Unveiling a Dermatological Rarity: The Enigma of Vulvar Intraepithelial Neoplasia Grade III (HSIL) and the Role of p53 in Its Development
Abstract
1. Introduction
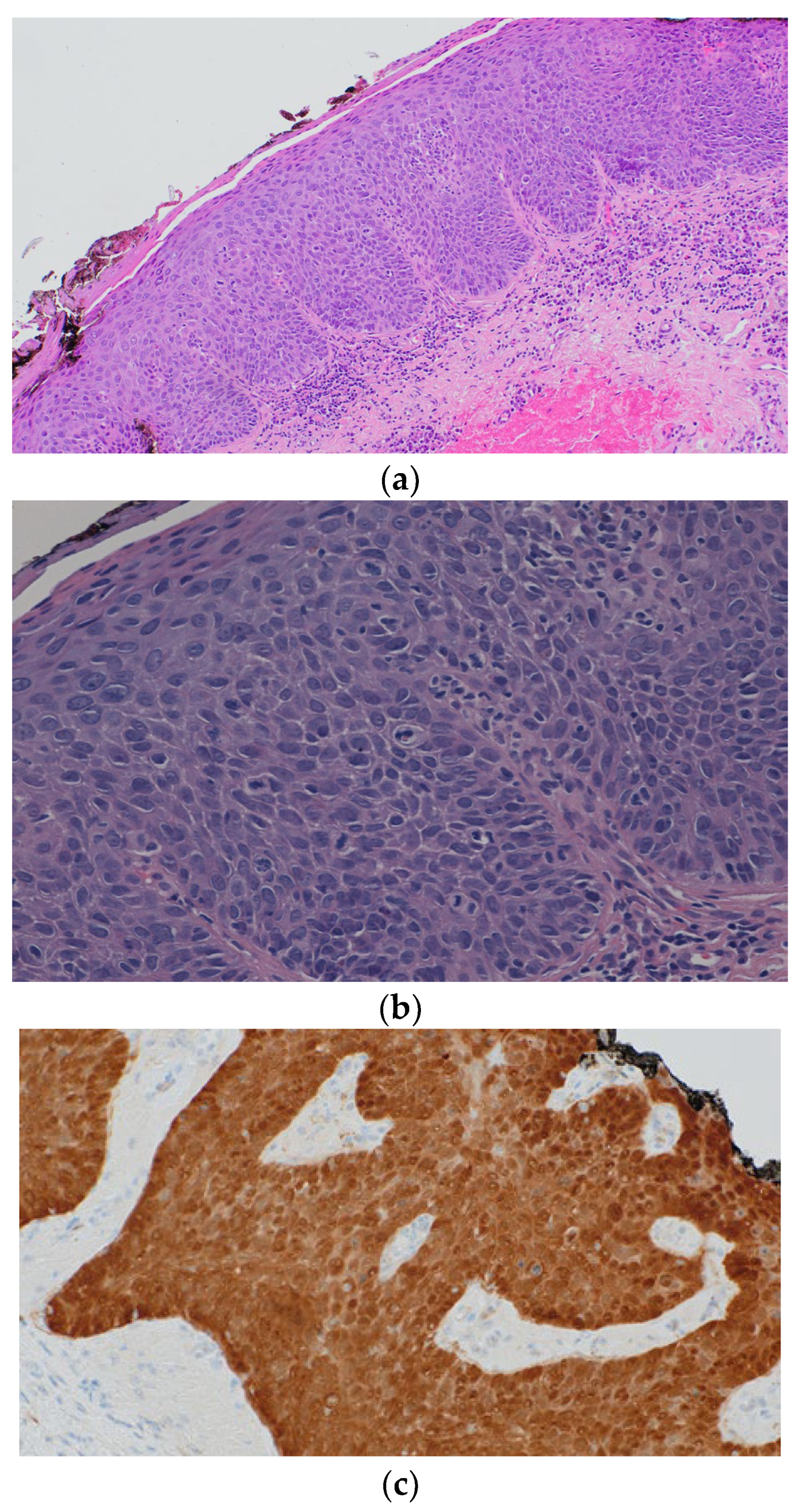
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bornstein, J.; Bogliatto, F.; Haefner, H.K.; Stockdale, C.K.; Preti, M.; Bohl, T.G.; Reutter, J.; ISSVD Terminology Committee. The 2015 International Society for the Study of Vulvovaginal Disease (ISSVD) Terminology of Vulvar Squamous Intraepithelial Lesions. J. Low. Genit. Tract Dis. 2016, 20, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Darragh, T.M.; Colgan, T.J.; Cox, J.T.; Heller, D.S.; Henry, M.R.; Luff, R.D.; McCalmont, T.; Nayar, R.; Palefsky, J.M.; Stoler, M.H.; et al. The Lower Anogenital Squamous Terminology Standardization Project for HPV-Associated Lesions: Background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. J. Low. Genit. Tract Dis. 2012, 16, 205–242. [Google Scholar] [CrossRef] [PubMed]
- Sideri, M.G.; Jones, R.W.; Wilkinson, E.J.; Preti, M.; Heller, D.S.; Scurry, J.; Haefner, H.; Neill, S. Squamous Vulvar Intraepithelial Neoplasia: 2004 Modified Terminology, ISSVD Vulvar Oncology Subcommittee. J. Reprod. Med. 2005, 50, 807–810. [Google Scholar] [CrossRef] [PubMed]
- Woelber, L.; Prieske, K.; Eulenburg, C.; Oliveira-Ferrer, L.; de Gregorio, N.; Klapdor, R.; Kalder, M.; Braicu, I.; Fuerst, S.; Klar, M.; et al. p53 and p16 expression profiles in vulvar cancer: Atranslational analysis by the Arbeitsgemeinschaft Gynäkologische Onkologie Chemo and Radiotherapy in Epithelial Vulvar Cancer study group. Am. J. Obstet. Gynecol. 2021, 224, 595.e1–595.e11. [Google Scholar] [CrossRef] [PubMed]
- Liebl, M.C.; Hofmann, T.G. The Role of p53 Signaling in Colorectal Cancer. Cancers 2021, 13, 2125. [Google Scholar] [CrossRef] [PubMed]
- Zawacka-Pankau, J.E. The Role of p53 Family in Cancer. Cancers 2022, 14, 823. [Google Scholar] [CrossRef] [PubMed]
- Marei, H.E.; Althani, A.; Afifi, N.; Hasan, A.; Caceci, C.; Pozzoli, G.; Morrione, A.; Giordano, A.; Cenciarelli, C. p53 signaling in cancer progression and therapy. Cancer Cell Int. 2021, 21, 703. [Google Scholar] [CrossRef] [PubMed]
- Rahmé, R.; Braun, T.; Manfredi, J.J.; Fenaux, P. TP53 Alterations in Myelodysplastic Syndromes and Acute Myeloid Leukemia. Biomedicines 2023, 11, 1152. [Google Scholar] [CrossRef] [PubMed]
