Insights into the Potential Impact of Quetiapine on the Microglial Trajectory and Inflammatory Response in Organotypic Cortical Cultures Derived from Rat Offspring
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Prenatal Exposure to LPS
2.3. Organotypic Cortical Cultures
2.4. Chemicals and Drugs
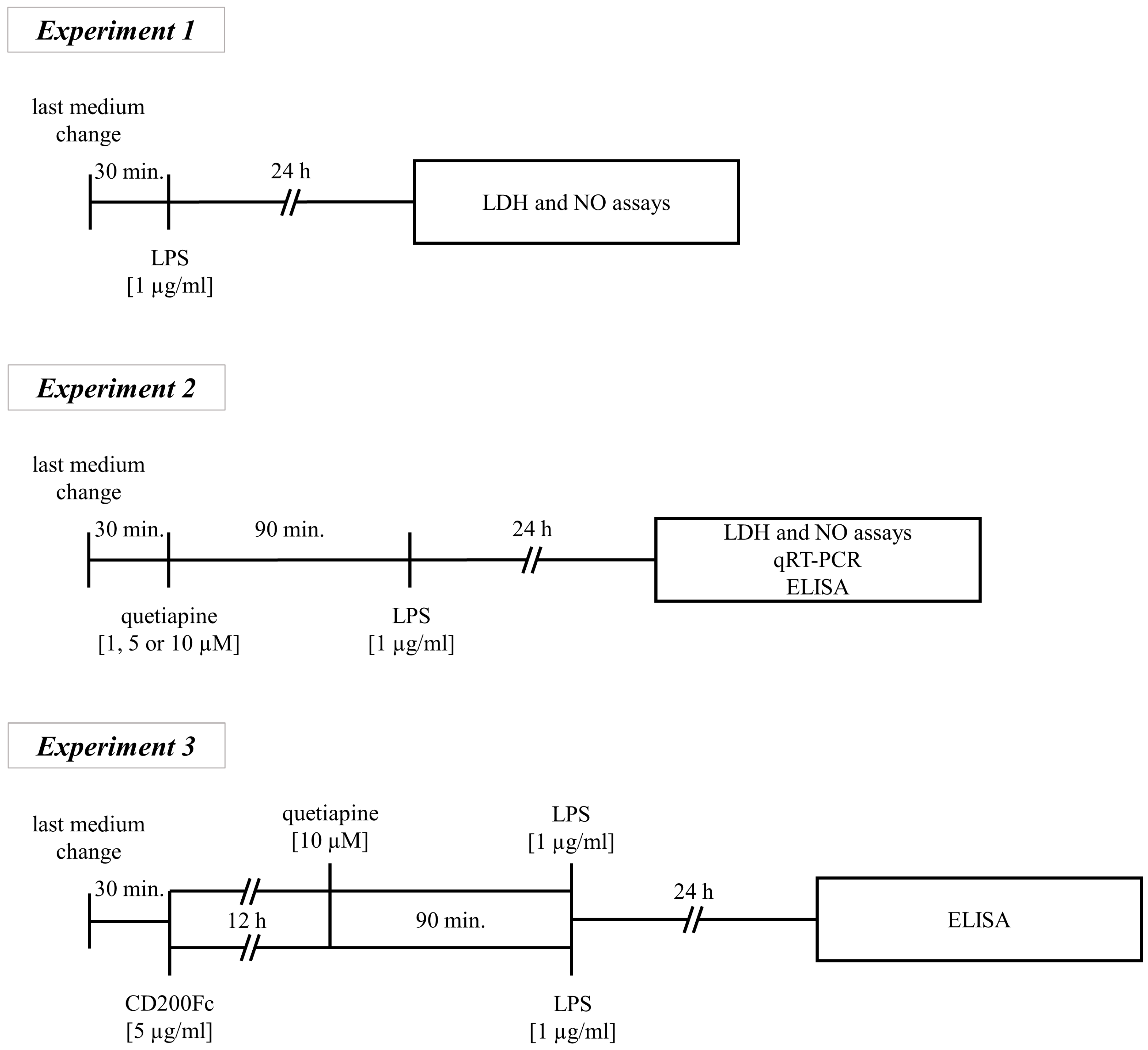
2.5. Treatment of the OCCs
- Experiment 1
- Experiment 2
- Experiment 3
2.6. Culture Collection and Sample Preparation
2.7. Lactate Dehydrogenase Release
2.8. Nitric Oxide Release
2.9. Enzyme-Linked Immunosorbent Assay
2.10. Quantitative Real-Time Polymerase Chain Reaction
2.11. Statistical Analysis
3. Results
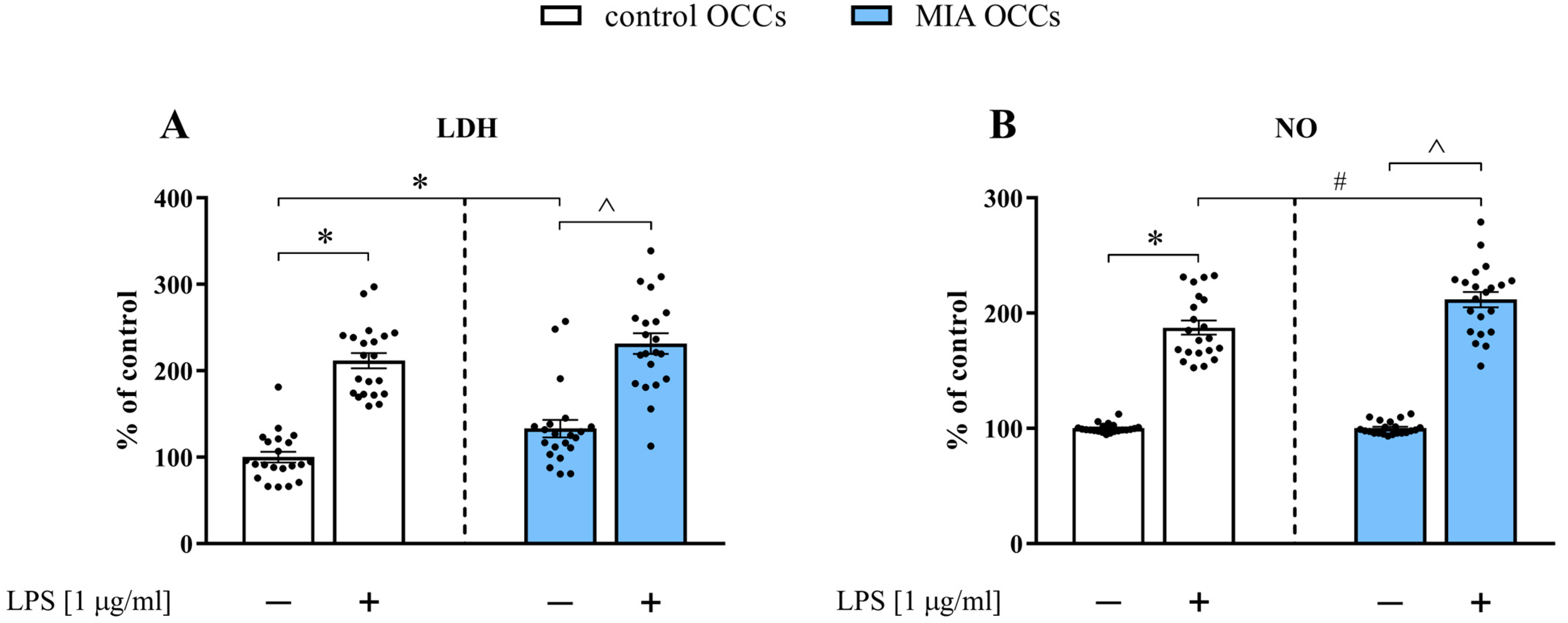
3.1. Release of Lactate Dehydrogenase and Nitric Oxide in Control and MIA OCCs under Basal and LPS-Induced Conditions
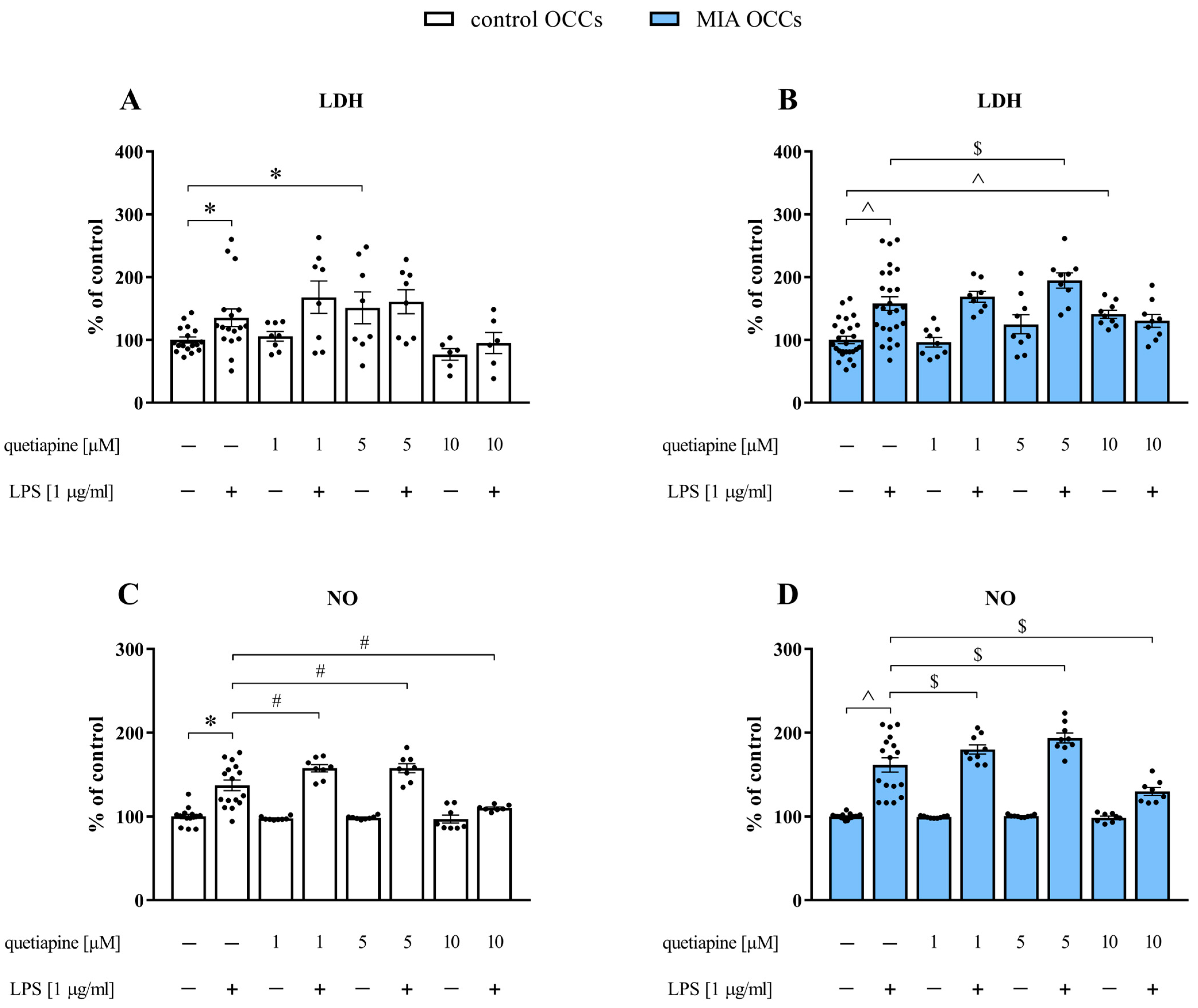
3.2. The Impact of Different Doses of Quetiapine on Lactate Dehydrogenase and Nitric Oxide Release in Control and MIA OCCs under Basal and LPS-Induced Conditions
3.3. The Impact of Quetiapine on the mRNA Expression of the Cd200-Cd200r and Cx3cl1-Cx3cr1 Axes in Control and MIA OCCs under Basal and LPS-Induced Conditions

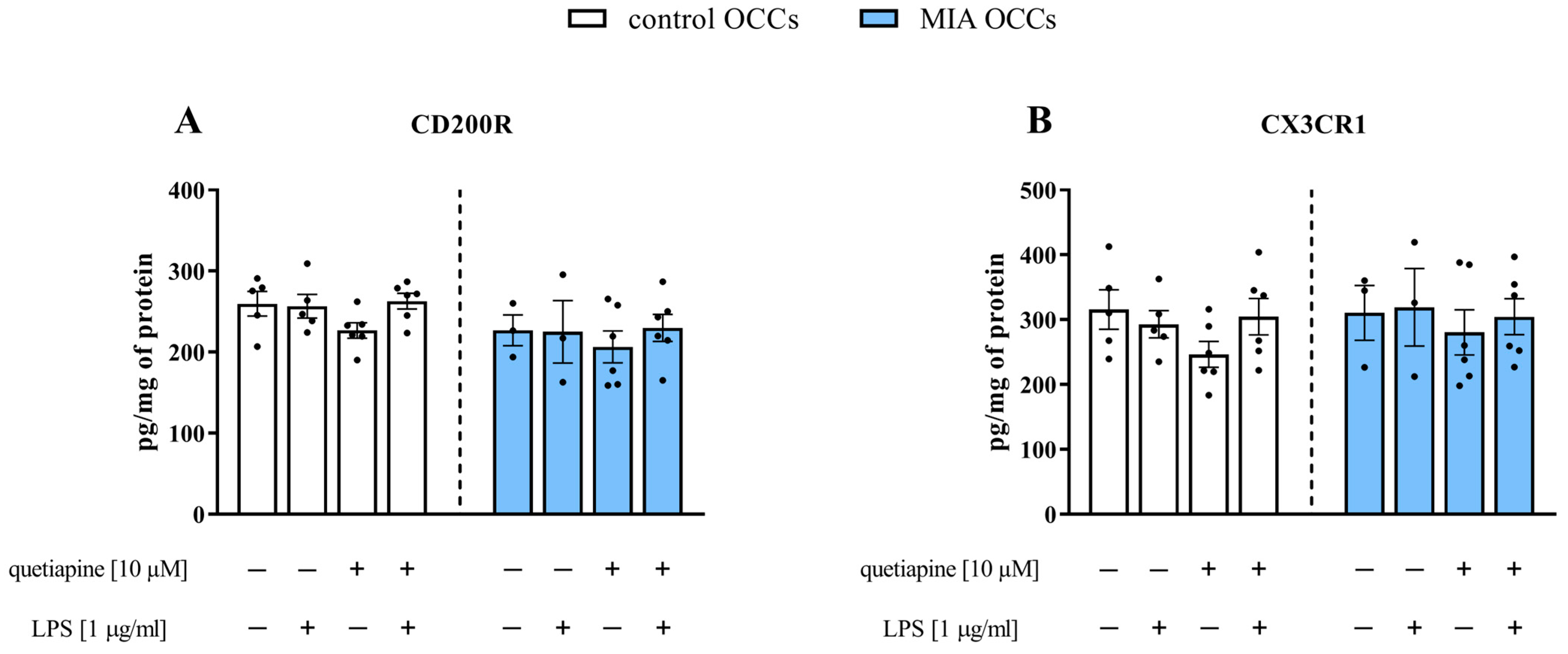
3.4. The Impact of Quetiapine on the CD200R and CX3CR1 Protein Levels in Control and MIA OCCs under Basal and LPS-Induced Conditions
3.5. The Impact of Quetiapine on the mRNA Expression of Microglial Markers in Control and MIA OCCs under Basal and LPS-Induced Conditions

3.6. The Impact of Quetiapine and CD200Fc on IL-6 and IL-10 Protein Levels in Control and MIA OCCs under Basal and LPS-Induced Conditions

4. Discussion
4.1. Maternal Immune Activation Affects Lactate Dehydrogenase Release in Organotypic Cortical Cultures and Partially Their Response to Stimulation with Lipopolysaccharide
4.2. Quetiapine Exerts Immunomodulatory Effects in Organotypic Cortical Cultures
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hudepohl, N.S.; Nasrallah, H.A. Antipsychotic Drugs. Handb. Clin. Neurol. 2012, 106, 657–667. [Google Scholar]
- Kaar, S.J.; Natesan, S.; McCutcheon, R.; Howes, O.D. Antipsychotics: Mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacology 2020, 172, 107704. [Google Scholar] [CrossRef]
- Meltzer, H.Y. Update on Typical and Atypical Antipsychotic Drugs. Annu. Rev. Med. 2013, 64, 393–406. [Google Scholar] [CrossRef]
- Stępnicki, P.; Kondej, M.; Kaczor, A.A. Current Concepts and Treatments of Schizophrenia. Molecules 2018, 23, 2087. [Google Scholar] [CrossRef]
- Kane, J.M.; Correll, C.U. Past and Present Progress in the Pharmacologic Treatment of Schizophrenia. J. Clin. Psychiatry 2010, 71, 1115–1124. [Google Scholar] [CrossRef]
- Kusumi, I.; Boku, S.; Takahashi, Y. Psychopharmacology of atypical antipsychotic drugs: From the receptor binding profile to neuroprotection and neurogenesis. Psychiatry Clin. Neurosci. 2015, 69, 243–258. [Google Scholar] [CrossRef]
- Adityanjee; Schulz, S.C. Clinical use of quetiapine in disease states other than schizophrenia. J. Clin. Psychiatry 2002, 63 (Suppl. S1), 32–38. [Google Scholar]
