Evaluation of Safety and Potency of Kyasanur Forest Disease (KFD) Vaccine Inactivated with Different Concentrations of Formalin and Comparative Evaluation of In Vitro and In Vivo Methods of Virus Titration in KFD Vaccine
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure for Chick Embryo Fibroblast Monolayer Culture
2.2. Inactivation of the KFD Virus
2.3. Safety and Potency Test
2.3.1. Safety Test Procedure
2.3.2. Potency Test Procedure
2.4. Comparison of In Vitro and In Vivo Tests for Titration of Non-Cytopathic KDFV in the Vaccine
2.4.1. Titration of Virus in Vaccine for MLD50
2.4.2. Quantification of KFDV by Real-Time, Reverse Transcriptase Polymerase Chain Reaction
2.5. Regulatory Permission to Conduct Research on KFD
3. Results
3.1. Preparation of Kyasanur Forest Disease (KFD) Vaccine in Chick Embryo Fibroblast (CEF) Primary Culture
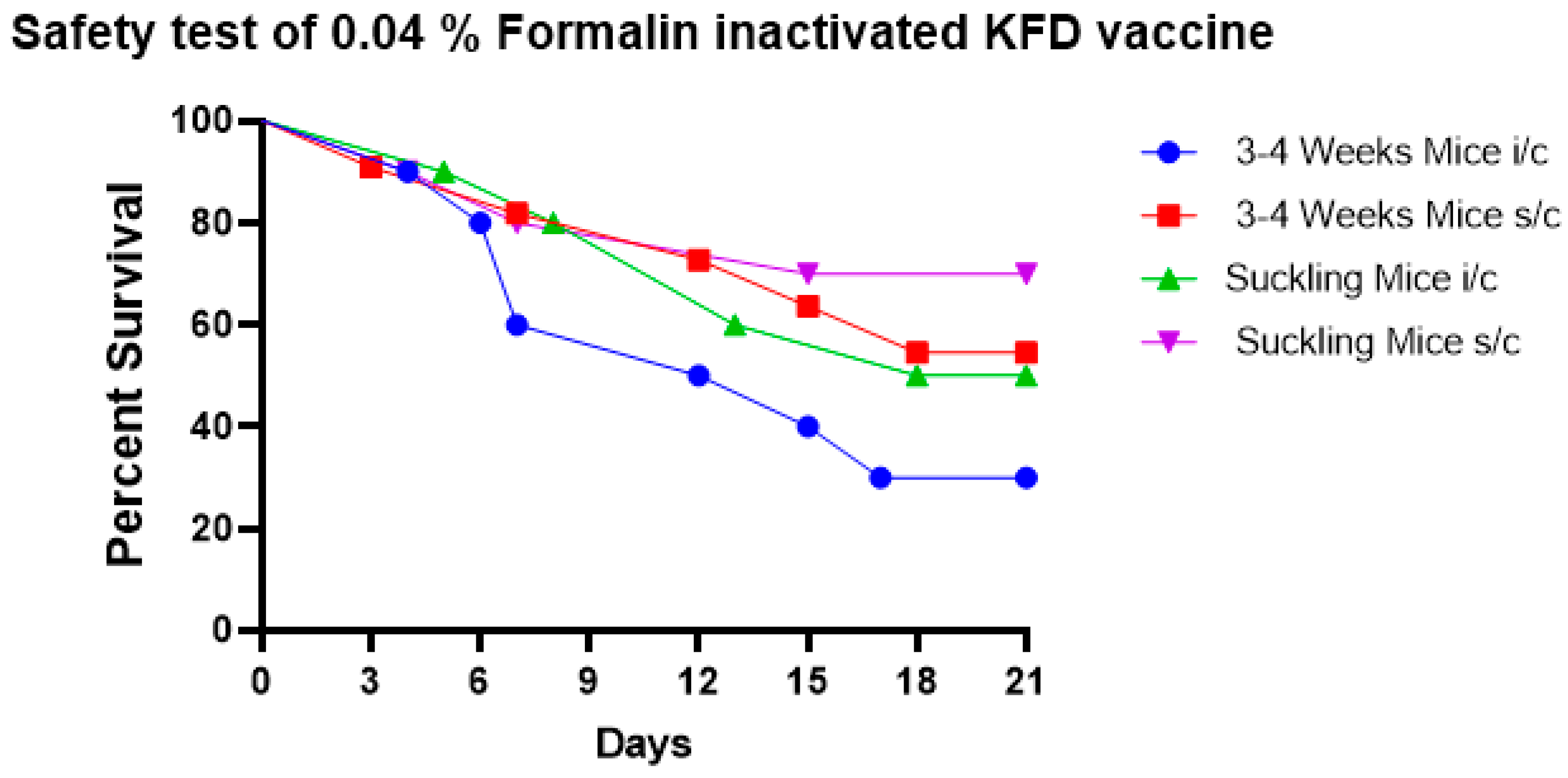
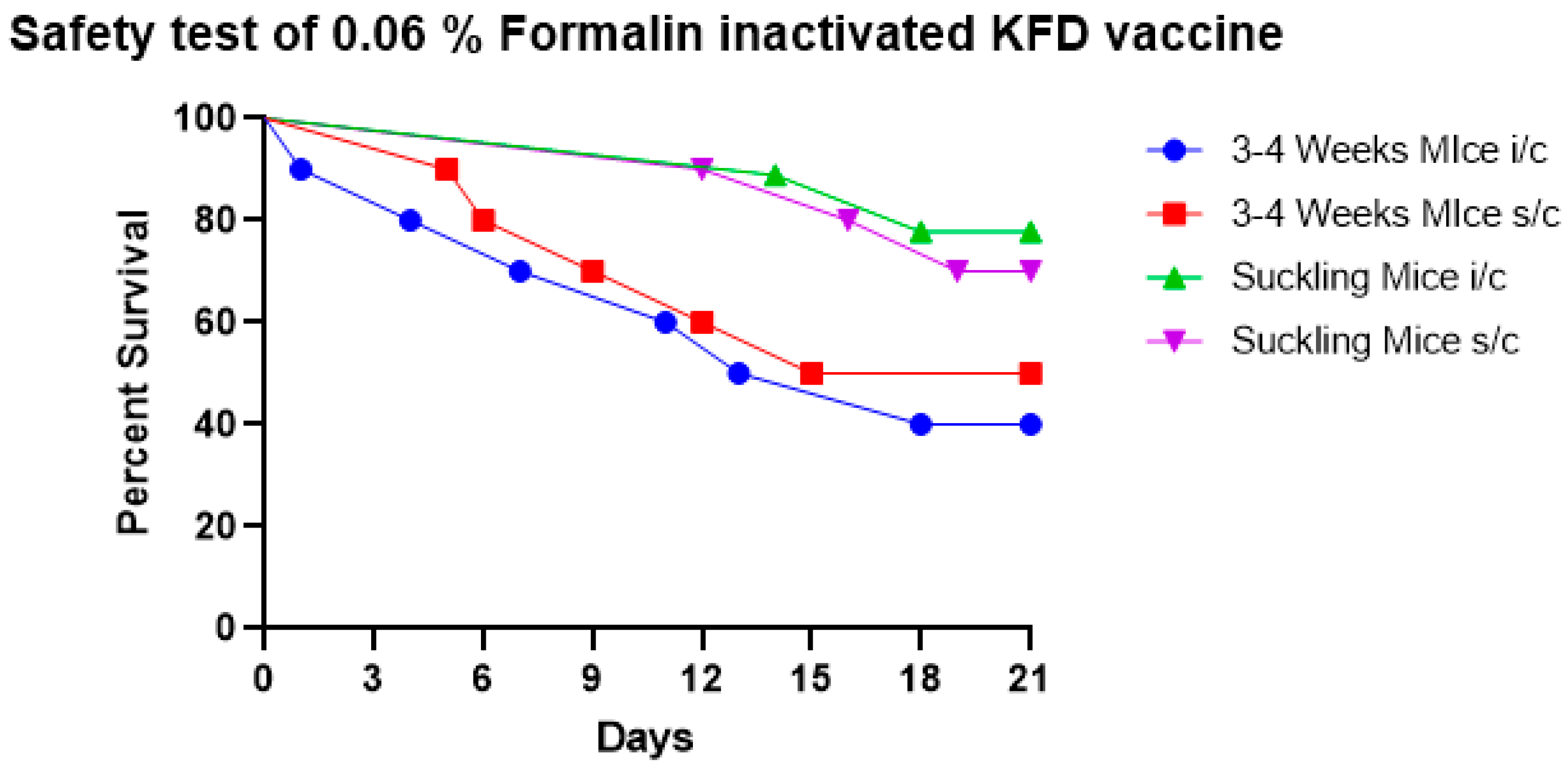
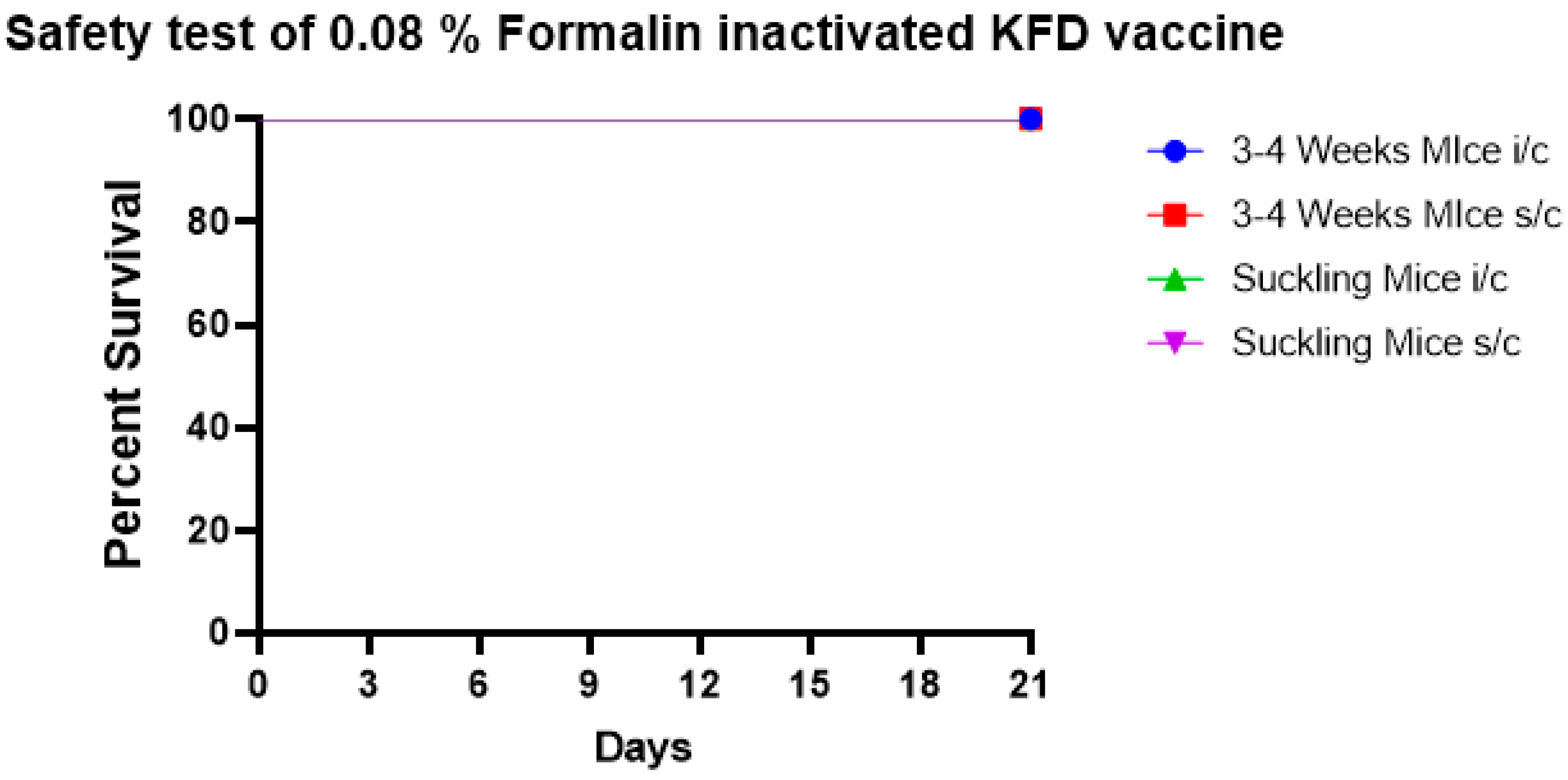
3.2. Safety Test KFD Vaccine in Mice
3.2.1. Safety Test of 0.04% Formalin Inactivated KFD Vaccine in Mice
3.2.2. Safety Test of 0.06% Formalin Inactivated KFD Vaccine in Mice
3.2.3. Safety Test of 0.08% Formalin Inactivated KFD Vaccine in Mice
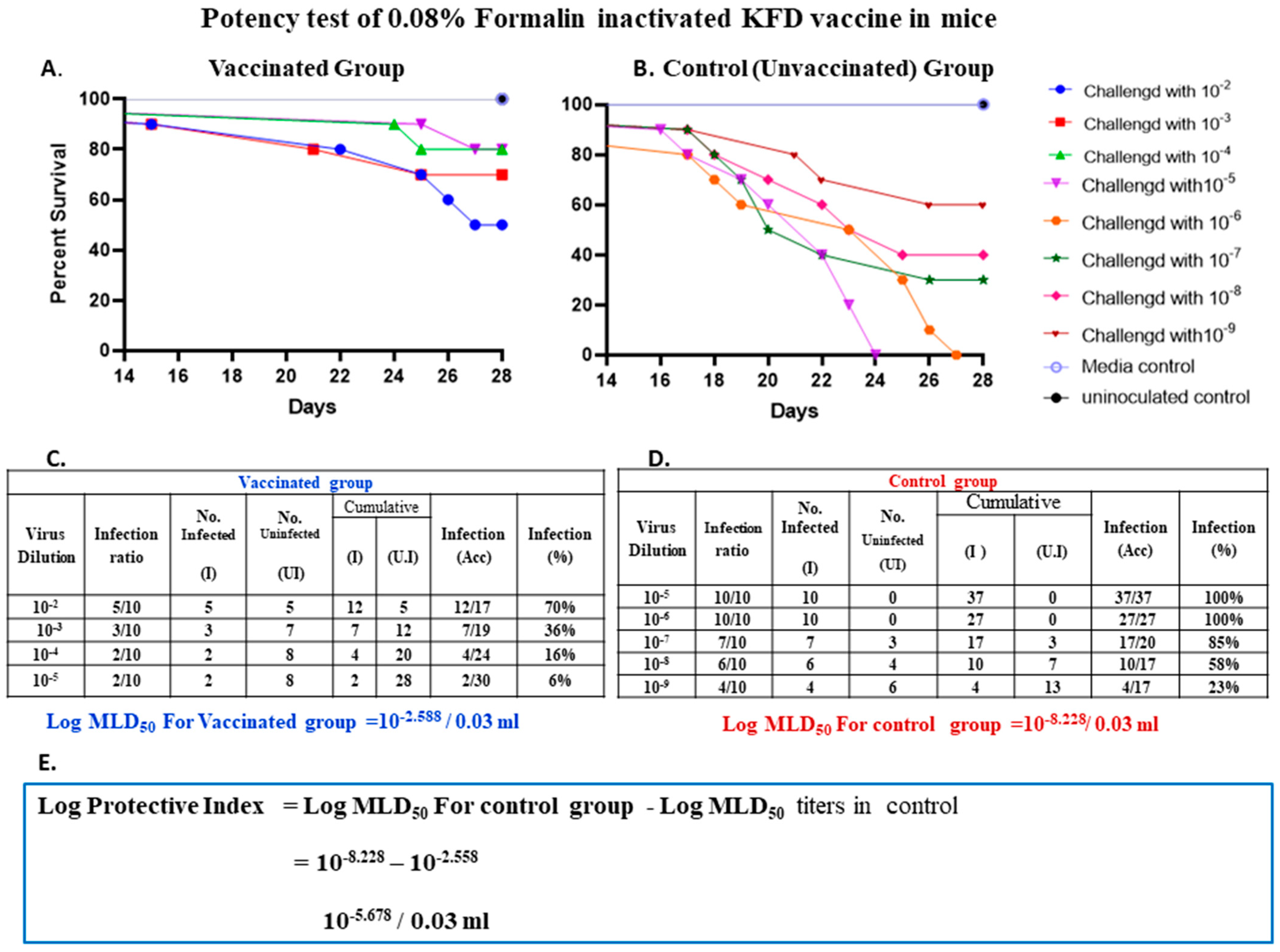
3.3. Potency Test for 0.08% Formalin Inactivated KFD Vaccine
3.4. Quantification of Kyasanur Forest Disease Virus by Real-Time PCR and Its Comparison with In Vivo Titration in Mice
