 102, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.E.; Christensen, R.E.; Baekgaard, J.; Steinmetz, J.; Rasmussen, L.S. Supplemental oxygen for traumatic brain injury: A systematic review. Anaesthesiol. Scand. 2022, 66, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Taran, S.; Cho, S.M.; Stevens, R.D. Mechanical Ventilation in Patients with Traumatic Brain Injury: Is it so Different? Neurocritical Care 2023, 38, 178–191. [Google Scholar] [CrossRef]
- Siig, H.H.; Nielsen, J.F.; Odgaard, L. Epilepsy after severe traumatic brain injury: Frequency and injury severity. Brain Inj 2020, 34, 889–894. [Google Scholar] [CrossRef] [PubMed]
- Souter, M.J.; Kirschen, M. Brain death: Optimizing support of the traumatic brain injury patient awaiting organ procurement. Curr. Opin. Crit. Care 2020, 26, 155–161. [Google Scholar] [CrossRef]
- Heppekcan, D.; Ekin, S.; Çivi, M.; Tok, A.D. Impact of Secondary Insults in Brain Death After Traumatic Brain Injury. Transpl. Proc. 2019, 51, 2186–2188. [Google Scholar] [CrossRef]
| Frequency | Percentage | 95% CI | Mean (S.D.) | 95% CI | ||
|---|---|---|---|---|---|---|
| Mortality | Age (years) | 37.81 (16.72) | 34.4–41.2 | |||
| Alive | 75 | 77.30% | 0.69–0.87 | Weight (kg) | 78.29 (14.18) | 75.3–81.2 |
| Deceased | 19 | 19.60% | 0.12–0.30 | Initial GCS (points) | 8.97 (3.67) | 8.2–9.7 |
| Sex | SBP emergencies (mmHg) | 126.75 (25.81) | 121.3–132.1 | |||
| Men | 82 | 87.20% | 0.77–0.92 | DBP emergencies (mmHg) | 72.69 (14.24) | 69.7–75.6 |
| Women | 12 | 12.70% | 0.07–0.22 | Vasopressor dosage (mcg/kg/min) | 0.15 (0.12) | 0.09–0.21 |
| Influence of illegal drugs at time of injury | Initial Sh (g/dL) | 13.24 (2.63) | 12.6–13.8 | |||
| Present | 5 | 5.30% | 0.01–0.11 | Initial Sc (mg/dL) | 1.02 (0.41) | 0.9–1.1 |
| Absent | 89 | 95.60% | 0.88–0.98 | Hospital stays (days) | 31.37 (30.49) | 25.1–37.5 |
| Influence of alcohol at time of injury | Hospital arrival time (days) | 7.78 (31.37) | 27.3–48.2 | |||
| Present | 22 | 23.40% | 0.15–0.33 | |||
| Absent | 72 | 76.50% | 0.66–0.84 | |||
| Glasgow Coma Scale (points) | ||||||
| Mild | 21 | 22.34% | 0.15–0.32 | |||
| Moderate | 21 | 22.34% | 0.15–0.33 | |||
| Severe | 52 | 55.31% | 0.43–0.64 | |||
| Trauma mechanism | ||||||
| Physical aggression | 6 | 6.30% | 0.02–0.13 | |||
| Assault with weapon | 8 | 8.50% | 0.04–0.16 | |||
| Falls | 31 | 32.90% | 0.23–0.43 | |||
| Injured pedestrian | 5 | 5.31% | 0.01–0.12 | |||
| Car accident | 11 | 11.70% | 0.06–0.20 | |||
| Motorcycle accident | 33 | 35.10% | 0.25–0.45 |
| Mean (SD) | p-Value | 95% CI | ||
|---|---|---|---|---|
| alive (n = 75) | deceased (n = 19) | |||