- Suttajit, S.; Srisurapanont, M.; Maneeton, N.; Maneeton, B. Quetiapine for acute bipolar depression: A systematic review and meta-analysis. Drug Des. Dev. Ther. 2014, 8, 827–838. [Google Scholar] [CrossRef]
- Chen, J.J.; Hua, H.; Massihi, L.; Portillo, I.; Alipour, A.; Ondo, W.; Dashtipour, K. Systematic Literature Review of Quetiapine for the Treatment of Psychosis in Patients With Parkinsonism. J. Neuropsychiatry Clin. Neurosci. 2019, 31, 188–195. [Google Scholar] [CrossRef]
- Kasper, S.; Tauscher, J.; Heiden, A. Quetiapine: Efficacy and tolerability in schizophrenia. Eur. Neuropsychopharmacol. 2001, 11, S405–S413. [Google Scholar] [CrossRef]
- Leucht, S.; Cipriani, A.; Spineli, L.; Mavridis, D.; Örey, D.; Richter, F.; Samara, M.; Barbui, C.; Engel, R.R.; Geddes, J.R.; et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet 2013, 382, 951–962. [Google Scholar] [CrossRef]
- Cheer, S.M.; Wagstaff, A.J. Quetiapine. CNS Drugs 2004, 18, 173–199. [Google Scholar] [CrossRef]
- Shoemaker, J.M.; Pitcher, L.; Noh, H.R.; Swerdlow, N.R. Quetiapine produces a prolonged reversal of the sensorimotor gating-disruptive effects of basolateral amygdala lesions in rats. Behav. Neurosci. 2003, 117, 136–143. [Google Scholar] [CrossRef]
- Carreño, F.; Helfer, V.E.; Staudt, K.J.; Paese, K.; Meyer, F.S.; Herrmann, A.P.; Guterres, S.S.; Rates, S.M.K.; Dalla Costa, T. Quetiapine lipid core nanocapsules restore prepulse inhibition deficits in a neurodevelopmental model of schizophrenia in male and female rats. Schizophr. Res. 2020, 218, 173–179. [Google Scholar] [CrossRef]
- Chamera, K.; Curzytek, K.; Kamińska, K.; Trojan, E.; Basta-Kaim, A. Quetiapine Ameliorates MIA-Induced Impairment of Sensorimotor Gating: Focus on Neuron-Microglia Communication and the Inflammatory Response in the Frontal Cortex of Adult Offspring of Wistar Rats. Cells 2022, 11, 2788. [Google Scholar] [CrossRef]
- He, J.; Zu, Q.; Wen, C.; Liu, Q.; You, P.; Li, X.; Wang, W. Quetiapine Attenuates Schizophrenia-Like Behaviors and Demyelination in a MK-801–Induced Mouse Model of Schizophrenia. Front. Psychiatry 2020, 11, 843. [Google Scholar] [CrossRef]
- Baldwin, C.M.; Scott, L.J. Quetiapine Extended Release. CNS Drugs 2009, 23, 261–269. [Google Scholar] [CrossRef]
- Mauri, M.C.; Paletta, S.; Maffini, M.; Colasanti, A.; Dragogna, F.; Di Pace, C.; Altamura, A.C. Clinical pharmacology of atypical antipsychotics: An update. EXCLI J. 2014, 13, 1163–1191. [Google Scholar]
- Bian, Q.; Kato, T.; Monji, A.; Hashioka, S.; Mizoguchi, Y.; Horikawa, H.; Kanba, S. The effect of atypical antipsychotics, perospirone, ziprasidone and quetiapine on microglial activation induced by interferon-γ. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2008, 32, 42–48. [Google Scholar] [CrossRef]
- Shao, Y.; Peng, H.; Huang, Q.; Kong, J.; Xu, H. Quetiapine mitigates the neuroinflammation and oligodendrocyte loss in the brain of C57BL/6 mouse following cuprizone exposure for one week. Eur. J. Pharmacol. 2015, 765, 249–257. [Google Scholar] [CrossRef]
