Acute Kidney Injury in Hospitalized Patients with COVID-19: Risk Factors and Serum Biomarkers
Abstract
1. Introduction
2. Materials and Methods
2.1. The Biomarkers Levels Assessment
2.2. Statistical Analysis
3. Results
3.1. Subject Characteristics
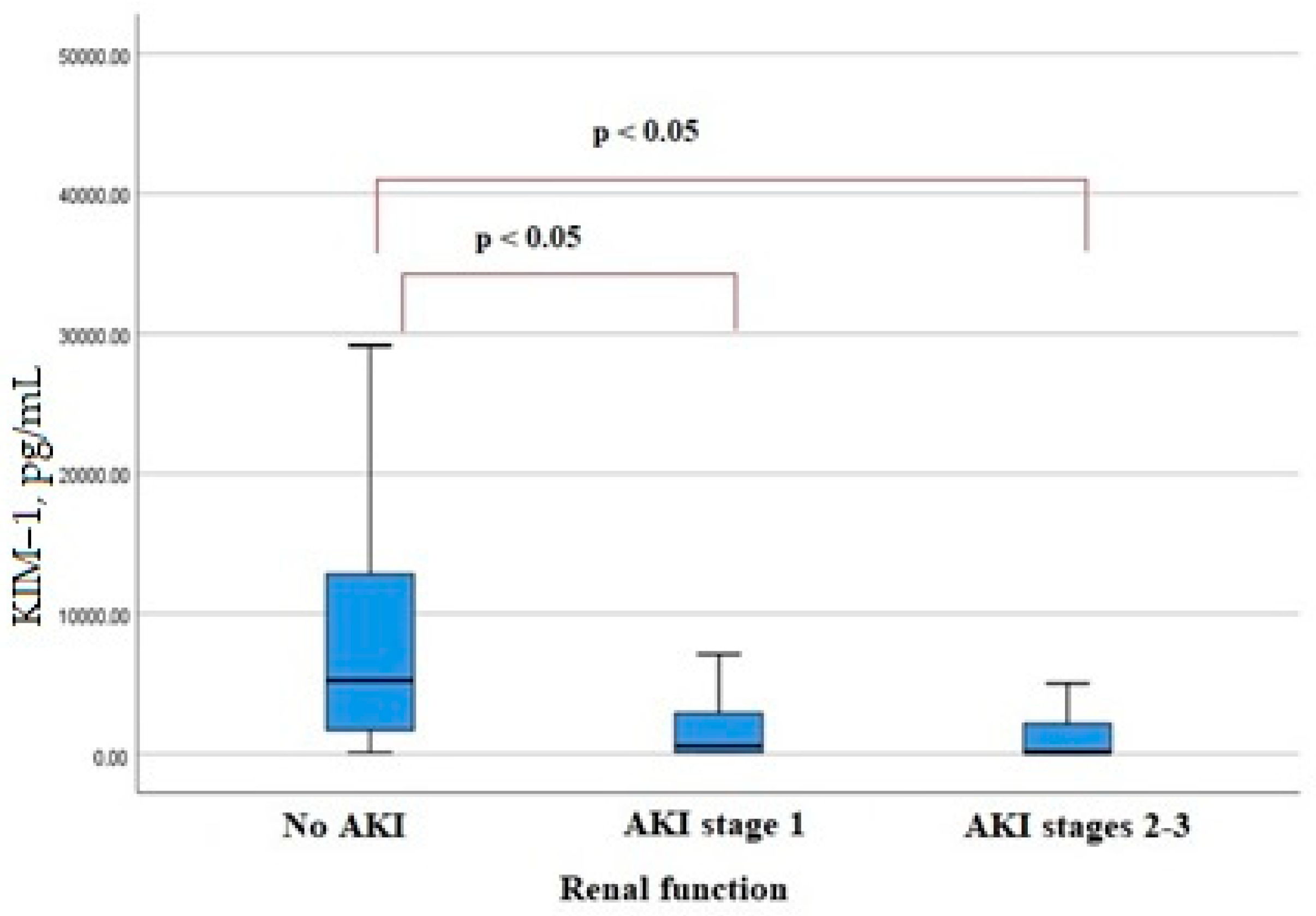
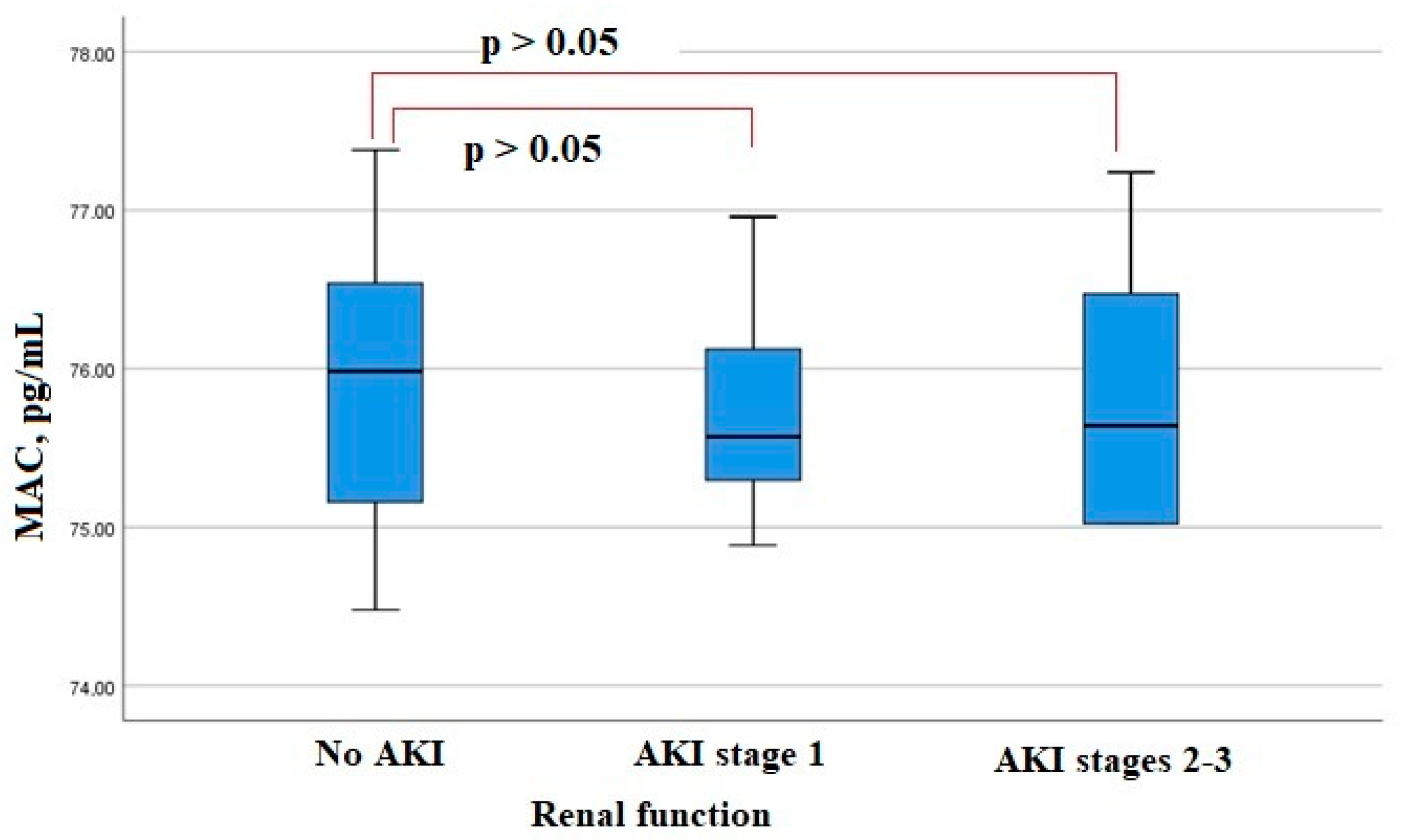
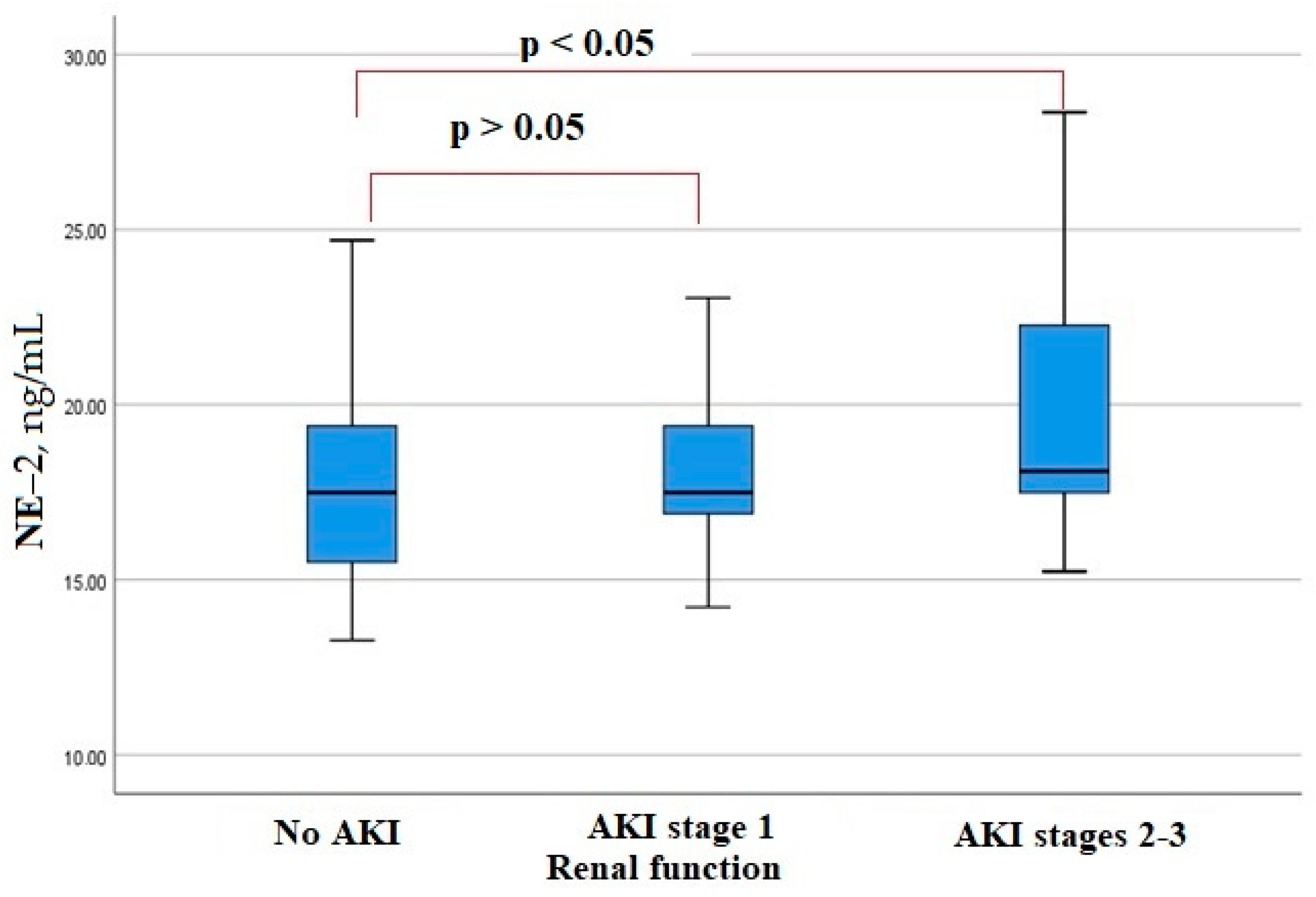
3.2. Serum Angiopoetin-1, KIM-1, Neutrophil Elastase 2, MAC Levels in Patients with COVID-19
3.3. Uni- and Multifactorial Regression Analysis
3.4. ROC Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Ali, H.; Daoud, A.; Mohamed, M.M.; Salim, S.A.; Yessayan, L.; Baharani, J.; Murtazaf, A.; Rao, V.; Soliman, K.M. Survival rate in acute kidney injury superimposed COVID-19 patients: A systematic review and meta-analysis. Ren. Fail. 2020, 42, 393–397. [Google Scholar] [CrossRef]
- Hirsch, J.S.; Ng, J.H.; Ross, D.W.; Sharma, P.; Shah, H.H.; Barnett, R.L.; Hazzan, A.D.; Fishbane, S.; Jhaveri, K.D. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020, 98, 209–218. [Google Scholar] [CrossRef]
- Lin, L.; Wang, X.; Ren, J.; Sun, Y.; Yu, R.; Li, K.; Zheng, L.; Yang, J. Risk factors and prognosis for COVID-19-induced acute kidney injury: A meta-analysis. BMJ. Open 2020, 10, e042573. [Google Scholar] [CrossRef]
- Li, X.Q.; Liu, H.; Meng, Y.; Yin, H.Y.; Gao, W.Y.; Yang, X.; Xu, D.-S.; Cai, X.-D.; Guan, Y.; Lerman, L.O.; et al. Critical roles of cytokine storm and secondary bacterial infection in acute kidney injury development in COVID-19: A multi-center retrospective cohort study. J. Med. Virol. 2021, 93, 6641–6652. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with COVID-19. New Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Braun, F.; Lütgehetmann, M.; Pfefferle, S.; Wong, M.N.; Carsten, A.; Lindenmeyer, M.T.; Nörz, D.; Heinrich, F.; Meißner, K.; Wichmann, D.; et al. SARS-CoV-2 renal tropism associates with acute kidney injury. Lancet 2020, 396, 597–598. [Google Scholar] [CrossRef]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020, 220, 1–13. