Abstract
Cell-based therapies using periodontal ligament stromal cells (PDLSC) for periodontal regeneration may represent an alternative source for mesenchymal stromal cells (MSC) to MSC derived from bone marrow (MSC(M)) and adipose tissue (MSC(AT)). We aimed to characterize the osteogenic/periodontal potential of PDLSC in comparison to MSC(M) and MSC(AT). PDLSC were obtained from surgically extracted healthy human third molars, while MSC(M) and MSC(AT) were obtained from a previously established cell bank. Flow cytometry, immunocytochemistry, and cell proliferation analyses provided cellular characteristics from each group. Cells from the three groups presented MSC-like morphology, MSC-related marker expression, and multilineage differentiation capacity (adipogenic, chondrogenic, and osteogenic). In this study, PDLSC expressed osteopontin, osteocalcin, and asporin, while MSC(M) and MSC(AT) did not. Of note, only PDLSC expressed CD146, a marker previously applied to identify PDLSC, and presented higher proliferative potential compared to MSC(M) and MSC(AT). Upon osteogenic induction, PDLSC exhibited higher calcium content and enhanced upregulation of osteogenic/periodontal genes compared to MSC(M) and MSC(AT), such as Runx2, Col1A1 and CEMP-1. However, the alkaline phosphatase activity of PDLSC did not increase. Our findings suggest that PDLSC might be a promising cell source for periodontal regeneration, presenting enhanced proliferative and osteogenic potential compared to MSC(M) and MSC(AT).
1. Introduction
Conditions affecting the periodontium are among the most prevalent worldwide and have been increasing in the last three decades [,]. The most relevant is periodontitis, an inflammatory non-communicable disease characterized by the progressive destruction of tooth-supporting tissues []. Triggered by a dysbiotic dental plaque accumulation, periodontitis affects the quality of life, with aesthetic implications, occasional pain, discomfort, and impaired mastication [,]. Beyond that, periodontitis also comes with socioeconomic impacts []. If untreated, periodontitis can lead to bone destruction, damaging both hard and soft periodontal tissues, resulting in tooth attachment and bone loss []. Additionally, its impact on systemic health is consistently proven [], thus making its treatment and resolution of its sequelae a priority.
Regenerative periodontal surgical treatments intend to re-establish lost periodontal tissues. In efforts to guide and increase the attachment of the teeth to the periodontium and induce bone gain, several surgical approaches have been proposed. Recent advances rely on guided tissue regeneration strategies using resorbable membranes, grafts and/or scaffolds []. Furthermore, scaffold-based therapies allow the delivery of cells and proteins directly to the defect site. However, despite these efforts, regeneration of a functional periodontium has never been achieved []. Recently, the potential use of cell therapies, in particular mesenchymal stromal cells (MSC), for periodontal tissue engineering applications has been explored [,]. Thus, understanding the source and the distinct differentiation patterns of these cells is crucial to elucidate their potential therapeutic use.
MSC have appeared as an appealing progenitor cell source for bone tissue engineering applications []. Originally isolated from bone marrow, MSC can also be derived from several adult tissues, including adipose tissue, umbilical cord, and Wharton’s jelly []. However, most of these sources require invasive procedures to isolate MSC with limited availability. As an alternative, dental MSC are an interesting source with less associated invasiveness []. Among dental MSC, periodontal ligament stromal cells (PDLSC) can potentially act as a source of renewable progenitor cells, capable of producing cementoblasts, osteoblasts and MSC []. Seo and colleagues successfully isolated PDLSC with stem/stromal cell characteristics from the human periodontal ligament (PDL) []. PDLSC have been previously compared to bone marrow-derived MSC (MSC(M)) as they are widely used in clinical studies []. Compared to MSC(M), PDLSC show a similar phenotypic profile and the capacity to develop into cementoblast-like cells, osteoblasts and adipocytes in vitro []. In vivo results also demonstrated that, upon transplantation, PDLSC formed cementum/PDL-like tissues in immunocompromised mice []. Moreover, PDLSC have demonstrated immunomodulatory and anti-inflammatory potential []. However, challenges remain to be addressed concerning the identification and characterization of PDLSC, in particular, aiming to find specific markers associated with PDL. Human PDLSC were first isolated from PDL heterogeneous cell populations using two early MSC-related cell surface markers: Stro-1 and CD146 []. Although Stro-1+ MSC were able to form clonogenic fibroblast colonies in vitro [], the use of Stro-1 alone for cell isolation is not sufficient to obtain pure populations of PDLSC. In fact, the reported percentage of Stro-1+ cells in the PDL tissue varies widely between 1.2% and 33.5% [,].
Since its isolation, studies on PDLSC reported the expression of several additional cell surface markers. However, more data regarding PDLSC characterization is required to confirm PDLSC identity and assess their use in clinical studies and stem cell therapy in dentistry. On the other hand, the osteogenic potential of PDLSC remains to be investigated: in particular, their performance compared to MSC derived from other adult tissues, such as adipose tissue and bone marrow. Therefore, the present study aims to explore the proliferative and osteogenic capacity of PDLSC for applications in periodontal regeneration. For this, we characterized and compared the osteogenic/periodontal potential of MSC derived from different adult sources, such as bone marrow, adipose tissue, and PDL. In this study, we compared the morphology, immunophenotype, proliferation rate, and trilineage differentiation potential of adipose tissue-derived MSC (MSC(AT)), MSC(M), and PDLSC. Moreover, the osteogenic potential and gene expression analysis of these cells were compared to evaluate their clinical application potential in repairing bone defects. We believe that this work may provide important data to support the selection of the most promising cells for periodontal tissue engineering applications.
2. Materials and Methods
2.1. Isolation and Culture of Human PDLSC
Healthy human third molars were extracted for orthodontic reasons from two healthy male patients (20 and 28 years old) by dentists from the Egas Moniz Dental Clinic, a university dental clinic located at Egas Moniz School of Health and Science (Almada, Portugal). Samples were washed with phosphate-buffered saline solution (PBS, Gibco, Thermo Fisher Scientific, Bohemia, NY, USA) supplemented with 1% antibiotic-antimycotic (A/A, Gibco, Thermo Fisher Scientific) (washing buffer). Then, the PDL was gently separated from the surface of the root and plated into a six-well plate containing a washing buffer. The solution containing the PDL tissue was transferred into a 15 mL tube and centrifuged at 1500 rpm for 10 min. After discarding the supernatant, cells were digested in a solution of 3 mg/mL collagenase type I (Sigma-Aldrich, St. Louis, MO, USA) and 4 mg/mL dispase (Sigma-Aldrich) for 1 h at 37 °C. To neutralize enzyme activity, an excess volume of washing buffer was added to the digested tissue and was then strained through a 70 μm cell strainer to remove undigested tissue from cells. Cells were centrifuged at 1500 rpm for 10 min and resuspended in 2 mL of low-glucose Dulbecco’s modified Eagle’s medium (DMEM, Gibco, Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (FBS MSC qualified, Gibco, Thermo Fisher Scientific) and 1% A/A. Upon reaching confluency, adherent PDLSC were harvested using a solution of 0.05% trypsin (Gibco, Thermo Fisher Scientific) and counted using the Trypan Blue exclusion method (Gibco, Thermo Fisher Scientific). Cells were then plated on T-75 flasks using low-glucose DMEM supplemented with 10% FBS and 1% A/A and kept at 37 °C, 5% CO2 in a humidified atmosphere. The medium renewal was performed every three to four days.
2.2. Culture of MSC(M) and MSC(AT)
MSC(M) and MSC(AT) were isolated and expanded from healthy donors (male, 32–46 years old) according to previously established protocols [,]. Human tissue samples were obtained from hospitals under a collaboration agreement with the Institute for Bioengineering and Biosciences at Instituto Superior Técnico (bone marrow: Instituto Português de Oncologia Francisco Gentil, Lisboa; adipose tissue: Clínica de Todos-os-Santos, Lisboa). Samples were obtained from healthy donors after written informed consent according to Directive 2004/23/EC of the European Parliament and of the Council of 31 March 2004 on setting standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells (Portuguese Law 22/2007, 29 June), with the approval of the Ethics Committee of the respective clinical institution. MSC(M) and MSC(AT) were plated using low-glucose DMEM supplemented with 10% FBS and 1% A/A. The medium was changed every three to four days. Two donors from each cell type (PDLSC, MSC(M) and MSC(AT)) were used in this work. The study design is shown in Scheme 1.
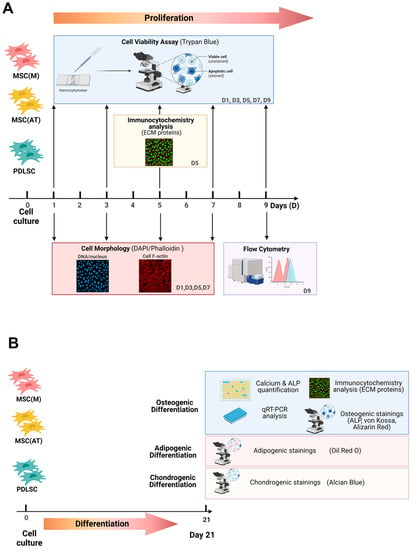
Scheme 1.
