The Role of LINC01564, RAMS11, CBX4 and TOP2A in Hepatocellular Carcinoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection of Samples and Laboratory Tests
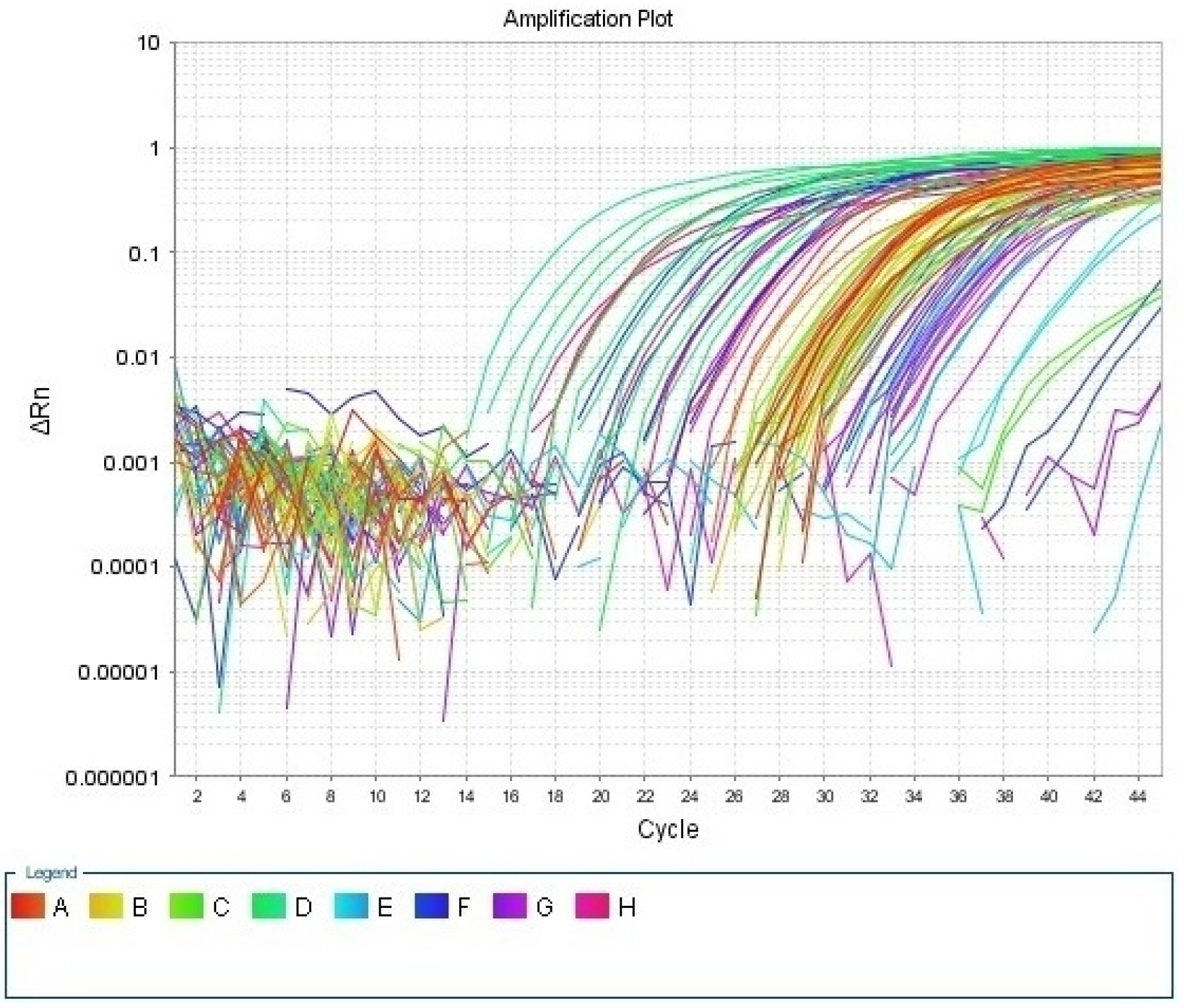
2.2. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR) for LncRNAs (RAMS11, Linc01564), CBX4, and TOP2A Genes as a Target and GAPDH Gene as an Endogenous Reference Gene
2.3. Statistical Analysis of the Data
3. Results
3.1. Clinical and Biochemical Characteristics of the Studied Groups
3.2. The Relative Expression Level of lncRNA in Studied Groups
3.3. Regarding Correlations between the Relative Expression Level of lncRNA with Clinical and Biochemical Parameters among Case Group Showed That
3.4. Linear Regression Analysis in the HCC Group Revealed That
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Torre, L.A.; Siegel, R.L.; Ward, E.M. Jemal A Global cancer incidence and mortality rates and trends—An update. Cancer Epidemiol. Prev. Biomark. 2016, 25, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Holah, N.S.; El-Azab, D.S.; Aiad, H.A.; Sweed, D.M. Hepatocellular carcinoma in Egypt: Epidemiological and histopathological properties. Menoufia Med. J. 2015, 28, 718. [Google Scholar]
- Wang, B.; Tang, J.; Liao, D.; Wang, G.; Zhang, M.; Sang, Y.; Cao, J.; Wu, A.; Zhang, R.; Li, S.; et al. Chromobox homolog 4 is correlated with prognosis and tumor cell growth in hepatocellular carcinoma. Ann. Surg. Oncol. 2013, 20, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.J.; Yang, H.I.; Su, J.U.; Jen, C.L.; You, S.L.; Lu, S.N.; Huang, G.T.; Iloeje, U.H. Reveal-HBV Study Group. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA 2006, 295, 65–73. [Google Scholar] [CrossRef]
- Yang, S.F.; Chang, C.W.; Wei, R.J.; Shiue, Y.L.; Wang, S.N.; Yeh, Y.T. Involvement of DNA damage response pathways in hepatocellular carcinoma. BioMed Res. Int. 2014, 2014, 14–18. [Google Scholar] [CrossRef]
- DiStefano, J.K. Long noncoding RNAs in the initiation, progression, and metastasis of hepatocellular carcinoma. Noncoding RNA Res. 2017, 2, 129–136. [Google Scholar] [CrossRef]
- Dhanoa, J.K.; Sethi, R.S.; Verma, R.; Arora, J.S.; Mukhopadhyay, C.S. Long non-coding RNA: Its evolutionary relics and biological implications in mammals: A review. J. Anim. Sci. Technol. 2018, 60, 25. [Google Scholar] [CrossRef]