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Salehi, S.; Abedi, A.; Balakrishnan, S.; Gholamrezanezhad, A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. Am. J. Roentgenol. 2020, 215, 87–93. [Google Scholar] [CrossRef]
- Summary of Recommendation Statements. Kidney Int. Suppl. (2011) 2012, 2, 8–12. [CrossRef]
- Chan, L.; Chaudhary, K.; Saha, A.; Chauhan, K.; Vaid, A.; Zhao, S.; Paranjpe, I.; Somani, S.; Richter, F.; Miotto, R.; et al. AKI in Hospitalized Patients with COVID-19. J. Am. Soc. Nephrol. 2021, 32, 151–160. [Google Scholar] [CrossRef]
- Feng, X.; Li, P.; Ma, L.; Liang, H.; Lei, J.; Li, W.; Wang, K.; Song, Y.; Li, S.; Yang, W.; et al. Clinical Characteristics and Short-Term Outcomes of Severe Patients With COVID-19 in Wuhan, China. Front. Med. 2020, 7, 491. [Google Scholar] [CrossRef]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Sullivan, M.K.; Lees, J.S.; Drake, T.M.; Docherty, A.B.; Oates, G.; Hardwick, H.E.; Russell, C.D.; Merson, L.; Dunning, J.; Nguyen-Van-Tam, J.S.; et al. Acute kidney injury in patients hospitalized with COVID-19 from the ISARIC WHO CCP-UK Study: A prospective, multicentre cohort study. Nephrol. Dial. Transplant. 2022, 37, 271–284. [Google Scholar] [CrossRef]
- Fang, L.; Karakiulakis, G.; Roth, M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020, 8, e21. [Google Scholar] [CrossRef]
- Kolhe, N.V.; Fluck, R.J.; Selby, N.M.; Taal, M.W. Acute kidney injury associated with COVID-19: A retrospective cohort study. PLoS Med. 2020, 17, e1003406. [Google Scholar] [CrossRef]