Schematic overview of the experimental procedure. Periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)) and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) were seeded in expansion conditions (day 0). (A) Cell viability assays were performed on days 1, 3, 5, 7, and 9. Cell morphology was evaluated on days 1, 3, 5, and 7. On day 5, an immunocytochemistry analysis of ECM proteins was performed. On day 9, immunophenotypical characterization was assessed. (B) Multilineage differentiation potential was evaluated after 21 days under specific differentiation conditions (osteogenic, adipogenic, and chondrogenic).
2.3. Multilineage Differentiation and Stainings
To investigate the multipotency of MSC derived from different sources, in vitro differentiation studies (osteogenic, adipogenic, and chondrogenic lineages) were performed. Cells that were not cultured under differentiation conditions (i.e., expansion medium, DMEM + 10% FBS) were used as negative controls.
2.3.1. Osteogenic Differentiation
PDLSC, MSC(M), and MSC(AT) were cultured at 3000 cells/cm2 on 24-well plates with DMEM + 10% FBS + 1% A/A. At 80% confluence, cells were incubated with osteogenic differentiation medium composed of low-glucose DMEM supplemented with 10% FBS and 1% A/A, 10 mM β-glycerophosphate (Sigma-Aldrich), 10 nM dexamethasone (Sigma-Aldrich), and 50 μg/mL ascorbic acid-2-phosphate (Sigma-Aldrich). After 21 days of osteogenic stimuli, cells were fixed in a 4% paraformaldehyde (PFA) (Sigma-Aldrich) solution and stained for alkaline phosphatase (ALP), von Kossa (VK), and Alizarin Red stainings as previously described [].
Alkaline Phosphatase (ALP) Activity Assay
After 21 days of osteogenic differentiation, ALP activity was evaluated using a colorimetric ALP kit (BioAssays Systems, Hayward, CA, USA) according to the manufacturer’s protocol. Firstly, samples were washed with PBS and incubated in lysis buffer (0.1% Triton X-100 in PBS) by shaking for 30 min at room temperature. Then, the lysate was added to a p-nitrophenyl phosphate solution (10 mM). Absorbance at 405 nm was measured with a plate reader and normalized to the metabolic activity. Three different samples were used for each condition, and absorbance was measured in triplicate. The metabolic activity of MSC was evaluated using AlamarBlue® cell viability reagent (Thermo Fisher Scientific) following the manufacturer’s guidelines. A 10% AlamarBlue® solution was added to cells and incubated for 3 h at 37 °C. Fluorescence intensity was measured in a plate reader (Infinite M200 Pro, Tecan, Männedorf, Switzerland) at an excitation/emission wavelength of 560/590 nm. Three samples were used for each condition, and fluorescence measurements were performed in triplicate.
Calcium Quantification Assay
After 21 days of osteogenic differentiation, samples were incubated with a 0.5 M HCl solution (Sigma-Aldrich) by shaking overnight at 4 °C. Total calcium content was determined using a calcium colorimetric assay kit (Sigma-Aldrich), according to manufacturer’s instructions. Calcium standard solutions were prepared in parallel. Absorbance at 575 nm was measured in triplicate for each condition and normalized to the metabolic activity. Three samples were used for each condition.
2.3.2. Adipogenic Differentiation
For adipogenic differentiation, PDLSC, MSC(M), and MSC(AT) were cultured at 3000 cells/cm2 in expansion conditions until 80% confluency. After 21 days under adipogenic differentiation medium (StemPro™ Adipogenesis Differentiation Kit, Gibco, Thermo Fisher Scientific), cells were fixed with 4% PFA and stained with Oil Red O solution, as previously described [].
2.3.3. Chondrogenic Differentiation
For chondrogenic differentiation, cells were cultured as cell aggregates on ultra-low attachment plates (Corning), as previously reported []. Cells were maintained in a chondrogenic differentiation medium (MesenCult™ Chondrogenic Differentiation Kit, Stemcell Technologies, Vancouver, BC, Canada) for 21 days, and chondrogenic differentiation was confirmed with Alcian Blue staining (Sigma-Aldrich) [].
2.4. Flow Cytometry Analysis
Immunophenotypic analysis of PDLSC, MSC(M) and MSC(AT) was performed by flow cytometry to assess the expression of CD14, CD19, CD29, CD34, CD44, CD45, CD73, CD80, CD90, CD105, CD106, CD146, CD166, HLA-DR, and STRO-1 (BioLegend, San Diego, CA, USA). Cells were incubated with each mouse anti-human monoclonal antibody, as previously reported []. A minimum of 10,000 events were collected, and flow cytometric analysis was performed using FACScalibur flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA) and CellQuestTM software (Becton Dickinson) was used for acquisition. Lastly, data analysis was conducted using Flowing Software (University of Turku, Turku, Finland).
2.5. Immunocytochemistry Analysis
The distribution of several ECM proteins, such as collagen I (Col I), asporin, fibronectin, laminin, osteopontin, osteocalcin, cementum protein 1, and Stro-1, was analyzed in MSC(M), MSC(AT), and PDLSC. After PFA fixation, cells were blocked and permeabilized for 45 min in 1% bovine serum albumin (BSA, Sigma-Aldrich), 10% FBS, and 0.3% Triton X-100 (Sigma-Aldrich). Primary antibodies (dilution 1:500 in 1% BSA, 10% FBS, and 0.3% Triton X-100), including rabbit anti-human collagen I (Thermo Fisher Scientific), asporin (Abcam, Cambridge, UK), laminin (Thermo Fisher Scientific), osteopontin (Abcam), osteocalcin (Sigma-Aldrich), cementum protein 1 (Abcam) and mouse anti-human collagen IV (Thermo Fisher Scientific), fibronectin (Thermo Fisher Scientific) and stro-1 (Thermo Fisher Scientific) were incubated overnight at 4 °C. After washing with 1% BSA, goat anti-mouse IgG Alexa Fluor 546, goat anti-rabbit IgG Alexa Fluor 546 and goat anti-mouse IgG Alexa Fluor 488 (Thermo Fisher Scientific, dilution 1:200 in 1% BSA solution) were used as secondary antibodies and incubated for 1 h at room temperature. Finally, cell nuclei were stained with DAPI (Thermo Fisher Scientific, 1.5 μg/mL) for 5 min.
2.6. Cell Morphology Assays
Cells were seeded on 24-well plates at 3000 cells/cm2, and cell morphology was assessed at different time points. Cytoskeleton actin filaments were stained with Phalloidin-TRITC (Sigma-Aldrich; dilution 1:250, 2 μg/mL) for 45 min in the dark. Afterward, nuclei were stained with DAPI (1.5 μg/mL) for 5 min.
2.7. Proliferation Assays
PDLSC, MSC(M), and MSC(AT) were cultured for 9 days on 12-well plates at different cell densities: 1500 cells/cm2 and 3000 cells/cm2 in expansion conditions (DMEM + 10% FBS). At each time point, cells were harvested using a 0.05% trypsin solution (Gibco, Thermo Fisher Scientific) and counted using the Trypan Blue exclusion method to determine cell numbers.
2.8. Quantitative Reverse Transcription-Polymerase Chain Reaction (qRT-PCR) Analysis
After 21 days of osteogenic differentiation, PDLSC, MSC(M) and MSC(AT) total RNA was extracted using RNeasy Mini Kit (QIAGEN, Hilden, Germany), followed by cDNA synthesis with High-Capacity cDNA Reverse Transcription kit (Life Technologies, Carlsbad, CA, USA). Primer sequences used are summarized in Table 1, and qRT-PCR was performed using NZYSpeedy qPCR Green Master Mix (2×), ROX plus (NZYTech, Lisbon, Portugal) and StepOnePlus real-time PCR system (Applied Biosystems, Waltham, MA, USA). Reactions were performed in triplicate and carried out for 10 min at 95 °C, followed by 40 cycles of 15 sec at 95 °C and 1 min at 60 °C. Gene expression was normalized to the housekeeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH), and fold-change was calculated considering baseline expression at day 0 (undifferentiated cells). A threshold cycle (Ct) was observed in the exponential phase. ΔΔCt values were calculated using geometric means and expressed as 2−ΔΔCt.

Table 1.
Primers used for qRT-PCR.
2.9. Statistical Analysis
For each experiment, two different donors of each cell source (MSC(M), MSC(AT) and PDLSC) were used, and three independent experiments (cells from different passages, P3–P5) for each donor were performed with three technical replicates of each. The statistical analysis of the data was performed using one-way ANOVA, followed by the Tukey post-hoc test. GraphPad Prism version 7 software was used in the analysis, and data was considered to be significant when the p-values obtained were less than 0.05 (95% confidence intervals, * p < 0.05).
