Diagnostic Value of Fasting and Bedtime Saliva Pepsin Measurements in Laryngopharyngeal Reflux
Abstract
1. Introduction
2. Material and Methods
2.1. Subjects and Setting
2.2. Hypopharyngeal–Esophageal Multichannel Intraluminal Impedance-pH Monitoring
2.3. Saliva Pepsin Measurement
2.4. Demographics, Symptoms, and Signs
3. Statistical Methods
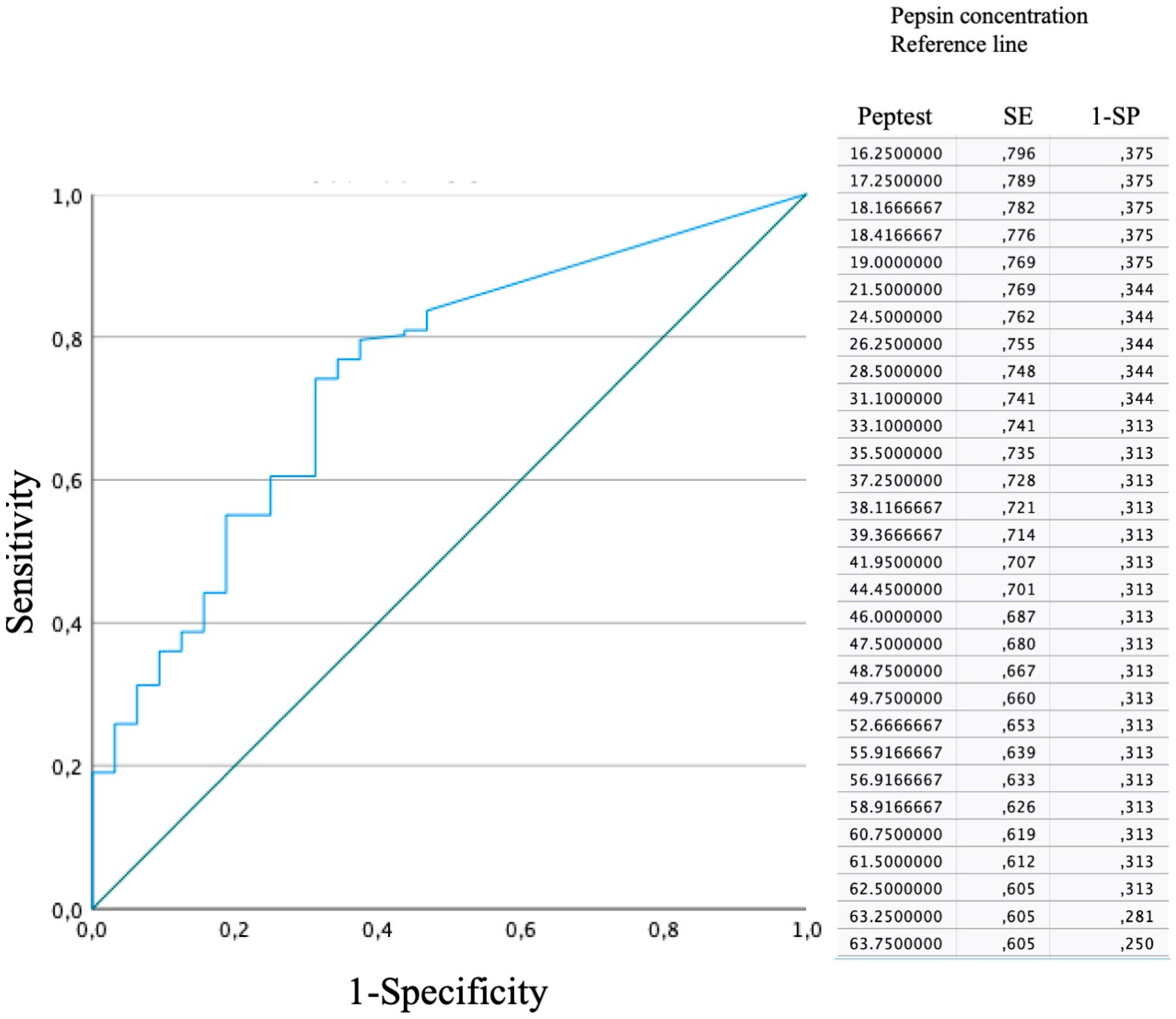
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lechien, J.R.; Akst, L.M.; Hamdan, A.L.; Schindler, A.; Karkos, P.D.; Barillari, M.R.; Calvo-Henriquez, C.; Crevier-Buchman, L.; Finck, C.; Eun, Y.; et al. Evaluation and Management of Laryngopharyngeal Reflux Disease: State of the Art Review. Otolaryngol.-Head Neck Surg. 2019, 160, 762–782. [Google Scholar] [CrossRef]
- Wang, L.; Liu, X.; Liu, Y.L.; Zeng, F.F.; Wu, T.; Yang, C.; Shen, H.; Li, X. Correlation of pepsin-measured laryngopharyngeal reflux disease with symptoms and signs. Otolaryngol.-Head Neck Surg. 2010, 143, 765–771. [Google Scholar] [CrossRef]
- Lechien, J.R.; Bobin, F.; Dapri, G.; Eisendrath, P.; Salem, C.; Mouawad, F.; Horoi, M.; Thill, M.P.; Dequanter, D.; Rodriguez, A.; et al. Hypopharyngeal-Esophageal Impedance-pH Monitoring Profiles of Laryngopharyngeal Reflux Patients. Laryngoscope 2021, 131, 268–276. [Google Scholar] [CrossRef]
- Lechien, J.R.; Allen, J.; Mouawad, F.; Ayad, T.; Barillari, M.R.; Huet, K.; Crevier-Buchman, L.; Hans, S.; Karkos, P.D.; Eun, Y.; et al. Do Laryngologists and General Otolaryngologists Manage Laryngopharyngeal Reflux Differently? Laryngoscope 2020, 130, E539–E547. [Google Scholar] [CrossRef]
- Lechien, J.R.; Mouawad, F.; Mortuaire, G.; Remacle, M.; Bobin, F.; Huet, K.; Nacci, A.; Barillari, M.R.; Crevier-Buchman, L.; Hans, S.; et al. Awareness of European Otolaryngologists and General Practitioners toward Laryngopharyngeal Reflux. Ann. Otol. Rhinol. Laryngol. 2019, 128, 3489419858090. [Google Scholar] [CrossRef]
- Maldonado, A.; Diederich, L.; Castell, D.O.; Gideon, R.M.; Katz, P.O.; Mba, L.D. Laryngopharyngeal reflux identified using a new catheter design: Defining normal values and excluding artifacts. Laryngoscope 2003, 113, 349–355. [Google Scholar] [CrossRef]
- Hayat, J.O.; Gabieta-Somnez, S.; Yazaki, E.; Kang, J.-Y.; Woodcock, A.; Dettmar, P.; Mabary, J.; Knowles, C.H.; Sifrim, D. Pepsin in saliva for the diagnosis of gastro-oesophageal reflux disease. Gut 2015, 64, 373–380. [Google Scholar] [CrossRef]