- Baugh, E.H.; Ke, H.; Levine, A.J.; Bonneau, R.A.; Chan, C.S. Why are there hotspot mutations in the TP53 gene in human cancers? Cell Death Differ. 2018, 25, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Nobori, T.; Miura, K.; Wu, D.J.; Lois, A.; Takabayashi, K.; Carson, D.A. Deletions of the cyclin-dependent kinase-4 inhibitor gene in multiple human cancers. Nature 1994, 368, 753–756. [Google Scholar] [CrossRef] [PubMed]
- Stone, S.; Jiang, P.; Dayananth, P.; Tavtigian, S.V.; Katcher, H.; Parry, D.; Peters, G.; Kamb, A. Complex structure and regulation of the P16 (MTS1) locus. Cancer Res. 1995, 55, 2988–2994. [Google Scholar] [PubMed]
- Fedak, E.A.; Adler, F.R.; Abegglen, L.M.; Schiffman, J.D. ATM and ATR Activation Through Crosstalk Between DNA Damage Response Pathways. Bull. Math. Biol. 2021, 83, 38. [Google Scholar] [CrossRef] [PubMed]
- Committee on Gynecologic Practice of American College Obstetricians and Gynecologists. ACOG Committee Opinion No. 509: Management of vulvar intraepithelial neoplasia. Obstet. Gynecol. 2011, 118, 1192–1194. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, E.J.; Rush, D.S. The histopathology of vulvar neoplasia. In Global Library of Women’s Medicine; GLOWM: London, UK, 2008. [Google Scholar] [CrossRef]
- Reyes, M.C.; Cooper, K. An update on vulvar intraepithelial neoplasia: Terminology and a practical approach to diagnosis. J. Clin. Pathol. 2014, 67, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Grapsa, D.; Frangou-Plemenou, M.; Kondi-Pafiti, A.; Stergiou, E.; Nicolopoulou-Stamati, P.; Patsouris, E.; Chelidonis, G.; Athanassiadou, P. Immunocytochemical expression of P53, PTEN, FAS (CD95), P16INK4A and HPV L1 major capsid proteins in ThinPrep cervical samples with squamous intraepithelial lesions. Diagn. Cytopathol. 2014, 42, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Thuijs, N.B.; van Beurden, M.; Duin, S.; Heideman, D.A.M.; Berkhof, J.; Steenbergen, R.D.M.; Bleeker, M.C.G. High-grade vulvar intraepithelial neoplasia: Comprehensive characterization and long-term vulvar carcinoma risk. Histopathology 2024, 84, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Van Seters, M.; van Beurden, M.; de Craen, A.J.M. Is the assumed natural history of vulvar intraepithelial neoplasia III based on enough evidence? A systematic review of 3322 published patients. Gynecol. Oncol. 2005, 97, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Van de Nieuwenhof, H.P.; van der Avoort, I.A.M.; de Hullu, J.A. Review of squamous premalignant vulvar lesions. Crit. Rev. Oncol. Hematol. 2008, 68, 131–156. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, N.; Kjaer, S.K.; Sigurdsson, K.; Iversen, O.-E.; Hernandez-Avila, M.; Wheeler, C.M.; Perez, G.; Brown, D.R.; Koutsky, L.A.; Tay, E.H.; et al. Impact of human papillomavirus (HPV)-6/11/16/18 vaccine on all HPV-associated genital diseases in young women. J. Natl. Cancer Inst. 2010, 102, 325–339. [Google Scholar] [CrossRef]