- Ng, J.H.; Bijol, V.; Sparks, M.A.; Sise, M.E.; Izzedine, H.; Jhaveri, K.D. Pathophysiology and Pathology of Acute Kidney Injury in Patients With COVID-19. Adv. Chronic. Kidney Dis. 2020, 27, 365–376. [Google Scholar] [CrossRef]
- Aulagnon, F.; Lapidus, N.; Canet, E.; Galicier, L.; Boutboul, D.; Peraldi, M.N.; Reuter, D.; Bernard, R.; Schlemmer, B.; Azoulay, E.; et al. Acute kidney injury in adults with hemophagocytic lymphohistiocytosis. Am. J. Kidney Dis. 2015, 65, 851–859. [Google Scholar] [CrossRef]
- Yildirim, C.; Ozger, H.S.; Yasar, E.; Tombul, N.; Gulbahar, O.; Yildiz, M.; Bozdayi, G.; Derici, U.; Dizbay, M. Early predictors of acute kidney injury in COVID-19 patients. Nephrology 2021, 26, 513–521. [Google Scholar] [CrossRef]
- Maisonpierre, P.C.; Suri, C.; Jones, P.F.; Bartunkova, S.; Wiegand, S.J.; Radziejewski, C.; Compton, D.; McClain, J.; Aldrich, T.H.; Papadopoulos, N.; et al. Angiopoietin-2, a Natural Antagonist for Tie2 That Disrupts in vivo Angiogenesis. Science 1997, 277, 55–60. [Google Scholar] [CrossRef]
- Ricciuto, D.R.; dos Santos, C.C.; Hawkes, M.; Toltl, L.J.; Conroy, A.L.; Rajwans, N.; Lafferty, E.I.; Cook, D.J.; Fox-Robichaud, A.; Kahnamoui, K.; et al. Angiopoietin-1 and angiopoietin-2 as clinically informative prognostic biomarkers of morbidity and mortality in severe sepsis. Crit. Care Med. 2011, 39, 702–710. [Google Scholar] [CrossRef]
- Henry, B.M.; de Oliveira MH, S.; Cheruiyot, I.; Benoit, J.; Rose, J.; Favaloro, E.J.; Lippi, G.; Benoit, S.; Shakked, N.P. Cell-Free DNA, Neutrophil extracellular traps (NETs), and Endothelial Injury in Coronavirus Disease 2019–(COVID-19–) Associated Acute Kidney Injury. Mediat. Inflamm 2022, 2022, 9339411. [Google Scholar] [CrossRef]
- Zucoloto, A.Z.; Jenne, C.N. Platelet-Neutrophil Interplay: Insights into Neutrophil Extracellular Trap (NET)-Driven Coagulation in Infection. Front. Cardiovasc. Med. 2019, 6, 85. [Google Scholar] [CrossRef]
