The Interactions between Smoking and Sleep
Abstract
1. Introduction
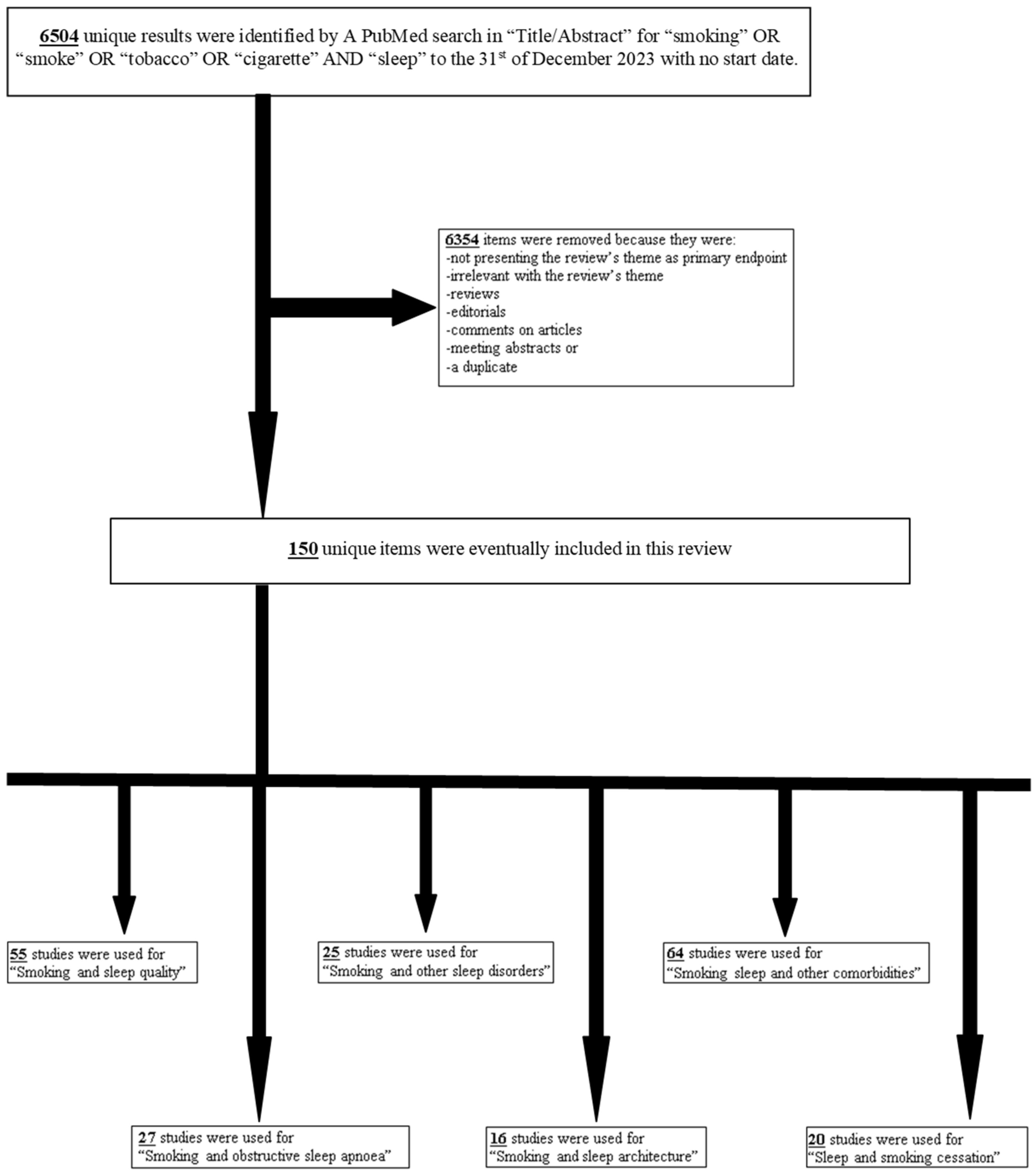
2. Methods
3. Discussion
3.1. Smoking and Sleep Quality
3.2. Smoking and Obstructive Sleep Apnea
3.3. Smoking and Other Sleep Disorders
3.4. Smoking and Sleep Architecture
3.5. Smoking, Sleep and Other Medical Conditions
3.6. Smoking Cessation and Sleep
3.7. Limitations
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Woo, D.H.; Park, M.; Jang, S.Y.; Park, S.; Jang, S.I. Association between smoking status and subjective quality of sleep in the South Korean population: A cross-sectional study. Sleep Breath. 2023, 27, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Riemerth, A.; Kunze, U.; Groman, E. Nocturnal sleep-disturbing nicotine craving and accomplishment with a smoking cessation program. Wien. Med. Wochenschr. 2009, 159, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Truong, M.K.; Berger, M.; Haba-Rubio, J.; Siclari, F.; Marques-Vidal, P.; Heinzer, R. Impact of smoking on sleep macro- and microstructure. Sleep Med. 2021, 84, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Purani, H.; Friedrichsen, S.; Allen, A.M. Sleep quality in cigarette smokers: Associations with smoking-related outcomes and exercise. Addict. Behav. 2019, 90, 71–76. [Google Scholar] [CrossRef]
- Yosunkaya, S.; Kutlu, R.; Vatansev, H. Effects of smoking on patients with obstructive sleep apnea syndrome. Clin. Respir. J. 2021, 15, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Nuñez, A.; Rhee, J.U.; Haynes, P.; Chakravorty, S.; Patterson, F.; Killgore, W.D.S.; Gallagher, R.A.; Hale, L.; Branas, C.; Carrazco, N.; et al. Smoke at night and sleep worse? The associations between cigarette smoking with insomnia severity and sleep duration. Sleep Health 2021, 7, 177–182. [Google Scholar] [CrossRef]
- Grigoriou, I.; Skalisti, P.; Papagiouvanni, I.; Michailidou, A.; Charalampidis, K.; Kotoulas, S.C.; Porpodis, K.; Spyratos, D.; Pataka, A. Smoking-Induced Disturbed Sleep. A Distinct Sleep-Related Disorder Pattern? Healthcare 2023, 11, 205. [Google Scholar] [CrossRef] [PubMed]
- Provini, F.; Vetrugno, R.; Montagna, P. Sleep-related smoking syndrome. Sleep Med. 2008, 9, 903–905. [Google Scholar] [CrossRef] [PubMed]
- Frosztega, W.; Wieckiewicz, M.; Nowacki, D.; Michalek-Zrabkowska, M.; Poreba, R.; Wojakowska, A.; Kanclerska, J.; Mazur, G.; Martynowicz, H. Polysomnographic Assessment of Effects of Tobacco Smoking and Alcohol Consumption on Sleep Bruxism Intensity. J. Clin. Med. 2022, 11, 7453. [Google Scholar] [CrossRef]
- Lavigne, G.L.; Lobbezoo, F.; Rompré, P.H.; Nielsen, T.A.; Montplaisir, J. Cigarette smoking as a risk factor or an exacerbating factor for restless legs syndrome and sleep bruxism. Sleep 1997, 20, 290–293. [Google Scholar]
- Alsulami, S.; Althagafi, N.; Hazazi, E.; Alsayed, R.; Alghamdi, M.; Almohammadi, T.; Almurashi, S.; Baig, M. Obesity and Its Associations with Gender, Smoking, Consumption of Sugary Drinks, and Hour of Sleep among King Abdulaziz University Students in Saudi Arabia. Diabetes Metab. Syndr. Obes. 2023, 16, 925–934. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Xu, H.; Chen, R.; Liu, S.; Xia, Y.; Fu, Y.; Li, X.; Qian, Y.; Zou, J.; Yi, H.; et al. Smoking, obstructive sleep apnea syndrome and their combined effects on metabolic parameters: Evidence from a large cross-sectional study. Sci. Rep. 2017, 7, 8851. [Google Scholar] [CrossRef] [PubMed]
- Ioannidou, D.; Kalamaras, G.; Kotoulas, S.C.; Pataka, A. Smoking and Obstructive Sleep Apnea: Is There an Association between These Cardiometabolic Risk Factors?-Gender Analysis. Medicina 2021, 57, 1137. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Wang, J.; Chen, B.; Ji, X.; Zhao, C.; Chen, M.; Liao, S.; Jiang, S.; Pan, Z.; Wang, W.; et al. Association of multiple air pollutants with oxygen saturation during sleep in COPD patients: Effect modification by smoking status and airway inflammatory phenotypes. J. Hazard. Mater. 2023, 454, 131550. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Yin, H.; Shu, X.; Jia, Y.; Leng, M.; Chen, L. Multi-angles of smoking and mild cognitive impairment: Is the association mediated by sleep duration? Neurol. Sci. 2019, 40, 1019–1027. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Zhou, J.; Li, X.; Wang, R. Investigating the causal effects of smoking, sleep, and BMI on major depressive disorder and bipolar disorder: A univariable and multivariable two-sample Mendelian randomization study. Front. Psychiatry 2023, 14, 1206657. [Google Scholar] [CrossRef] [PubMed]
- Merikanto, I.; Paavonen, E.J.; Saarenpää-Heikkilä, O.; Paunio, T.; Partonen, T. Eveningness associates with smoking and sleep problems among pregnant women. Chronobiol. Int. 2017, 34, 650–658. [Google Scholar] [CrossRef]
- Mennella, J.A.; Yourshaw, L.M.; Morgan, L.K. Breastfeeding and smoking: Short-term effects on infant feeding and sleep. Pediatrics 2007, 120, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, C.R.; Kales, J.D.; Scharf, M.B.; Bixler, E.O.; Kales, A. Cigarette smoking associated with sleep difficulty. Science 1980, 207, 551–553. [Google Scholar] [CrossRef]
- Delasnerie-Laupretre, N.; Patois, E.; Valatx, J.L.; Kauffmann, F.; Alperovitch, A. Sleep, snoring and smoking in high school students. J. Sleep Res. 1993, 2, 138–142. [Google Scholar] [CrossRef]
- Wetter, D.W.; Young, T.B. The relation between cigarette smoking and sleep disturbance. Prev. Med. 1994, 23, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Phillips, B.A.; Danner, F.J. Cigarette smoking and sleep disturbance. Arch. Intern. Med. 1995, 155, 734–737. [Google Scholar] [CrossRef] [PubMed]
- Bale, P.; White, M. The effects of smoking on the health and sleep of sportswomen. Br. J. Sports Med. 1982, 16, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Lexcen, F.J.; Hicks, R.A. Does cigarette smoking increase sleep problems. Percept. Mot. Ski. 1993, 77, 16–18. [Google Scholar] [CrossRef] [PubMed]
- Patten, C.A.; Choi, W.S.; Gillin, J.C.; Pierce, J.P. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics 2000, 106, E23. [Google Scholar] [CrossRef] [PubMed]
- Jaehne, A.; Unbehaun, T.; Feige, B.; Lutz, U.C.; Batra, A.; Riemann, D. How smoking affects sleep: A polysomnographical analysis. Sleep Med. 2012, 13, 1286–1292. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.T.; Lee, I.H.; Wang, C.H.; Chen, K.C.; Lee, C.I.; Yang, Y.K. Cigarette smoking might impair memory and sleep quality. J. Formos. Med. Assoc. 2013, 112, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, H.; Li, G.; Kang, Y.; Shi, J.; Kong, T.; Yang, X.; Xu, J.; Li, C.; Su, K.P.; et al. Active smoking, sleep quality and cerebrospinal fluid biomarkers of neuroinflammation. Brain Behav. Immun. 2020, 89, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Peters, E.N.; Fucito, L.M.; Novosad, C.; Toll, B.A.; O’Malley, S.S. Effect of night smoking, sleep disturbance, and their co-occurrence on smoking outcomes. Psychol. Addict. Behav. 2011, 25, 312–319. [Google Scholar] [CrossRef]