3.5. In Vivo Quantification of Virus by Mice Inoculation Test
3.6. Quantification of KFDV Titre by Real-Time PCR
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Work, T.H.; Trapido, H. Kyasanur Forest Disease. A New Virus Disease in India. Summary of Preliminary Report of Investigations of the Virus Research Centre on an Epidemic Disease Affecting Forest Villagers and Wild Monkeys of Shimoga District, Mysore. Indian J. Med. Sci. 1957, 11, 341–342. [Google Scholar] [PubMed]
- Trapido, H.; Rajagopalan, P.K.; Work, T.H.; Varma, M.G. Kyasanur Forest disease. VIII. Isolation of Kyasanur Forest disease virus from naturally infected ticks of the genus Haemaphysalis. Indian J. Med. Res. 1959, 47, 133–138. [Google Scholar] [PubMed]
- Bhat, H.R.; Sreenivasan, M.A.; Goverdhan, M.K.; Naik, S.V.; Banerjee, K. Antibodies to Kyasanur Forest disease virus in bats in theepizootic-epidemic area and neighbourhood. Indian J. Med. Res. 1978, 68, 387–392. [Google Scholar]
- Boshell, J.; Rajagopalan, P.K. Observations on the experimental exposure of monkeys, rodents, and shrews to infestation of ticks in forest in Kyasanur Forest diseases area. Indian J. Med. Res. 1968, 56, 573–588. [Google Scholar] [PubMed]
- Anderson, C.R.; Singh, K.R.P. The reaction of cattle to Kyasanur Forest disease virus. Indian J. Med. Res. 1971, 59, 195–198. [Google Scholar] [PubMed]
- Pattnaik, P. Kyasanur forest disease: An epidemiological view in India. Rev. Med. Virol. 2006, 16, 151–165. [Google Scholar] [CrossRef]