- Zhang, M.; Chia, C.; Stanley, C.; Phyland, D.J.; Paddle, P.M. Diagnostic Utility of Salivary Pepsin as Compared with 24-Hour Dual pH/Impedance Probe in Laryngopharyngeal Reflux. Otolaryngol.-Head Neck Surg. 2021, 164, 375–380. [Google Scholar] [CrossRef]
- Zeleník, K.; Hránková, V.; Vrtková, A.; Staníková, L.; Komínek, P.; Formánek, M. Diagnostic Value of the PeptestTM in Detecting Laryngopharyngeal Reflux. J. Clin. Med. 2021, 10, 2996. [Google Scholar] [CrossRef]
- Calvo-Henríquez, C.; Ruano-Ravina, A.; Vaamonde, P.; Martínez-Capoccioni, G.; Martín-Martín, C. Is Pepsin a Reliable Marker of Laryngopharyngeal Reflux? A Systematic Review. Otolaryngol.-Head Neck Surg. 2017, 157, 385–391. [Google Scholar] [CrossRef]
- Lechien, J.R.; Bobin, F.; Rodriguez, A.; Dequanter, D.; Muls, V.; Huet, K.; Harmegnies, B.; Crevier-Buchman, L.; Hans, S.; Saussez, S.; et al. Development and Validation of the Short Version of the Reflux Symptom Score: Reflux Symptom Score–12. Otolaryngol.-Head Neck Surg. 2021, 164, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Ruiz, A.R.; Dequanter, D.; Bobin, F.; Mouawad, F.; Muls, V.; Huet, K.; Harmegnies, B.; Remacle, S.; Finck, C.; et al. Validity and Reliability of the Reflux Sign Assessment (RSA). Ann. Otol. Rhinol. Laryngol. 2019, 129, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Chan, W.W.; Akst, L.M.; Hoppo, T.; Jobe, B.A.; Chiesa-Estomba, C.M.; Muls, V.; Bobin, F.; Saussez, S.; Carroll, T.L.; et al. Normative Ambulatory Reflux Monitoring Metrics for Laryngopharyngeal Reflux: A Systematic Review of 720 Healthy Individuals. Otolaryngol.-Head Neck Surg. 2022, 166, 802–819. [Google Scholar] [CrossRef] [PubMed]
- Bobin, F.; Journe, F.; Lechien, J.R. Saliva pepsin level of laryngopharyngeal reflux patients is not correlated with reflux episodes. Laryngoscope 2019, 130, 1278–1281. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.J.; Park, J.M.; Choi, S.Y.; Kim, S.I.; Lee, Y.C.; Eun, Y.G.; Ko, S.G. Comparison Between Manual and Automated Analyses in Multichannel Intraluminal Impedance: pH Monitoring for Laryngopharyngeal Reflux. Otolaryngol.-Head Neck Surg. 2022, 166, 128–132. [Google Scholar] [CrossRef]
- Kim, S.I.; Jeong, S.J.; Kwon, O.E.; Park, J.M.; Lee, Y.C.; Eun, Y.G.; Ko, S.G. 24-Hour Multichannel Intraluminal Impedance–pH in Proton Pump Inhibitor Nonresponders vs Responders in Patients with Laryngopharyngeal Reflux. Otolaryngol.-Head Neck Surg. 2022, 166, 910–916. [Google Scholar] [CrossRef]