- Vogel, M.J.; Mustroph, J.; Staudner, S.T.; Leininger, S.B.; Hubauer, U.; Wallner, S.; Meindl, C.; Hanses, F.; Zimmermann, M.; Maier, L.S.; et al. Kidney injury molecule-1: Potential biomarker of acute kidney injury and disease severity in patients with COVID-19. J. Nephrol. 2021, 34, 1007–1018. [Google Scholar] [CrossRef]
- Huang, Y.; Craig Don-Wauchope, A. The Clinical Utility of Kidney Injury Molecule 1 in the Prediction, Diagnosis and Prognosis of Acute Kidney Injury: A Systematic Review. Inflamm Allergy Drug Targets. 2011, 10, 260–271. [Google Scholar] [CrossRef]
- Kerget, B.; Kerget, F.; Aksakal, A.; Aşkın, S.; Uçar, E.Y.; Sağlam, L. Evaluation of the relationship between KIM-1 and suPAR levels and clinical severity in COVID-19 patients: A different perspective on suPAR. J. Med. Virol. 2021, 93, 5568–5573. [Google Scholar] [CrossRef]
- Ichimura, T.; Nasr, M.L.; Yu SM, W.; Mori, Y.; Bonventre, J.V. Kidney injury molecule 1 is a receptor for SARS-CoV-2. J. Am. Soc. Nephrol. 2020, 31, 296. [Google Scholar]
- Karmakova, T.A.; Sergeeva, N.S.; Kanukoev KYu Alekseev BYa Kaprin, A.D. Kidney Injury Molecule 1 (KIM-1): A Multifunctional Glycoprotein and Biological Marker (Review). Sovrem. Tehnol. V Medicine. 2021, 13, 64. [Google Scholar] [CrossRef]
- Pfister, F.; Vonbrunn, E.; Ries, T.; Jäck, H.M.; Überla, K.; Lochnit, G.; Sheriff, A.; Herrmann, M.; Büttner-Herold, M.; Amann, K.; et al. Complement Activation in Kidneys of Patients With COVID-19. Front. Immunol. 2021, 11, 594849. [Google Scholar] [CrossRef]
- Larisa, A.; Anastasia, S.; Victoria, S.; Michael, B.; Sergey, M.; Alisa, Y.; Denis, K. Association between type of antihyperglycemic therapy and COVID-19 outcomes in patients with type 2 DM. Eur. Respir. J. Sep. 2021, 58 (Suppl. S65), PA3653. [Google Scholar] [CrossRef]
