Wessex Head Injury Matrix in Patients with Prolonged Disorders of Consciousness: A Reliability Study
Abstract
:1. Introduction
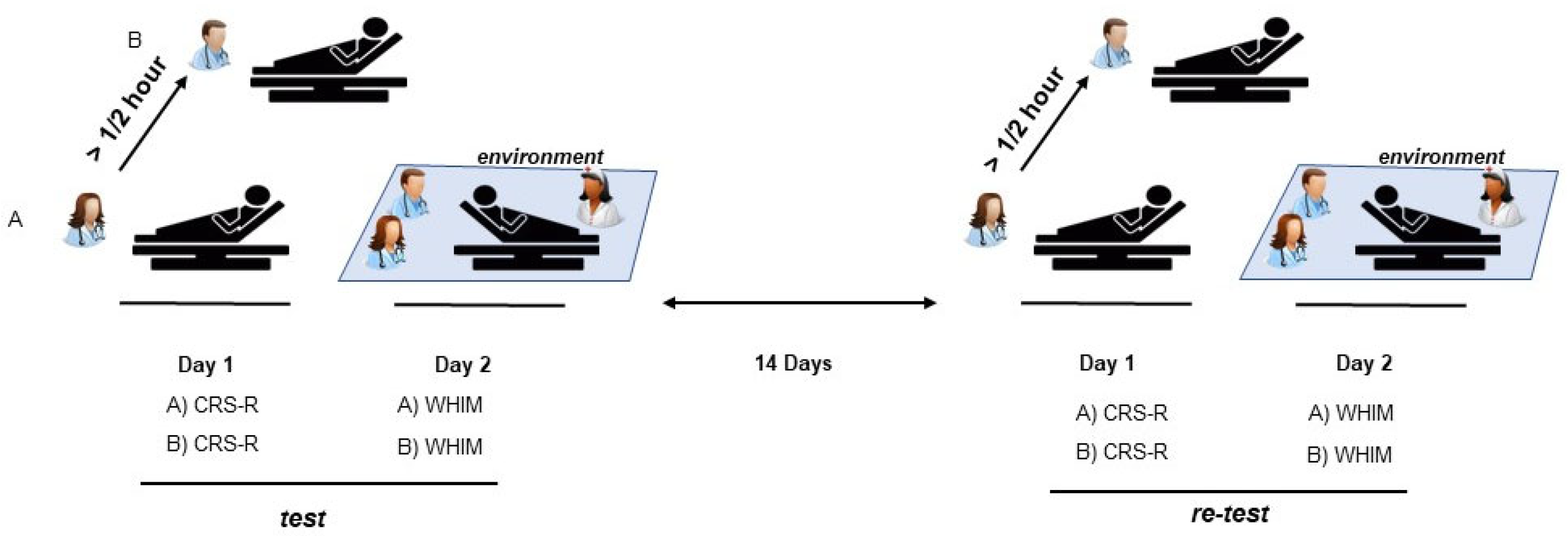
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zeman, A. Consciousness. In Encyclopedia of Cognitive Science; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2006. [Google Scholar]
- Schnakers, C. Update on diagnosis in disorders of consciousness. Expert Rev. Neurother. 2020, 20, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Katz, D.I.; Schiff, N.D.; Whyte, J.; Ashman, E.J.; Ashwal, S.; Barbano, R.; Hammond, F.M.; Laureys, S.; Ling, G.S.; et al. Comprehensive systematic review update summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology 2018, 91, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Kondziella, D.; Bender, A.; Diserens, K.; van Erp, W.; Estraneo, A.; Formisano, R.; Laureys, S.; Naccache, L.; Ozturk, S.; Rohaut, B.; et al. European Academy of Neurology guideline on the diagnosis of coma and other disorders of consciousness. Eur. J. Neurol. 2020, 27, 741–756. [Google Scholar] [CrossRef] [PubMed]
- Giacino, J.T.; Kalmar, K.; Whyte, J. The JFK Coma Recovery Scale-Revised: Measurement characteristics and diagnostic utility. Arch. Phys. Med. Rehabil. 2004, 85, 2020–2029. [Google Scholar] [CrossRef] [PubMed]
- Shiel, A.; Horn, S.A.; Wilson, B.A.; Watson, M.J.; Campbell, M.J.; Mclellan, D.L. The Wessex Head Injury Matrix (WHIM) main scale: A preliminary report on a scale to assess and monitor patient recovery after severe head injury. Clin. Rehabil. 2000, 14, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Gouvier, W.D.; Blanton, P.D.; LaPorte, K.K.; Nepomuceno, C. Reliability and validity of the Disability Rating Scale and the Levels of Cognitive Functioning Scale in monitoring recovery from severe head injury. Arch. Phys. Med. Rehabil. 1987, 68, 94–97. [Google Scholar] [CrossRef]
- Seel, R.T.; Sherer, M.; Whyte, J.; Katz, D.I.; Giacino, J.T.; Rosenbaum, A.M.; Hammond, F.M.; Kalmar, K.; DrPH, T.L.-B.P.; Zafonte, R.; et al. Assessment Scales for Disorders of Consciousness: Evidence-Based Recommendations for Clinical Practice and Research. Arch. Phys. Med. Rehabil. 2010, 91, 1795–1813. [Google Scholar] [CrossRef]
- Gill-Thwaites, H. The Sensory Modality Assessment Rehabilitation Technique—A tool for assessment and treatment of patients with severe brain injury in a vegetative state. Brain Inj. 1997, 11, 723–734. [Google Scholar] [CrossRef]
- Wijdicks, E.F.M.; Bamlet, W.R.; Maramattom, B.V.; Manno, E.M.; McClelland, R.L. Validation of a new coma scale: The FOUR score. Ann. Neurol. 2005, 58, 585–593. [Google Scholar] [CrossRef]