- Prensner, J.R.; Chinnaiyan, A.M. The emergence of lncRNAs in cancer biology. Cancer Discov. 2011, 1, 391–407. [Google Scholar] [CrossRef]
- Iyer, M.K.; Niknafs, Y.S.; Malik, R.; Singhal, U.; Sahu, A.; Hosono, Y.; Poliakov, A. The landscape of long noncoding RNAs in the human transcriptome. Nat. Genet. 2015, 47, 199–208. [Google Scholar] [CrossRef]
- Wilusz, J.E.; Sunwoo, H.; Spector, D.L. Long noncoding RNAs: Functional surprises from the RNA world. Genes Dev. 2009, 23, 1494–1504. [Google Scholar] [CrossRef]
- Sasaki, R.; Kanda, T.; Yokosuka, O.; Kato, N.; Matsuoka, S.; Moriyama, M. Exosomes and Hepatocellular Carcinoma: From Bench to Bedside. Int. J. Mol. Sci. 2019, 20, 1406. [Google Scholar] [CrossRef] [PubMed]
- De Toro, J.; Herschlik, L.; Waldner, C.; Mongini, C. Emerging roles of exosomes in normal and pathological conditions: New insights for diagnosis and therapeutic applications. Front. Immunol. 2015, 6, 203. [Google Scholar] [CrossRef] [PubMed]
- Philley, J.V.; Kannan, A.; Griffith, D.E.; Devine, M.S.; Benwill, J.L.; Wallace, R.J.; Brown-Elliott, B.A.; Thakkar, F.; Taskar, V.; Fox, J.G.; et al. Exosome secretome and mediated signaling in breast cancer patients with nontuberculous mycobacterial disease. Oncotarget 2017, 8, 18070–18081. [Google Scholar] [CrossRef] [PubMed]
- Riancho, J.; Vázquez-Higuera, J.L.; Pozueta, A.; Lage, C.; Kazimierczak, M.; Bravo, M.; Calero, M.; Gonalezález, A.; Rodríguez, E.; Lleó, A.; et al. Micro RNA Profile in Patients with Alzheimer’s Disease: Analysis of miR-9-5 pand miR-598 in Raw and Exosome Enriched Cerebrospinal Fluid Samples. J. Alzheimers 2017, 57, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hu, Y.W.; Zheng, L.; Wang, Q. Characteristics and Roles of Exosomes in Cardiovascular Disease. DNA Cell Biol. 2017, 36, 202–211. [Google Scholar] [CrossRef]
- Song, J.; Kim, D.; Han, J.; Kim, Y.; Lee, M.; Jin, E.J. PBMC and exosome-derived Hotair is a critical regulator and potent marker for rheumatoid arthritis. Clin. Exp. Med. 2015, 15, 121–126. [Google Scholar] [CrossRef]
- Su, H.; Yang, J.R.; Xu, T.; Huang, J.; Xu, L.; Yuan, Y.; Zhuang, S.M. MicroRNA-101, down-regulated in hepatocellular carcinoma, promotes apoptosis and suppresses tumorigenicity. Cancer Res. 2009, 69, 1135–1142. [Google Scholar] [CrossRef]