- Lechien, J.R. Sensitivity, Specificity, and Predictive Values of Laryngopharyngeal Reflux Symptoms and Signs in Clinical Practice. Otolaryngol.-Head Neck Surg. 2022, 169, 97–104. [Google Scholar] [CrossRef]
- Krause, A.J.; Yadlapati, R. Review article: Diagnosis and management of laryngopharyngeal reflux. Aliment Pharmacol Ther. 2024. [Google Scholar] [CrossRef]
- Krause, A.J.; Greytak, M.; Kaizer, A.M.; Carlson, D.A.; Chan, W.W.; Chen, C.-L.; Gyawali, C.P.; Jenkins, A.; Pandolfino, J.E.; Polamraju, V.; et al. Diagnostic Yield of Ambulatory Reflux Monitoring Systems for Evaluation of Chronic Laryngeal Symptoms. Am. J. Gastroenterol. 2023. [Google Scholar] [CrossRef]
- Wang, J.; Li, J.; Nie, Q.; Zhang, R. Are Multiple Tests Necessary for Salivary Pepsin Detection in the Diagnosis of Laryngopharyngeal Reflux? Otolaryngol.-Head Neck Surg. 2022, 166, 477–481. [Google Scholar] [CrossRef]
- Guo, Z.M.; Jiang, J.M.; Wu, H.M.; Zhu, J.; Zhang, S.; Zhang, C. Salivary peptest for laryngopharyngeal reflux and gastroesophageal reflux disease: A systemic review and meta-analysis. Medicine 2021, 100, e26756. [Google Scholar] [CrossRef] [PubMed]
- Klimara, M.J.; Johnston, N.; Samuels, T.L.; Visotcky, A.M.; Poetker, D.M.; Loehrl, T.A.; Blumin, J.H.; Bock, J.M. Correlation of salivary and nasal lavage pepsin with MII-pH testing. Laryngoscope 2020, 130, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Weitzendorfer, M.; Antoniou, S.A.; Schredl, P.; Witzel, K.; Weitzendorfer, I.C.; Majerus, A.; Emmanuel, K.; Koch, O.O. Pepsin and oropharyngeal pH monitoring to diagnose patients with laryngopharyngeal reflux. Laryngoscope 2020, 130, 1780–1786. [Google Scholar] [CrossRef] [PubMed]
- Ocak, E.; Kubat, G.; Yorulmaz, İ. Immunoserologic pepsin detection in the saliva as a non-invasive rapid diagnostic test for laryngopharyngeal reflux. Balk. Med. J. 2015, 32, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Yuksel, E.S.; Hong, S.K.; Strugala, V.; Slaughter, J.C.; Goutte, M.; Garrett, C.G.; Dettmar, P.W.; Vaezi, M.F. Rapid salivary pepsin test: Blinded assessment of test performance in gastroesophageal reflux disease. Laryngoscope 2012, 122, 1312–1316. [Google Scholar] [CrossRef] [PubMed]
- Potluri, S.; Friedenberg, F.; Parkman, H.P.; Chang, A.; MacNeal, R.; Manus, C.; Bromer, M.Q.; Malik, A.; Fisher, R.S.; Nugent, T.; et al. Comparison of a salivary/sputum pepsin assay with 24-h esophageal pH monitoring for detection of gastric reflux into the proximal esophagus, oropharynx, and lung. Dig. Dis. Sci. 2003, 48, 1813–1817. [Google Scholar] [CrossRef]