- Hwang, J.H.; Park, S.W. The relationship between poor sleep quality measured by the Pittsburgh Sleep Quality Index and smoking status according to sex and age: An analysis of the 2018 Korean Community Health Survey. Epidemiol. Health 2022, 44, e2022022. [Google Scholar] [CrossRef]
- Al-Mshari, A.; AlSheikh, M.H.; Latif, R.; Mumtaz, S.; Albaker, W.; Al-Hariri, M. Impact of smoking intensities on sleep quality in young Saudi males: A comparative study. J. Med. Life 2022, 15, 1392–1396. [Google Scholar] [CrossRef]
- Li, H.; Liu, Y.; Xing, L.; Yang, X.; Xu, J.; Ren, Q.; Su, K.P.; Lu, Y.; Wang, F. Association of Cigarette Smoking with Sleep Disturbance and Neurotransmitters in Cerebrospinal Fluid. Nat. Sci. Sleep 2020, 12, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Bellatorre, A.; Choi, K.; Lewin, D.; Haynie, D.; Simons-Morton, B. Relationships between Smoking and Sleep Problems in Black and White Adolescents. Sleep 2017, 40, zsw031. [Google Scholar] [CrossRef]
- Sahlin, C.; Franklin, K.A.; Stenlund, H.; Lindberg, E. Sleep in women: Normal values for sleep stages and position and the effect of age, obesity, sleep apnea, smoking, alcohol and hypertension. Sleep Med. 2009, 10, 1025–1030. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.P.; Wang, J.; Holiday, D.B.; Warren, J.Y.; Paradoa, M.; Balkhi, A.M.; Fernandez-Baca, J.; McCrae, C.S. Sleep disturbances associated with cigarette smoking. Psychol. Health Med. 2014, 19, 410–419. [Google Scholar] [CrossRef]
- Mak, K.K.; Ho, S.Y.; Thomas, G.N.; Lo, W.S.; Cheuk, D.K.; Lai, Y.K.; Lam, T.H. Smoking and sleep disorders in Chinese adolescents. Sleep Med. 2010, 11, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Mehari, A.; Weir, N.A.; Gillum, R.F. Gender and the association of smoking with sleep quantity and quality in American adults. Women Health 2014, 54, 1–14. [Google Scholar] [CrossRef]
- Merianos, A.L.; Mahabee-Gittens, E.M.; Hill, M.J.; Olaniyan, A.C.; Smith, M.L.; Choi, K. Electronic cigarette use and cigarette smoking associated with inadequate sleep duration among U.S. young adults. Prev. Med. 2023, 175, 107712. [Google Scholar] [CrossRef]
- Sujarwoto, S. Sleep Disturbance in Indonesia: How Much Does Smoking Contribute? Behav. Sleep Med. 2020, 18, 760–773. [Google Scholar] [CrossRef]
- AlRyalat, S.A.; Kussad, S.; El Khatib, O.; Hamad, I.; Al-Tanjy, A.; Alshnneikat, M.; AbuMahfouz, B. Assessing the effect of nicotine dose in cigarette smoking on sleep quality. Sleep Breath. 2021, 25, 1319–1324. [Google Scholar] [CrossRef]
- Nasri, O.; Pouragha, H.; Baigi, V.; Shalyari, N.; Yunesian, M. Quality of life and sleep disorders in Tehran Employees Cohort (TEC); Association with secondhand smoking and wealth index. J. Environ. Health Sci. Eng. 2021, 19, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Banna, M.H.A.; Brazendale, K.; Hamiduzzaman, M.; Ahinkorah, B.O.; Abid, M.T.; Rifat, M.A.; Sultana, M.S.; Tetteh, J.K.; Kundu, S.; Shekhar, M.S.R.; et al. Exposure to secondhand smoke is associated with poor sleep quality among non-smoking university students in Bangladesh: A cross-sectional survey. Sci. Rep. 2023, 13, 16735. [Google Scholar] [CrossRef] [PubMed]
- Nakata, A.; Takahashi, M.; Haratani, T.; Ikeda, T.; Hojou, M.; Fujioka, Y.; Araki, S. Association of active and passive smoking with sleep disturbances and short sleep duration among Japanese working population. Int. J. Behav. Med. 2008, 15, 81–91. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Shankar, A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2011, 12, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Bilsky, S.A.; Feldner, M.T.; Knapp, A.A.; Babson, K.A.; Leen-Feldner, E.W. The interaction between anxiety sensitivity and cigarette smoking level in relation to sleep onset latency among adolescent cigarette smokers. J. Adolesc. 2016, 51, 123–132. [Google Scholar] [CrossRef]
- Bar-Zeev, Y.; Shauly-Aharonov, M.; Neumark, Y.; Hirshoren, N. Changes in Smoking Behavior, Stress, and Sleep Duration among Israeli Hospital Workers During the COVID-19 Pandemic: A Cross-sectional Study. Nicotine Tob. Res. 2023, 25, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Patterson, F.; Malone, S.K.; Lozano, A.; Grandner, M.A.; Hanlon, A.L. Smoking, Screen-Based Sedentary Behavior, and Diet Associated with Habitual Sleep Duration and Chronotype: Data from the UK Biobank. Ann. Behav. Med. 2016, 50, 715–726. [Google Scholar] [CrossRef] [PubMed]
- Parkes, K.R. Age, smoking, and negative affectivity as predictors of sleep patterns among shiftworkers in two environments. J. Occup. Health Psychol. 2002, 7, 156–173. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Takeshima, O.; Itani, O.; Matsumoto, Y.; Kaneita, Y. Associations among Alcohol Drinking, Smoking, and Nonrestorative Sleep: A Population-Based Study in Japan. Clocks Sleep 2022, 4, 595–606. [Google Scholar] [CrossRef]
- Hattatoğlu, D.G.; Aydin, Ş.; Yildiz, B.P. Does smoking impair sleep hygiene? Arq. Neuro-Psiquiatr. 2021, 79, 1123–1128. [Google Scholar] [CrossRef]
- Oh, S.; Kim, S.; Sung, E.; Kim, C.H.; Kang, J.H.; Shin, H.; Cho, I.Y. The association between cotinine-measured smoking intensity and sleep quality. Tob. Induc. Dis. 2022, 20, 77. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Ma, Y.; Wei, F.; Zhang, L.; Chen, X.; Peng, S.; Xiong, F.; Peng, X.; NiZam, B.; Zou, Y.; et al. Association of active/passive smoking and urinary 1-hydroxypyrene with poor sleep quality: A cross-sectional survey among Chinese male enterprise workers. Tob. Induc. Dis. 2018, 16, 23. [Google Scholar] [CrossRef] [PubMed]
- Gibson, M.; Munafò, M.R.; Taylor, A.E.; Treur, J.L. Evidence for Genetic Correlations and Bidirectional, Causal Effects between Smoking and Sleep Behaviors. Nicotine Tob. Res. 2019, 21, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Metse, A.P.; Clinton-McHarg, T.; Skinner, E.; Yogaraj, Y.; Colyvas, K.; Bowman, J. Associations between Suboptimal Sleep and Smoking, Poor Nutrition, Harmful Alcohol Consumption and Inadequate Physical Activity (‘SNAP Risks’): A Comparison of People with and without a Mental Health Condition in an Australian Community Survey. Int. J. Environ. Res. Public Health 2021, 18, 5946. [Google Scholar] [CrossRef] [PubMed]
- Riera-Sampol, A.; Rodas, L.; Martínez, S.; Moir, H.J.; Tauler, P. Caffeine Intake among Undergraduate Students: Sex Differences, Sources, Motivations, and Associations with Smoking Status and Self-Reported Sleep Quality. Nutrients 2022, 14, 1661. [Google Scholar] [CrossRef] [PubMed]
- Leger, D.; Andler, R.; Richard, J.B.; Nguyen-Thanh, V.; Collin, O.; Chennaoui, M.; Metlaine, A. Sleep, substance misuse and addictions: A nationwide observational survey on smoking, alcohol, cannabis and sleep in 12,637 adults. J. Sleep Res. 2022, 31, e13553. [Google Scholar] [CrossRef] [PubMed]