- Committee on Gynecologic Practice of American College Obstetricians and Gynecologists. ACOG Committee Opinion No. 704: Human Papillomavirus Vaccination. Obstet. Gynecol. 2017, 129, e173–e178. [Google Scholar] [CrossRef] [PubMed]
- Dehlendorff, C.; Baandrup, L.; Kjaer, S.K. Real-World Effectiveness of Human Papillomavirus Vaccination Against Vulvovaginal High-Grade Precancerous Lesions and Cancers. J. Natl. Cancer Inst. 2021, 113, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.W. Vulval intraepithelial neoplasia: Current perspectives. Eur. J. Gynaecol. Oncol. 2001, 22, 393–402. [Google Scholar] [PubMed]
- Newcomb, P.A.; Weiss, N.S.; Daling, J.R. Incidence of vulvar carcinoma in relation to menstrual, reproductive, and medical factors. J. Natl. Cancer Inst. 1984, 73, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Thuis, Y.N.; Campion, M.; Fox, H.; Hacker, N.F. Contemporary experience with the management of vulvar intraepithelial neoplasia. Int. J. Gynecol. Cancer 2000, 10, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Bleeker, M.C.; Visser, P.J.; Overbeek, L.I.H.; van Beurden, M.; Berkhof, J. Lichen Sclerosus: Incidence and Risk of Vulvar Squamous Cell Carcinoma. Cancer Epidemiol. Biomark. Prev. 2016, 25, 1224–1230. [Google Scholar] [CrossRef] [PubMed]
- Rodolakis, A.; Diakomanolis, E.; Vlachos, G.; Iconomou, T.; Protopappas, A.; Stefanidis, C.; Elsheikh, H.; Michalas, S. Vulvar intraepithelial neoplasia (VIN)—Diagnostic and therapeutic challenges. Eur. J. Gynaecol. Oncol. 2003, 24, 317–322. [Google Scholar] [PubMed]
- Fox, H.; Wells, M. Recent advances in the pathology of the vulva. Histopathology 2003, 42, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.W.; Cheung, A.N.Y. Predictive and prognostic biomarkers in female genital tract tumours: An update highlighting their clinical relevance and practical issues. Pathology 2024, 56, 214–227. [Google Scholar] [CrossRef] [PubMed]
- Gage, J.C.; Schiffman, M.; Hunt, W.C.; Joste, N.; Ghosh, A.; Wentzensen, N.; Wheeler, C.M.; New Mexico HPV Pap Registry Steering Committee. Cervical histopathology variability among laboratories: A population-based statewide investigation. Am. J. Clin. Pathol. 2013, 139, 330–335. [Google Scholar] [CrossRef] [PubMed]
