Inflammatory Markers as Predictors of Shunt Dependency and Functional Outcome in Patients with Aneurysmal Subarachnoid Hemorrhage
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Sample Collection
2.2. Inflammatory Panel
2.3. Statistical Analysis
3. Results
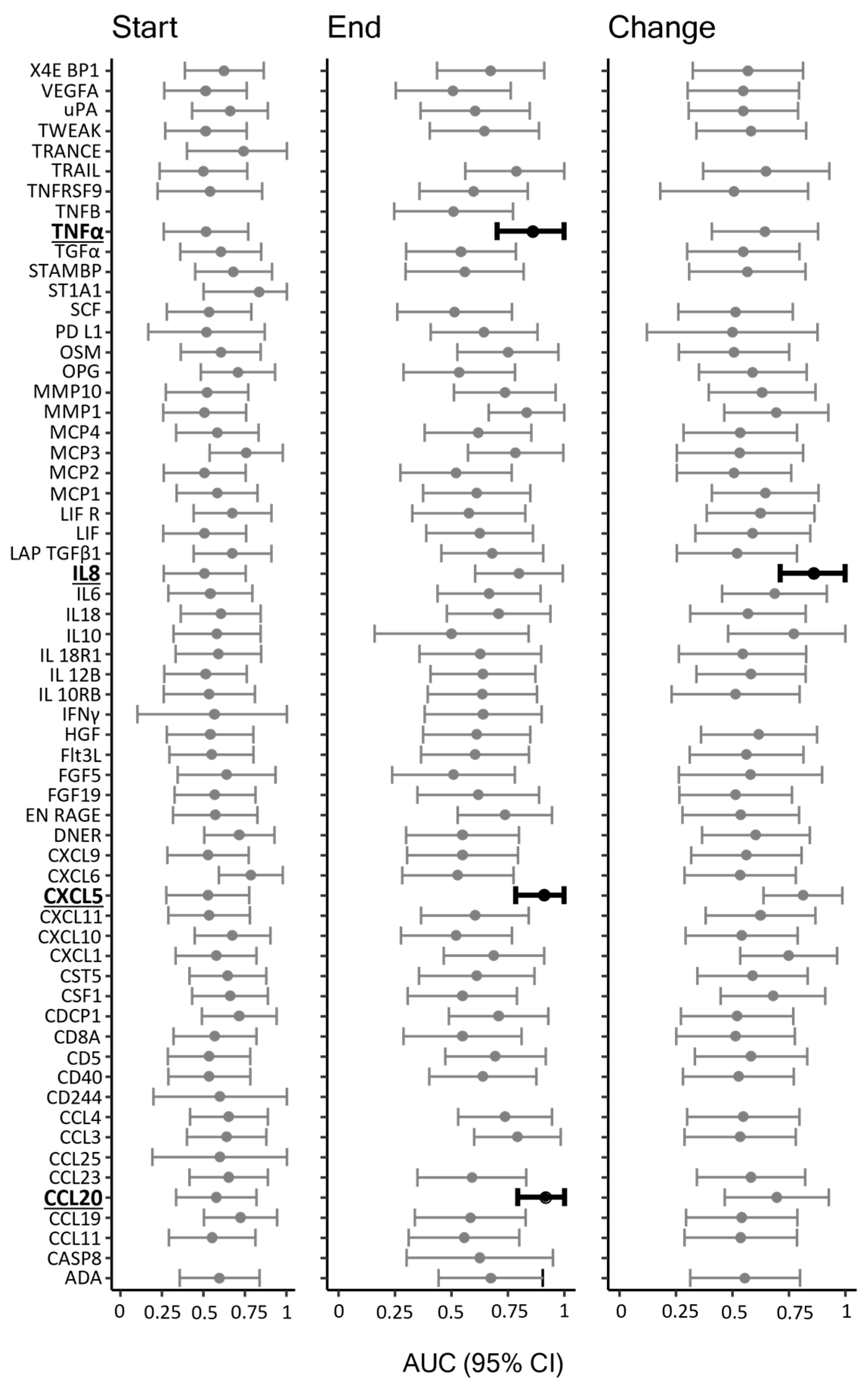
3.1. Shunt Dependency
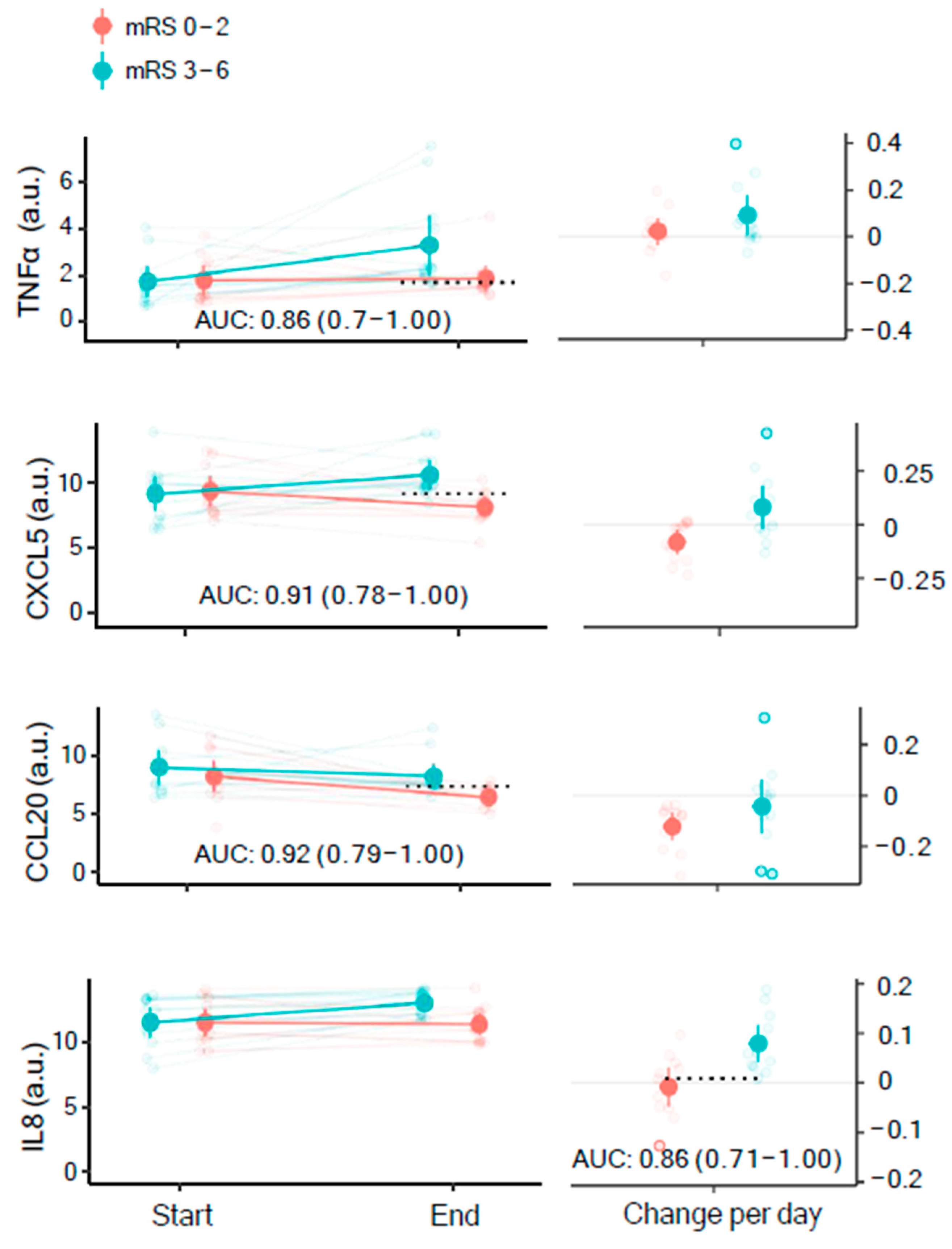
3.2. Functional Outcome
4. Discussion
4.1. Hydrocephalus and Shunt Dependency
4.2. Functional Outcome
4.3. Neuroinflammation and Therapeutic Targets
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Olsen, M.H.; Orre, M.; Leisner, A.C.W.; Rasmussen, R.; Bache, S.; Welling, K.; Eskesen, V.; Møller, K. Delayed cerebral ischaemia in patients with aneurysmal subarachnoid haemorrhage: Functional outcome and long-term mortality. Acta Anaesthesiol. Scand. 2019, 63, 1191–1199. [Google Scholar] [CrossRef] [PubMed]
- Claassen, J.; Park, S. Spontaneous subarachnoid haemorrhage. Lancet 2022, 400, 846–862. [Google Scholar] [CrossRef] [PubMed]
- Suarez, J.I.; Tarr, R.W.; Selman, W.R. Aneurysmal subarachnoid hemorrhage. N. Engl. J. Med. 2006, 354, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Cahill, J.; Cahill, W.J.; Calvert, J.W.; Calvert, J.H.; Zhang, J.H. Mechanisms of early brain injury after subarachnoid hemorrhage. J. Cereb. Blood Flow Metab. 2006, 26, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- Grote, E.; Hassler, W. The critical first minutes after subarachnoid hemorrhage. Neurosurgery 1988, 22, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Papaioannou, V.; Czosnyka, Z.; Czosnyka, M. Hydrocephalus and the neuro-intensivist: CSF hydrodynamics at the bedside. Intensive Care Med. Exp. 2022, 10, 20. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Luo, J.; Reis, C.; Manaenko, A.; Zhang, J. Hydrocephalus after Subarachnoid Hemorrhage: Pathophysiology, Diagnosis, and Treatment. Biomed. Res. Int. Hindawi 2017, 2017, 8584753. [Google Scholar] [CrossRef]
- Lolansen, S.D.; Rostgaard, N.; Barbuskaite, D.; Capion, T.; Olsen, M.H.; Norager, N.H.; Vilhardt, F.; Andreassen, S.N.; Toft-Bertelsen, T.L.; Ye, F.; et al. Posthemorrhagic hydrocephalus associates with elevated inflammation and CSF hypersecretion via activation of choroidal transporters. Fluids Barriers CNS 2022, 19, 62. [Google Scholar] [CrossRef]
- Capion, T.; Lilja-Cyron, A.; Juhler, M.; Mathiesen, T.I.; Wetterslev, J. Prompt closure versus gradual weaning of external ventricular drainage for hydrocephalus in adult patients with aneurysmal subarachnoid haemorrhage: A systematic review. BMJ Open 2020, 10, e040722. [Google Scholar] [CrossRef]