3. Results
3.1. Characterization of MSC Derived from Different Adult Tissue Sources: Periodontal Ligament, Bone Marrow and Adipose Tissue
In order to identify the immunophenotypic differences between MSC isolated from different sources, comparative studies with MSC(M), MSC(AT) and PDLSC were performed by flow cytometry for cells cultured for passages 3, 5, and 7 (Figure 1, Supplementary Figures S1–S3).
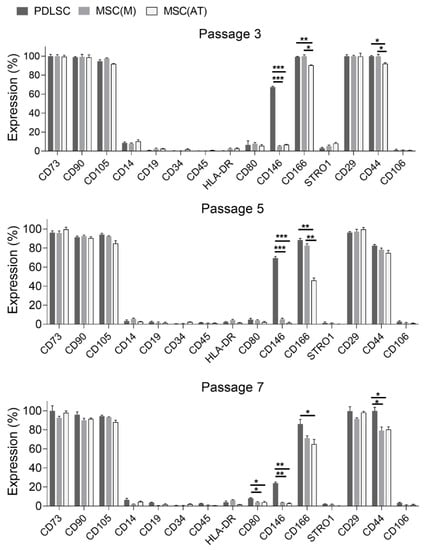
Figure 1.
Immunophenotypic analysis of periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)) and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) cultured in expansion conditions (DMEM + 10% FBS) at passages 3, 5, and 7 by flow cytometry (day 9). Data are expressed as mean ± SD (2 donors per tissue source, 3 independent experiments, 3 technical replicates); * p < 0.05, ** p < 0.01, *** p < 0.001.
All cells displayed strongly positive expression (>90%) of MSC-associated cell surface markers CD29, CD44, CD73, CD90 and CD105 in passage 3. Results showed that CD166 expression was positive for PDLSC (>86.1%) and MSC(M) (>71.3%) in passages 3, 5, and 7 (Figure 1). Additionally, when compared with MSC(AT), PDLSC presented a statistically significant enhancement of CD166 expression in all passages studied. When comparing CD166 expression between MSC(M) and MSC(AT), results showed that MSC(M) presented higher CD166 expression regardless of passage, with statistically significant differences in passages 3 and 5. Thus, CD166 expression of MSC(AT) was lower for all passages in comparison with both PDL- and bone marrow-derived counterparts. Moreover, the CD166 expression levels of MSC(AT) decreased with increasing passages, presenting an expression of (90.45 ± 0.33)% in passage 3, (45.94 ± 2.65)% in passage 5, and (64.87 ± 5.12)% in passage 7. CD106 and Stro-1 expression levels were low (<10%) in all samples analyzed in passages 3, 5, and 7, regardless of the tissue source (Figure 1). As expected, lack of expression of hematopoietic cell-associated markers (CD14, CD19, CD34, CD45, and HLA-DR) was also verified for PDLSC, MSC(M) and MSC(AT) in passages 3, 5, and 7. Additionally, the immune cell-related marker CD80 presented low expression levels by samples from all MSC sources. Lastly, results showed that CD146, a marker previously used to identify PDLSC, was only expressed by PDLSC in passages 3, 5, and 7. Despite this, results showed that CD146 expression by PDLSC decreased with passaging, expressing (67.40 ± 0.91)% in passage 3, (69.51 ± 1.63)% in passage 5, and (24.06 ± 1.23)% in passage 7 (Figure 1).
Despite presenting some differences, cells from the different tissues exhibited similar spindle-shaped morphology (Figure 2). After seven days of culture, PDLSC cultures were completely confluent, contrary to bone marrow and adipose tissue-derived cultures, as observed by DAPI/Phalloidin staining (Figure 2).
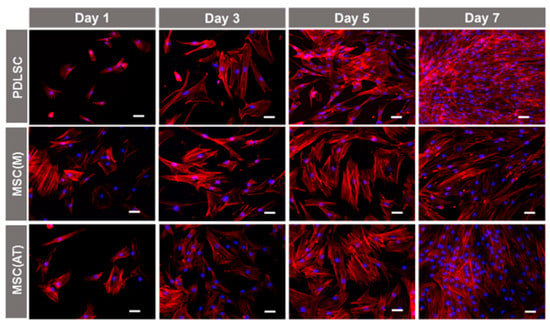
Figure 2.
Morphology of periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)) and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) at days 1, 3, 5, and 7 of culture under expansion conditions (DMEM + 10% FBS) at 3000 cells/cm2 (passage 3). Nuclei were stained with DAPI (blue), and cytoskeleton actin filaments were stained with phalloidin (red). Scale bars, 50 µm.
To further explore differences in protein expression between PDLSC, MSC(M) and MSC(AT), a comparative immunocytochemistry analysis was performed (Figure 3). Results confirmed the expression of the common extracellular matrix (ECM) proteins, such as laminin and fibronectin, in all samples. Additionally, expression of the known MSC marker Stro-1, asporin, osteocalcin (OC) and osteopontin (OPN) was only detected on undifferentiated PDLSC and not detected in undifferentiated MSC(M) and MSC(AT) (Figure 3). The positive stainings of osteogenic markers OPN and OC suggested that PDLSC might have higher osteogenic potential, even when not cultured under osteogenic differentiation conditions (i.e., expansion medium).
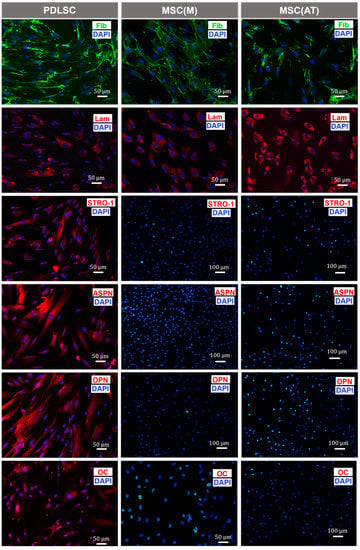
Figure 3.
Comparison of immunofluorescence staining images for periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)) and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) cultured in expansion conditions (DMEM + 10% FBS) at passage 3, after five days. Fib: fibronectin (green); Lam: laminin (red); STRO-1; Stro-1 (red):), ASPN: asporin (red), OPN: osteopontin (red), OC: osteocalcin (red). Nuclei were stained with DAPI (blue). Representative images from one donor are shown.
3.2. Proliferative Potential of MSC Derived from Periodontal Ligament, Bone Marrow and Adipose Tissue
To assess the proliferative capacity of MSC from different sources (PDLSC, MSC(M) and MSC(AT)), cells (P3–P5) were plated at different cell seeding densities: 1500 cells/cm2 and 3000 cells/cm2 (Figure 4).
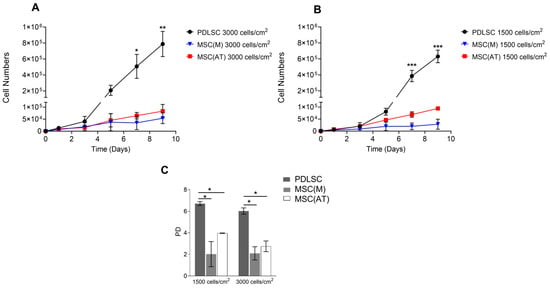
Figure 4.
Proliferation of periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)) and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) cultured for nine days in expansion conditions (DMEM + 10% FBS) seeded at (A) 3000 cells/cm2 and (B) 1500 cells/cm2 (P3–P5). (C) Population doublings (PD) of PDLSC, MSC(M) and MSC(AT) after nine days of culture when seeded at different cell densities: 1500 cells/cm2 and 3000 cells/cm2. Values are expressed as mean ± SD (two donors per tissue source, three independent experiments, three technical replicates); * p < 0.5, ** p < 0.01, *** p < 0.001.
Under the conditions of our study, PDLSC presented a significantly higher proliferative rate in comparison with MSC(M) and MSC(AT). After nine days of culture at 3000 cells/cm2, a significant increase in cell numbers was observed for PDLSC compared to MSC(M) and MSC(AT) (Figure 4A). PDLSC reached a cell number of (7.90 ± 1.60) × 105, whereas MSC(M) and MSC(AT) only reached a cell number of (0.54 ± 0.22) × 105 and (0.83 ± 0.28) × 105, respectively. When cells were seeded at 1500 cells/cm2, PDLSC reached a cell number of (6.30 ± 0.79) × 105, while MSC(M) and MSC(AT) presented cell numbers of (0.29 ± 0.21) × 105 and (0.94 ± 0.01) × 105, respectively (Figure 4B). Additionally, MSC(AT) presented higher cell numbers compared to MSC(M) (Figure 4).