- Na, S.Y.; Kwon, O.E.; Lee, Y.C.; Eun, Y.G. Optimal timing of saliva collection to detect pepsin in patients with laryngopharyngeal reflux. Laryngoscope 2016, 126, 2770–2773. [Google Scholar] [CrossRef]
- Sereg-Bahar, M.; Jerin, A.; Jansa, R.; Stabuc, B.; Hocevar-Boltezar, I. Pepsin and bile acids in saliva in patients with laryngopharyngeal reflux—A prospective comparative study. Clin. Otolaryngol. 2015, 40, 234–239. [Google Scholar] [CrossRef]
- Lechien, J.R.; Bobin, F.; Muls, V.; Horoi, M.; Thill, M.-P.; Dequanter, D.; Rodriguez, A.; Saussez, S. Patients with acid, high-fat and low-protein diet have higher laryngopharyngeal reflux episodes at the impedance-pH monitoring. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 511–520. [Google Scholar] [CrossRef]
- Surdea-Blaga, T.; Negrutiu, D.E.; Palage, M.; Dumitrascu, D.L. Food and Gastroesophageal Reflux Disease. Curr. Med. Chem. 2019, 26, 3497–3511. [Google Scholar] [CrossRef]
- Johnston, N.; Wells, C.W.; Samuels, T.L.; Blumin, J.H. Pepsin in nonacidic refluxate can damage hypopharyngeal epithelial cells. Ann. Otol. Rhinol. Laryngol. 2009, 118, 677–685. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Baroni, S.; Salonna, G.; Marchese, M.; Graziadio, M.; Di Cintio, G.; Paludetti, G.; Costamagna, G.; Galli, J. Impact of bile acids on the severity of laryngo-pharyngeal reflux. Clin. Otolaryngol. 2021, 46, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, C.T.; Doukas, S.G.; Costa, J.; Vageli, D.P. Biliary reflux as a causal factor in hypopharyngeal carcinoma: New clinical evidence and implications. Cancer 2020, 125, 3554–3565. [Google Scholar] [CrossRef] [PubMed]
- Tutar, H.; Erdamar, H.; Köybaşioğlu, A.; Dinç, A.E.; Ceylan, A.; Uslu, S. Can bile acids be an etiological factor for laryngeal carcinoma? ORL J. Otorhinolaryngol. Relat. Spec. 2011, 73, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.-W.; Roh, J.-L.; Park, B.J.; Park, S.W.; Kwon, T.-K.; Lee, S.J.; Kim, K.H. Bile acid induces cyclo-oxygenase-2 expression in cultured human pharyngeal cells: A possible mechanism of carcinogenesis in the upper aerodigestive tract by laryngopharyngeal reflux. Laryngoscope 2003, 113, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Sereg-Bahar, M.; Jerin, A.; Hocevar-Boltezar, I. Higher levels of total pepsin and bile acids in the saliva as a possible risk factor for early laryngeal cancer. Radiol. Oncol. 