- Hussain, J.; Ling, L.; Alonzo, R.T.; Rodrigues, R.; Nicholson, K.; Stranges, S.; Anderson, K.K. Associations between sleep patterns, smoking, and alcohol use among older adults in Canada: Insights from the Canadian Longitudinal Study on Aging (CLSA). Addict. Behav. 2022, 132, 107345. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.D.; Harrison, G.A.; Hiorns, R.W. Association between smoking and drinking and sleep duration. Ann. Hum. Biol. 1980, 7, 103–107. [Google Scholar] [CrossRef]
- Manzar, M.D.; Salahuddin, M.; Alamri, M.; Maru, T.T.; Pandi-Perumal, S.R.; Bahammam, A.S. Poor sleep in concurrent users of alcohol, khat, and tobacco smoking in community-dwelling Ethiopian adults. Ann. Thorac. Med. 2018, 13, 220–225. [Google Scholar] [CrossRef]
- Masood, S.; Cappelli, C.; Li, Y.; Tanenbaum, H.; Chou, C.P.; Spruijt-Metz, D.; Palmer, P.H.; Johnson, C.A.; Xie, B. Cigarette smoking is associated with unhealthy patterns of food consumption, physical activity, sleep impairment, and alcohol drinking in Chinese male adults. Int. J. Public Health 2015, 60, 891–899. [Google Scholar] [CrossRef]
- Chang, L.Y.; Chang, H.Y.; Wu, W.C.; Lin, L.N.; Wu, C.C.; Yen, L.L. Dual Trajectories of Sleep Duration and Cigarette Smoking during Adolescence: Relation to Subsequent Internalizing Problems. J. Abnorm. Child Psychol. 2018, 46, 1651–1663. [Google Scholar] [CrossRef]
- Sabatier, T.; Kousignian, I.; Gomajee, R.; Barry, K.; Melchior, M.; Mary-Krause, M. Association between Sleep Disturbances During Childhood and Smoking Trajectories During Adulthood: The Longitudinal TEMPO Cohort Study. Behav. Sleep Med. 2023, 21, 556–569. [Google Scholar] [CrossRef]
- Oshri, A.; Kogan, S.; Liu, S.; Sweet, L.; Mackillop, J. Pathways Linking Adverse Childhood Experiences to Cigarette Smoking among Young Black Men: A Prospective Analysis of the Role of Sleep Problems and Delayed Reward Discounting. Ann. Behav. Med. 2017, 51, 890–898. [Google Scholar] [CrossRef]
- Patterson, F.; Grandner, M.A.; Lozano, A.; Satti, A.; Ma, G. Transitioning from adequate to inadequate sleep duration associated with higher smoking rate and greater nicotine dependence in a population sample. Addict. Behav. 2018, 77, 47–50. [Google Scholar] [CrossRef]
- Hamidovic, A.; de Wit, H. Sleep deprivation increases cigarette smoking. Pharmacol. Biochem. Behav. 2009, 93, 263–269. [Google Scholar] [CrossRef]
- Kageyama, T.; Kobayashi, T.; Nishikido, N.; Oga, J.; Kawashima, M. Associations of sleep problems and recent life events with smoking behaviors among female staff nurses in Japanese hospitals. Ind. Health 2005, 43, 133–141. [Google Scholar] [CrossRef][Green Version]
- Nair, U.S.; Haynes, P.; Collins, B.N. Baseline sleep quality is a significant predictor of quit-day smoking self-efficacy among low-income treatment-seeking smokers. J. Health Psychol. 2019, 24, 1484–1493. [Google Scholar] [CrossRef]
- Chen, H.; Bo, Q.G.; Jia, C.X.; Liu, X. Sleep Problems in Relation to Smoking and Alcohol Use in Chinese Adolescents. J. Nerv. Ment. Dis. 2017, 205, 353–360. [Google Scholar] [CrossRef]
- Fillo, J.; Alfano, C.A.; Paulus, D.J.; Smits, J.A.; Davis, M.L.; Rosenfield, D.; Marcus, B.H.; Church, T.S.; Powers, M.B.; Otto, M.W.; et al. Emotion dysregulation explains relations between sleep disturbance and smoking quit-related cognition and behavior. Addict. Behav. 2016, 57, 6–12. [Google Scholar] [CrossRef]
- Kim, K.S.; Kim, J.H.; Park, S.Y.; Won, H.R.; Lee, H.J.; Yang, H.S.; Kim, H.J. Smoking induces oropharyngeal narrowing and increases the severity of obstructive sleep apnea syndrome. J. Clin. Sleep Med. 2012, 8, 367–374. [Google Scholar] [CrossRef]
- Dülger, S.; Çapkur, Ç.; Gençay, S.; Özmen, S.; Solmaz, F.; Şengören Dikiş, Ö.; Yıldız, T. The relationship between nasal mucociliary clearance time and the degree of smoking dependence in smokers with obstructive sleep apnea syndrome. Adv. Respir. Med. 2021, 89, 353–358. [Google Scholar] [CrossRef]
- Virkkula, P.; Bachour, A.; Hytönen, M.; Malmberg, H.; Salmi, T.; Maasilta, P. Patient- and bed partner-reported symptoms, smoking, and nasal resistance in sleep-disordered breathing. Chest 2005, 128, 2176–2182. [Google Scholar] [CrossRef]
- Jang, Y.S.; Nerobkova, N.; Hurh, K.; Park, E.C.; Shin, J. Association between smoking and obstructive sleep apnea based on the STOP-Bang index. Sci. Rep. 2023, 13, 9085. [Google Scholar] [CrossRef]
- Zhang, Q.; Yang, Z.W.; He, Q.Y.; Xing, Z.L.; Pang, G.F.; Wu, R.Q.; Yang, L.Y.; Sun, L.X.; Han, F.; Wang, Y.; et al. Epidemiologic study on the relationship between smoking and sleep apnea/hypopnea syndrome. Zhonghua Liu Xing Bing Xue Za Zhi 2007, 28, 841–843. [Google Scholar]
- Wetter, D.W.; Young, T.B.; Bidwell, T.R.; Badr, M.S.; Palta, M. Smoking as a risk factor for sleep-disordered breathing. Arch. Intern. Med. 1994, 154, 2219–2224. [Google Scholar] [CrossRef]
- Kashyap, R.; Hock, L.M.; Bowman, T.J. Higher prevalence of smoking in patients diagnosed as having obstructive sleep apnea. Sleep Breath. 2001, 5, 167–172. [Google Scholar] [CrossRef]
- Cohen, O.; Strizich, G.M.; Ramos, A.R.; Zee, P.C.; Reid, K.J.; Mani, V.; Rapoport, D.M.; Redline, S.; Kaplan, R.C.; Shah, N.A. Sex Differences in the Association between Smoking and Sleep-Disordered Breathing in the Hispanic Community Health Study/Study of Latinos. Chest 2019, 156, 944–953. [Google Scholar] [CrossRef]
- Esen, A.D.; Akpinar, M. Relevance of obstructive sleep apnea and smoking: Obstructive sleep apnea and smoking. Fam. Pract. 2021, 38, 181–186. [Google Scholar] [CrossRef]
- Oțelea, M.R.; Trenchea, M.; Rașcu, A.; Antoniu, S.; Zugravu, C.; Busnatu, Ș.; Simionescu, A.A.; Arghir, O.C. Smoking Obstructive Sleep Apnea: Arguments for a Distinctive Phenotype and a Personalized Intervention. J. Pers. Med. 2022, 12, 293. [Google Scholar] [CrossRef]
- Varol, Y.; Anar, C.; Tuzel, O.E.; Guclu, S.Z.; Ucar, Z.Z. The impact of active and former smoking on the severity of obstructive sleep apnea. Sleep Breath. 2015, 19, 1279–1284. [Google Scholar] [CrossRef]
- Bielicki, P.; Trojnar, A.; Sobieraj, P.; Wąsik, M. Smoking status in relation to obstructive sleep apnea severity (OSA) and cardiovascular comorbidity in patients with newly diagnosed OSA. Adv. Respir. Med. 2019, 87, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Boussoffara, L.; Boudawara, N.; Sakka, M.; Knani, J. Smoking habits and severity of obstructive sleep apnea hypopnea syndrome. Rev. Mal. Respir. 2013, 30, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Porebska, I.; Kosacka, M.; Choła, J.; Gładka, A.; Wnek, P.; Brzecka, A.; Renata, J. Smoking among patients with obstructive sleep apnea syndrome—Preliminary report. Pol. Merkur. Lek. 2014, 37, 265–268. [Google Scholar]
- Shao, C.; Qi, H.; Fang, Q.; Tu, J.; Li, Q.; Wang, L. Smoking history and its relationship with comorbidities in patients with obstructive sleep apnea. Tob. Induc. Dis. 2020, 18, 56. [Google Scholar] [CrossRef] [PubMed]