- Zhao, Z.; Luo, G.; Liu, M.; Guo, H.; Xue, M.; Wang, X.; Li, X.-M.; He, J. Quetiapine reduces microglial number in the hippocampus of a transgenic mouse model of Alzheimer’s disease. Neuroreport 2014, 25, 870–874. [Google Scholar] [CrossRef]
- Zhu, S.; Shi, R.; Li, V.; Wang, J.-F.; Zhang, R.; Tempier, A.; He, J.; Kong, J.; Wang, J.-F.; Li, X.-M. Quetiapine Attenuates Glial Activation and Proinflammatory Cytokines in APP/PS1 Transgenic Mice via Inhibition of Nuclear Factor-κB Pathway. Int. J. Neuropsychopharmacol. 2015, 18, pyu022. [Google Scholar] [CrossRef]
- Szepesi, Z.; Manouchehrian, O.; Bachiller, S.; Deierborg, T. Bidirectional Microglia–Neuron Communication in Health and Disease. Front. Cell. Neurosci. 2018, 12, 323. [Google Scholar] [CrossRef]
- Chamera, K.; Trojan, E.; Szuster-Głuszczak, M.; Basta-Kaim, A. The Potential Role of Dysfunctions in Neuron-Microglia Communication in the Pathogenesis of Brain Disorders. Curr. Neuropharmacol. 2020, 18, 408–430. [Google Scholar] [CrossRef]
- Gorczynski, R.M.; Cattral, M.S.; Chen, Z.; Hu, J.; Lei, J.; Min, W.P.; Yu, G.; Ni, J. An immunoadhesin incorporating the molecule OX-2 is a potent immunosuppressant that prolongs allo- and xenograft survival. J. Immunol. 1999, 163, 1654–1660. [Google Scholar] [CrossRef]
- Erin, N.; Tanrıöver, G.; Curry, A.; Akman, M.; Duymuş, Ö.; Gorczynski, R. CD200fc enhances anti-tumoral immune response and inhibits visceral metastasis of breast carcinoma. Oncotarget 2018, 9, 19147–19158. [Google Scholar] [CrossRef]
- Humpel, C. Organotypic Brain Slice Cultures. Curr. Protoc. Immunol. 2018, 123, e59. [Google Scholar] [CrossRef]
- Romero, E.; Ali, C.; Molina-Holgado, E.; Castellano, B.; Guaza, C.; Borrell, J. Neurobehavioral and Immunological Consequences of Prenatal Immune Activation in Rats. Influence of Antipsychotics. Neuropsychopharmacology 2007, 32, 1791–1804. [Google Scholar] [CrossRef]
- Basta-Kaim, A.; Szczęsny, E.; Leśkiewicz, M.; Głombik, K.; Ślusarczyk, J.; Budziszewska, B.; Regulska, M.; Kubera, M.; Nowak, W.; Wędzony, K.; et al. Maternal immune activation leads to age-related behavioral and immunological changes in male rat offspring—The effect of antipsychotic drugs. Pharmacol. Rep. 2012, 64, 1400–1410. [Google Scholar] [CrossRef]
- Chamera, K.; Kotarska, K.; Szuster-Głuszczak, M.; Trojan, E.; Skórkowska, A.; Pomierny, B.; Krzyżanowska, W.; Bryniarska, N.; Basta-Kaim, A. The prenatal challenge with lipopolysaccharide and polyinosinic:polycytidylic acid disrupts CX3CL1-CX3CR1 and CD200-CD200R signalling in the brains of male rat offspring: A link to schizophrenia-like behaviours. J. Neuroinflamm. 2020, 17, 247. [Google Scholar] [CrossRef]
- Vojtechova, I.; Maleninska, K.; Kutna, V.; Klovrza, O.; Tuckova, K.; Petrasek, T.; Stuchlik, A. Behavioral Alterations and Decreased Number of Parvalbumin-Positive Interneurons in Wistar Rats after Maternal Immune Activation by Lipopolysaccharide: Sex Matters. Int. J. Mol. Sci. 2021, 22, 3274. [Google Scholar] [CrossRef] [PubMed]