- El Faqyr, I.; Dref, M.; Zahid, S.; Oualla, J.; Mansouri, N.; Rais, H.; Hocar, O.; Amal, S. Syringocystadenoma papilliferum presented as an ulcerated nodule of the vulva in a patient with Neurofi bromatosis type 1. Our Dermatol. Online 2020, 11, 174–176. [Google Scholar] [CrossRef]
- Shivamurthy, A.; Jaiprakash, P.; Lavany, P. Aggressive angiomyxoma of the vulva—A rare entity. Our Dermatol. Online 2016, 7, 436–438. [Google Scholar] [CrossRef][Green Version]
- Eleni, K. Giant vulvar ulcers in the course of adult onset cyclic neutropenia. Our Dermatol. Online 2018, 9, 337–338. [Google Scholar] [CrossRef]
- Puri, N.; Puri, A. A study on dermatoses of pregnancy. Our Dermatol. Online 2013, 4, 56–60. [Google Scholar] [CrossRef]
- Tziotzios, C.; Lee, J.Y.W.; Brier, T.; Sait, R.; Hsu, C.-K.; Bhargava, K.; Stefanato, C.M.; Fenton, D.A.; McGrath, J.A. Lichen planus and lichenoid dermatoses: Clinical overview and molecular basis. J. Am. Acad. Dermatol. 2018, 79, 789–804. [Google Scholar] [CrossRef] [PubMed]
- Puri, N.; Puri, A. A study on non venereal genital dermatoses in north India. Our Dermatol. Online 2012, 3, 304–307. [Google Scholar] [CrossRef]
- Bachaspatimayum, R.; Zamzachin, G.; Devi, T.B. Clinical and laboratory profi les of genital ulcers (sexually transmitted diseases) in a tertiary care center in northeastern India. Our Dermatol. Online 2021, 12, 120–129. [Google Scholar] [CrossRef]
- Nassiri, A.; Moustaide, K.; Elloudi, S.; Baybay, H.; Mernissi, F.Z. Vulvar pruritus: A view over a life. Our Dermatol. Online 2020, 11, 191–193. [Google Scholar] [CrossRef]
- Tiwary, A.; Bachaspatimayum, R. Herpes simplex virus serology in genital ulcer disease in a tertiary care hospital. Our Dermatol. Online 2020, 11 (Suppl. S3), 6–9. [Google Scholar] [CrossRef]
- Inamura, Y.; Kitamura, S.; Imafuku, K.; Hata, H.; Shimizu, H. Treatment option of advanced of vulvar carcinoma with cisplatin, 5-FU, and TS-1. Our Dermatol. Online 2016, 7, 110–111. [Google Scholar] [CrossRef]
- Wallbillich, J.J.; Rhodes, H.E.; Milbourne, A.M.; Munsell, M.F.; Frumovitz, M.; Brown, J.; Trimble, C.L.; Schmeler, K.M. Vulvar intraepithelial neoplasia (VIN 2/3): Comparing clinical outcomes and evaluating risk factors for recurrence. Gynecol. Oncol. 2012, 127, 312–315. [Google Scholar] [CrossRef]