During the nine-day culture period, all cells exhibited similar cell growth behavior regardless of cell seeding density. Moreover, after nine days in culture, PDLSC reached statistically significant higher population doublings compared to MSC(M) and MSC(AT) (6.0 ± 0.3 vs. 2.1 ± 0.6 vs. 2.8 ± 0.5 for PDLSC, MSC(M), and MSC(AT), respectively, when cultured at 3000 cells/cm2) (Figure 4C). PDLSC exhibited higher cell growth rates regardless of seeding density (Supplementary Table S1).
3.3. Osteogenic Potential of MSC Derived Periodontal Ligament, Bone Marrow and Adipose Tissue
After 21 days under differentiation conditions towards adipogenic, chondrogenic, and osteogenic lineages, stainings confirmed the successful in vitro trilineage differentiation of PDLSC, MSC(M), and MSC(AT) (Figure 5) at passages 3 and 5. Figure 5 revealed positive stainings of adipocytes, osteoblasts, and chondrocytes with Oil red O, Alkaline Phosphatase (ALP)/von Kossa (VK) and Alcian blue stainings, respectively. Cells cultured under expansion conditions (DMEM) were used as negative controls. Although stainings were not quantified, qualitative studies on multilineage differentiation were able to suggest some differences between the three cell sources. Regarding adipogenic differentiation, PDLSC exhibited a lower amount of Oil Red O-stained liquid droplets compared with MSC(M) and MSC(AT), suggesting a decreased adipogenic potential. Interestingly, osteogenic differentiation stainings revealed that PDLSC produced a lower amount of ALP compared with MSC(M) and MSC(AT) (Figure 5). MSC(M) and MSC(AT) multilineage differentiation assays presented similar ALP/VK, Alizarin Red, and Oil Red-O stainings (Figure 5).
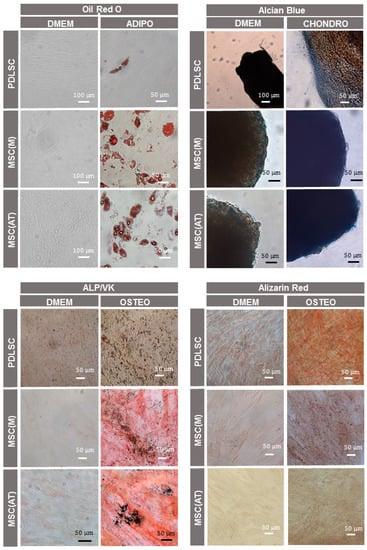
Figure 5.
In vitro multilineage differentiation of periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)), and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) at passage 3, after 21 days. Adipogenic differentiation was detected with Oil red O staining showing the lipid vacuoles in red. Alcian blue stained sulfated glycosaminoglycans in blue. Alkaline phosphatase (ALP) and von Kossa (VK) stainings showed ALP activity in red and mineralized extracellular matrix deposits in black. Alizarin red stained calcium deposits in the extracellular matrix in red. As controls, all stainings were also performed using an expansion medium (DMEM + 10% FBS). Representative images from one donor are shown.
To evaluate the impact of tissue source on the in vitro osteogenic potential of MSC, calcium deposition, ALP activity and osteogenic/periodontal gene expression were evaluated after 21 days of culture under osteogenic differentiation conditions (P3–P5). As expected, results showed that cells from all sources cultured under osteogenic induction conditions (OSTEO) presented higher calcium accumulation compared to cells cultured under expansion conditions (DMEM) (Figure 6A). These differences confirmed the successful osteogenic differentiation of MSC from different sources. A statistically significant enhancement in calcium accumulation was observed for MSC derived from PDL compared to MSC(M) and MSC(AT) ([17.17 ± 2.02] × 10−7 μg·μL−1) (Figure 6A). However, MSC(M)and MSC(AT) did not present statistically significant differences in calcium accumulation after 21 days of osteogenic differentiation (MSC(M): [9.20 ± 1.21] × 10−7 μg·μL−1, MSC(AT): [11.74 ± 0.35] × 10−7 μg·μL−1). These results demonstrated a higher mineralization capacity from PDLSC compared to bone marrow and adipose tissue-derived cells under the conditions of our study.
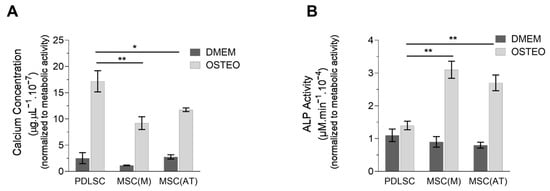
Figure 6.
Quantitative assessment of calcium content and alkaline phosphatase (ALP) activity of periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)), and adipose tissue-derived mesenchymal stromal cells (MSC(AT)), cultured for 21 days under expansion (DMEM + 10% FBS) and osteogenic differentiation (OSTEO) conditions (P3–P5). (A) Calcium concentration. (B) ALP activity. Data are expressed as mean ± SD (two donors per tissue source, three independent experiments, and three technical replicates); * p < 0.05, ** p < 0.01.
Furthermore, results demonstrated that ALP activity of PDLSC did not increase after osteogenic differentiation ([1.40 ± 0.13] × 10−4 μg·μL−1) (Figure 6B). On the other hand, MSC(M) and MSC(AT) presented a statistically significant increase in ALP activity compared to PDLSC after 21 days of culture under osteogenic conditions (MSC(M): [3.10 ± 0.26] × 10−4 μg·μL−1, MSC(AT): [2.70 ± 0.24] × 10−4 μg·μL−1) (Figure 6B). Despite this, the ALP activity of MSC(M) and MSC(AT) was not statistically significantly different, suggesting a similar osteogenic potential between these cells.
Gene expression levels of osteogenic/periodontal markers were evaluated by quantitative reverse transcription-polymerase chain reaction (qRT-PCR), namely runt-related transcription factor 2 (Runx2), collagen type I (Col1A1), ALP, OPN, OC, cementum protein-1 (CEMP-1) and periostin (POSTN) (Figure 7). After 21 days under osteogenic differentiation conditions, cells isolated from the different tissues upregulated the expression of osteogenic gene markers compared to the control (undifferentiated cells at day 0), confirming the successful osteogenic differentiation of MSC. Statistically significant differences in the expression levels of Col1A1 (p < 0.001), Runx2 (p < 0.01), OC (p < 0.001), CEMP-1 (p < 0.05) and POSTN (p < 0.001) were observed between PDLSC and the bone-marrow and adipose tissue-derived cells (Figure 7). OPN (p < 0.001) and ALP (p < 0.001) gene expression of PDLSC was statistically enhanced compared to MSC(AT), however similar to MSC(M). Moreover, under the conditions tested, MSC(AT) presented the lowest osteogenic/periodontal potential, as suggested by the lower levels of OPN, OC and POSTN gene expression (Figure 7). Lastly, regarding Col1A1, Runx2 and CEMP-1 expression levels, MSC(AT) and MSC(M) did not present significant differences.
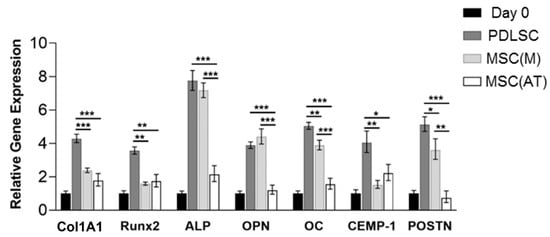
Figure 7.
Osteogenic/periodontal gene expression by periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)) and adipose tissue-derived mesenchymal stromal cells (MSC(AT)), after 21 days under osteogenic differentiation conditions (P3–P5). Results were normalized to the endogenous control GAPDH and presented as fold change expression relative to undifferentiated MSC from the different sources (day 0). Values are expressed as mean ± SD (two donors per tissue source, three independent experiments, and three technical replicates); * p < 0.05, ** p < 0.01, *** p < 0.001.
After 21 days of culture under osteogenic conditions, immunocytochemistry analysis of PDLSC, MSC(M), and MSC(AT) was performed (Figure 8). Results confirmed the expression of the common ECM proteins, laminin, and fibronectin, in all samples. Additionally, MSC derived from all sources stained positive for osteogenic and periodontal-related markers, namely OC, OPN and asporin. Interestingly, CEMP-1 was exclusively expressed by PDLSC (Figure 8).
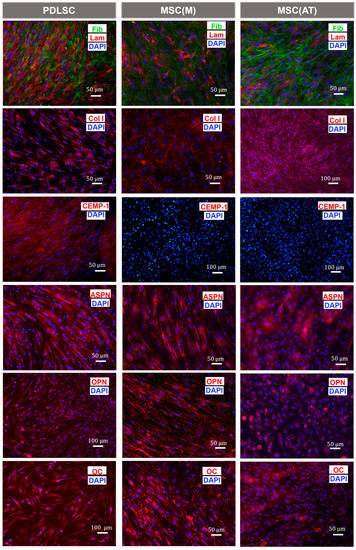
Figure 8.