- Singh, B.B.; Gajadhar, A.A. Role of India’s wildlife in the emergence and re-emergence of zoonotic pathogens, risk factors and public health implications. Acta Tropica 2014, 138, 67–77. [Google Scholar] [CrossRef]
- Dandawate, C.N.; Desai, G.B.; Banerjee, K. Field Evaluation of Formalin Inactivated Kyasanur Forest Disease Virus Tissue Culture Vaccine in Three Districts of Karnataka State. Indian J. Med. Res. 1994, 99, 152–158. [Google Scholar]
- Kasabi, G.S.; Murhekar, M.V.; Yadav, P.D.; Raghunandan, R.; Kiran, S.K.; Sandhya, V.K.; Channabasappa, G.H.; Mishra, A.C.; Mourya, D.T.; MehendalE, S.M. Kyasanur forest disease, India, 2011–2012. Emerg. Inf. Dis. 2013, 19, 27–28. [Google Scholar] [CrossRef]
- Dandawate, C.N. Experiences on the development and field evaluation of vaccine against Kyasanur Forest Disease virus. Proc. Natl. Semin. Vaccine Pune 1980, 103–109. [Google Scholar]
- National Institute of Virology (NIV). Manual of Kyasanur Forest Disease Vaccine Production; National Institute of Virology (NIV): Pune, India, 1980; pp. 1–25. [Google Scholar]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Mourya, D.T.; Pragya, D.Y.; Rajeev, M.; Pradip, V.B.; Prasanna, N.Y.; Sandeep, R.P.; Thakare, J.P.; Mishra, A.C. Diagnosis of Kyasanur Forest Disease by Nested RT-PCR, Real-Time RT-PCR and IgM Capture ELISA. J. Virol. Methods 2012, 186, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Stokes, A.; Bauer, J.H.; Hudson, N.P. The transmission of yellow fever to Macacus rhesus: Preliminary note. J. Am. Med. Assoc. 1928, 90, 253–254. [Google Scholar] [CrossRef]