- Do, J.Y.; Kim, S.W.; Park, J.W.; Cho, K.H.; Kang, S.H. Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19? Diabetes Metab. 2021, 47, 101208. [Google Scholar] [CrossRef]
- Luo, P.; Qiu, L.; Liu, Y.; Liu, X.L.; Zheng, J.L.; Xue, H.Y.; Liu, W.H.; Liu, D.; Li, J. Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis. Am. J. Trop Med. Hyg. 2020, 103, 69–72. [Google Scholar] [CrossRef]
- Bell, S.; Farran, B.; McGurnaghan, S.; McCrimmon, R.J.; Leese, G.P.; Petrie, J.R.; McKeigue, P.; Sattar, N.; Wild, S.; McKnight, J.; et al. Risk of acute kidney injury and survival in patients treated with Metformin: An observational cohort study. BMC Nephrol. 2017, 8, 163. [Google Scholar] [CrossRef]
- Saisho, Y. Metformin and Inflammation: Its Potential Beyond Glucose-lowering Effect. Endocr. Metab. Immune Disord. Drug Targets. 2015, 15, 196–205. [Google Scholar] [CrossRef]
- Kim, J.; You, Y.J. Regulation of organelle function by metformin. IUBMB Life. 2017, 69, 459–469. [Google Scholar] [CrossRef]
- Xin, G.; Wei, Z.; Ji, C.; Zheng, H.; Gu, J.; Ma, L.; Huang, W.; Morris-Natschke, S.L.; Yeh, J.-L.; Zhang, R.; et al. Metformin Uniquely Prevents Thrombosis by Inhibiting Platelet Activation and mtDNA Release. Sci. Rep. 2016, 6, 36222. [Google Scholar] [CrossRef]
- Menegazzo, L.; Scattolini, V.; Cappellari, R.; Bonora, B.M.; Albiero, M.; Bortolozzi, M.; Romanato, F.; Ceolotto, G.; de Kreutzeberg, S.V.; Avogaro, A.; et al. The antidiabetic drug metformin blunts NETosis in vitro and reduces circulating NETosis biomarkers in vivo. Acta. Diabetol. 2018, 55, 593–601. [Google Scholar] [CrossRef]
- Cameron, A.R.; Morrison, V.L.; Levin, D.; Mohan, M.; Forteath, C.; Beall, C.; McNeilly, A.D.; Balfour, D.J.K.; Savinko, T.; Wong, A.K.F.; et al. Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status. Circ. Res. 2016, 119, 652–665. [Google Scholar] [CrossRef]