2015, 49, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Galli, J.; Calò, L.; Agostino, S.; Cadoni, G.; Sergi, B.; Cianci, R.; Cammarota, G. Bile reflux as possible risk factor in laryngopharyngeal inflammatory and neoplastic lesions. Acta Otorhinolaryngol. Ital. 2003, 23, 377–382. [Google Scholar]
- Salgado, S.; Borges, L.F.; Cai, J.X.; Lo, W.-K.; Carroll, T.L.; Chan, W.W. Symptoms classically attributed to laryngopharyngeal reflux correlate poorly with pharyngeal reflux events on multichannel intraluminal impedance testing. Dis. Esophagus 2022, 36, doac041. [Google Scholar] [CrossRef]
- Lien, H.-C.; Lee, P.-H.; Wang, C.-C. Diagnosis of Laryngopharyngeal Reflux: Past, Present, and Future—A Mini-Review. Diagnostics 2023, 13, 1643. [Google Scholar] [CrossRef]
- Chen, J.W.; Vela, M.F.; Peterson, K.A.; Carlson, D.A. AGA Clinical Practice Update on the Diagnosis and Management of Extraesophageal Gastroesophageal Reflux Disease: Expert Review. Clin. Gastroenterol. Hepatol. 2023, 21, 1414–1421.e3. [Google Scholar] [CrossRef]
- Sikavi, D.R.; Cai, J.X.; Leung, R.; Carroll, T.L.; Chan, W.W. Impaired Proximal Esophageal Contractility Predicts Pharyngeal Reflux in Patients with Laryngopharyngeal Reflux Symptoms. Clin. Transl. Gastroenterol. 2021, 12, e00408. [Google Scholar] [CrossRef] [PubMed]
- Vance, D.; Park, J.; Alnouri, G.; Turner, R.R.; Daggumati, S.; Ferster, A.P.O.; Ahmad, A.; Lyons, K.; Ross, J.; Russell, K.; et al. Diagnosing Laryngopharyngeal Reflux: A Comparison between 24-h pH-Impedance Testing and Pharyngeal Probe (Restech) Testing, with Introduction of the Sataloff Score. J. Voice 2023, 37, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Divakaran, S.; Rajendran, S.; Thomas, R.M.; Jacob, J.; Kurien, M. Laryngopharyngeal Reflux: Symptoms, Signs, and Presence of Pepsin in Saliva—A Reliable Diagnostic Triad. Int. Arch. Otorhinolaryngol. 2021, 25, e273–e278. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | |
|---|---|
| Age (mean, SD) | 53.8 ± 14.5 |
| BMI (mean, SD) | 26.7 ± 6.2 |
| Male (N, %) | 57 (38.8) |
| Female (N, %) | 90 (61.2) |
| Gastrointestinal endoscopy (N = 107) | |
| Normal | 34 (31.8) |
| Esophagitis | 12 (11.2) |
| Hiatal hernia | 43 (40.2) |
| LES insufficiency | 45 (42.1) |
| Gastritis | 11 (10.3) |
| HEMII-pH (mean, SD) | |