- Smorodintsev, A.A. Results of the three years’ work of the Soviet medicine on the study of the spring-summer (tayga, tick-borne, endemic) encephalitis. Arkh. Biol. Nauk. 1939, 56, 11–38. [Google Scholar]
- Mansharamani, H.J.; Dandawate, C.N.; Krishnamurthy, B.G. Experimental vaccine against Kyasanur Forest Disease (KFD) virus from tissue culture source I. Indian J. Pathol. Bacteriol. 1967, 10, 9–24. [Google Scholar]
- National Centre for Disease Control (NCDC). Scientific Compendium on of KFD. 2020. Available online: https://monkeyfeverrisk.ceh.ac.uk/sites/default/files/2022-05/NCDC-Consultation-book-3rd-update.pdf (accessed on 5 May 2023).
- Banerjee, K.; Dandawate, C.N.; Bhatt, P.N.; Ramachandra, R.T. Serological response in humans to a formolized Kyasanur Forest disease vaccine. Indian J. Med. Res. 1969, 57, 969–974. [Google Scholar] [PubMed]
- Rodrigues, F.M.; Bhat, H.R.; Prasad, S.R. A new focal outbreak of Kyasanur Forest disease in Belthangady Taluk, South Kanara District, Karnataka State. NIV Bulletin. 1983, 1, 6–7. [Google Scholar]
- Salk, J.E. Poliomyelitis vaccine in the fall of 1955. Am. J. Public Health NIH 1956, 46, 1–14. [Google Scholar] [CrossRef]