| Parameters | General Cohort (n = 500) | AKI Group (n = 190) | No AKI Group (n = 310) | p-Value |
|---|---|---|---|---|
| Age, years | 73 [63; 80] | 76 [65.75; 82] | 71.5 [59; 79] | 0.001 |
| Men, n (%) | 231 (46.2%) | 104 (54.7%) | 127 (41%) | 0.003 |
| Comorbidities: | ||||
| AH, n (%) | 362 (72.4%) | 151 (79.5%) | 211 (68.1%) | 0.006 |
| DM, n (%) | 124 (24.8%) | 53 (27.9%) | 71 (22.9%) | 0.21 |
| History of MI, n (%) | 50 (10%) | 29 (15.3%) | 21 (6.8%) | 0.002 |
| AF, n (%) | 74 (14.8%) | 38 (20%) | 36 (11.6%) | 0.01 |
| CKD C3-4, n (%) | 117 (23.4%) | 57 (30%) | 60 (19.4%) | 0.008 |
| CHD III-IV FC, n (%) | 47 (9.4%) | 35 (18.4%) | 12 (3.9%) | 0.0001 |
| BMI, kg/m2 | 28.4 [25.4; 32] | 28.9 [25.8; 32.9] | 28.1 [25.15; 31.7] | 0.197 |
| Obesity, n (%) | 188 (37.6%) | 78 (41.1%) | 110 (35.5%) | 0.154 |
| Maximum area of lung damage on chest CT: | 0.0001 | |||
| No pneumonia, n (%) | 5 (1%) | 2 (1.1%) | 3 (1%) | |
| Less than 25%, n (%) | 98 (19.6%) | 31 (16.3%) | 67 (21.6%) | |
| 25–50%, n (%) | 191 (38.2%) | 61 (32.1%) | 130 (41.9%) | |
| 51–75%, n (%) | 150 (30%) | 54 (28.4%) | 81 (26.1%) | |
| More than 75%, n (%) | 50 (10%) | 11 (5.8%) | 8 (2.6%) | |
| Oxygen saturation on admission, % | 95 [92; 96] | 94 [91; 96] | 95 [93; 96] | 0.024 |
| AKI, n (%) | 190 (38%) | |||
| Stage 1, n (%) | 151 (79.5%) | |||
| Stage 2, n (%) | 25 (13.1%) | |||
| Stage 3, n (%) | 14 (7.4%) | |||
| Respiratory support | 0.0001 | |||
| Oxygen insufflation, n (%) | 194 (38.8%) | 74 (38.9%) | 120 (38.7%) | |
| Mechanical ventilation: | ||||
| Non-invasive, n (%) | 8 (1.6%) | 8 (4.2%) | - | |
| Invasive, n (%) | 50 (10%) | 43 (22.6%) | 7 (2.3%) | |
| Glucocorticoids, n (%), | 357 (71.4%) | 135 (71.1%) | 222 (71.6%) | 0.893 |
| Antibiotics, n (%) | 325 (65%) | 157 (82.6%) | 168 (54.2%) | 0.0001 |
| Beta-lactames/fluorochinolones, n (%) | 285 (57%) | 126 (25.2%) | 159 (31.8%) | 0.0001 |