- Benzer, A.; Mitterschiffthaler, G.; Pühkringer, F.; De La Renotiere, K.; Marosi, M.; Luef, G.; Lehner, H.; Schmutzhard, E. Prediction of non-survival after trauma: Innsbruck Coma Scale. Lancet 1991, 338, 977–978. [Google Scholar] [CrossRef]
- Wilson, B.A.; Coleman, M.R.; Pickard, J.D. Neuropsychological Assessment and Management of People in States of Impaired Consciousness: An Overview of Some Recent Studies. Brain Impair. 2008, 9, 28–35. [Google Scholar] [CrossRef]
- Majerus, S.; De Linden, M.V.; Shiel, A. Wessex Head Injury Matrix and Glasgow/Glasgow-Liege Coma Scale: A Validation and Comparison Study. Neuropsychol. Rehabil. 2000, 10, 167–184. [Google Scholar] [CrossRef]
- Turner-Stokes, L.; Bassett, P.; Rose, H.; Ashford, S.; Thu, A. Serial measurement of Wessex Head Injury Matrix in the diagnosis of patients in vegetative and minimally conscious states: A cohort analysis. BMJ Open 2015, 5, e006051. [Google Scholar] [CrossRef] [PubMed]
- Dhamapurkar, S.; Wilson, B.; Rose, A.; Florschutz, G.; Watson, P.; Shiel, A. Does a regular Wessex Head Injury Matrix (WHIM) assessment identify early signs of infections in people with Prolonged Disorders of Consciousness (PDOC)? Brain Inj. 2018, 32, 1103–1109. [Google Scholar] [CrossRef] [PubMed]
- Cortese, M.D.; Vatrano, M.; Arcuri, F.; Raso, M.G.; Tonin, P.; Calabrò, R.S.; Riganello, F. Behavioral scales variability in patients with prolonged disorders of consciousness. Neurol. Sci. 2023, 44, 3107–3122. [Google Scholar] [CrossRef]
- Pistoia, F.; Shiel, A.; Ornello, R.; Saporito, G.; Gentili, L.; Carolei, A.; Marini, C.; Sacco, S.; Marinangeli, F. Translation and Transcultural Adaptation of the Wessex Head Injury Matrix, Italian Version: A Preliminary Report. Brain Sci. 2021, 11, 810. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Park, J.H.; Kim, A.R.; Park, M.; Kim, T.-W. Coma Recovery Scale-r: Variability in the Disorder of Consciousness. BMC Neurol. 2015, 15, 186. [Google Scholar] [CrossRef]
- Candelieri, A.; Cortese, M.D.; Dolce, G.; Riganello, F.; Sannita, W.G. Visual Pursuit: Within-Day Variability in the Severe Disorder of Consciousness. J. Neurotrauma 2011, 28, 2013–2017. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Giacino, J.T.; Zasler, N.D.; Katz, D.I.; Kelly, J.P.; Rosenberg, J.H.; Filley, C.M. Development of Practice Guidelines for Assessment and Management of the Vegetative and Minimally Conscious States. J. Head Trauma Rehabil. 1997, 12, 79–89. [Google Scholar] [CrossRef]