- Dandawate, C.N.; Upadhyaya, S.; Banerjee, K. Serological response to formolized Kyasanur forest disease virus vaccine in humans at Sagar and Sorab Talukas of Shimoga district. J. Biol. Stand. 1980, 8, 1–6. [Google Scholar] [CrossRef]
- Institute of Animal Health And Veterinary Biologicals (IAH & VB). Annual Reports (2020); Institute of Animal Health And Veterinary Biologicals (IAH & VB): Karnataka, India, 2020. [Google Scholar]
- Chowdhury, P.; Topno, R.; Khan, S.A.; Mahanta, J. Comparison of β-Propiolactone and Formalin Inactivation on Antigenicity and Immune Response of West Nile Virus. Adv. Virol. 2015, 61, 68–98. [Google Scholar] [CrossRef]
- Fan, Y.C.; Chiu, H.C.; Chen, L.K.; Chang, G.J.; Chiou, S.S. Formalin Inactivation of Japanese Encephalitis Virus Vaccine Alters the Antigenicity and Immunogenicity of a Neutralization Epitope in Envelope Protein Domain III. PLoS Negl. Trop. Dis. 2015, 239, e0004167. [Google Scholar] [CrossRef]
- Kon, T.C.; Onu, A.; Berbecila, L.; Lupulescu, E.; Ghiorgisor, A.; Kersten, G.F.; Cui, Y.Q.; Amorij, J.P.; Vander, P.L. Influenza Vaccine Manufacturing: Effect of Inactivation, Splitting and Site of Manu facturing. Comparison of Influenza Vaccine Production Processes. PLoS ONE 2016, 11, e0150700. [Google Scholar] [CrossRef]
- Mehla, R.; Kumar, S.R.; Yadav, P.; Barde, P.V.; Yergolkar, P.N.; Erickson, B.R.; Carroll, S.A.; Mishra, A.C.; Nichol, S.T.; Mourya, D.T. Recent ancestry of Kyasanur Forest disease virus. Emerg. Inf. Dis. 2009, 15, 1431–1437. [Google Scholar] [CrossRef]