| Amikacine/Vancomycine/Colistine/, n (%) | 40 (8%) | 37 (19.5%) | 3 (1%) | 0.0001 |
| Immunobiological drugs (tocilizumab, olokizumab, levilimab), n (%) | 108 (21.6%) | 55 (28.9%) | 53 (17.1%) | 0.002 |
| Hydroxychloroquine, n (%) | 83 (16.6%) | 42 (22.1%) | 41 (13.2%) | 0.01 |
| Azithromycine, n (%) | 71 (14.2%) | 35 (18.4%) | 36 (11.6%) | 0.01 |
| Diuretics, n (%) | 104 (20.8%) | 50 (26.3%) | 54 (17.4%) | 0.02 |
| iACE/ARB, n (%) | 217 (43.4%) | 79 (41.6%) | 138 (44.5%) | 0.461 |
| Metformin, n (%) | 67 (13.4%) | 24 (12.6%) | 43 (13.9%) | 0.03 |
| Inotropes, n (%) | 33 (6.6%) | 29 (15.3%) | 4 (1.3%) | 0.001 |
| ICU admission, n (%) | 76 (15.2%) | 65 (34.2%) | 11 (3.5%) | 0.0001 |
| Outcomes: | 0.0001 | |||
| Discharged, n (%) | 416 (83.2%) | 123 (64.7%) | 293 (94.5%) | |
| Died, n (%) | 84 (16.8%) | 67 (35.3%) | 17 (5.5%) | |
| Duration of hospitalization, days | 12 [9; 15] | 14 [10; 18] | 11 [9; 14] | 0.0001 |
| Factor | OR (95% CI) | p-Value | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Unifactorial logistic regression | Multifactorial logistic regression | |||
| Male sex | 1.7 (1.2–2.5) | 0.003 | 2.1 (1.4–3.1) | 0.0001 |
| CHD III-IV FC | 5.6 (2.8–11.2) | 0.0001 | 4 (1.9–8.2) | 0.0001 |
| ELA2, ng/mL | 1 (0.9–1.1) | 0.313 | ||
| Ang-1, ng/mL | 5.7 (1.7–19.1) | 0.005 | 5.8 (1.7–20) | 0.006 |
| MAC, pg/mL | 0.9 (0.9–1.1) | 0.572 | ||
| KIM-1, pg/mL | 0.56 (0.46–0.68) | 0.038 | 1 (1–1) | 0.036 |
| Minimal lymphocytes | 0.4 (0.3–0.7) | 0.0001 | 0.005 (0–0.9) | 0.049 |
| Minimal fibrinogen | 0.7 (0.6–0.8) | 0.0001 | 0.2 (0.1–0.8) | 0.002 |
| Proteinuria | 1.8 (1.1–2.9) | 0.021 | 1.2 (1.1–1.4) | 0.049 |
| Antibiotics | 3.9 (2.6–6.2) | 0.0001 | 1.9 (1.1–3.3) | 0.019 |
| Metformin | 0.6 (0.3–0.9) | 0.022 | 0.4 (0.2–0.7) | 0.002 |
| Mechanical ventilation | 2.6 (2–3.3) | 0.0001 | 2.2 (1.7–2.9) | 0.0001 |