- Mauries, S.; Bertrand, L.; Frija-Masson, J.; Benzaquen, H.; Kalamarides, S.; Sauvage, K.; Lejoyeux, M.; d’Ortho, M.P.; Geoffroy, P.A. Effects of smoking on sleep architecture and ventilatory parameters including apneas: Results of the Tab-OSA study. Sleep Med. X 2023, 6, 100085. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, W.; Zhou, J.; Wei, Z.; Li, X.; Xu, J.; Zhang, F.; Wang, W. Smoking and sleep apnea duration mediated the sex difference in daytime sleepiness in OSA patients. Sleep Breath. 2021, 25, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Casasola, G.G.; Alvarez-Sala, J.L.; Marques, J.A.; Sánchez-Alarcos, J.M.; Tashkin, D.P.; Espinós, D. Cigarette smoking behavior and respiratory alterations during sleep in a healthy population. Sleep Breath. 2002, 6, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Conway, S.G.; Roizenblatt, S.S.; Palombini, L.; Castro, L.S.; Bittencourt, L.R.; Silva, R.S.; Tufik, S. Effect of smoking habits on sleep. Braz. J. Med. Biol. Res. 2008, 41, 722–727. [Google Scholar] [CrossRef] [PubMed]
- Hoflstein, V. Relationship between smoking and sleep apnea in clinic population. Sleep 2002, 25, 519–524. [Google Scholar]
- Ben Amar, J.; Ben Mansour, A.; Zaibi, H.; Ben Safta, B.; Dhahri, B.; Aouina, H. Impact of smoking on the severity of Obstructive Sleep Apnea Hypopnea Syndrome. Tunis. Medicale 2018, 96, 477–482. [Google Scholar]
- Suzgun, M.A.; Kabeloglu, V.; Senel, G.B.; Karadeniz, D. Smoking Disturbs the Beneficial Effects of Continuous Positive Airway Pressure Therapy on Leptin Level in Obstructive Sleep Apnea. J. Obes. Metab. Syndr. 2023, 32, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Yi, H.; Guan, J.; Zou, J.; Xu, H.; Liu, Y. Effect of smoking on glucose, lipid metabolism and sleep structure in postoperative patients with obstructive sleep apnea. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2021, 35, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wu, J.; Li, S.; Yu, W.; Zhu, H.; Wang, Y.; Li, Y. Smoking, Coffee Consumption, Alcohol Intake, and Obstructive Sleep Apnea: A Mendelian Randomization Study. Curr. Neurovasc. Res. 2023, 20, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Eskici İlgin, V.; Yayla, A.; Karaman Özlü, Z.; Özlü, İ.; Toraman, R.L.; Toraman, M.M. Pain, Sleep Disturbance and Smoking among Patients with Covid-19 Presenting to the Emergency Department. Florence Nightingale J. Nurs. 2023, 31, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Stipelman, B.A.; Augustson, E.; McNeel, T. The relationship among smoking, sleep, and chronic rheumatic conditions commonly associated with pain in the National Health Interview Survey. J. Behav. Med. 2013, 36, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Fucito, L.M.; Redeker, N.S.; Ball, S.A.; Toll, B.A.; Ikomi, J.T.; Carroll, K.M. Integrating a Behavioural Sleep Intervention into Smoking Cessation Treatment for Smokers with Insomnia: A Randomised Pilot Study. J. Smok. Cessat. 2014, 9, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Riedel, B.W.; Durrence, H.H.; Lichstein, K.L.; Taylor, D.J.; Bush, A.J. The relation between smoking and sleep: The influence of smoking level, health, and psychological variables. Behav. Sleep Med. 2004, 2, 63–78. [Google Scholar] [CrossRef]
- Kazi, S.E.; Mohammed, J.M.M.; Schenck, C.H. Sleepwalking, sleep-related eating disorder and sleep-related smoking successfully treated with topiramate: A case report. Sleep Sci. 2022, 15, 370–373. [Google Scholar] [CrossRef]
- O’Callaghan, F.; O’Callaghan, M.; Scott, J.G.; Najman, J.; Al Mamun, A. Effect of maternal smoking in pregnancy and childhood on child and adolescent sleep outcomes to 21 years: A birth cohort study. BMC Pediatr. 2019, 19, 70. [Google Scholar] [CrossRef]
- Yahia, N.; Brown, C.; Potter, S.; Szymanski, H.; Smith, K.; Pringle, L.; Herman, C.; Uribe, M.; Fu, Z.; Chung, M.; et al. Night eating syndrome and its association with weight status, physical activity, eating habits, smoking status, and sleep patterns among college students. Eat Weight Disord. 2017, 22, 421–433. [Google Scholar] [CrossRef]
- Kaneita, Y.; Ohida, T.; Takemura, S.; Sone, T.; Suzuki, K.; Miyake, T.; Yokoyama, E.; Umeda, T. Relation of smoking and drinking to sleep disturbance among Japanese pregnant women. Prev. Med. 2005, 41, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Ahlberg, J.; Lobbezoo, F.; Hublin, C.; Piirtola, M.; Kaprio, J. Smoking cessation is not associated with a decline in reported sleep bruxism in middle-aged Finnish twins: Data revisited. J. Oral Rehabil. 2024, 51, 117–118. [Google Scholar] [CrossRef] [PubMed]
- Prosise, G.L.; Bonnet, M.H.; Berry, R.B.; Dickel, M.J. Effects of abstinence from smoking on sleep and daytime sleepiness. Chest 1994, 105, 1136–1141. [Google Scholar] [CrossRef] [PubMed]
- Pataka, A.; Frantzidis, C.; Kalamaras, G.; Gkivogkli, P.; Kotoulas, S.; Nday, C.; Chriskos, P.; Karagianni, M.; Styliadis, C.; Paraskevopoulos, E.; et al. Varenicline administration for smoking cessation may reduce apnea hypopnea index in sleep apnea patients. Sleep Med. 2021, 88, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Staner, L.; Luthringer, R.; Dupont, C.; Aubin, H.J.; Lagrue, G. Sleep effects of a 24-h versus a 16-h nicotine patch: A polysomnographic study during smoking cessation. Sleep Med. 2006, 7, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Sawnani, H.; Jackson, T.; Murphy, T.; Beckerman, R.; Simakajornboon, N. The effect of maternal smoking on respiratory and arousal patterns in preterm infants during sleep. Am. J. Respir. Crit. Care Med. 2004, 169, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.; Colodner, R.; Masalha, R.; Haimov, I. The Relationship between Tobacco Smoking, Cortisol Secretion, and Sleep Continuity. Subst. Use Misuse 2019, 54, 1705–1714. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Samet, J.; Caffo, B.; Punjabi, N.M. Cigarette smoking and nocturnal sleep architecture. Am. J. Epidemiol. 2006, 164, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Aubin, H.J.; Luthringer, R.; Demazières, A.; Dupont, C.; Lagrue, G. Comparison of the effects of a 24-hour nicotine patch and a 16-hour nicotine patch on smoking urges and sleep. Nicotine Tob. Res. 2006, 8, 193–201. [Google Scholar] [CrossRef]
- Salin-Pascual, R.J. Relationship between mood improvement and sleep changes with acute nicotine administration in non-smoking major depressed patients. Rev. Investig. Clin. 2002, 54, 36–40. [Google Scholar]
- Stéphan-Blanchard, E.; Telliez, F.; Léké, A.; Djeddi, D.; Bach, V.; Libert, J.P.; Chardon, K. The influence of in utero exposure to smoking on sleep patterns in preterm neonates. Sleep 2008, 31, 1683–1689. [Google Scholar] [CrossRef]