- Yadav, P.D.; Patil, S.; Jadhav, S.M.; Nyayanit, D.A.; Kumar, V.; Jain, S.; Sampath, J.; Mourya, D.T.; Cherian, S.S. Phylogeography of Kyasanur Forest Disease virus in India (1957–2017) reveals evolution and spread in the Western Ghats region. Sci. Rep. 2020, 10, 1966. [Google Scholar] [CrossRef]
- Chandranaik, B.M.; Rathnamma, D.; Patil, S.S.; Kovi, R.C.; Dhawan, J.; Ranganatha, S.; Isloor, S.; Renukaprasad, C.; Prabhudas, K. Development of a probe based real time PCR assay for detection of bovine herpes virus-1 in semen and other clinical samples. Indian. J. Virol. 2013, 24, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Pang, Z.; Li, A.; Li, J.; Qu, J.; He, C.; Zhang, S.; Li, C.; Zhang, Q.; Liang, M.; Li, D. Comprehensive multiplex one-step real-time TaqMan qRT-PCR assays for detection and quantification of hemorrhagic fever viruses. PLoS ONE 2014, 9, e95635. [Google Scholar] [CrossRef]
- Moreira, B.L.C.; Pereira, L.A.; Gimenez, A.P.L.; Inagaki, J.M.F.; Raboni, S.M. Development and validation of a real-time RT-PCR assay for the quantification of rabies virus as quality control of inactivated rabies vaccines. J. Virol. Methods 2019, 270, 46–51. [Google Scholar] [CrossRef]