- Wilson, B.A.; Shiel, A.; McLellan, L.; Horn, S.; Watson, M.A. Monitoring Recovery of Cognitive Function Following Severe Traumatic Brain Injury. Brain Impair. 2001, 2, 22–28. [Google Scholar] [CrossRef]
- Doig, E.J.; Lane-Brown, A.T. Responsiveness of Instruments to Assess Disorders of Consciousness: A Literature Review. Brain Impair. 2012, 13, 285–315. [Google Scholar] [CrossRef]
- Verity Stokes Gunn, S.; Schouwenaars, K.; Badwan, D. Neurobehavioural assessment and diagnosis in disorders of consciousness: A preliminary study of the Sensory Tool to Assess Responsiveness (STAR). Neuropsychol. Rehabil. 2018, 28, 966–983. [Google Scholar] [CrossRef]
- Gosseries, O.; Vanhaudenhuyse, A.; Bruno, M.A.; Demertzi, A.; Schnakers, C.; Boly, M.M.; Maudoux, A.; Moonen, G.; Laureys, S. Disorders of Consciousness: Coma, Vegetative and Minimally Conscious States. In States of Consciousness; Cvetkovic, D., Cosic, I., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 29–55. [Google Scholar]
| UWS/VS | MCS | ||||||
|---|---|---|---|---|---|---|---|
| Gender | Age | Time from Injury (Days) | Etiology | Gender | Age | Time from Injury (Days) | Etiology |
| female | 69 | 280 | HEM | female | 48 | 214 | HEM |
| 49 | 200 | 65 | 182 | ||||
| 49 | 538 | 71 | 1591 | ||||
| 75 | 309 | 47 | 1040 | ||||
| 56 | 192 | 65 | 183 | ||||
| 56 | 219 | 40 | 200 | ||||
| 58 | 1072 | 69 | 2568 | TBI | |||
| 42 | 213 | ANOX | |||||
| 64 | 182 | male | 51 | 295 | HEM | ||
| 59 | 280 | TBI | 76 | 2143 | |||
| 30 | 250 | 64 | 822 | ||||
| male | 63 | 185 | HEM | 66 | 241 | ||
| 56 | 297 | 19 | 190 | TBI | |||
| 81 | 340 | 70 | 3325 | ||||
| 59 | 968 | 40 | 317 | ||||
| 74 | 254 | 44 | 3012 | ||||
| 41 | 277 | 47 | 1488 | ||||
| 62 | 258 | TBI | 27 | 411 | |||
| 47 | 394 | 47 | 394 | ||||
| 29 | 290 | ||||||
| 45 | 253 | ||||||
| 49 | 190 | ||||||
| 42 | 2320 | ANOX | 39 | 194 | OTHER | ||
| 52 | 213 | ||||||
| 70 | 190 | ||||||
| 64 | 214 | ||||||
| 56 | 200 | ||||||
| 64 | 299 | ||||||
| 61 | 195 | ||||||
| 51 | 185 | ||||||
| 47 | 189 | OTHER | |||||
| 39 | 194 | ||||||
| Test | Retest | ||||
|---|---|---|---|---|---|
| Raters A | Raters A | ||||
| WHIM TNB | WHIM MAB | WHIM TNB | WHIM MAB | ||
| CRS-R | Rho = 0.90; p = 0.0001 | Rho = 0.77; p = 0.0001 | CRS-R | Rho = 0.88; p = 0.0001 | Rho = 0.86; p = 0.0001 |
| Raters B | Raters B | ||||
| WHIM TNB | WHIM MAB | WHIM TNB | WHIM MAB | ||
| CRS-R | Rho = 0.90; p = 0.0001 | Rho = 0.76; p = 0.0001 | CRS-R | Rho = 0.88; p = 0.0001 | Rho = 0.86; p = 0.0001 |
| Test (n = 51) | Retest (n = 51) | ||||
|---|---|---|---|---|---|
| A vs. B | |||||