Comparison of immunofluorescence staining images for periodontal ligament stromal cells (PDLSC), bone marrow (MSC(M)), and adipose tissue-derived mesenchymal stromal cells (MSC(AT)) after 21 days of culture under osteogenic conditions (passage 3). Fib: fibronectin (green); Lam: laminin (red); Col I: collagen I (red), CEMP-1: cementum protein-1 (red); ASPN: asporin (red), OPN: osteopontin (red); OC: osteocalcin (red). Nuclei were stained with DAPI (blue). Representative images from one donor are shown.
Overall, the results presented in this work demonstrated that MSC isolated from PDL, bone marrow and adipose tissue were able to differentiate into the osteogenic lineage. However, under the conditions tested, significant differences between PDLSC, MSC(M), and MSC(AT) were observed concerning the levels of mineralization and osteogenic/periodontal gene expression, suggesting that PDLSC present a higher osteogenic potential.
4. Discussion
The results presented in our study suggest that PDL can be a promising cell source for periodontal tissue engineering applications. MSC derived from PDL (PDLSC) exhibited enhanced proliferative capacity and superior osteogenic/periodontal potential when compared to other adult MSC sources commonly used in regenerative medicine applications, namely MSC(M) and MSC(AT).
Successful periodontal regeneration requires coordinated regeneration of soft (PDL) and hard (cementum and alveolar bone) tissues. Limitations in current regeneration strategies remain due to outcome variability. Cell-based therapies have been investigated to improve clinical outcomes of periodontal regeneration []. In fact, several studies have supported the potential application of ex vivo expanded MSC for periodontal tissue regeneration []. For instance, MSC(M) injected into periodontal defects have demonstrated anti-inflammatory and immunomodulatory effects leading to tissue regeneration []. Although MSC(M) are considered the gold standard of cells for bone tissue engineering applications [], dental-derived MSC, such as PDLSC, represent an attractive alternative cell source for periodontal regeneration due to their relative ease and less invasive access in comparison to MSC(M). Despite this, only few clinical trials are using PDLSC to treat periodontal intrabody defects []. Moreover, there is a lack of evidence to support the use of PDLSC for periodontal tissue engineering purposes compared to MSC derived from other adult tissues, such as MSC(M) and MSC(AT). Therefore, in this work, we evaluated the potential of PDLSC application in periodontal regeneration by comparing the osteogenic/periodontal potential of MSC derived from other adult tissues, including bone marrow, adipose tissue and PDL. Previous works have already demonstrated that PDLSC had a greater osteogenic potential than other dental derived-MSC, such as dental pulp stem/progenitor cells and stem/progenitor cells from human exfoliated deciduous teeth []. However, this is the first study performing a comprehensive characterization on the osteogenic potential of PDLSC and MSC isolated from the most common adult tissues exploited in clinical studies (MSC(M) and MSC(AT)).
To assess differences among MSC derived from different adult tissues, cell surface marker expression profiles were analyzed for cells at passages 3, 5, and 7 and compared by flow cytometry. As expected, and in line with previous reports, PDLSC [,], MSC(M) [,], and MSC(AT) [,] presented a positive expression of MSC-related markers CD29, CD44, CD73, CD90, and CD105. CD44 is a cell surface marker associated with MSC []. In fact, MSC(M) and MSC(AT) have been reported to present similar levels of expression of CD44 in early passages (passage 3 or lower) [,]. Moreover, reports have shown that MSC(M) can maintain a strong positive expression of CD44 despite cell passages []. However, under the conditions tested, our results demonstrated that CD44 expression of MSC(M) and MSC(AT) was negatively affected by passaging, whereas PDLSC were consistently positive for CD44 in early and late passages. Additionally, our results showed that Stro-1, a known MSC marker [], was presenting low expressing levels by MSC derived from PDL, bone marrow and adipose tissue (<11.3%). In fact, it is unclear whether Stro-1 expression correlates with multipotency, and it has been reported that Stro-1 is not universally expressed by MSC derived from different sources [,]. Concerning CD146 expression, a cell surface marker previously applied in the identification of PDLSC [] and commonly used as a marker for endothelial cells [], both MSC(M) and MSC(AT) expressed low levels of CD146 in all passages studied (<7%). Interestingly, PDLSC robustly expressed CD146 presenting expression values of (67.40 ± 0.91)% in passage 3 and (69.51 ± 1.63)% in passage 5. However, the expression of CD146 by PDLSC decreased with passaging, reaching expression values of (24.06 ± 1.23)% in passage 7. Indeed, previous reports have demonstrated a reduced expression of CD146 in MSC derived from dental pulp and exfoliated deciduous teeth when cultured under continuous passage conditions []. Moreover, CD146+ PDLSC have been reported to exhibit higher colony-forming efficiency and proliferation rate when compared to CD146− PDLSC []. Thus, we hypothesize that CD146 might contribute to enhanced cell proliferation of PDLSC. These results are in line with previous reports, which suggested that CD146 expression might be used as a marker for PDLSC []
Immunocytochemistry analysis of PDLSC, MSC(M) and MSC(AT) confirmed the presence of commonly expressed ECM molecules, including laminin and fibronectin. Overall, comparative analysis of PDLSC, MSC(M) and MSC(AT) revealed phenotypic similarities regarding the expression of MSC-related markers. Despite this, differences in PDLSC expression were observed, such as positive immunofluorescence stainings of asporin (a protein associated with the PDL []), OPN and OC (bone ECM proteins []) which were not expressed by bone marrow- and adipose tissue-derived cells. In fact, the positive stainings of osteogenic markers OPN and OC suggested that PDLSC might have a higher osteogenic potential, even when not cultured under osteogenic differentiation conditions (i.e., expansion medium). Still, additional comparative studies are necessary to assess if phenotypic differences between PDLSC and MSC derived from other sources have an impact on what concerns cell function and therapeutic potential.
Concerning the growth curves of PDLSC, MSC(M) and MSC(AT), substantial differences in terms of proliferative potential were noticed. Despite MSC(M) and MSC(AT) exhibiting similar growth patterns, cells from adipose tissue reached higher cell numbers, which is in line with previous research [,]. PDLSC exhibited significantly higher proliferation capacity reaching higher cell numbers compared to bone marrow- and adipose tissue-derived cells. Additionally, PDLSC also presented higher cell population doublings, regardless of the initial cell seeding density. In line with these findings, morphology assays revealed higher confluency in PDLSC culture after seven days in expansion conditions. Interestingly, immunocytochemistry analysis revealed that only PDLSC expressed OPN. In fact, previous studies demonstrated that OPN has chemoattractant properties that induce migration of MSC [,], neural stem cells [], endothelial cells [], and hematopoietic stem cells []. Furthermore, OPN promotes cell adhesion by interacting with several cell surface integrins. In this context, we hypothesize that positive OPN expression of PDLSC might be associated with the higher proliferation rate presented by PDLSC compared to MSC(M) and MSC(AT). In fact, this high proliferative capacity presented by PDLSC can be considered a technical advantage since MSC-based therapies depend on ex vivo expansion prior to in vivo administration in order to reach clinically meaningful cell numbers.
As expected, multipotency of PDLSC, MSC(M) and MSC(AT) was confirmed with positive stainings for multilineage differentiation across mesodermal lineages (osteogenic, adipogenic, and chondrogenic). The qualitative nature of in vitro stainings did not allow an accurate assessment of disparities in what concerns differentiation potential. Thus, further studies should consider staining’s quantification. However, it is relevant to note that PDLSC produced lower amounts of red-stained lipid vacuoles after adipogenic differentiation compared with MSC(M) and MSC(AT), suggesting a decreased adipogenic potential for cells obtained from PDL. Nevertheless, the Oil red O staining results did not allow a clear comparison between the three different cell types. Further quantitative assays are necessary to fully assess the adipogenic differentiation capacity of PDLSC, such as adipogenic gene expression analysis.
In what concerns osteogenic potential, PDLSC displayed increased osteogenic capacity in vitro compared to the other sources. We observed that, although MSC(M) and MSC(AT) presented similar values of calcium deposits after 21 days under osteogenic differentiation conditions, PDLSC significantly outperformed their amount of calcium. In fact, reports have shown that PDLSC have a phenotype characteristic of osteoblast-like cells [,], upregulating osteogenic marker genes and generating new bone following tooth extraction []. Surprisingly, ALP staining and its quantification demonstrated that the ALP activity of PDLSC did not increase significantly after culturing under osteogenic induction conditions. Yu and colleagues have shown that PDLSC are composed of a heterogeneous population of cells, presenting ALP+ and ALP− cells []. They found that both ALP+ and ALP− cells showed similar osteogenic potential with no observable difference in the amount of mineral deposits after osteogenic differentiation []. Therefore, the lack of ALP activity observed in this work might be due to the presence of a population of ALP− cells. It is important to highlight that the lower levels of ALP activity of PDLSC did not compromise the osteogenic differentiation of these cells, as observed by the enhancement of mineralization and upregulation of osteogenic marker genes. Interestingly, the low levels of ALP activity in PDLSC might be related to the decreased adipogenic potential presented by PDLSC. In fact, ALP, besides being traditionally used as a marker of early osteogenesis, is involved in the control of intracellular lipid accumulation in adipocyte maturation. Thus, the absence of ALP may prevent formation of lipids in cells [,]. However, isolation of PDLSC from additional donors is required to understand the low levels of ALP activity observed by PDLSC.