- Djeddi, D.; Stephan-Blanchard, E.; Léké, A.; Ammari, M.; Delanaud, S.; Lemaire-Hurtel, A.S.; Bach, V.; Telliez, F. Effects of Smoking Exposure in Infants on Gastroesophageal Reflux as a Function of the Sleep-Wakefulness State. J. Pediatr. 2018, 201, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Aldahash, F.D.; Alasmari, S.A.; Alnomsi, S.J.; Alshehri, A.M.; Alharthi, N.F.; Aloufi, A.A.H.; Al Atawi, M.S.; Alotaibi, A.A.; Mirghani, H.O. Relationship of body mass index to sleep duration, and current smoking among medical students in Tabuk City, Saudi Arabia. Electron. Physician 2018, 10, 7273–7278. [Google Scholar] [CrossRef][Green Version]
- Aksu, K.; Firat Güven, S.; Aksu, F.; Ciftci, B.; Ulukavak Ciftci, T.; Aksaray, S.; Sipit, T.; Peker, Y. Obstructive sleep apnoea, cigarette smoking and plasma orexin-A in a sleep clinic cohort. J. Int. Med. Res. 2009, 37, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Gong, S.; Xu, C.; Zhou, J.Y.; Wang, K.S. Sleep duration and smoking are associated with coronary heart disease among US adults with type 2 diabetes: Gender differences. Diabetes Res. Clin. Pract. 2017, 124, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Donovan, L.M.; Feemster, L.C.; Billings, M.E.; Spece, L.J.; Griffith, M.F.; Rise, P.J.; Parsons, E.C.; Palen, B.N.; O’Hearn, D.J.; Redline, S.; et al. Risk of Cardiovascular Disease Related to Smoking Is Greater Among Women with Sleep-Disordered Breathing. J. Clin. Sleep Med. 2018, 14, 1929–1935. [Google Scholar] [CrossRef]
- Lavie, L.; Lavie, P. Smoking interacts with sleep apnea to increase cardiovascular risk. Sleep Med. 2008, 9, 247–253. [Google Scholar] [CrossRef]
- Oliveira, G.; Silva, T.L.N.D.; Silva, I.B.D.; Coutinho, E.S.F.; Bloch, K.V.; Oliveira, E.R.A. Aggregation of cardiovascular risk factors: Alcohol, smoking, excess weight, and short sleep duration in adolescents in the ERICA study. Cad. Saúde Pública 2019, 35, e00223318. [Google Scholar] [CrossRef]
- Blazejová, K.; Sonka, K.; Skodová, Z.; Nevsímalová, S. Prevalence of obesity, hypertension and smoking in patients with the sleep apnea syndrome—Comparison with the Czech population. Cas. Lek. Cesk. 2000, 139, 339–342. [Google Scholar]
- Özkan, E.; Celik, Y.; Yucel-Lindberg, T.; Peker, Y. Current Smoking Determines the Levels of Circulating MPO and MMP-9 in Adults with Coronary Artery Disease and Obstructive Sleep Apnea. J. Clin. Med. 2023, 12, 4053. [Google Scholar] [CrossRef]
- Lui, M.M.; Mak, J.C.; Lai, A.Y.; Hui, C.K.; Lam, J.C.; Lam, D.C.; Ip, M.S. The Impact of Obstructive Sleep Apnea and Tobacco Smoking on Endothelial Function. Respiration 2016, 91, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Javaheri, S.; Shukla, R.; Wexler, L. Association of smoking, sleep apnea, and plasma alkalosis with nocturnal ventricular arrhythmias in men with systolic heart failure. Chest 2012, 141, 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- Wada, K.; Mizuguchi, Y.; Wada, Y.; Ohno, Y.; Iino, Y. Hyperlipidaemia, lack of sleep and smoking as risk factors for proteinuria among high altitude mountain trekkers. Nephrology 2006, 11, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Kirbas, G.; Abakay, A.; Topcu, F.; Kaplan, A.; Unlü, M.; Peker, Y. Obstructive sleep apnoea, cigarette smoking and serum testosterone levels in a male sleep clinic cohort. J. Int. Med. Res. 2007, 35, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Mikolasevic, I.; Domislovic, V.; Filipec Kanizaj, T.; Radic-Kristo, D.; Krznaric, Z.; Milovanovic, T.; Juric, T.; Klapan, M.; Skenderevic, N.; Delija, B.; et al. Relationship between coffee consumption, sleep duration and smoking status with elastographic parameters of liver steatosis and fibrosis; controlled attenuation parameter and liver stiffness measurements. Int. J. Clin. Pract. 2021, 75, e13770. [Google Scholar] [CrossRef] [PubMed]
- Custodio, L.; Carlson, C.R.; Upton, B.; Okeson, J.P.; Harrison, A.L.; de Leeuw, R. The impact of cigarette smoking on sleep quality of patients with masticatory myofascial pain. J. Oral Facial Pain Headache 2015, 29, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Patterson, F.; Connick, E.; Brewer, B.; Grandner, M.A. HIV status and sleep disturbance in college students and relationship with smoking. Sleep Health 2019, 5, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Kokubun, K.; Pineda, J.C.D.; Yamakawa, Y. Unhealthy lifestyles and brain condition: Examining the relations of BMI, living alone, alcohol intake, short sleep, smoking, and lack of exercise with gray matter volume. PLoS ONE 2021, 16, e0255285. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.N.; Zhou, L.N.; Zhang, X.J.; Li, Q.Y.; Wang, Q.; Xu, H.J. Combined effect of obstructive sleep apnea and chronic smoking on cognitive impairment. Sleep Breath. 2016, 20, 51–59. [Google Scholar] [CrossRef]
- Nakamura, M.; Aoki, N.; Nakashima, T.; Hoshino, T.; Yokoyama, T.; Morioka, S.; Kawamura, T.; Tanaka, H.; Hashimoto, T.; Ohno, Y.; et al. Smoking, alcohol, sleep and risk of idiopathic sudden deafness: A case-control study using pooled controls. J. Epidemiol. 2001, 11, 81–86. [Google Scholar] [CrossRef]
- Hahad, O.; Beutel, M.; Gilan, D.A.; Michal, M.; Schulz, A.; Pfeiffer, N.; König, J.; Lackner, K.; Wild, P.; Daiber, A.; et al. The association of smoking and smoking cessation with prevalent and incident symptoms of depression, anxiety, and sleep disturbance in the general population. J. Affect. Disord. 2022, 313, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Miadich, S.A.; Everhart, R.S.; Heron, K.E.; Cobb, C.O. Medication use, sleep, and caregiver smoking status among urban children with asthma. J. Asthma 2018, 55, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Özden Mat, D.; Firat, S.; Aksu, K.; Aksu, F.; Duyar, S.Ş. Obstructive sleep apnea is a determinant of asthma control independent of smoking, reflux, and rhinitis. Allergy Asthma Proc. 2021, 42, e25–e29. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.X.; Liu, L.Y.; Xiang, Y.J.; Wang, F.; Zhou, F.; Huang, S.Y.; Zheng, C.; Ye, C.M.; Zhou, W.Z.; Yin, G.S.; et al. XRCC5/6 polymorphisms and their interactions with smoking, alcohol consumption, and sleep satisfaction in breast cancer risk: A Chinese multi-center study. Cancer Med. 2021, 10, 2752–2762. [Google Scholar] [CrossRef] [PubMed]
- Teni, M.T.; Loux, T.; Sebert Kuhlmann, A. Racial disparity in gestational diabetes mellitus and the association with sleep-disordered breathing and smoking cigarettes: A cross-sectional study. J. Matern.-Fetal Neonatal Med. 2022, 35, 10601–10607. [Google Scholar] [CrossRef] [PubMed]
- Ohida, T.; Kaneita, Y.; Osaki, Y.; Harano, S.; Tanihata, T.; Takemura, S.; Wada, K.; Kanda, H.; Hayashi, K.; Uchiyama, M. Is passive smoking associated with sleep disturbance among pregnant women? Sleep 2007, 30, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Stone, K.C. Postpartum Behavioral Sleep Intervention for Smoking Relapse Prevention: A Pilot Trial. Matern. Child Health J. 2023, 27, 272–285. [Google Scholar] [CrossRef] [PubMed]