- Monte, A.S.; Mello, B.S.F.; Borella, V.C.M.; da Silva Araujo, T.; da Silva, F.E.R.; de Sousa, F.C.F.; de Oliveira, A.C.P.; Gama, C.S.; Seeman, M.V.; Vasconcelos, S.M.M.; et al. Two-hit model of schizophrenia induced by neonatal immune activation and peripubertal stress in rats: Study of sex differences and brain oxidative alterations. Behav. Brain Res. 2017, 331, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Chamera, K.; Szuster-Głuszczak, M.; Trojan, E.; Basta-Kaim, A. Maternal Immune Activation Sensitizes Male Offspring Rats to Lipopolysaccharide-Induced Microglial Deficits Involving the Dysfunction of CD200–CD200R and CX3CL1–CX3CR1 Systems. Cells 2020, 9, 1676. [Google Scholar] [CrossRef] [PubMed]
- Basta-Kaim, A.; Fijał, K.; Budziszewska, B.; Regulska, M.; Leśkiewicz, M.; Kubera, M.; Gołembiowska, K.; Lasoń, W.; Wędzony, K. Prenatal lipopolysaccharide treatment enhances MK-801-induced psychotomimetic effects in rats. Pharmacol. Biochem. Behav. 2011, 98, 241–249. [Google Scholar] [CrossRef]
- Basta-Kaim, A.; Budziszewska, B.; Leśkiewicz, M.; Fijał, K.; Regulska, M.; Kubera, M.; Wȩdzony, K.; Lasoń, W. Hyperactivity of the hypothalamus-pituitary-adrenal axis in lipopolysaccharide-induced neurodevelopmental model of schizophrenia in rats: Effects of antipsychotic drugs. Eur. J. Pharmacol. 2011, 650, 586–595. [Google Scholar] [CrossRef]
- Stoppini, L.; Buchs, P.-A.; Muller, D. A simple method for organotypic cultures of nervous tissue. J. Neurosci. Methods 1991, 37, 173–182. [Google Scholar] [CrossRef]
- Nicholls, S.M.; Copland, D.A.; Vitova, A.; Kuffova, L.; Forrester, J.V.; Dick, A.D. Local targeting of the CD200-CD200R axis does not promote corneal graft survival. Exp. Eye Res. 2015, 130, 1–8. [Google Scholar] [CrossRef]
- Trojan, E.; Tylek, K.; Leśkiewicz, M.; Lasoń, W.; Brandenburg, L.-O.; Leopoldo, M.; Lacivita, E.; Basta-Kaim, A. The N-Formyl Peptide Receptor 2 (FPR2) Agonist MR-39 Exhibits Anti-Inflammatory Activity in LPS-Stimulated Organotypic Hippocampal Cultures. Cells 2021, 10, 1524. [Google Scholar] [CrossRef]
- Chomczynski, P. A reagent for the single-step simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. Biotechniques 1993, 15, 532–534, 536–537. [Google Scholar]
- Comer, A.L.; Carrier, M.; Tremblay, M.-È.; Cruz-Martín, A. The Inflamed Brain in Schizophrenia: The Convergence of Genetic and Environmental Risk Factors That Lead to Uncontrolled Neuroinflammation. Front. Cell. Neurosci. 2020, 14, 274. [Google Scholar] [CrossRef]
- Kabba, J.A.; Xu, Y.; Christian, H.; Ruan, W.; Chenai, K.; Xiang, Y.; Zhang, L.; Saavedra, J.M.; Pang, T. Microglia: Housekeeper of the Central Nervous System. Cell. Mol. Neurobiol. 2018, 38, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Boksa, P. Effects of prenatal infection on brain development and behavior: A review of findings from animal models. Brain. Behav. Immun. 2010, 24, 881–897. [Google Scholar] [CrossRef] [PubMed]
- Estes, M.L.; McAllister, A.K. Maternal immune activation: Implications for neuropsychiatric disorders. Science. 2016, 353, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.S.; Meyer, U. Maternal Immune Activation and Neuropsychiatric Illness: A Translational Research Perspective. Am. J. Psychiatry 2018, 175, 1073–1083. [Google Scholar] [CrossRef]