- Modesitt, S.C.; Waters, A.B.; Walton, L.; Fowler, W.C., Jr.; Van Le, L. Vulvar intraepithelial neoplasia III: Occult cancer and the impact of margin status on recurrence. Obstet. Gynecol. 1998, 92, 962–966. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.W.; Baranyai, J.; Stables, S. Trends in squamous cell carcinoma of the vulva: The influence of vulvar intraepithelial neoplasia. Obstet. Gynecol. 1997, 90, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Terlou, A.; van Seters, M.; Ewing, P.C.; Aaronson, N.K.; Gundy, C.M.; Heijmans-Antonissen, C.; Quint, W.G.V.; Blok, L.J.; van Beurden, M.; Helmerhorst, T.J.M. Treatment of vulvar intraepithelial neoplasia with topical imiquimod: Seven years median follow-up of a randomized clinical trial. Gynecol. Oncol. 2011, 121, 157–162. [Google Scholar] [CrossRef] [PubMed]

| 1986 ISSVD | 2004 ISSVD | 2012 LAST | 2015 ISSVD |
|---|---|---|---|
| VIN 1 (mild dysplasia) | Condyloma | LSIL | LSIL of the vulva (flat condyloma, vulvar LSIL, HPV effect) |
| VIN 2 (moderate dysplasia) | VIN, usual type | ||
| VIN, warty type VIN, basaloid type VIN, mixed type | HSIL | HSIL (vulvar HSIL, VIN usual type) | |
| VIN 3 (severe dysplasia) VIN 3 (carcinoma in situ) | |||
| VIN differentiated | N/A | Differentiated VIN | |
| Differentiated VIN | |||
| Type | p53(+) % (n) | p53(−) % (n) | p16(+) % (n) | p16(−)% (n) |
|---|---|---|---|---|
| LSIL | 0% (0) | 100% (61) | 44.3% (27) | 55.7% (34) |
| HSIL | 36.4% (4) | 63.6% (7) | 90.9% (10) | 9.1% (1) |
| Total | 4.3% (4) | 95.7% (88) | 40.2% (37) | 59.8% (55) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brzeziński, P.; Feszak, I.; Ortiz, B.D.M.; Feszak, S.; Kawczak, P.; Bączek, T. Unveiling a Dermatological Rarity: The Enigma of Vulvar Intraepithelial Neoplasia Grade III (HSIL) and the Role of p53 in Its Development. Biomedicines 2024, 12, 1799. https://doi.org/10.3390/biomedicines12081799
Brzeziński P, Feszak I, Ortiz BDM, Feszak S, Kawczak P, Bączek T. Unveiling a Dermatological Rarity: The Enigma of Vulvar Intraepithelial Neoplasia Grade III (HSIL) and the Role of p53 in Its Development. Biomedicines. 2024; 12(8):1799. https://doi.org/10.3390/biomedicines12081799
Chicago/Turabian StyleBrzeziński, Piotr, Igor Feszak, Beatriz Di Martino Ortiz, Sylwia Feszak, Piotr Kawczak, and Tomasz Bączek. 2024. "Unveiling a Dermatological Rarity: The Enigma of Vulvar Intraepithelial Neoplasia Grade III (HSIL) and the Role of p53 in Its Development" Biomedicines 12, no. 8: 1799. https://doi.org/10.3390/biomedicines12081799
APA StyleBrzeziński, P., Feszak, I., Ortiz, B. D. M., Feszak, S., Kawczak, P., & Bączek, T. (2024). Unveiling a Dermatological Rarity: The Enigma of Vulvar Intraepithelial Neoplasia Grade III (HSIL) and the Role of p53 in Its Development. Biomedicines, 12(8), 1799. https://doi.org/10.3390/biomedicines12081799