- Capion, T.; Lilja-Cyron, A.; Bartek, J.; Forsse, A.; Logallo, N.; Juhler, M.; Mathiesen, T. Discontinuation of External Ventricular Drainage in Patients with Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage—A Scandinavian Multi-institutional Survey. Acta Neurochir. 2020, 162, 1363–1370. [Google Scholar] [CrossRef]
- Zhu, Y.; Wen, L.; You, W.; Wang, Y.; Wang, H.; Li, G.; Chen, Z.; Yang, X. Influence of Ward Environments on External Ventricular Drain Infections: A Retrospective Risk Factor Analysis. Surg. Infect. 2021, 22, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Champey, J.; Mourey, C.; Francony, G.; Pavese, P.; Gay, E.; Gergele, L.; Manet, R.; Velly, L.; Bruder, N.; Payen, J.-F. Strategies to reduce external ventricular drain–related infections: A multicenter retrospective study. J. Neurosurg. 2019, 130, 2034–2039. [Google Scholar] [CrossRef] [PubMed]
- Walek, K.W.; Leary, O.P.; Sastry, R.; Asaad, W.F.; Walsh, J.M.; Horoho, J.; Mermel, L.A. Risk factors and outcomes associated with external ventricular drain infections. Infect. Control. Hosp. Epidemiol. 2022, 43, 1859–1866. [Google Scholar] [CrossRef] [PubMed]
- Camacho, E.F.; Boszczowski, I.; Basso, M.; Jeng, B.C.P.; Freire, M.P.; Guimarães, T.; Teixeira, M.J.; Costa, S.F. Infection rate and risk factors associated with infections related to external ventricular drain. Infection 2011, 39, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Palasz, J.; D’Antona, L.; Farrell, S.; Elborady, M.A.; Watkins, L.D.; Toma, A.K. External ventricular drain management in subarachnoid haemorrhage: A systematic review and meta-analysis. Neurosurg. Rev. 2021, 45, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.S.; Chung, D.Y.; Wolcott, Z.; Sheriff, F.; Khawaja, A.M.; Lee, H.; Guanci, M.M.; Leslie-Mazwi, T.M.; Kimberly, W.T.; Patel, A.B.; et al. Intermittent CSF drainage and rapid EVD weaning approach after subarachnoid hemorrhage: Association with fewer VP shunts and shorter length of stay. J. Neurosurg. 2019, 132, 1583–1588. [Google Scholar] [CrossRef]
- Yang, Y.-C.; Yin, C.-H.; Chen, K.-T.; Lin, P.-C.; Lee, C.-C.; Liao, W.-C.; Chen, J.-S. Prognostic Nomogram of Predictors for Shunt-Dependent Hydrocephalus in Patients with Aneurysmal Subarachnoid Hemorrhage Receiving External Ventricular Drain Insertion: A Single-Center Experience and Narrative Review. World Neurosurg. 2021, 150, e12–e22. [Google Scholar] [CrossRef]
- Dorai, Z.; Hynan, L.S.; Kopitnik, T.A.; Samson, D. Factors Related to Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage. Neurosurgery 2003, 52, 763–771; discussion 769–771. [Google Scholar] [CrossRef]