Additionally, qRT-PCR results confirmed effective osteogenic differentiation of MSC after 21 days of culture under osteogenic differentiation conditions, independently of the tissue of origin. After osteogenic induction, MSC(AT) presented lower relative expression of osteogenic genes and downregulated POSTN gene expression compared to MSC(M) and PDLSC. Overall, these results suggested that, under the conditions of our study, adipose tissue-derived MSC possessed lower osteogenic capacity compared with PDLSC and MSC(M). In fact, previous comparative studies reported that MSC(AT) presented limited osteogenic potential compared to MSC(M), showing lower ALP activity, calcium content and expression of early and late osteogenic genes [,]. Although PDLSC upregulated the ALP gene after 21 days of osteogenic differentiation, enhancement of ALP activity was not observed. Despite the mRNA levels and protein activity of ALP tending to be correlated, there is not a linear correlation due to mRNA and protein regulation. The Runx2 gene regulates downstream genes that determine the osteogenic phenotype and controls the expression of osteogenic marker genes such as Col1A1, ALP, OPN, and OC [,]. OC and OPN are non-collagenous proteins that play key roles in the biological and mechanical functions of bone [,]. Our results revealed that PDLSC presented higher upregulation of the Runx2 gene than bone marrow and adipose tissue-derived cells. Furthermore, both MSC(M) and PDLSC exhibited higher upregulation of late osteogenic marker genes, OC and OPN. Collagen I is the most abundant protein in bone ECM (90% of the organic bone ECM) and is pivotal for matrix mineralization [,]. In fact, previous studies showed that, during osteogenic differentiation, PDLSC displays better collagen-forming capacity than MSC(M) []. After 21 days under osteogenic differentiation conditions, analysis of gene expression levels revealed higher upregulation of Col1A1 and CEMP-1 genes by PDLSC compared with MSC(M) and MSC(AT). Indeed, CEMP-1 has been identified as a novel cementum-specific protein and is strongly expressed by cementoblasts and their progenitors [], including cells located near the blood vessels in the PDL []. Combined with the expression of CEMP-1 observed by immunocytochemistry analysis, enhanced upregulation of CEMP-1 gene expression suggested that PDLSC may comprise a subpopulation of cementum progenitor cells, as previously proposed by McCulloch and Melcher [] and further supported by recent studies []. Periostin is a matricellular protein with a fundamental role in bone and tooth tissue development and repair, namely remodeling of the collagen matrix [] and maintenance of the integrity of the PDL in response to mechanical stresses []. Interestingly, after 21 days under osteogenic differentiation conditions, PDLSC presented higher POSTN gene expression levels compared with MSC(M) and MSC(AT), as assessed by qRT-PCR analysis. Immunofluorescence results corroborated the successful osteogenic differentiation of the three cell types, regardless of their tissue of origin. As expected, common ECM proteins, including laminin and fibronectin, were positively stained in all samples. Additionally, positive stainings for collagen I, OPN and OC were observed in MSC from all tissue sources. Concerning CEMP-1, only differentiated PDLSC displayed positive staining.
Overall, our comparative study demonstrates that PDLSC show an enhanced osteogenic/periodontal potential compared to bone marrow and adipose tissue-derived cells, showing promising results for periodontal tissue engineering applications [,,]. Future studies should include more donors from each cell source to determine the impact of donor variability on cells’ osteogenic/periodontal potential. As a limitation of this study, cells isolated from the different tissues were not collected from the same donors as different procedures required to harvest PDLSC, MSC(M) and MSC(AT) are extremely invasive and are often carried out in different medical facilities. Moreover, future studies should include transcriptome analysis of PDLSC compared to MSC from other sources.
5. Conclusions
In summary, we have successfully isolated and characterized PDLSC, and we have shown that these cells exhibited enhanced proliferative and osteogenic/periodontal potential compared to MSC from other sources (bone marrow and adipose tissue). Our results showed that only PDLSC expressed OPN, a non-collagenous bone ECM protein important for cell proliferation and migration. Moreover, gene expression analysis revealed that PDLSC presented a significant enhancement in osteogenic/periodontal marker gene expression levels, such as Runx2, OC, CEMP-1, and POSTN, compared to MSC(M) and MSC(AT). Therefore, this work suggests that PDLSC are promising candidates for periodontal regeneration therapies, providing enhanced proliferative and osteogenic capacity. Future in vivo studies will be needed to assess if PDLSC retain their osteogenic and periodontal potential after administration and to determine the number of PDLSC required to obtain a clinical benefit.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines11051352/s1, Figure S1: Flow cytometry analysis of MSC(AT), MSC(M) and PDLSC at passage 3; Figure S2: Flow cytometry analysis of MSC(AT), MSC(M) and PDLSC at passage 5; Figure S3: Flow cytometry analysis of MSC(AT), MSC(M) and PDLSC at passage 7; Table S1: Exponential regression parameters and respective coefficient of determination (R2) estimated using MS Excel for PDLSC, MSC(M) and MSC(AT).
Author Contributions
Conceptualization, L.A., J.M.S.C., C.L.d.S. and M.S.C.; investigation, L.A., V.M., J.B. and M.S.C.; writing—original draft preparation, L.A. and M.S.C.; writing—review and editing, L.A., V.M., J.B., J.J.M., J.M.S.C., C.L.d.S. and M.S.C.; supervision, C.L.d.S. and M.S.C.; funding acquisition, J.M.S.C., C.L.d.S. and M.S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was financed by national funds from FCT-Fundação para a Ciência e a Tecnologia, I.P., in the scope of the project UIDB/04565/2020 and UIDP/04565/2020 of the Research Unit Institute for Bioengineering and Biosciences—iBB and the project LA/P/0140/2020 of the Associate Laboratory Institute for Health and Bioeconomy—i4HB. Funding was also provided from the FCT project PTDC/BTM-BTM/3538/2020—DentalBioMatrix.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the ethics committee of Instituto Superior Técnico and Instituto Português de Oncologia de Lisboa Francisco Gentil (120308).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The authors declare that the data generated in the current study are available within the article or from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Chen, M.X.; Zhong, Y.J.; Dong, Q.Q.; Wong, H.M.; Wen, Y.F. Global, Regional, and National Burden of Severe Periodontitis, 1990–2019: An Analysis of the Global Burden of Disease Study 2019. J. Clin. Periodontol. 2021, 48, 1165–1188. [Google Scholar] [CrossRef]
- Machado, V.; Botelho, J.; Escalda, C.; Hussain, S.B.; Luthra, S.; Mascarenhas, P.; Orlandi, M.; Mendes, J.J.; D’Aiuto, F. Serum C-Reactive Protein and Periodontitis: A Systematic Review and Meta-Analysis. Front. Immunol. 2021, 12, 706432. [Google Scholar] [CrossRef]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal Diseases. Nat. Rev. Dis. Prim. 2017, 3, 17038. [Google Scholar] [CrossRef]