| Cut-Point | Sensitivity, % | Specificity, % | PPV (%) | NPV (%) | AUC (95% CI) |
|---|---|---|---|---|---|
| Ang-1 | |||||
| 1.66 ng/mL | 63.6 | 68.6 | 73.7 | 57.9 | 0.69 (0.58–0.81) |
| KIM-1 | |||||
| 905.1 pg/mL | 93.3 | 52 | 53.9 | 92.9 | 0.72 (0.51–0.85) |
| ELA-2 | |||||
| 20.075 ng/mL | 53.4 | 84.6 | 60 | 78.6 | 0.67 (0.47–0.71) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shchepalina, A.; Chebotareva, N.; Akulkina, L.; Brovko, M.; Sholomova, V.; Androsova, T.; Korotchaeva, Y.; Kalmykova, D.; Tanaschuk, E.; Taranova, M.; et al. Acute Kidney Injury in Hospitalized Patients with COVID-19: Risk Factors and Serum Biomarkers. Biomedicines 2023, 11, 1246. https://doi.org/10.3390/biomedicines11051246
Shchepalina A, Chebotareva N, Akulkina L, Brovko M, Sholomova V, Androsova T, Korotchaeva Y, Kalmykova D, Tanaschuk E, Taranova M, et al. Acute Kidney Injury in Hospitalized Patients with COVID-19: Risk Factors and Serum Biomarkers. Biomedicines. 2023; 11(5):1246. https://doi.org/10.3390/biomedicines11051246
Chicago/Turabian StyleShchepalina, Anastasia, Natalia Chebotareva, Larissa Akulkina, Mikhail Brovko, Viktoria Sholomova, Tatiana Androsova, Yulia Korotchaeva, Diana Kalmykova, Elena Tanaschuk, Marina Taranova, and et al. 2023. "Acute Kidney Injury in Hospitalized Patients with COVID-19: Risk Factors and Serum Biomarkers" Biomedicines 11, no. 5: 1246. https://doi.org/10.3390/biomedicines11051246
APA StyleShchepalina, A., Chebotareva, N., Akulkina, L., Brovko, M., Sholomova, V., Androsova, T., Korotchaeva, Y., Kalmykova, D., Tanaschuk, E., Taranova, M., Lebedeva, M., Beketov, V., & Moiseev, S. (2023). Acute Kidney Injury in Hospitalized Patients with COVID-19: Risk Factors and Serum Biomarkers. Biomedicines, 11(5), 1246. https://doi.org/10.3390/biomedicines11051246