- Brisman, J.L.; Berenstein, A. Factors Related to Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage. Neurosurgery 2004, 54, 1031. [Google Scholar] [CrossRef]
- Chan, M.; Alaraj, A.; Calderon, M.; Herrera, S.R.; Gao, W.; Ruland, S.; Roitberg, B.Z. Prediction of ventriculoperitoneal shunt dependency in patients with aneurysmal subarachnoid hemorrhage. J. Neurosurg. 2009, 110, 44–49. [Google Scholar] [CrossRef]
- Rincon, F.; Gordon, E.; Starke, R.M.; Buitrago, M.M.; Fernandez, A.; Schmidt, J.M.; Claassen, J.; Wartenberg, K.E.; A Frontera, J.; Seder, D.; et al. Predictors of long-term shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage. Clinical article. J Neurosurg. 2010, 113, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Brandner, S.; Xu, Y.; Schmidt, C.; Emtmann, I.; Buchfelder, M.; Kleindienst, A. Shunt-dependent hydrocephalus following subarachnoid hemorrhage correlates with increased S100B levels in cerebrospinal fluid and serum. Acta Neurochir. Suppl. 2012, 114, 217–220. [Google Scholar] [PubMed]
- Lai, L.; Morgan, M.K. Predictors of in-hospital shunt-dependent hydrocephalus following rupture of cerebral aneurysms. J. Clin. Neurosci. 2013, 20, 1134–1138. [Google Scholar] [CrossRef]
- Chaudhry, S.R.; Hafez, A.; Jahromi, B.R.; Kinfe, T.M.; Lamprecht, A.; Niemelä, M.; Muhammad, S. Role of Damage Associated Molecular Pattern Molecules (DAMPs) in Aneurysmal Subarachnoid Hemorrhage (aSAH). Int. J. Mol. Sci. 2018, 19, 2035. [Google Scholar] [CrossRef] [PubMed]
- Karimy, J.K.; Reeves, B.C.; Damisah, E.; Duy, P.Q.; Antwi, P.; David, W.; Wang, K.; Schiff, S.J.; Limbrick, D.D., Jr.; Alper, S.L.; et al. Inflammation in acquired hydrocephalus: Pathogenic mechanisms and therapeutic targets. Nat. Rev. Neurol. 2020, 16, 285–296. [Google Scholar] [CrossRef]
- Lolansen, S.D.; Rostgaard, N.; Oernbo, E.K.; Juhler, M.; Simonsen, A.H.; MacAulay, N. Inflammatory Markers in Cerebrospinal Fluid from Patients with Hydrocephalus: A Systematic Literature Review. Dis. Markers 2021, 2021, 8834822. [Google Scholar] [CrossRef]
- Jabbarli, R.; Pierscianek, D.; Oppong, M.D.; Sato, T.; Dammann, P.; Wrede, K.H.; Kaier, K.; Köhrmann, M.; Forsting, M.; Kleinschnitz, C.; et al. Laboratory biomarkers of delayed cerebral ischemia after subarachnoid hemorrhage: A systematic review. Neurosurg. Rev. 2020, 43, 825–833. [Google Scholar] [CrossRef]