- Fu, X.; Liu, M.; Qu, S.; Ma, J.; Zhang, Y.; Shi, T.; Wen, H.; Yang, Y.; Wang, S.; Wang, J.; et al. Exosomal microRNA-32-5p induces multidrug resistance in hepatocellular carcinoma via the PI3K/Akt pathway. J. Exp. Clin. Cancer Res. 2018, 37, 52. [Google Scholar] [CrossRef]
- Lee, H.Y.; Chen, C.K.; Ho, C.M.; Lee, S.S.; Chang, C.Y.; Chen, K.J.; Jou, Y.S. EIF3C-enhanced exosome secretion promotes angiogenesis and tumorigenesis of human hepatocellular carcinoma. Oncotarget 2018, 9, 13193–13205. [Google Scholar] [CrossRef]
- Rao, Q.; Zuo, B.; Lu, Z.; Gao, X.; You, A.; Wu, C.; Du, Z.; Yin, H. Tumor-derived exosomes elicit tumor suppression in murine hepatocellular carcinoma models and humans in vitro. Hepatology 2016, 64, 456–472. [Google Scholar] [CrossRef]
- Takahashi, K.; Yan, I.K.; Kogure, T.; Haga, H.; Patel, T. Extracellular vesicle-mediated transfer of long non-coding RNA ROR modulates chemosensitivity in human hepatocellular cancer. FEBS Open Bio 2014, 4, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Yan, I.K.; Wood, J.; Haga, H.; Patel, T. Involvement of Extracellular Vesicle Long Noncoding RNA (linc-VLDLR) in Tumor Cell Responses to Chemotherapy. Mol. Cancer Res. 2014, 12, 1377–1387. [Google Scholar] [CrossRef]
- Li, B.; Mao, R.; Liu, C.; Zhang, W.; Tang, Y.; Guo, Z. LncRNA FAL1 promotes cell proliferation and migration by acting as a CeRNA of miR-1236 in hepatocellular carcinoma cells. Life Sci. 2018, 197, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Yang, X.; Qi, Q.; Gao, Y.; Wei, Q.; Han, S. lncRNA-HEIH in serum and exosomes as a potential biomarker in the HCV-related hepatocellular carcinoma. Cancer Biomark. 2018, 21, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Chen, Y.; Dong, X.; Wang, X. Serum Exosomal Long Noncoding RNAs ENSG00000258332.1 and LINC00635 for the Diagnosis and Prognosis of Hepatocellular Carcinoma. Cancer Epidemiol. Biomark. Prev. 2018, 27, 710–716. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Hou, F.; Tang, L.; Xiao, K.; Yang, T.; Wang, Z.; Liu, G. The interaction between long non-coding RNA LINC01564 and POU2F1 promotes the proliferation and metastasis of gastric cancer. J. Transl. Med. 2022, 20, 220. [Google Scholar] [CrossRef] [PubMed]