- Hannan, K.E.; Smith, R.A.; Barfield, W.D.; Hwang, S.S. Association between Neonatal Intensive Care Unit Admission and Supine Sleep Positioning, Breastfeeding, and Postnatal Smoking among Mothers of Late Preterm Infants. J. Pediatr. 2020, 227, 114–120.e1. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.S.; Ferens, D.; Watts, A.M.; Vitkovic, J.; Lacey, B.; Andrew, S.; Cranage, S.M.; Chau, B.; Greaves, R.; Adamson, T.M. Effects of maternal tobacco smoking, sleeping position, and sleep state on arousal in healthy term infants. Arch. Dis. Child.-Fetal Neonatal Ed. 2002, 87, F100–F105. [Google Scholar] [CrossRef]
- Nelson, E.A.; Taylor, B.J. International Child Care Practices Study: Infant sleep position and parental smoking. Early Hum. Dev. 2001, 64, 7–20. [Google Scholar] [CrossRef]
- Anderson, M.E.; Johnson, D.C.; Batal, H.A. Sudden Infant Death Syndrome and prenatal maternal smoking: Rising attributed risk in the Back to Sleep era. BMC Med. 2005, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Tirosh, E.; Libon, D.; Bader, D. The effect of maternal smoking during pregnancy on sleep respiratory and arousal patterns in neonates. J. Perinatol. 1996, 16, 435–438. [Google Scholar]
- Peltier, M.R.; Lee, J.; Ma, P.; Businelle, M.S.; Kendzor, D.E. The influence of sleep quality on smoking cessation in socioeconomically disadvantaged adults. Addict. Behav. 2017, 66, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Buechele, G.; Weiland, S.K. Sleep duration and smoking cessation in student nurses. Addict. Behav. 2007, 32, 1505–1510. [Google Scholar] [CrossRef]
- Farris, S.G.; Matsko, S.V.; Uebelacker, L.A.; Brown, R.A.; Price, L.H.; Abrantes, A.M. Anxiety sensitivity and daily cigarette smoking in relation to sleep disturbances in treatment-seeking smokers. Cogn. Behav. Ther. 2020, 49, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Arzi, A.; Holtzman, Y.; Samnon, P.; Eshel, N.; Harel, E.; Sobel, N. Olfactory aversive conditioning during sleep reduces cigarette-smoking behavior. J. Neurosci. 2014, 34, 15382–15393. [Google Scholar] [CrossRef]
- Okun, M.L.; Levine, M.D.; Houck, P.; Perkins, K.A.; Marcus, M.D. Subjective sleep disturbance during a smoking cessation program: Associations with relapse. Addict. Behav. 2011, 36, 861–864. [Google Scholar] [CrossRef][Green Version]
- Ashare, R.L.; Lerman, C.; Tyndale, R.F.; Hawk, L.W.; George, T.P.; Cinciripini, P.; Schnoll, R.A. Sleep Disturbance During Smoking Cessation: Withdrawal or Side Effect of Treatment? J. Smok. Cessat. 2017, 12, 63–70. [Google Scholar] [CrossRef]
- Wolter, T.D.; Hauri, P.J.; Schroeder, D.R.; Wisbey, J.A.; Croghan, I.T.; Offord, K.P.; Dale, L.C.; Hurt, R.D. Effects of 24-hr nicotine replacement on sleep and daytime activity during smoking cessation. Prev. Med. 1996, 25, 601–610. [Google Scholar] [CrossRef]
- Ghotbi, N.; Rabenstein, A.; Pilz, L.K.; Rüther, T.; Roenneberg, T. Chronotype, Social Jetlag, and Nicotine Use. J. Biol. Rhythms 2023, 38, 392–406. [Google Scholar] [CrossRef]
| Reference | Studies’ Main Findings |
|---|---|
| Soldatos CR et al. 1980 [19] Delasnerie-Laupretre N, et al. 1993 [20] Wetter DW et al. 1994 [21] Phillips BA et al. 1995 [22] Bale P et al. 1982 [23] Lexcen FJ et al. 1993 [24] | The last five decades, these studies had correlated smoking with various aspects of poor sleep quality, such as difficulty in initiating sleep, staying asleep and waking up, nightmares, snoring, excessive daytime sleepiness and minor accidents. Sleep duration was inversely correlated with smoking even in athletes, whilst the effects of smoking on sleep were partly attributed to the fact that smokers consume greater quantities of caffeine and alcohol as well. |
| Patten CA et al. 2000 [25] | Cigarette smoking status showed a dose–response relationship with development of sleep problems, frequent sleep problems and with persisting frequent sleep problems. |
| Jaehne A et al. 2012 [26] Liu JT et al. 2013 [27] Liu Y et al. 2020 [28] Woo DH et al. 2023 [1] Hwang JH et al. 2022 [30] Al-Mshari A et al. 2022 [31] Li H et al. 2020 [32] | Pittsburgh Sleep Quality Index (PSQI) scores were persistently higher in smokers compared to non-smokers, in both males and females, even after controlling for psychological factors, while a quantitative relation between sleep disturbance and smoking with significantly longer sleep latency in heavy smokers compared to non-smokers, also existed. |
| Peters EN et al. 2011 [29] | Individuals who both wake during the night to smoke and report clinically significant sleep disturbance represent a high-risk group of smokers. |
| Purani H et al. 2019 [4] | Poorer sleep quality was associated with increased withdrawal, craving and total smoking urges. |
| Bellatorre A et al. 2017 [33] Nuñez A et al. 2021 [6] Sahlin C et al. 2009 [34] McNamara JP et al. 2014 [35] Mak KK et al. 2010 [36] Mehari A et al. 2014 [37] Merianos AL et al. 2023 [38] Sujarwoto S et al. 2020 [39] AlRyalat SA et al. 2021 [40] Nasri O et al. 2021 [41] Banna MHA et al. 2023 [42] Nakata A et al. 2023 [43] Sabanayagam C et al. 2011 [44] | Apart from the PSQI, there are also other sleep parameters that present deterioration with smoking, such as difficulty in falling and staying asleep, longer sleep latency, shorter sleep time, often in a dose-dependent manner, or after second-hand smoke exposure. |
| Bilsky SA et al. 2016 [45] Bar-Zeev Y et al. 2023 [46] Merikanto I et al. 2017 [17] Patterson F et al. 2016 [47] Parkes KR. 2002 [48] | Other factors that seem to intervene in the relationship between smoking and sleep disturbances are stress, especially during stressful occasions like a pandemic, late chronotypes and night shiftwork. |
| Otsuka Y et al. 2022 [49] Hattatoğlu DG et al. 2021 [50] | These studies have not identified a relationship between smoking and sleep quality, apart from indirect confounding factors or effects in sleep hygiene. |
| Oh S et al. 2022 [51] Zhou B et al. 2018 [52] Gibson M et al. 2019 [53] | These studies have identified a significant relationship between smoking and sleep quality, by using biochemical or genetic examinations. |
| Metse AP et al. 2021 [54] Riera-Sampol A et al. 2022 [55] Leger D et al. 2022 [56] Hussain J et al. 2022 [57] Palmer CD et al. 1980 [58] Manzar MD et al. 2018 [59] Masood S et al. 2015 [60] | Another aspect in the relationship between smoking and poor sleep quality is their common effect on other unhealthy habits such as bad nutrition, caffeine intake, alcohol consumption, illicit drug usage and lack of physical activity. |
| Chang LY et al. 2018 [61] Sabatier T et al. 2023 [62] Oshri A et al. 2017 [63] | Studies that investigated the relationship between sleep problems in adolescence and subsequent smoking trajectories have resulted in conflicting evidence. |
| Patterson F et al. 2018 [64] Hamidovic A et al. 2009 [65] Kageyama T et al. 2005 [66] Nair US et al. 2019 [67] Chen H et al. 2017 [68] Fillo J et al. 2016 [69] | Sleep deprivation or a transition from adequate to inadequate sleep causes increased tobacco cigarette consumption, probably due to the expectance that nicotine might reduce subjective sleepiness, thus smoking cessation programs should target smokers with poor sleep and promote interventions in this direction. |