- Toft-Bertelsen, T.L.; Barbuskaite, D.; Heerfordt, E.K.; Lolansen, S.D.; Andreassen, S.N.; Rostgaard, N.; Olsen, M.H.; Norager, N.H.; Capion, T.; Rath, M.F.; et al. Lysophosphatidic acid as a CSF lipid in posthemorrhagic hydrocephalus that drives CSF accumulation via TRPV4-induced hyperactivation of NKCC1. Fluids Barriers CNS 2022, 19, 69. [Google Scholar] [CrossRef]
- del Campo, M.; Mollenhauer, B.; Bertolotto, A.; Engelborghs, S.; Hampel, H.; Simonsen, A.H.; Kapaki, E.; Kruse, N.; Le Bastard, N.; Lehmann, S.; et al. Recommendations to standardize preanalytical confounding factors in Alzheimer’s and Parkinson’s disease cerebrospinal fluid biomarkers: An update. Biomark. Med. 2012, 6, 419–430. [Google Scholar] [CrossRef]
- Assarsson, E.; Lundberg, M.; Holmquist, G.; Björkesten, J.; Thorsen, S.B.; Ekman, D.; Eriksson, A.; Dickens, E.R.; Ohlsson, S.; Edfeldt, G.; et al. Homogenous 96-Plex PEA Immunoassay Exhibiting High Sensitivity, Specificity, and Excellent Scalability. PLoS ONE 2014, 9, e95192. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Qin, L.; Wang, D.; Gong, J.; Pan, J.; Zhu, Y.; Sun, T.; Xu, K.; Zhan, R. Comparing the Risk of Shunt-Dependent Hydrocephalus in Patients with Ruptured Intracranial Aneurysms Treated by Endovascular Coiling or Surgical Clipping: An Updated Meta-Analysis. World Neurosurg. 2019, 121, e731–e738. [Google Scholar] [CrossRef] [PubMed]
- Lenski, M.; Biczok, A.; Huge, V.; Forbrig, R.; Briegel, J.; Tonn, J.-C.; Thon, N. Role of Cerebrospinal Fluid Markers for Predicting Shunt-Dependent Hydrocephalus in Patients with Subarachnoid Hemorrhage and External Ventricular Drain Placement. World Neurosurg. 2019, 121, e535–e542. [Google Scholar] [CrossRef] [PubMed]
- Lenski, M.; Huge, V.; Briegel, J.; Tonn, J.-C.; Schichor, C.; Thon, N. Interleukin 6 in the Cerebrospinal Fluid as a Biomarker for Onset of Vasospasm and Ventriculitis After Severe Subarachnoid Hemorrhage. World Neurosurg. 2017, 99, 132–139. [Google Scholar] [CrossRef]
- Chaudhry, S.R.; Stoffel-Wagner, B.; Kinfe, T.M.; Güresir, E.; Vatter, H.; Dietrich, D.; Lamprecht, A.; Muhammad, S. Elevated systemic IL-6 levels in patients with aneurysmal subarachnoid hemorrhage is an unspecific marker for post-SAH complications. Int. J. Mol. Sci. 2017, 18, 2580. [Google Scholar] [CrossRef]
- Kaestner, S.; Dimitriou, I. TGF Beta1 and TGF Beta2 and Their Role in Posthemorrhagic Hydrocephalus Following SAH and IVH. J. Neurol. Surg. Part A Central Eur. Neurosurg. 2013, 74, 279–284. [Google Scholar] [CrossRef]