| WHIM MAB | WHIM TNB | CRS-R | WHIM MAB | WHIM TNB | CRS-R |
| K = 0.96 CI 95% (0.90–1) | K = 0.81 CI 95% (0.70–0.92) | K = 1 | K = 0.96 CI 95% (0.90–1) | K = 0.94 CI 95% (0.86–1) | K = 0.98 CI 95% (0.93–1) |
| A (n = 51) | B (n = 51) | ||||
| Test vs. retest | Test vs. retest | ||||
| WHIM MAB | WHIM TNB | CRS-R | WHIM MAB | WHIM TNB | CRS-R |
| K = 0.62 CI 95% (0.47–0.76) | K = 0.31 CI 95% (0.17–0.44) | K = 0.28 CI 95% (0.14–0.43) | K = 0.62 CI 95% (0.47–0.76) | K = 0.31 CI 95% (0.17–0.44) | K = 0.31 CI 95% (0.17–0.44) |
| Test | Retest | |||||
|---|---|---|---|---|---|---|
| A vs. B | ||||||
| WHIM MAB | WHIM TNB | CRS-R | WHIM MAB | WHIM TNB | CRS-R | |
| a1 (n = 21) | 0.94 | 0.79 | 1 | 0.90 | 0.95 | 0.94 |
| a2 (n = 20) | 0.94 | 0.71 | 1 | 1 | 0.94 | 1 |
| a3 (n = 10) | 1 | 1 | 1 | 1 | 0.88 | 1 |
| m1 (n = 36) | 0.97 | 0.79 | 1 | 0.97 | 0.94 | 0.97 |
| m2 (n = 15) | 0.93 | 0.85 | 1 | 0.92 | 0.92 | 1 |
| A | B | |||||
| Test vs. retest | Test vs. retest | |||||
| WHIM MAB | WHIM TNB | CRS-R | WHIM MAB | WHIM TNB | CRS-R | |
| a1 (n = 21) | 0.63 | 0.30 | 0.08 | 0.63 | 0.29 | 0.14 |
| a2 (n = 20) | 0.53 | 0.10 | 0.26 | 0.53 | 0.15 | 0.26 |
| a3 (n = 10) | 0.67 | 0.66 | 0.65 | 0.67 | 0.55 | 0.65 |
| m1 (n = 36) | 0.57 | 0.22 | 0.22 | 0.57 | 0.27 | 0.26 |
| m2 (n = 15) | 0.70 | 0.50 | 0.34 | 0.70 | 0.35 | 0.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cortese, M.D.; Arcuri, F.; Vatrano, M.; Pioggia, G.; Cerasa, A.; Raso, M.G.; Tonin, P.; Riganello, F. Wessex Head Injury Matrix in Patients with Prolonged Disorders of Consciousness: A Reliability Study. Biomedicines 2024, 12, 82. https://doi.org/10.3390/biomedicines12010082
Cortese MD, Arcuri F, Vatrano M, Pioggia G, Cerasa A, Raso MG, Tonin P, Riganello F. Wessex Head Injury Matrix in Patients with Prolonged Disorders of Consciousness: A Reliability Study. Biomedicines. 2024; 12(1):82. https://doi.org/10.3390/biomedicines12010082
Chicago/Turabian StyleCortese, Maria Daniela, Francesco Arcuri, Martina Vatrano, Giovanni Pioggia, Antonio Cerasa, Maria Girolama Raso, Paolo Tonin, and Francesco Riganello. 2024. "Wessex Head Injury Matrix in Patients with Prolonged Disorders of Consciousness: A Reliability Study" Biomedicines 12, no. 1: 82. https://doi.org/10.3390/biomedicines12010082
APA StyleCortese, M. D., Arcuri, F., Vatrano, M., Pioggia, G., Cerasa, A., Raso, M. G., Tonin, P., & Riganello, F. (2024). Wessex Head Injury Matrix in Patients with Prolonged Disorders of Consciousness: A Reliability Study. Biomedicines, 12(1), 82. https://doi.org/10.3390/biomedicines12010082