| Reference | Studies’ Main Findings |
|---|---|
| Kim KS et al. 2012 [70] Dülger S et al. 2021 [71] Virkkula P et al. 2005 [72] | Smoking might contribute to the pathogenesis of obstructive sleep apnea (OSA) through the increased thickness and edema of the uvular mucosa lamina propria and the increased total nasal resistance in a supine position in smokers. |
| Jang YS et al. 2023 [73] Zhang Q et al. 2007 [74] Wetter DW et al. 1994 [75] Kashyap R et al. 2001 [76] | Smokers present a higher odds ratio in a dose-dependent way for sleep-disordered breathing or OSA, adjusted for confounders such as age, sex, body mass index (BMI) and alcohol. |
| Ioannidou D et al. 2021 [13] Cohen O et al. 2019 [77] Esen AD et al. 2021 [78] | Smoking was not related to the prevalence of OSA, when adjusted for covariates, apart from in younger females or in patients with BMI < 30. |
| Yosunkaya S et al. 2021 [5] Grigoriou I et al. 2023 [7] Oțelea MR et al. 2022 [79] Varol Y et al. 2015 [80] Bielicki P et al. 2019 [81] Boussoffara L et al. 2013 [82] Porebska I et al. 2014 [83] Shao C et al. 2020 [84] Mauries S et al. 2023 [85] Wang X et al. 2021 [86] Casasola GG et al. 2002 [87] Conway SG et al. 2008 [88] Hoflstein V. 2002 [89] Ben Amar J et al. 2018 [90] Suzgun MA et al. 2023 [91] | Current smokers present OSA earlier and more severly with worse oxygen desaturation index (ODI), mean and minimum SaO2, total sleep time and sleep time ratio with SaO2 below 90%, mean apnea duration, nocturnal hypoxia index and COHb levels and the Epworth sleepiness scale (ESS), while the evidence for the relationship between smoking and apnea–hypopnea index (AHI) are conflicting with some studies showing a dose-dependent relationship, while others showing no relationship. |
| Zhu H et al. 2021 [92] | The postoperative improvement of sleep structure in non-smoking OSA patients was better than smokers. |
| Yang Y et al. 2023 [93] | Smoking initiation was associated with increased risk of OSA, while never smoking was associated with decreased risk of OSA. |
| Reference | Studies’ Main Findings |
|---|---|
| Nuñez A et al. 2021 [6] Kageyama T et al. 2005 [66] Eskici İlgin V et al. 2023 [94] Stipelman BA et al. 2013 [95] Hussain J et al. 2022 [57] Leger D et al. 2022 [56] Fucito LM et al. 2014 [96] Mak KK et al. 2010 [36] Riedel BW et al. 2004 [97] Gibson M et al. 2019 [53] | Compared to non-smoking, smoking was associated with experiencing increased insomnia, while night-time smoking was significantly associated with greater insomnia and shorter sleep duration with a dose-dependent manner in night shiftworkers, in patients with chronic pain and rheumatic diseases or during the pandemic, with or without alcohol consumption, after controlling for covariates or in genetic studies, while smoking cessation counseling improved insomnia symptoms. |
| Provini F et al. 2008 [8] Kazi SE et al. 2022 [98] O’Callaghan F et al. 2019 [99] Yahia N et al. 2017 [100] Grigoriou I et al. 2023 [7] | Smoking was related to various types of parasomnia such as compulsive eating disorder and compulsive smoking during sleep, sleepwalking, sleeptalking, nightmares, abnormal movements and restless sleep. |
| Jaehne A et al. 2012 [26] Kaneita Y et al. 2005 [101] Lavigne GL et al. 1997 [10] Frosztega W et al. 2022 [9] Ahlberg J et al. 2024 [102] | The evidence on the relationship between smoking and restless legs syndrome or bruxism is conflicting, with some studies showing worsening, and others showing no connection. |
| Conway SG et al. 2008 [88] Prosise GL et al. 1994 [103] Pataka A et al. 2021 [104] Staner L et al. 2006 [105] Sawnani H et al. 2004 [106] | The arousal index was significantly increased in current and former smokers and decreased in maternal smoking infants, while relative arousals were also increased in smokers who abstained from smoking or received treatment for smoking cessation. |
| Reference | Studies’ Main Findings |
|---|---|
| Truong MK et al. 2021 [3] | Current smokers had lower delta power in non-rapid eye movement (REM) sleep and higher alpha power compared with never smokers. |
| Cohen A et al. 2019 [107] | Smoking is associated with reduced sleep continuity, something that may involve the hypothalamic–pituitary–adrenocortical axis. |
| Yosunkaya S et al. 2021 [5] Varol Y et al. 2015 [80] Mauries S et al. 2023 [85] Zhang L et al. 2006 [108] | The N3 stage or slow-wave sleep is decreased in smokers, while the N1 and N2 stages are increased, changes that seem to be dose dependent, as they are more evident in heavy smokers compared to mild smokers, or in current smokers compared to former smokers. |
| Jaehne A et al. 2012 [26] | Smokers had a shorter sleep period time and higher REM sleep density than non-smokers. |
| Prosise GL et al. 1994 [103] | The multiple sleep latency tests latency to stage 1 sleep decreased during smoking cessation. |
| Staner L et al. 2006 [105] Aubin HJ et al. 2006 [109] Salin-Pascual RJ. 2002 [110] | Nicotine patches, especially the 24 h compared to the 16 h ones, significantly increase the proportion of slow-wave sleep, REM density and REM beta activities, while decreasing REM latency and N2 sleep stage duration. |
| Pataka A et al. 2021 [104] | No significant differences were observed in sleep macro architecture treatment with Varenicline apart from prolongation of N2 and N3 latency in smokers. |
| Zhu H et al. 2021 [92] | Postoperative smoking was associated with worse sleep structure. |
| Stéphan-Blanchard E, et al. 2008 [111] | Neonates born to heavy-smoking mothers displayed disturbed sleep structure and continuity, higher proportion of active sleep and lower proportion of quiet sleep. |
| Djeddi D et al. 2018 [112] | Gastroesophageal reflux associated with smoking exposure was particularly obvious during REM sleep. |
| Reference | Studies’ Main Findings |
|---|---|
| Alsulami S et al. 2023 [11] Aldahash FD et al. 2018 [113] Suzgun MA et al. 2023 [91] Aksu K et al. 2009 [114] | Obesity is positively correlated with the number of cigarettes and negatively correlated with sleep duration, smoking acts as a predisposing factor to leptin resistance in OSA patients, increasing its secretion, while orexin-A levels are significantly lower in smokers with OSA compared to ex- or current smokers. |
| Frosztega W et al. 2022 [9] Zhu H et al. 2017 [12] Ioannidou D et al. 2021 [13] Bielicki P et al. 2019 [81] Porebska I et al. 2014 [83] Li L et al. 2017 [115] Donovan LM et al. 2018 [116] Lavie L et al. 2008 [117] Oliveira G et al. 2019 [118] Blazejova K et al. 2000 [119] Zhu H et al. 2021 [92] | The co-existence of OSA or short sleep duration with smoking was related to metabolic diseases such as resistance to insulin or type II diabetes mellitus, increased triglycerides, increased low-density lipoprotein (LDL) cholesterol and decreased high-density lipoprotein (HDL) cholesterol levels and also with cardiovascular diseases such as hypertension and coronary artery disease. |