- Lv, S.Y.; Wu, Q.; Liu, J.P.; Shao, J.; Wen, L.; Xue, J.; Zhang, X.S.; Zhang, Q.R.; Zhang, X. Levels of Interleukin-1β, Interleukin-18, and Tumor Necrosis Factor-α in Cerebrospinal Fluid of Aneurysmal Subarachnoid Hemorrhage Patients May Be Predictors of Early Brain Injury and Clinical Prognosis. World Neurosurg. 2018, 111, e362–e373. [Google Scholar] [CrossRef]
- Lucke-Wold, B.; Dodd, W.; Motwani, K.; Hosaka, K.; Laurent, D.; Martinez, M.; Dugan, V.; Chalouhi, N.; Lucke-Wold, N.; Barpujari, A.; et al. Investigation and modulation of interleukin-6 following subarachnoid hemorrhage: Targeting inflammatory activation for cerebral vasospasm. J. Neuroinflamm. 2022, 19, 228. [Google Scholar] [CrossRef]
- Wostrack, M.; Reeb, T.; Martin, J.; Kehl, V.; Shiban, E.; Preuss, A.; Ringel, F.; Meyer, B.; Ryang, Y.-M. Shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: The role of intrathecal interleukin-6. Neurocrit. Care 2014, 21, 78–84. [Google Scholar] [CrossRef]
- Karimy, J.K.; Zhang, J.; Kurland, D.B.; Theriault, B.C.; Duran, D.; Stokum, J.A.; Furey, C.G.; Zhou, X.; Mansuri, M.S.; Montejo, J.; et al. Inflammation-dependent cerebrospinal fluid hypersecretion by the choroid plexus epithelium in posthemorrhagic hydrocephalus. Nat. Med. 2017, 23, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Mahlamäki, K.; Rautalin, I.; Korja, M. Case Fatality Rates of Subarachnoid Hemorrhage Are Decreasing with Substantial between-Country Variation: A Systematic Review of Population-Based Studies between 1980 and 2020. Neuroepidemiology 2022, 56, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Dayyani, M.; Sadeghirad, B.; Grotta, J.C.; Zabihyan, S.; Ahmadvand, S.; Wang, Y.; Guyatt, G.H.; Amin-Hanjani, S. Prophylactic Therapies for Morbidity and Mortality After Aneurysmal Subarachnoid Hemorrhage: A Systematic Review and Network Meta-Analysis of Randomized Trials. Stroke 2022, 53, 1993–2005. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Lan, F.; Zhang, Y. Associations between C-reactive protein and white blood cell count, occurrence of delayed cerebral ischemia and poor outcome following aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. Acta Neurol. Belg. 2021, 121, 1311–1324. [Google Scholar] [CrossRef] [PubMed]
- Oka, F.; Chung, D.Y.; Suzuki, M.; Ayata, C. Delayed Cerebral Ischemia After Subarachnoid Hemorrhage: Experimental-Clinical Disconnect and the Unmet Need. Neurocrit. Care 2020, 32, 238–251. [Google Scholar] [CrossRef] [PubMed]
- de Winkel, J.; Cras, T.Y.; Dammers, R.; van Doormaal, P.-J.; van der Jagt, M.; Dippel, D.W.J.; Roozenbeek, B. Early predictors of functional outcome in poor-grade aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. BMC Neurol. 2022, 22, 239. [Google Scholar] [CrossRef]