- Basta-Kaim, A.; Fijał, K.; Ślusarczyk, J.; Trojan, E.; Głombik, K.; Budziszewska, B.; Leśkiewicz, M.; Regulska, M.; Kubera, M.; Lasoń, W.; et al. Prenatal administration of lipopolysaccharide induces sex-dependent changes in glutamic acid decarboxylase and parvalbumin in the adult rat brain. Neuroscience 2015, 287, 78–92. [Google Scholar] [CrossRef]
- Zager, A.; Pinheiro, M.L.; Ferraz-de-Paula, V.; Ribeiro, A.; Palermo-Neto, J. Increased cell-mediated immunity in male mice offspring exposed to maternal immune activation during late gestation. Int. Immunopharmacol. 2013, 17, 633–637. [Google Scholar] [CrossRef]
- Savareh, E.; Davoodian, N.; Mousaviyan, R.; Ghasemi-Kasman, M.; Atashabparvar, A.; Eftekhar, E. Prenatal Zinc Supplementation Ameliorates Hippocampal Astrocytes Activation and Inflammatory Cytokines Expression Induced by Lipopolysaccharide in a Rat Model of Maternal Immune Activation. Basic Clin. Neurosci. J. 2022, 13, 335–348. [Google Scholar] [CrossRef]
- Paolicelli, R.C.; Bisht, K.; Tremblay, M.-Ã. Fractalkine regulation of microglial physiology and consequences on the brain and behavior. Front. Cell. Neurosci. 2014, 8, 129. [Google Scholar] [CrossRef]
- Wohleb, E.S. Neuron–Microglia Interactions in Mental Health Disorders: “For Better, and For Worse”. Front. Immunol. 2016, 7, 544. [Google Scholar] [CrossRef]
- Amodeo, D.A.; Lai, C.-Y.; Hassan, O.; Mukamel, E.A.; Behrens, M.M.; Powell, S.B. Maternal immune activation impairs cognitive flexibility and alters transcription in frontal cortex. Neurobiol. Dis. 2019, 125, 211–218. [Google Scholar] [CrossRef]
- Tendilla-Beltrán, H.; del Carmen Sanchez-Islas, N.; Marina-Ramos, M.; Leza, J.C.; Flores, G. The prefrontal cortex as a target for atypical antipsychotics in schizophrenia, lessons of neurodevelopmental animal models. Prog. Neurobiol. 2021, 199, 101967. [Google Scholar] [CrossRef] [PubMed]
- Hanson, K.L.; Grant, S.E.; Funk, L.H.; Schumann, C.M.; Bauman, M.D. Impact of Maternal Immune Activation on Nonhuman Primate Prefrontal Cortex Development: Insights for Schizophrenia. Biol. Psychiatry 2022, 92, 460–469. [Google Scholar] [CrossRef] [PubMed]
- Humpel, C. Organotypic brain slice cultures: A review. Neuroscience 2015, 305, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Beach, R.L.; Bathgate, S.L.; Cotman, C.W. Identification of cell types in rat hippocampal slices maintained in organotypic cultures. Dev. Brain Res. 1982, 3, 3–20. [Google Scholar] [CrossRef]
- Staal, J.A.; Alexander, S.R.; Liu, Y.; Dickson, T.D.; Vickers, J.C. Characterization of Cortical Neuronal and Glial Alterations during Culture of Organotypic Whole Brain Slices from Neonatal and Mature Mice. PLoS ONE 2011, 6, e22040. [Google Scholar] [CrossRef]
- Croft, C.L.; Futch, H.S.; Moore, B.D.; Golde, T.E. Organotypic brain slice cultures to model neurodegenerative proteinopathies. Mol. Neurodegener. 2019, 14, 45. [Google Scholar] [CrossRef]