- Ferreira, M.C.; Dias-Pereira, A.C.; Branco-de-Almeida, L.S.; Martins, C.C.; Paiva, S.M. Impact of Periodontal Disease on Quality of Life: A Systematic Review. J. Periodontal Res. 2017, 52, 651–665. [Google Scholar] [CrossRef]
- Botelho, J.; Machado, V.; Leira, Y.; Proença, L.; Chambrone, L.; Mendes, J.J. Economic Burden of Periodontitis in the United States and Europe—An Updated Estimation. J. Periodontol. 2021, 93, 373–379. [Google Scholar] [CrossRef]
- Preshaw, P.M.; Seymour, R.A.; Heasman, P.A. Current Concepts in Periodontal Pathogenesis. Dent. Update 2004, 31, 570–578. [Google Scholar] [CrossRef]
- Botelho, J.; Mascarenhas, P.; Viana, J.; Proença, L.; Orlandi, M.; Leira, Y.; Chambrone, L.; Mendes, J.J.; Machado, V. An Umbrella Review of the Evidence Linking Oral Health and Systemic Health: From the Prevalence to Clinical and Circulating Markers. medRxiv 2022. [Google Scholar] [CrossRef]
- Larsson, L.; Decker, A.M.; Nibali, L.; Pilipchuk, S.P.; Berglundh, T.; Giannobile, W.V. Regenerative Medicine for Periodontal and Peri-Implant Diseases. J. Dent. Res. 2016, 95, 255–266. [Google Scholar] [CrossRef]
- Du, J.; Shan, Z.; Ma, P.; Wang, S.; Fan, Z. Allogeneic Bone Marrow Mesenchymal Stem Cell Transplantation for Periodontal Regeneration. J. Dent. Res. 2014, 93, 183–188. [Google Scholar] [CrossRef]
- Citterio, F.; Gualini, G.; Fierravanti, L.; Aimetti, M. Stem Cells and Periodontal Regeneration: Present and Future. Plast. Aesthetic Res. 2020, 7, 41. [Google Scholar] [CrossRef]
- Carvalho, M.S.; Alves, L.; Bogalho, I.; Cabral, J.M.S.; da Silva, C.L. Impact of Donor Age on the Osteogenic Supportive Capacity of Mesenchymal Stromal Cell-Derived Extracellular Matrix. Front. Cell Dev. Biol. 2021, 9, 747521. [Google Scholar] [CrossRef]
- Viswanathan, S.; Ciccocioppo, R.; Galipeau, J.; Krampera, M.; Le Blanc, K.; Martin, I.; Moniz, K.; Nolta, J.; Phinney, D.G.; Shi, Y.; et al. Consensus International Council for Commonality in Blood Banking Automation–International Society for Cell & Gene Therapy Statement on Standard Nomenclature Abbreviations for the Tissue of Origin of Mesenchymal Stromal Cells. Cytotherapy 2021, 23, 1060–1063. [Google Scholar] [CrossRef]
- Seo, B.; Miura, M.; Gronthos, S.; Bartold, P.M.; Batouli, S.; Brahim, J.; Young, M.; Robey, P.G.; Wang, C.; Shi, S. Investigation of Multipotent Postnatal Stem Cells from Human Periodontal Ligament. Lancet 2004, 364, 149–155. [Google Scholar] [CrossRef]
- Bartold, P.M.; Shi, S.; Gronthos, S. Stem Cells and Periodontal Regeneration. Periodontol. 2000 2006, 40, 164–172. [Google Scholar] [CrossRef]
- Qu, G.; Li, Y.; Chen, L.; Chen, Q.; Zou, D.; Yang, C.; Zhou, Q. Comparison of Osteogenic Differentiation Potential of Human Dental-Derived Stem Cells Isolated from Dental Pulp, Periodontal Ligament, Dental Follicle, and Alveolar Bone. Stem Cells Int. 2021, 2021, 6631905. [Google Scholar] [CrossRef]
- Simmons, P.J.; Torok-Storb, B. Identification of Stromal Cell Precursors in Human Bone Marrow by a Novel Monoclonal Antibody, STRO-1. Blood 1991, 78, 55–62. [Google Scholar] [CrossRef]
- Nagatomo, K.; Komaki, M.; Sekiya, I.; Sakaguchi, Y.; Noguchi, K.; Oda, S.; Muneta, T.; Ishikawa, I. Stem Cell Properties of Human Periodontal Ligament Cells. J. Periodontal Res. 2006, 41, 303–310. [Google Scholar] [CrossRef]
- Itaya, T.; Kagami, H.; Okada, K.; Yamawaki, A.; Narita, Y.; Inoue, M.; Sumita, Y.; Ueda, M. Characteristic Changes of Periodontal Ligament-Derived Cells during Passage. J. Periodontal Res. 2009, 44, 425–433. [Google Scholar] [CrossRef]
- Gimble, J.M.; Katz, A.J.; Bunnell, B.A. Adipose-Derived Stem Cells for Regenerative Medicine. Circ. Res. 2007, 100, 1249–1260. [Google Scholar] [CrossRef]
- Dos Santos, F.; Andrade, P.Z.; Boura, J.S.; Abecasis, M.M.; da Silva, C.L.; Cabral, J.M.S. Ex Vivo Expansion of Human Mesenchymal Stem Cells: A More Effective Cell Proliferation Kinetics and Metabolism under Hypoxia. J. Cell. Physiol. 2009, 223, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Moreno Sancho, F.; Leira, Y.; Orlandi, M.; Buti, J.; Giannobile, W.V.; D’Aiuto, F. Cell-Based Therapies for Alveolar Bone and Periodontal Regeneration: Concise Review. Stem Cells Transl. Med. 2019, 8, 1286–1295. [Google Scholar] [CrossRef] [PubMed]
- Ouchi, T.; Nakagawa, T. Mesenchymal Stem Cell-Based Tissue Regeneration Therapies for Periodontitis. Regen. Ther. 2020, 14, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Winning, L.; El Karim, I.A.; Lundy, F.T. A Comparative Analysis of the Osteogenic Potential of Dental Mesenchymal Stem Cells. Stem Cells Dev. 2019, 28, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Wada, N.; Menicanin, D.; Shi, S.; Bartold, P.M.; Gronthos, S. Immunomodulatory Properties of Human Periodontal Ligament Stem Cells. J. Cell. Physiol. 2009, 219, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Banavar, S.R.; Rawal, S.Y.; Paterson, I.C.; Singh, G.; Davamani, F.; Khoo, S.P.; Tan, E.L. Establishing a Technique for Isolation and Characterization of Human Periodontal Ligament Derived Mesenchymal Stem Cells. Saudi Dent. J. 2020, 33, 693–701. [Google Scholar] [CrossRef]
- Xu, L.; Liu, Y.; Sun, Y.; Wang, B.; Xiong, Y.; Lin, W.; Wei, Q.; Wang, H.; He, W.; Wang, B.; et al. Tissue Source Determines the Differentiation Potentials of Mesenchymal Stem Cells: A Comparative Study of Human Mesenchymal Stem Cells from Bone Marrow and Adipose Tissue. Stem Cell Res. Ther. 2017, 8, 275. [Google Scholar] [CrossRef]
- Mohamed-Ahmed, S.; Fristad, I.; Lie, S.A.; Suliman, S.; Mustafa, K.; Vindenes, H.; Idris, S.B. Adipose-Derived and Bone Marrow Mesenchymal Stem Cells: A Donor-Matched Comparison. Stem Cell Res. Ther. 2018, 9, 168. [Google Scholar] [CrossRef]
- Kobolak, J.; Dinnyes, A.; Memic, A.; Khademhosseini, A.; Mobasheri, A. Mesenchymal Stem Cells: Identification, Phenotypic Characterization, Biological Properties and Potential for Regenerative Medicine through Biomaterial Micro-Engineering of Their Niche. Methods 2016, 99, 62–68. [Google Scholar] [CrossRef]
- Tamaki, Y.; Nakahara, T.; Ishikawa, H.; Sato, S. In Vitro Analysis of Mesenchymal Stem Cells Derived from Human Teeth and Bone Marrow. Odontology 2013, 101, 121–132. [Google Scholar] [CrossRef]
- Petrenko, Y.; Vackova, I.; Kekulova, K.; Chudickova, M.; Koci, Z.; Turnovcova, K.; Kupcova Skalnikova, H.; Vodicka, P.; Kubinova, S. A Comparative Analysis of Multipotent Mesenchymal Stromal Cells Derived from Different Sources, with a Focus on Neuroregenerative Potential. Sci. Rep. 2020, 10, 4290. [Google Scholar] [CrossRef]
- Yang, Y.-H.K.; Ogando, C.R.; Wang See, C.; Chang, T.-Y.; Barabino, G.A. Changes in Phenotype and Differentiation Potential of Human Mesenchymal Stem Cells Aging in Vitro. Stem Cell Res. Ther. 2018, 9, 131. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; Liu, G.; Banie, L.; Wang, G.; Ning, H.; Lue, T.F.; Lin, C.-S. Tissue Distribution of Mesenchymal Stem Cell Marker Stro-1. Stem Cells Dev. 2011, 20, 1747–1752. [Google Scholar] [CrossRef] [PubMed]
- Lv, F.-J.; Tuan, R.S.; Cheung, K.M.C.; Leung, V.Y.L. Concise Review: The Surface Markers and Identity of Human Mesenchymal Stem Cells. Stem Cells 2014, 32, 1408–1419. [Google Scholar] [CrossRef] [PubMed]
- Guezguez, B.; Vigneron, P.; Lamerant, N.; Kieda, C.; Jaffredo, T.; Dunon, D. Dual Role of Melanoma Cell Adhesion Molecule (MCAM)/CD146 in Lymphocyte Endothelium Interaction: MCAM/CD146 Promotes Rolling via Microvilli Induction in Lymphocyte and Is an Endothelial Adhesion Receptor. J. Immunol. 2007, 179, 6673–6685. [Google Scholar] [CrossRef]