- Rass, V.; Gaasch, M.; Kofler, M.; Schiefecker, A.J.; Ianosi, B.-A.; Rhomberg, P.; Beer, R.; Pfausler, B.; Gizewski, E.R.; Thomé, C.; et al. Systemic Inflammatory Response Syndrome as Predictor of Poor Outcome in Nontraumatic Subarachnoid Hemorrhage Patients. Crit. Care Med. 2018, 46, e1152–e1159. [Google Scholar] [CrossRef]
- Yoshimoto, Y.; Tanaka, Y.; Hoya, K. Acute systemic inflammatory response syndrome in subarachnoid hemorrhage. Stroke 2001, 32, 1989–1993. [Google Scholar] [CrossRef]
- Yu, T.; Wang, Z. Use of A Systemic Inflammatory Response Index to Predict Non-Traumatic Non-Aneurysmal Subarachnoid Hemorrhage Patient Outcomes. J. Stroke Cerebrovasc. Dis. 2022, 31, 106863. [Google Scholar] [CrossRef]
- Holste, K.G.; Xia, F.; Ye, F.; Keep, R.F.; Xi, G. Mechanisms of neuroinflammation in hydrocephalus after intraventricular hemorrhage: A review. Fluids Barriers CNS 2022, 19, 28. [Google Scholar] [CrossRef]
- Sokół, B.; Woźniak, A.; Jankowski, R.; Jurga, S.; Wąsik, N.; Shahid, H.; Grześkowiak, B. HMGB1 Level in Cerebrospinal Fluid as a Marker of Treatment Outcome in Patients with Acute Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage. J. Stroke Cerebrovasc. Dis. 2015, 24, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Massicotte, E.M.; Del Bigio, M.R. Human arachnoid villi response to subarachnoid hemorrhage: Possible relationship to chronic hydrocephalus. J. Neurosurg. 1999, 91, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Wagshul, M.E.; Eide, P.K.; Madsen, J.R. The pulsating brain: A review of experimental and clinical studies of intracranial pulsatility. Fluids Barriers CNS 2011, 8, 5. [Google Scholar] [CrossRef] [PubMed]
- Robert, S.M.; Reeves, B.C.; Kiziltug, E.; Duy, P.Q.; Karimy, J.K.; Mansuri, M.S.; Marlier, A.; Allington, G.; Greenberg, A.B.; DeSpenza, T.; et al. The choroid plexus links innate immunity to CSF dysregulation in hydrocephalus. Cell 2023, 186, 764–785.e21. [Google Scholar] [CrossRef]
- Keep, R.F.; Hua, Y.; Xi, G. Intracerebral haemorrhage: Mechanisms of injury and therapeutic targets. Lancet Neurol. 2012, 11, 720–731. [Google Scholar] [CrossRef]
- Ramesh, G.; MacLean, A.G.; Philipp, M.T. Cytokines and chemokines at the crossroads of neuroinflammation, neurodegeneration, and neuropathic pain. Mediators Inflamm. 2013, 2013, 480739. [Google Scholar] [CrossRef]
- Liao, F.; Li, G.; Yuan, W.; Chen, Y.; Zuo, Y.; Rashid, K.; Zhang, J.H.; Feng, H.; Liu, F. LSKL peptide alleviates subarachnoid fibrosis and hydrocephalus by inhibiting TSP1-mediated TGF-β1 signaling activity following subarachnoid hemorrhage in rats. Exp. Ther. Med. 2016, 12, 2537–2543. [Google Scholar] [CrossRef]