| Pharyngeal acid events | 8.4 ± 13.3 |
| Pharyngeal nonacid events | 17.3 ± 32.0 |
| Pharyngeal events (total number) | 25.7 ± 33.3 |
| Clinical data | |
| Reflux Symptom Score-12 (mean, SD) | 64.9 ± 49.2 |
| Reflux Sign Assessment (mean, SD) | |
| Oral score | 5.3 ± 2.4 |
| Pharyngeal score | 9.4 ± 4.2 |
| Laryngeal score | 8.6 ± 5.0 |
| Reflux Sign Assessment | 21.9 ± 8.5 |
| Pepsin Tests | Accuracy |
|---|---|
| Morning (N = 141) | |
| ≥16 ng/mL | 66.0 |
| ≥36 ng/mL | 56.7 |
| ≥45 ng/mL | 55.3 |
| ≥100 ng/mL | 43.3 |
| Bedtime (N = 146) | |
| ≥16 ng/mL | 63.7 |
| ≥36 ng/mL | 58.2 |
| ≥45 ng/mL | 55.5 |
| ≥100 ng/mL | 43.8 |
| Highest sample concentration (N = 147) | |
| ≥16 ng/mL | 81.6 |
| ≥36 ng/mL | 77.5 |
| ≥45 ng/mL | 74.8 |
| ≥100 ng/mL | 61.5 |
| Morning Pepsin Test | Bedtime Pepsin Test | Highest Pepsin Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SE | SP | PPV | NPV | SE | SP | PPV | NPV | SE | SP | PPV | NPV | |
| ≥16 ng/mL | 65.1 | 62.5 | 88.8 | 28.2 | 63.9 | 64.5 | 89.3 | 27.8 | 81.6 | 53.1 | 88.9 | 38.6 |
| ≥36 ng/mL | 56.8 | 78.1 | 92.2 | 28.4 | 57.6 | 74.1 | 91.2 | 27.4 | 77.5 | 65.6 | 91.2 | 38.9 |
| ≥45 ng/mL | 52.7 | 81.8 | 92.8 | 28.1 | 56.2 | 75.0 | 91.0 | 27.6 | 74.8 | 70.6 | 91.7 | 39.3 |
| ≥100 ng/mL | 42.2 | 86.2 | 93.9 | 22.7 | 44.8 | 84.4 | 92.9 | 25.2 | 61.5 | 78.1 | 92.9 | 30.5 |
| Author | Year | LPR/CT | Diagnosis of LPR | Sample Time | Pepsin Analysis | Cutoffs | SE | SP | PPV | NPV | Accuracy |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang [18] | 2022 | 112/26 | HEMII-pH (Sandhill); | Each hour from | Pepsin lateral | >45 ng/mL | 38.4 | 84.6 | 91.5 | 24.2 | 55.7 |
| ≥1 pharyngeal event | 7:00 a.m. (fasting) | flow device; | Fasting test | ||||||||
| to 6:00 p.m. | highest of | >45 ng/mL | 86.6 | 80.8 | 95.1 | 58.3 | 73.9 | ||||
| concentrations | Highest test | ||||||||||
| in morning | |||||||||||
| Zelenik [9] | 2021 | 45/1 | HEMII-pH (Medtronic); | Fasting | PepTest | ≥16 ng/mL | 48.0 | 27.0 | 63.0 | 40.0 | 48.0 |
| >1 pharyngeal event | |||||||||||
| Zhang [8] | 2020 | 26/4 | HEMII-pH (Sandhill); | Fasting; | PepTest | ≥16 ng/mL | 76.9 | 25.0 | 87.0 | 14.3 | 87.0 |
| ≥2 pharyngeal events, | 1 h post-lunch, | ≥75 ng/mL | 57.7 | 75.0 | 93.8 | 21.4 | N.P. | ||||
| ≥6 proximal events | 1 h post-dinner, | ||||||||||
| when symptoms | |||||||||||
| Klimara [19] | 2019 | 19/7 | HEMII-pH (Sandhill); | Fasting; | ELISA | >1 ng/mL | 29.4 | 50.0 | 62.5 | 20.0 | 42.0 |