- Chabaud-Riou, M.; Moreno, N.; Guinchard, F.; Nicolai, M.C.; Niogret-siohan, E.; Sève, N.; Manin, C.; Guinet-morlot, F.; Riou, P. G-protein based ELISA as a potency test for rabies vaccines. J. Biol. 2017, 46, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Chandranaik, B.M.; Renukaprasad, C.; Patil, S.S.; Julie, B.; Giridhar, P.; Venkatesha, M.D.; Byregowda, S.M.; Prabhudas, K. Development of cell culture based inactivated Classical swine fever vaccine. Indian Vet. J. 2011, 88, 16–22. [Google Scholar]
- Mantel, N.; Aguirre, M.; Gulia, S.; Girerd-chambaz, Y.; Colombani, S.; Moste, C.; Barban, V. Standardized quantitative RT-PCR assays for quantitation of yellow fever and chimeric yellow fever-dengue vaccines. J. Virol. Methods 2008, 151, 40–46. [Google Scholar] [CrossRef] [PubMed]
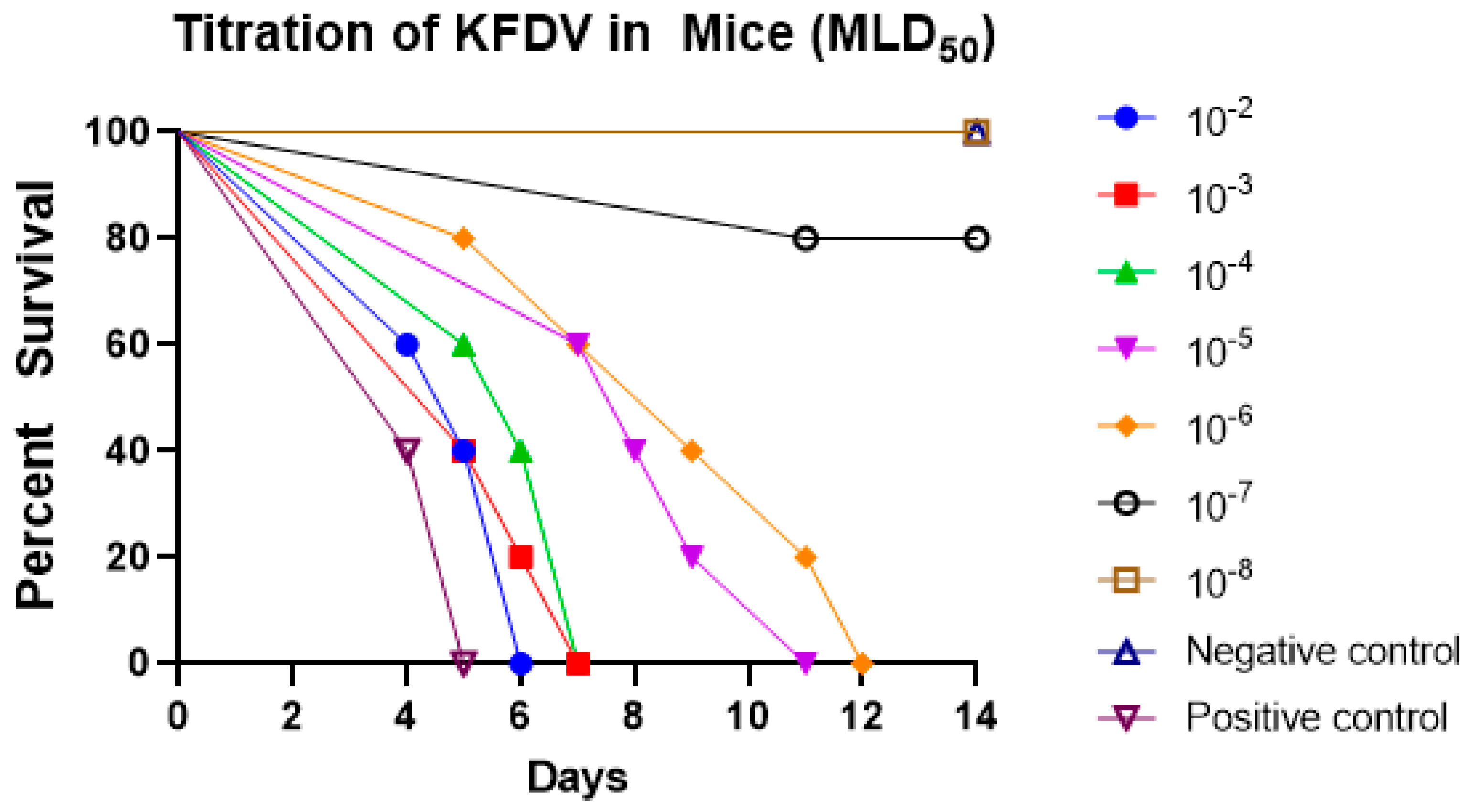
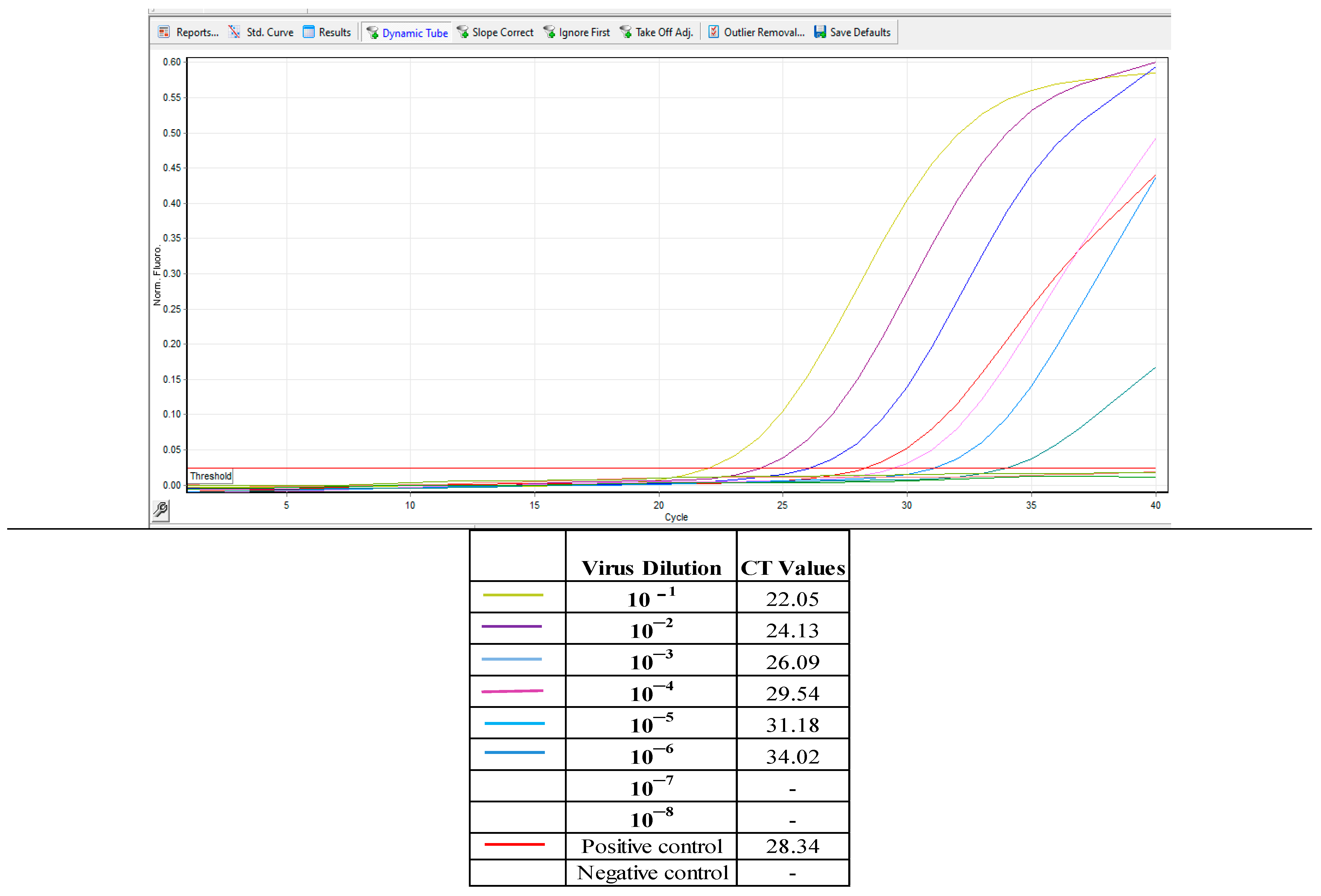
| Virus Dilutions | % Infectivity | CT Values |
|---|---|---|
| 10−1 | 100 | 22.05 |
| 10−2 | 100 | 24.13 |
| 10−3 | 100 | 26.09 |
| 10−4 | 100 | 29.54 |
| 10−5 | 100 | 31.18 |
| 10−6 | 100 | 34.02 |
| 10−7 | 20 | - |
| 10−8 | 0 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Srikanth, U.G.K.; Marinaik, C.B.; Gomes, A.R.; Rathnamma, D.; Byregowda, S.M.; Isloor, S.; Munivenkatarayappa, A.; Venkatesha, M.D.; Rao, S.; Rizwan, A.; et al. Evaluation of Safety and Potency of Kyasanur Forest Disease (KFD) Vaccine Inactivated with Different Concentrations of Formalin and Comparative Evaluation of In Vitro and In Vivo Methods of Virus Titration in KFD Vaccine. Biomedicines 2023, 11, 1871. https://doi.org/10.3390/biomedicines11071871