| Age (years) | 36.9 (15.23) | 40.5 (19.3) | 0.09 | −13.54–6.28 |
| Weight (kg) | 78.7(14.21) | 76 (14.81) | 0.78 | −5.47–10.91 |
| SBP (mmHg) | 125 (26.01) | 131.6 (25.21) | 0.61 | −20.29–7 |
| DBP (mmHg) | 71.7 (15.04) | 76 (11.09) | 0.054 | −11.8–3.23 |
| Initial GCS (points) | 9 (3.63) | 9.3 (3.8) | 0.77 | −2.35–1.61 |
| Vasopressor dosage (mcg/kg/min) | 0.15 (0.13) | 0.2 (0.05) | - | - |
| Sh (g/dL) | 13.4 (2.72) | 12.6 (1.98) | 0.98 | −0.6–2.19 |
| Sc (mg/dL) | 1.04 (0.42) | 0.91 (0.11) | 0.42 | −0.03–0.29 |
| Hospital stays (days) | 33.1 (30.54) | 21.7 (27.9) | 0.35 | −3.4–26.37 |
| Alive | Deceased | p-Value | OR | 95% CI | |
|---|---|---|---|---|---|
| Sex | |||||
| Men | 66 | 16 | 0.314 | 0.51 | −1.9–0.7 |
| Women | 9 | 3 | |||
| Influence of illegal drugs at time of injury | |||||
| Present | 4 | 1 | 0.817 | 1.31 | −2.7–2.3 |
| Absent | 71 | 18 | |||
| Influence of alcohol at time of injury | |||||
| Present | 18 | 4 | 0.765 | 0.82 | −1.5–0.9 |
| Absent | 56 | 16 | |||
| Pupil state | |||||
| Isochoric | 45 | 10 | 0.252 | 2.0 | −0.5–1.8 |
| Anisochoric | 15 | 7 | 0.131 | 5.0 | −0.6–3.8 |
| Mydriasis | 4 | 4 | 0.850 | 1.23 | −2.8–2.2 |
| Miosis | 6 | 2 | 0.995 | 3.1 × 10−7 | -- |
| Enucleation | 1 | 0 | 0.995 | 3.1 × 10−7 | -- |
| Pupillary reflex | |||||
| Reactive | 5 | 1 | 0.824 | 0.77 | −3.2–1.6 |
| Unknown | 70 | 18 | |||
| Complications | |||||
| Present | 40 | 9 | 0.642 | 0.78 | −1.2–0.7 |
| Absent | 35 | 10 | |||
| Use of vasopressors | |||||
| Present | 21 | 3 | 0.283 | 0.48 | −2.2–0.4 |
| Absent | 54 | 16 | |||
| Vasopressor type | |||||
| Norepinephrine | 57 | 17 | 0.994 | 1.21 × 107 | -- |
| Vasopressin | 5 | 0 | 1.000 | 1.0 | −98.8–98.8 |
| Norepinephrine and vasopressin | 10 | 5 | 0.994 | 1.59 × 107 | -- |
| Use of mechanical ventilation | |||||
| Present | 48 | 9 | 0.189 | 0.50 | −1.7–0.3 |
| Absent | 27 | 10 | |||
| Use of hypertonic solution | |||||
| Present | 16 | 5 | 0.663 | 1.29 | −0.9–1.3 |
| Absent | 58 | 14 | |||
| Marshall scale on entry | |||||
| Diffuse type I lesion | 4 | 2 | |||
| Diffuse type II lesion | 12 | 2 | 0.404 | 0.27 | −4.7–2.1 |
| Diffuse type III lesion | 19 | 11 | 0.675 | 1.66 | −1.6–3.5 |
| Diffuse type IV lesion | 21 | 5 | 0.689 | 0.60 | −2.8–2.6 |
| Evacuated mass | 4 | 0 | 0.991 | 1.91 × 10−7 | -- |
| Mass not evacuated | 12 | 2 | 0.404 | 0.27 | −4.7–2.1 |
| HR | SE | CI 95% | p-Value | |
|---|---|---|---|---|
| Encephalic-dead | 17.48 | 0.584 | 5.56–54.93 | *** |
| Sex M | 0.5111 | 0.573 | 0.16–1.57 | 0.242 |
| Additional trauma | ||||
| thorax | 0.70 | 0.806 | 0.15–3.73 | 0.745 |
| abdomen | 0 | 7860 | 0.00–inf | 0.998 |
| neck | 1.98 | 0.828 | 0.39–10.07 | 0.407 |