- Ślusarczyk, J.; Piotrowski, M.; Szczepanowicz, K.; Regulska, M.; Leśkiewicz, M.; Warszyński, P.; Budziszewska, B.; Lasoń, W.; Basta-Kaim, A. Nanocapsules with Polyelectrolyte Shell as a Platform for 1,25-dihydroxyvitamin D3 Neuroprotection: Study in Organotypic Hippocampal Slices. Neurotox. Res. 2016, 30, 581–592. [Google Scholar] [CrossRef]
- Basta-Kaim, A.; Ślusarczyk, J.; Szczepanowicz, K.; Warszyński, P.; Leśkiewicz, M.; Regulska, M.; Trojan, E.; Lasoń, W. Protective effects of polydatin in free and nanocapsulated form on changes caused by lipopolysaccharide in hippocampal organotypic cultures. Pharmacol. Rep. 2019, 71, 603–613. [Google Scholar] [CrossRef]
- Głombik, K.; Trojan, E.; Kurek, A.; Budziszewska, B.; Basta-Kaim, A. Inflammatory Consequences of Maternal Diabetes on the Offspring Brain: A Hippocampal Organotypic Culture Study. Neurotox. Res. 2019, 36, 357–375. [Google Scholar] [CrossRef]
- Doma, M.K.; Parker, R. RNA Quality Control in Eukaryotes. Cell 2007, 131, 660–668. [Google Scholar] [CrossRef]
- Houseley, J.; Tollervey, D. The Many Pathways of RNA Degradation. Cell 2009, 136, 763–776. [Google Scholar] [CrossRef] [PubMed]
- Frank, M.G.; Annis, J.L.; Watkins, L.R.; Maier, S.F. Glucocorticoids mediate stress induction of the alarmin HMGB1 and reduction of the microglia checkpoint receptor CD200R1 in limbic brain structures. Brain. Behav. Immun. 2019, 80, 678–687. [Google Scholar] [CrossRef] [PubMed]
- Le, C.; Hao, X.; Li, J.; Zhong, J.; Lin, H.; Zhou, Y.; Travis, Z.D.; Tong, L.; Gao, F. CD200Fc Improves Neurological Function by Protecting the Blood–brain Barrier after Intracerebral Hemorrhage. Cell Transplant. 2019, 28, 1321–1328. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Cherwinski, H.; Sedgwick, J.D.; Phillips, J.H. Molecular Mechanisms of CD200 Inhibition of Mast Cell Activation. J. Immunol. 2004, 173, 6786–6793. [Google Scholar] [CrossRef]
- Frank, M.G.; Fonken, L.K.; Annis, J.L.; Watkins, L.R.; Maier, S.F. Stress disinhibits microglia via down-regulation of CD200R: A mechanism of neuroinflammatory priming. Brain. Behav. Immun. 2018, 69, 62–73. [Google Scholar] [CrossRef]
- Chamera, K.; Trojan, E.; Kotarska, K.; Szuster-Głuszczak, M.; Bryniarska, N.; Tylek, K.; Basta-Kaim, A. Role of Polyinosinic:Polycytidylic Acid-Induced Maternal Immune Activation and Subsequent Immune Challenge in the Behaviour and Microglial Cell Trajectory in Adult Offspring: A Study of the Neurodevelopmental Model of Schizophrenia. Int. J. Mol. Sci. 2021, 22, 1558. [Google Scholar] [CrossRef]
- Smolders, S.; Smolders, S.M.T.; Swinnen, N.; Gärtner, A.; Rigo, J.-M.; Legendre, P.; Brône, B. Maternal immune activation evoked by polyinosinic:polycytidylic acid does not evoke microglial cell activation in the embryo. Front. Cell. Neurosci. 2015, 9, 301. [Google Scholar] [CrossRef]
- Giovanoli, S.; Weber-Stadlbauer, U.; Schedlowski, M.; Meyer, U.; Engler, H. Prenatal immune activation causes hippocampal synaptic deficits in the absence of overt microglia anomalies. Brain. Behav. Immun. 2016, 55, 25–38. [Google Scholar] [CrossRef]