- Kuo, L.-T.; Huang, A. The Pathogenesis of Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage. Int. J. Mol. Sci. 2021, 22, 5050. [Google Scholar] [CrossRef]
- Lin, J.; Liu, H.; Jiang, J.; Jia, C.; Zhang, B.; Gao, X. Clinical evidence of efficacy of simvastatin for aneurysmal subarachnoid hemorrhage. J. Int. Med. Res. 2017, 45, 2128–2138. [Google Scholar] [CrossRef]
- Liu, J.; Chen, Q. Effect of statins treatment for patients with aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis of observational studies and randomized controlled trials. Int. J. Clin. Exp. Med. 2015, 8, 7198–7208. [Google Scholar]
- Manno, E.M.; Gress, D.R.; Ogilvy, C.S.; Stone, C.M.; Zervas, N.T. The safety and efficacy of cyclosporine A in the prevention of vasospasm in patients with Fisher grade 3 subarachnoid hemorrhages: A pilot study. Neurosurgery 1997, 40, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Habibie, H.; Adhyatmika, A.; Schaafsma, D.; Melgert, B.N. The role of osteoprotegerin (OPG) in fibrosis: Its potential as a biomarker and/or biological target for the treatment of fibrotic diseases. Pharmacol Ther. 2021, 228, 107941. [Google Scholar] [CrossRef]
- Howe, M.D.; Furr, J.W.; Munshi, Y.; Roy-O’Reilly, M.A.; Maniskas, M.E.; Koellhoffer, E.C.; d’Aigle, J.; Sansing, L.; McCullough, L.; Urayama, A. Transforming growth factor-β promotes basement membrane fibrosis, alters perivascular cerebrospinal fluid distribution, and worsens neurological recovery in the aged brain after stroke. GeroScience 2019, 41, 543–559. [Google Scholar] [CrossRef] [PubMed]
- Justet, A.; Ghanem, M.; Boghanim, T.; Hachem, M.; Vasarmidi, E.; Jaillet, M.; Vadel, A.; Joannes, A.; Mordant, P.; Bonniaud, P.; et al. FGF19 Is Downregulated in Idiopathic Pulmonary Fibrosis and Inhibits Lung Fibrosis in Mice. Am. J. Respir. Cell Mol. Biol. 2022, 67, 173–187. [Google Scholar] [CrossRef] [PubMed]
- Kazakov, A.; Meier, T.; Werner, C.; Hall, R.; Klemmer, B.; Körbel, C.; Lammert, F.; Maack, C.; Böhm, M.; Laufs, U. C-kit + resident cardiac stem cells improve left ventricular fibrosis in pressure overload. Stem Cell Res. 2015, 15, 700–711. [Google Scholar] [CrossRef]
- Dyhrfort, P.; Wettervik, T.S.; Clausen, F.; Enblad, P.; Hillered, L.; Lewén, A. A Dedicated 21-Plex Proximity Extension Assay Panel for High-Sensitivity Protein Biomarker Detection Using Microdialysis in Severe Traumatic Brain Injury: The Next Step in Precision Medicine? Neurotrauma Rep. 2023, 4, 25–40. [Google Scholar] [CrossRef]