| neck and spine | 2.45 | 0.562 | 0.81–7.39 | 0.110 |
| extremities | 7.11 | 0.813 | 1.44–35.01 | 0.015 * |
| Convulsive crisis | 8.18 | 0.662 | 2.23–29.97 | 0.001 * |
| Vasopressor administration | ||||
| urgency | 7.55 × 107 | 8.04 × 103 | 0–Inf | 0.002 * |
| surgery | 2.10 × 109 | 8.04 × 103 | 0–Inf | 0.003 * |
| IMCU | 2.55 × 108 | 8.04 × 103 | 0–Inf | 0.002 * |
| ICU | 1.66 × 108 | 8.04 × 103 | 0–Inf | 0.002 * |
| Medical history | ||||
| DM | 6.64 | 7.80 × 10−1 | 1.44–30.63 | 0.015 * |
| SAH | 2.34 | 7.79 × 10−1 | 0.50–10.81 | 0.273 |
| HD | 3.51 | 1.09 × 100 | 0.41–29.81 | 0.248 |
| DM+SAH | 3.56 | 7.81 × 10−1 | 0.77–16.5 | 0.103 |
| CC | 2.10 × 10−7 | 5.31 × 103 | 0.00–inf | 0.997 |
| DM+SAH+PH+CHF | 11.3 | 1.07 × 100 | 1.38–92.91 | 0.023 * |
| Cox’s Regression | Coefficient | Hazard Ratio | 95% CI | SE (Coefficient) | p-Value |
|---|---|---|---|---|---|
| Encephalic death | 2.589 | 13.3 | 3.90–45.47 | 0.626 | *** |
| Seizures | 1.346 | 3.84 | 0.58–25.24 | 0.960 | 0.161 |
| Age | −0.002 | 0.99 | 0.96–1.03 | 0.018 | 0.888 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Herrera, E.; Galindo-Oseguera, E.; Castillo-Cruz, J.; Fuentes-Venado, C.E.; Gasca-López, G.A.; Calzada-Mendoza, C.C.; Ocharan-Hernández, E.; Zúñiga-Cruz, C.A.; Farfán-García, E.D.; Arellano-Ramírez, A.; et al. Mortality-Associated Factors in a Traumatic Brain Injury Population in Mexico. Biomedicines 2024, 12, 2037. https://doi.org/10.3390/biomedicines12092037
Martínez-Herrera E, Galindo-Oseguera E, Castillo-Cruz J, Fuentes-Venado CE, Gasca-López GA, Calzada-Mendoza CC, Ocharan-Hernández E, Zúñiga-Cruz CA, Farfán-García ED, Arellano-Ramírez A, et al. Mortality-Associated Factors in a Traumatic Brain Injury Population in Mexico. Biomedicines. 2024; 12(9):2037. https://doi.org/10.3390/biomedicines12092037
Chicago/Turabian StyleMartínez-Herrera, Erick, Evelyn Galindo-Oseguera, Juan Castillo-Cruz, Claudia Erika Fuentes-Venado, Gilberto Adrián Gasca-López, Claudia C. Calzada-Mendoza, Esther Ocharan-Hernández, Carlos Alberto Zúñiga-Cruz, Eunice D. Farfán-García, Alfredo Arellano-Ramírez, and et al. 2024. "Mortality-Associated Factors in a Traumatic Brain Injury Population in Mexico" Biomedicines 12, no. 9: 2037. https://doi.org/10.3390/biomedicines12092037
APA StyleMartínez-Herrera, E., Galindo-Oseguera, E., Castillo-Cruz, J., Fuentes-Venado, C. E., Gasca-López, G. A., Calzada-Mendoza, C. C., Ocharan-Hernández, E., Zúñiga-Cruz, C. A., Farfán-García, E. D., Arellano-Ramírez, A., & Pinto-Almazán, R. (2024). Mortality-Associated Factors in a Traumatic Brain Injury Population in Mexico. Biomedicines, 12(9), 2037. https://doi.org/10.3390/biomedicines12092037