- Tidball, J.G.; Villalta, S.A. Regulatory interactions between muscle and the immune system during muscle regeneration. Am. J. Physiol. Integr. Comp. Physiol. 2010, 298, R1173–R1187. [Google Scholar] [CrossRef]
- Stakenborg, M.; Abdurahiman, S.; De Simone, V.; Goverse, G.; Stakenborg, N.; van Baarle, L.; Wu, Q.; Pirottin, D.; Kim, J.-S.; Chappell-Maor, L.; et al. Enteric glial cells favor accumulation of anti-inflammatory macrophages during the resolution of muscularis inflammation. Mucosal Immunol. 2022, 15, 1296–1308. [Google Scholar] [CrossRef]
- Lee, S.J.; Evers, S.; Roeder, D.; Parlow, A.F.; Risteli, J.; Risteli, L.; Lee, Y.C.; Feizi, T.; Langen, H.; Nussenzweig, M.C. Mannose Receptor-Mediated Regulation of Serum Glycoprotein Homeostasis. Science 2002, 295, 1898–1901. [Google Scholar] [CrossRef] [PubMed]
- Porcheray, F.; Viaud, S.; Rimaniol, A.-C.; Léone, C.; Samah, B.; Dereuddre-Bosquet, N.; Dormont, D.; Gras, G. Macrophage activation switching: An asset for the resolution of inflammation. Clin. Exp. Immunol. 2005, 142, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Grolli, R.E.; Bertollo, A.G.; Behenck, J.P.; de Araujo Borba, L.; Plissari, M.E.; Soares, S.J.B.; Manica, A.; da Silva Joaquim, L.; Petronilho, F.; Quevedo, J.; et al. Quetiapine effect on depressive-like behaviors, oxidative balance, and inflammation in serum of rats submitted to chronic stress. Naunyn-Schmiedeberg’s. Arch. Pharmacol. 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Wolf, J.; Rose-John, S.; Garbers, C. Interleukin-6 and its receptors: A highly regulated and dynamic system. Cytokine 2014, 70, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Aliyu, M.; Zohora, F.T.; Anka, A.U.; Ali, K.; Maleknia, S.; Saffarioun, M.; Azizi, G. Interleukin-6 cytokine: An overview of the immune regulation, immune dysregulation, and therapeutic approach. Int. Immunopharmacol. 2022, 111, 109130. [Google Scholar] [CrossRef]
- Hunter, C.A.; Jones, S.A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 2015, 16, 448–457. [Google Scholar] [CrossRef]
- Bi, X.; Yan, B.; Fang, S.; Yang, Y.; He, J.; Li, X.-M.; Kong, J. Quetiapine regulates neurogenesis in ischemic mice by inhibiting NF- κ B p65/p50 expression. Neurol. Res. 2009, 31, 159–166. [Google Scholar] [CrossRef]
- Panizzutti, B.; Bortolasci, C.C.; Spolding, B.; Kidnapillai, S.; Connor, T.; Richardson, M.F.; Truong, T.T.T.; Liu, Z.S.J.; Morris, G.; Gray, L.; et al. Transcriptional Modulation of the Hippo Signaling Pathway by Drugs Used to Treat Bipolar Disorder and Schizophrenia. Int. J. Mol. Sci. 2021, 22, 7164. [Google Scholar] [CrossRef]
- Burmeister, A.R.; Marriott, I. The Interleukin-10 Family of Cytokines and Their Role in the CNS. Front. Cell. Neurosci. 2018, 12, 458. [Google Scholar] [CrossRef]
- Jaehne, E.J.; Corrigan, F.; Toben, C.; Jawahar, M.C.; Baune, B.T. The effect of the antipsychotic drug quetiapine and its metabolite norquetiapine on acute inflammation, memory and anhedonia. Pharmacol. Biochem. Behav. 2015, 135, 136–144. [Google Scholar] [CrossRef]