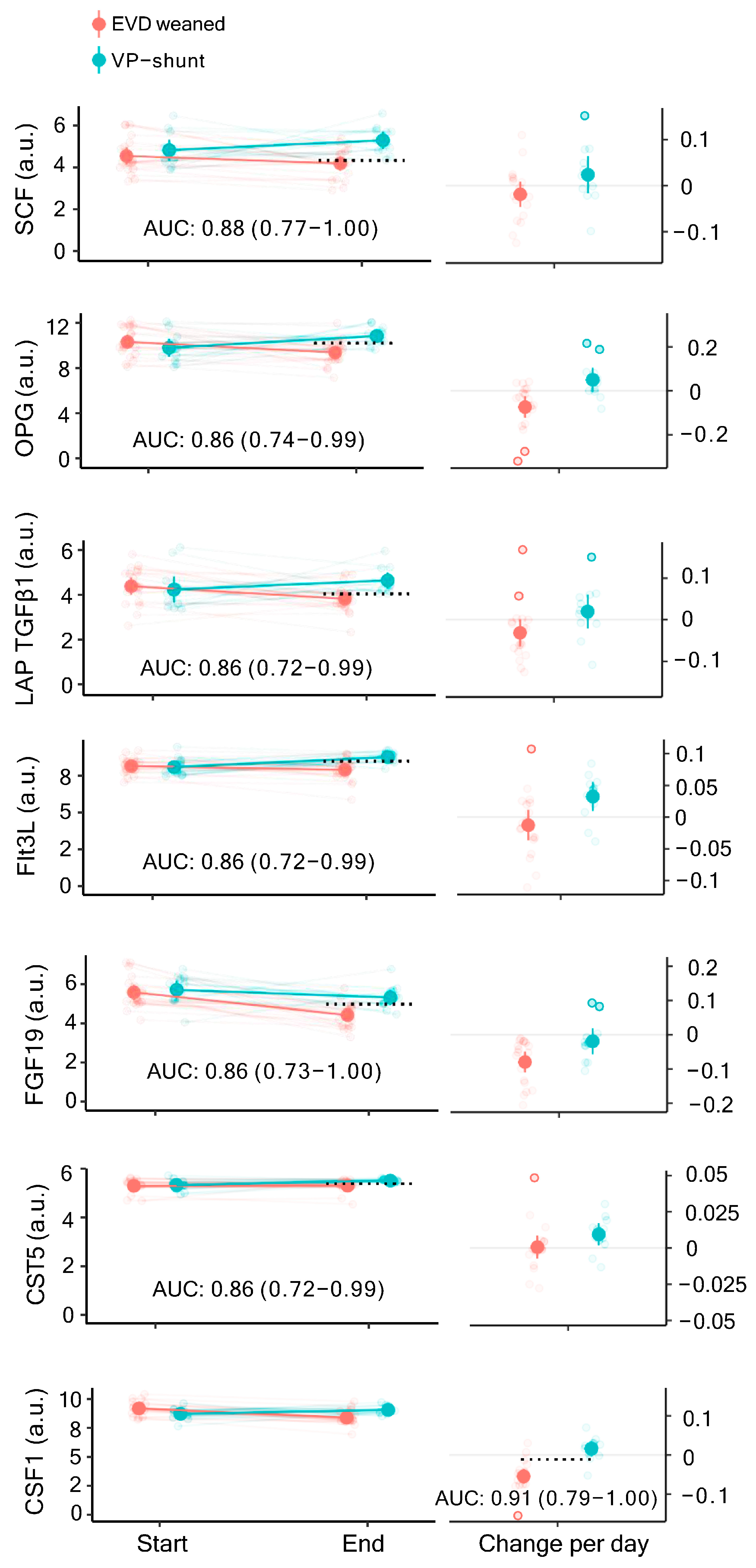
| Name | Time | EVD Weaned Mean (SD) [n] | VP-Shunt Mean (SD) [n] | AUC (95% CI) | Cut-Off | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| SCF | End | 4.18 (0.74) [19] | 5.29 (0.65) [12] | 0.88 (0.77–1.00) | 4.33 | 1.00 | 0.63 |
| OPG | End | 9.37 (1.13) [19] | 10.83 (0.80) [12] | 0.86 (0.74–0.99) | 10.20 | 0.83 | 0.79 |
| LAP TGFβ1 | End | 3.83 (0.63) [19] | 4.65 (0.57) [12] | 0.86 (0.72–0.99) | 4.05 | 1.00 | 0.68 |
| Flt3L | End | 7.90 (0.76) [19] | 8.76 (0.37) [12] | 0.86 (0.72–0.99) | 8.49 | 0.83 | 0.79 |
| FGF19 | End | 4.42 (0.63) [19] | 5.31 (0.61) [12] | 0.86 (0.73–1.00) | 4.97 | 0.83 | 0.89 |
| CST5 | End | 5.29 (0.25) [19] | 5.51 (0.06) [12] | 0.86 (0.72–0.99) | 5.38 | 1.00 | 0.68 |
| CSF1 | Daily Change | 0.05 (0.04) [19] | −0.02 (0.03) [12] | 0.91 (0.79–1.00) | 0.01 | 0.92 | 0.89 |
| Name | Time | mRS 0–2 - Mean (SD) [n] | mRS 3–6 - Mean (SD) [n] | AUC (95% CI) | Cut-Off | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| TNFα | End | 1.84 (0.88) [12] | 3.26 (2.01) [12] | 0.86 (0.7–1.00) | 1.66 | 1.00 | 0.67 |
| CXCL5 | End | 8.08 (1.23) [12] | 10.56 (1.75) [12] | 0.91 (0.78–1.00) | 9.11 | 0.92 | 0.83 |
| CCL20 | End | 6.33 (0.85) [11] | 8.12 (1.69) [12] | 0.92 (0.79–1.00) | 7.26 | 0.92 | 0.91 |
| IL8 | Daily Change | 0.01 (0.06) [12] | −0.08 (0.06) [12] | 0.86 (0.71–1.00) | −0.01 | 1.00 | 0.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rostgaard, N.; Olsen, M.H.; Capion, T.; MacAulay, N.; Juhler, M. Inflammatory Markers as Predictors of Shunt Dependency and Functional Outcome in Patients with Aneurysmal Subarachnoid Hemorrhage. Biomedicines 2023, 11, 997. https://doi.org/10.3390/biomedicines11040997
Rostgaard N, Olsen MH, Capion T, MacAulay N, Juhler M. Inflammatory Markers as Predictors of Shunt Dependency and Functional Outcome in Patients with Aneurysmal Subarachnoid Hemorrhage. Biomedicines. 2023; 11(4):997. https://doi.org/10.3390/biomedicines11040997
Chicago/Turabian StyleRostgaard, Nina, Markus Harboe Olsen, Tenna Capion, Nanna MacAulay, and Marianne Juhler. 2023. "Inflammatory Markers as Predictors of Shunt Dependency and Functional Outcome in Patients with Aneurysmal Subarachnoid Hemorrhage" Biomedicines 11, no. 4: 997. https://doi.org/10.3390/biomedicines11040997
APA StyleRostgaard, N., Olsen, M. H., Capion, T., MacAulay, N., & Juhler, M. (2023). Inflammatory Markers as Predictors of Shunt Dependency and Functional Outcome in Patients with Aneurysmal Subarachnoid Hemorrhage. Biomedicines, 11(4), 997. https://doi.org/10.3390/biomedicines11040997