| >1 pharyngeal event, | 1 h post-lunch, | Western blot; | |||||||||
| >40 proximal events | 1 h post-dinner, | highest | |||||||||
| 1 h post-breakfast | concentration | ||||||||||
| Weitzendorfer | 2019 | 41/29 | Oropharyngeal pH test; | 3 samples | PepTest; | >16 ng/mL | 85.4 | 27.6 | 62.5 | 57.1 | 85.4 |
| [20] | Ryan score >9.4 | highest of | >50 ng/mL | 78.1 | 41.4 | 65.3 | 57.1 | ||||
| 3 samples | >100 ng/mL | 68.3 | 58.6 | 70.0 | 56.7 | ||||||
| >150 ng/mL | 53.7 | 69.0 | 71.0 | 51.3 | |||||||
| >216 ng/mL | 41.5 | 86.2 | 81.0 | 51.0 | |||||||
| Hayat [7] | 2015 | 111/100 | MII-pH; | Fasting; | PepTest | >16 ng/mL | 77.6 | 63.2 | 58.4 | 80.4 | N.P. |
| esophageal acid | 1 h post-lunch, | >50 ng/mL | 67.2 | 76.3 | 67.2 | 76.8 | |||||
| exposure time pH < 4, | 1 h post-dinner | >100 ng/mL | 51.7 | 74.5 | 54.5 | 72.3 | |||||
| >4.2% | >150 ng/mL | 41.4 | 90.8 | 75.0 | 69.9 | ||||||
| >210 ng/mL | 44.2 | 96.3 | 95.7 | 36.5 | |||||||
| Ocak [21] | 2015 | 18/2 | Dual-probe pH testing; | N.P. | PepTest | ≥16 ng/mL | 33.0 | 100 | 100 | 14.2 | N.P. |
| distal esophageal pH | |||||||||||
| time pH < 4.0, >5% | |||||||||||
| Saritas [22] | 2012 | 22/25 | Wireless pH testing; | N.P. | PepTest | ≥50 ng/mL | 50.0 | 92.0 | 85.0 | 68.0 | N.P. |
| esophageal acid | |||||||||||
| exposure time pH < 4, | |||||||||||
| >4.2% | |||||||||||
| Potluri [22] | 2003 | 3/13 | Dual-probe pH testing; | When symptoms | Pepsin | >1 ng/mL | 100 | 92.3 | N.P. | N.P. | N.P. |
| ≥1 proximal acid | assay | ||||||||||
| esophageal event | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lechien, J.R.; Bobin, F. Diagnostic Value of Fasting and Bedtime Saliva Pepsin Measurements in Laryngopharyngeal Reflux. Biomedicines 2024, 12, 398. https://doi.org/10.3390/biomedicines12020398
Lechien JR, Bobin F. Diagnostic Value of Fasting and Bedtime Saliva Pepsin Measurements in Laryngopharyngeal Reflux. Biomedicines. 2024; 12(2):398. https://doi.org/10.3390/biomedicines12020398
Chicago/Turabian StyleLechien, Jerome R., and Francois Bobin. 2024. "Diagnostic Value of Fasting and Bedtime Saliva Pepsin Measurements in Laryngopharyngeal Reflux" Biomedicines 12, no. 2: 398. https://doi.org/10.3390/biomedicines12020398
APA StyleLechien, J. R., & Bobin, F. (2024). Diagnostic Value of Fasting and Bedtime Saliva Pepsin Measurements in Laryngopharyngeal Reflux. Biomedicines, 12(2), 398. https://doi.org/10.3390/biomedicines12020398