| Özkan E et al. 2023 [120] Lui MM et al. 2016 [121] Javaheri S et al. 2012 [122] | An oxidative stress marker, a plaque destabilizer and peripheral artery tonometry quantify endothelial dysfunction, while nocturnal vevtricular arrythmias might be proved fatal in smokers with OSA and coronary artery disease. |
| Yosunkaya S et al. 2021 [5] Wada K et al. 2006 [123] Cohen A et al. 2019 [107] Kirbas G et al. 2007 [124] Mikolasevic I et al. 2021 [125] | Poor sleep combined with smoking increase hemoglobulin (Hb) and along with hyperlipidemia are risk factors for proteinuria. They are related to lower levels of iron and magnesium and increased cortisol levels. However, sleep, but not smoking, is related to serum testosterone levels and liver steatosis. |
| Li H et al. 2020 [32] Liu Y et al. 2020 [28] | Poor sleep and smoking combined is associated with higher levels of dopamine and TNF-α in celebrospinal fluid. |
| Custodio L et al. 2015 [126] Stipelman BA et al. 2013 [95] Eskici İlgin V et al. 2023 [94] Bar-Zeev Y et al. 2023 [46] Patterson F et al. 2019 [127] Kokubun K et al. 2021 [128] Hu M et al. 2019 [15] Liu JT et al. 2013 [27] Lin YN et al. 2016 [129] Nakamura M et al. 2001 [130] | Smoking and poor sleep quality are related to masticatory myofascial pain, or pain related to rheumatic diseases, lower grey matter brain volume and several neurological defects, such as mild cognitive impairment, memory problems and even sudden deafness, or COVID-19 and HIV complications. |
| Metse AP et al. 2013 [54] Phillips BA et al. 1995 [22] Bilsky SA et al. 2016 [45] Hattatoğlu DG et al. 2021 [50] Hahad O et al. 2022 [131] He M et al. 2023 [16] Salin-Pascual RJ. 2002 [110] Leger D et al. 2022 [56] | Smoking combined with poor sleep quality have been associated with mental health problems such as anxiety, depression and bipolar disorder, while they have also been related to substance misuse, such as cannabis. |
| Miadich SA et al. 2018 [132] Özden Mat D et al. 2021 [133] Zhang W et al. 2023 [14] Oțelea MR et al. 2022 [79] Ben Amar J et al. 2018 [90] | Smoking and poor sleep quality are related to asthma control, while in chronic obstructive pulmonary disease (COPD), smoking-related airway inflammation is characterized by higher levels of exhaled CO and H2S and lower levels of NO, which consequently augments the effect of ozone on SpO2 during sleep. Also, patients with OSA who smoke have worse respiratory function and present more frequently with COPD. |
| Yu LX et al. 2021 [134] Teni MT et al. 2022 [135] Merikanto I et al. 2017 [17] Kaneita Y et al. 2005 [101] Ohida T et al. 2007 [136] Stone KC. 2023 [137] | Smoking and sleep quality combined are not related to breast cancer; however, they are related, even with passive smoking, to several problems in pregnant women such as gestational diabetes, difficulty in initiating or maintaining sleep, short sleep duration, insufficient sleep, poor sleep quality early-morning awakening, excessive daytime sleepiness and restless legs syndrome, while postpartum interventions in sleep prevent smoking relapse. |
| Mennella JA et al. 2007 [18] Stéphan-Blanchard E et al. 2008 [111] Djeddi D et al. 2018 [112] Hannan KE et al. 2020 [138] O’Callaghan F et al. 2019 [99] Sawnani H et al. 2004 [106] Horne RS et al. 2002 [139] Nelson EA et al. 2001 [140] Anderson ME et al. 2005 [141] Tirosh E et al. 1996 [142] | Infants of smoking mothers sleep less, with lower proportion of quiet sleep, more wakefulness after sleep onset, more body movements and more disturbed sleep. They also have increased risk of gastroesophageal reflux (GER) during REM sleep, neonatal intensive care unit admission, adolescent parasomnias, or other sleep problems in general, while maternal smoking along with supine sleep position are risk factors for sudden infant death syndrome. |
| Reference | Studies’ Main Findings |
|---|---|
| Peltier MR et al. 2017 [143] Rapp K et al. 2007 [144] Gibson M et al. 2019 [53] | Sleep duration is positively associated with smoking cessation, while insomnia decreases the odds of successful smoking cessation. |
| Riemerth A et al. 2009 [2] Purani H et al. 2019 [4] Prosise GL et al. 1994 [103] Fillo J et al. 2016 [69] Hahad O et al. 2022 [131] Farris SG et al. 2020 [145] Arzi A et al. 2014 [146] Nair US et al. 2019 [67] Stone KC. 2023 [137] Fucito LM et al. 2014 [96] Okun ML et al. 2011 [147] Ashare RL et al. 2017 [148] | Heavy smokers often suffer from nocturnal nicotine craving, while poor sleep quality during smoking cessation efforts leads to increased withdrawal, craving, irritability, anxiety, tension and smoking urges. Sleep disorders are considered withdrawal symptoms during smoking cessation, while emotional disturbances such as anxiety and depression are common in those who experience poor sleep quality during smoking cessation and might be a target for cognitive behavioral treatment. |
| Ahlberg J et al. 2024 [102] | Smoking cessation is not associated with a decline in reported sleep bruxism. |
| Pataka A et al. 2021 [104] | Varenicline treatment worsened sleep quality as a prolongation of sleep latency, N2 and N3 latency was observed. |
| Staner L et al. 2006 [105] Aubin HJ et al. 2006 [109] Wolter TD et al. 1996 [149] | The 24 h nicotine patch, compared to the 16 h one, improved sleep quality and decreased smoking urges. |
| Ghotbi N et al. 2023 [150] | Smoking may be a consequence of, rather than a cause, for social jetlag, while daytime sleepiness is a significant predictor of outcome, but did not improve with cessation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grigoriou, I.; Kotoulas, S.-C.; Porpodis, K.; Spyratos, D.; Papagiouvanni, I.; Tsantos, A.; Michailidou, A.; Mourelatos, C.; Mouratidou, C.; Alevroudis, I.; et al. The Interactions between Smoking and Sleep. Biomedicines 2024, 12, 1765. https://doi.org/10.3390/biomedicines12081765
Grigoriou I, Kotoulas S-C, Porpodis K, Spyratos D, Papagiouvanni I, Tsantos A, Michailidou A, Mourelatos C, Mouratidou C, Alevroudis I, et al. The Interactions between Smoking and Sleep. Biomedicines. 2024; 12(8):1765. https://doi.org/10.3390/biomedicines12081765
Chicago/Turabian StyleGrigoriou, Ioanna, Serafeim-Chrysovalantis Kotoulas, Konstantinos Porpodis, Dionysios Spyratos, Ioanna Papagiouvanni, Alexandros Tsantos, Anastasia Michailidou, Constantinos Mourelatos, Christina Mouratidou, Ioannis Alevroudis, and et al. 2024. "The Interactions between Smoking and Sleep" Biomedicines 12, no. 8: 1765. https://doi.org/10.3390/biomedicines12081765
APA StyleGrigoriou, I., Kotoulas, S.-C., Porpodis, K., Spyratos, D., Papagiouvanni, I., Tsantos, A., Michailidou, A., Mourelatos, C., Mouratidou, C., Alevroudis, I., Marneri, A., & Pataka, A. (2024). The Interactions between Smoking and Sleep. Biomedicines, 12(8), 1765. https://doi.org/10.3390/biomedicines12081765