Srikanth UGK, Marinaik CB, Gomes AR, Rathnamma D, Byregowda SM, Isloor S, Munivenkatarayappa A, Venkatesha MD, Rao S, Rizwan A, et al. Evaluation of Safety and Potency of Kyasanur Forest Disease (KFD) Vaccine Inactivated with Different Concentrations of Formalin and Comparative Evaluation of In Vitro and In Vivo Methods of Virus Titration in KFD Vaccine. Biomedicines. 2023; 11(7):1871. https://doi.org/10.3390/biomedicines11071871
Chicago/Turabian StyleSrikanth, Ullas Gowda K., Chandranaik B. Marinaik, Amitha Reena Gomes, Doddamane Rathnamma, Sonnahallipura M. Byregowda, Shrikrishna Isloor, Archana Munivenkatarayappa, Mudalagiri D. Venkatesha, Suguna Rao, Apsana Rizwan, and et al. 2023. "Evaluation of Safety and Potency of Kyasanur Forest Disease (KFD) Vaccine Inactivated with Different Concentrations of Formalin and Comparative Evaluation of In Vitro and In Vivo Methods of Virus Titration in KFD Vaccine" Biomedicines 11, no. 7: 1871. https://doi.org/10.3390/biomedicines11071871
APA StyleSrikanth, U. G. K., Marinaik, C. B., Gomes, A. R., Rathnamma, D., Byregowda, S. M., Isloor, S., Munivenkatarayappa, A., Venkatesha, M. D., Rao, S., Rizwan, A., & Hegde, R. (2023). Evaluation of Safety and Potency of Kyasanur Forest Disease (KFD) Vaccine Inactivated with Different Concentrations of Formalin and Comparative Evaluation of In Vitro and In Vivo Methods of Virus Titration in KFD Vaccine. Biomedicines, 11(7), 1871. https://doi.org/10.3390/biomedicines11071871