- Ahmed, S.T.; Ivashkiv, L.B. Inhibition of IL-6 and IL-10 Signaling and Stat Activation by Inflammatory and Stress Pathways. J. Immunol. 2000, 165, 5227–5237. [Google Scholar] [CrossRef]
- Minogue, A.M.; Barrett, J.P.; Lynch, M.A. LPS-induced release of IL-6 from glia modulates production of IL-1β in a JAK2-dependent manner. J. Neuroinflamm. 2012, 9, 629. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wang, J.; Yang, W.; Qi, X.; Lan, L.; Luo, L.; Yin, Z. Bergapten prevents lipopolysaccharide-induced inflammation in RAW264.7 cells through suppressing JAK/STAT activation and ROS production and increases the survival rate of mice after LPS challenge. Int. Immunopharmacol. 2017, 48, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Turra, B.O.; Barbisan, F.; Azzolin, V.F.; Teixeira, C.F.; Flores, T.; Braun, L.E.; de Oliveira Nerys, D.A.; Rissi, V.B.; de Oliveira Alves, A.; Assmann, C.E.; et al. Unmetabolized quetiapine exerts an in vitro effect on innate immune cells by modulating inflammatory response and neutrophil extracellular trap formation. Biomed. Pharmacother. 2020, 131, 110497. [Google Scholar] [CrossRef] [PubMed]
- Cox, F.F.; Carney, D.; Miller, A.-M.; Lynch, M.A. CD200 fusion protein decreases microglial activation in the hippocampus of aged rats. Brain. Behav. Immun. 2012, 26, 789–796. [Google Scholar] [CrossRef]
- Jiang, L.; Xu, F.; He, W.; Chen, L.; Zhong, H.; Wu, Y.; Zeng, S.; Li, L.; Li, M. CD200Fc reduces TLR4-mediated inflammatory responses in LPS-induced rat primary microglial cells via inhibition of the NF-κB pathway. Inflamm. Res. 2016, 65, 521–532. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chamera, K.; Curzytek, K.; Kamińska, K.; Trojan, E.; Leśkiewicz, M.; Tylek, K.; Regulska, M.; Basta-Kaim, A. Insights into the Potential Impact of Quetiapine on the Microglial Trajectory and Inflammatory Response in Organotypic Cortical Cultures Derived from Rat Offspring. Biomedicines 2023, 11, 1405. https://doi.org/10.3390/biomedicines11051405
Chamera K, Curzytek K, Kamińska K, Trojan E, Leśkiewicz M, Tylek K, Regulska M, Basta-Kaim A. Insights into the Potential Impact of Quetiapine on the Microglial Trajectory and Inflammatory Response in Organotypic Cortical Cultures Derived from Rat Offspring. Biomedicines. 2023; 11(5):1405. https://doi.org/10.3390/biomedicines11051405
Chicago/Turabian StyleChamera, Katarzyna, Katarzyna Curzytek, Kinga Kamińska, Ewa Trojan, Monika Leśkiewicz, Kinga Tylek, Magdalena Regulska, and Agnieszka Basta-Kaim. 2023. "Insights into the Potential Impact of Quetiapine on the Microglial Trajectory and Inflammatory Response in Organotypic Cortical Cultures Derived from Rat Offspring" Biomedicines 11, no. 5: 1405. https://doi.org/10.3390/biomedicines11051405
APA StyleChamera, K., Curzytek, K., Kamińska, K., Trojan, E., Leśkiewicz, M., Tylek, K., Regulska, M., & Basta-Kaim, A. (2023). Insights into the Potential Impact of Quetiapine on the Microglial Trajectory and Inflammatory Response in Organotypic Cortical Cultures Derived from Rat Offspring. Biomedicines, 11(5), 1405. https://doi.org/10.3390/biomedicines11051405