- Ma, L.; Huang, Z.; Wu, D.; Kou, X.; Mao, X.; Shi, S. CD146 Controls the Quality of Clinical Grade Mesenchymal Stem Cells from Human Dental Pulp. Stem Cell Res. Ther. 2021, 12, 488. [Google Scholar] [CrossRef]
- Yamada, S.; Kitamura, M.; Murakami, S. PLAP-1: A Novel Molecule Regulating Homeostasis of Periodontal Tissues. Jpn. Dent. Sci. Rev. 2008, 44, 137–144. [Google Scholar] [CrossRef]
- Stein, G.S.; Lian, J.B.; Owen, T.A. Relationship of Cell Growth to the Regulation of Tissue-Specific Gene Expression during Osteoblast Differentiation. FASEB J. 1990, 4, 3111–3123. [Google Scholar] [CrossRef]
- Li, X.; Bai, J.; Ji, X.; Li, R.; Xuan, Y.; Wang, Y. Comprehensive Characterization of Four Different Populations of Human Mesenchymal Stem Cells as Regards Their Immune Properties, Proliferation and Differentiation. Int. J. Mol. Med. 2014, 34, 695–704. [Google Scholar] [CrossRef]
- Raheja, L.F.; Genetos, D.C.; Yellowley, C.E. Hypoxic Osteocytes Recruit Human MSCs through an OPN/CD44-Mediated Pathway. Biochem. Biophys. Res. Commun. 2008, 366, 1061–1066. [Google Scholar] [CrossRef]
- Zou, C.; Luo, Q.; Qin, J.; Shi, Y.; Yang, L.; Ju, B.; Song, G. Osteopontin Promotes Mesenchymal Stem Cell Migration and Lessens Cell Stiffness via Integrin Β1, FAK, and ERK Pathways. Cell Biochem. Biophys. 2013, 65, 455–462. [Google Scholar] [CrossRef]
- Rogall, R.; Rabenstein, M.; Vay, S.; Bach, A.; Pikhovych, A.; Baermann, J.; Hoehn, M.; Couillard-Despres, S.; Fink, G.R.; Schroeter, M.; et al. Bioluminescence Imaging Visualizes Osteopontin-Induced Neurogenesis and Neuroblast Migration in the Mouse Brain after Stroke. Stem Cell Res. Ther. 2018, 9, 182. [Google Scholar] [CrossRef] [PubMed]
- Poggio, P.; Grau, J.B.; Field, B.C.; Sainger, R.; Seefried, W.F.; Rizzolio, F.; Ferrari, G. Osteopontin Controls Endothelial Cell Migration in Vitro and in Excised Human Valvular Tissue from Patients with Calcific Aortic Stenosis and Controls. J. Cell. Physiol. 2011, 226, 2139–2149. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.K.; Johnston, H.M.; Whitty, G.A.; Williams, B.; Webb, R.J.; Denhardt, D.T.; Bertoncello, I.; Bendall, L.J.; Simmons, P.J.; Haylock, D.N. Osteopontin, a Key Component of the Hematopoietic Stem Cell Niche and Regulator of Primitive Hematopoietic Progenitor Cells. Blood 2005, 106, 1232–1239. [Google Scholar] [CrossRef]
- Nojima, N.; Kobayashi, M.; Shionome, M.; Takahashi, N.; Suda, T.; Hasegawa, K. Fibroblastic Cells Derived from Bovine Periodontal Ligaments Have the Phenotypes of Osteoblasts. J. Periodontal Res. 1990, 25, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Basdra, E.K.; Komposch, G. Osteoblast-like Properties of Human Periodontal Ligament Cells: An in Vitro Analysis. Eur. J. Orthod. 1997, 19, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Pei, X.; Zhao, Y.; Tulu, U.S.; Liu, B.; Helms, J.A. A Wnt-Responsive PDL Population Effectuates Extraction Socket Healing. J. Dent. Res. 2018, 97, 803–809. [Google Scholar] [CrossRef]
- Yu, Z.; Philippe, G. Differential Properties of Human ALP+ Periodontal Ligament Stem Cells vs Their ALP− Counterparts. J. Stem Cell Res. Ther. 2015, 5, 292. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.T.; Penny, C.B.; Paiker, J.E.; Psaras, G.; Ikram, F.; Crowther, N.J. The Relationship between Alkaline Phosphatase Activity and Intracellular Lipid Accumulation in Murine 3T3-L1 Cells and Human Preadipocytes. Anal. Biochem. 2006, 354, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Ferris, W.; Penny, C.; Van der Merwe, M.-T.; Jacobson, B.; Paiker, J.; Crowther, N. Lipid Accumulation and Alkaline Phosphatase Activity in Human Preadipocytes Isolated from Different Body Fat Depots. J. Endocrinol. Metab. Diabetes S. Afr. 2013, 18, 58–64. [Google Scholar] [CrossRef]
- Birmingham, E.; Niebur, G.; McHugh, P.; Shaw, G.; Barry, F.; McNamara, L. Osteogenic Differentiation of Mesenchymal Stem Cells Is Regulated by Osteocyte and Osteoblast Cells in a Simplified Bone Niche. Eur. Cells Mater. 2012, 23, 13–27. [Google Scholar] [CrossRef]
- Hayrapetyan, A.; Jansen, J.A.; van den Beucken, J.J.J.P. Signaling Pathways Involved in Osteogenesis and Their Application for Bone Regenerative Medicine. Tissue Eng. Part B Rev. 2015, 21, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.S.; Poundarik, A.A.; Cabral, J.M.S.; da Silva, C.L.; Vashishth, D. Biomimetic Matrices for Rapidly Forming Mineralized Bone Tissue Based on Stem Cell-Mediated Osteogenesis. Sci. Rep. 2018, 8, 14388. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.S.; Cabral, J.M.; da Silva, C.L.; Vashishth, D. Synergistic Effect of Extracellularly Supplemented Osteopontin and Osteocalcin on Stem Cell Proliferation, Osteogenic Differentiation, and Angiogenic Properties. J. Cell. Biochem. 2019, 120, 6555–6569. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, F.; Zhang, N.; Geng, X.; Meng, C.; Wang, X.; Yang, Y. Osteogenic Capacity and Cytotherapeutic Potential of Periodontal Ligament Cells for Periodontal Regeneration in Vitro and in Vivo. PeerJ 2019, 7, e6589. [Google Scholar] [CrossRef]
- Kadokura, H.; Yamazaki, T.; Masuda, Y.; Kato, Y.; Hasegawa, A.; Sakagami, H.; Yokose, S. Establishment of a Primary Culture System of Human Periodontal Ligament Cells That Differentiate into Cementum Protein 1-Expressing Cementoblast-like Cells. In Vivo 2019, 33, 349–352. [Google Scholar] [CrossRef]
- Arzate, H.; Olson, S.W.; Page, R.C.; Gown, A.M.; Narayanan, A.S. Production of a Monoclonal Antibody to an Attachment Protein Derived from Human Cementum. FASEB J. 1992, 6, 2990–2995. [Google Scholar] [CrossRef]
- McCulloch, C.A.G.; Melcher, A.H. Cell Density and Cell Generation in the Periodontal Ligament of Mice. Am. J. Anat. 1983, 167, 43–58. [Google Scholar] [CrossRef]
- Shinagawa-Ohama, R.; Mochizuki, M.; Tamaki, Y.; Suda, N.; Nakahara, T. Heterogeneous Human Periodontal Ligament-Committed Progenitor and Stem Cell Populations Exhibit a Unique Cementogenic Property Under In Vitro and In Vivo Conditions. Stem Cells Dev. 2017, 26, 632–645. [Google Scholar] [CrossRef]
- Kii, I.; Amizuka, N.; Minqi, L.; Kitajima, S.; Saga, Y.; Kudo, A. Periostin Is an Extracellular Matrix Protein Required for Eruption of Incisors in Mice. Biochem. Biophys. Res. Commun. 2006, 342, 766–772. [Google Scholar] [CrossRef]
- Rios, H.; Koushik, S.V.; Wang, H.; Wang, J.; Zhou, H.-M.; Lindsley, A.; Rogers, R.; Chen, Z.; Maeda, M.; Kruzynska-Frejtag, A.; et al. Periostin Null Mice Exhibit Dwarfism, Incisor Enamel Defects, and an Early-Onset Periodontal Disease-Like Phenotype. Mol. Cell. Biol. 2005, 25, 11131–11144. [Google Scholar] [CrossRef]
- Iwata, T.; Yamato, M.; Washio, K.; Yoshida, T.; Tsumanuma, Y.; Yamada, A.; Onizuka, S.; Izumi, Y.; Ando, T.; Okano, T.; et al. Periodontal Regeneration with Autologous Periodontal Ligament-Derived Cell Sheets—A Safety and Efficacy Study in Ten Patients. Regen. Ther. 2018, 9, 38–44. [Google Scholar] [CrossRef]
- Zhao, Y.; Gong, Y.; Liu, X.; He, J.; Zheng, B.; Liu, Y. The Experimental Study of Periodontal Ligament Stem Cells Derived Exosomes with Hydrogel Accelerating Bone Regeneration on Alveolar Bone Defect. Pharmaceutics 2022, 14, 2189. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, P.; Wang, Y.; Li, J.; Qiao, D.; Chen, R.; Yang, W.; Yan, F. Gold Nanoparticles Promote the Bone Regeneration of Periodontal Ligament Stem Cell Sheets Through Activation of Autophagy. Int. J. Nanomed. 2021, 16, 61–73. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).