- Silva-Fisher, J.M.; Dang, H.X.; White, N.M.; Strand, M.S.; Krasnick, B.A.; Rozycki, E.B.; Jeffers, G.G.L.; Grossman, J.G.; Highkin, M.K.; Tang, C.; et al. Long non-coding RNA RAMS11 promotes metastatic colorectal cancer progression. Nat. Commun. 2020, 11, 2156. [Google Scholar] [CrossRef]
- Zeng, J.S.; Zhang, Z.D.; Pei, L.; Bai, Z.Z.; Yang, Y.; Yang, H.; Tian, Q.H. CBX4 exhibits oncogenic activities in breast cancer via Notch1 signaling. Int. J. Biochem. Cell Biol. 2018, 95, 1–8. [Google Scholar] [CrossRef]
- Antoniou-Kourounioti, M.; Mimmack, M.L.; Porter, A.C.; Farr, C.J. The impact of the C-terminal region on the interaction of topoisomerase ii alpha with mitotic chromatin. Int. J. Mol. Sci. 2019, 20, 1238. [Google Scholar] [CrossRef]
- Choi, I.Y.; Chung, I.K.; Muller, M.T. Eukaryotic topoisomerase II cleavage is independent of duplex DNA conformation. Biochim. Biophys. Acta (BBA)-Gene Struct. Expr. 1995, 1264, 209–214. [Google Scholar] [CrossRef]
- Janevska, D.; Chaloska-Ivanova, V.; Janevski, V. Hepatocellular carcinoma: Risk factors, diagnosis and treatment. Maced. J. Med. Sci. 2015, 3, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.; Yoon, S.; Lencioni, R. The etiology of hepatocellular carcinoma and consequences for treatment. Oncologist 2010, 15 (Suppl. S4), 14–22. [Google Scholar] [CrossRef] [PubMed]
- Collaboration Global Burden of Disease Liver Cancer. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: Results from the Global Burden of Disease Study 2015. JAMA Oncol. 2017, 3, 1683–1691. [Google Scholar] [CrossRef] [PubMed]
- Zoheiry, M.M.; Hasan, S.A.; El-Ahwany, E.; Nagy, F.M.; Taleb, H.A.; Nosseir, M.; Magdy, M.; Meshaal, S.; EL-Talkawy, M.D.; Raafat, I. Serum markers of epithelial-mesenchymal transition as predictors of HCV-induced liver fibrosis, cirrhosis, and hepatocellular carcinoma. Electron. Physician 2015, 7, 1626. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Irshad, M.; Gupta, P.; Irshad, K. Molecular basis of hepatocellular carcinoma induced by hepatitis C virus infection. World J. Hepatol. 2017, 9, 1305–1314. [Google Scholar] [CrossRef]
- Mesri, E.; Feitelson, M.; Munger, K. Human viral oncogenesis: A cancer hallmarks analysis. Cell Host Microbe 2014, 15, 266–282. [Google Scholar] [CrossRef]
- Bruno, S.; Crosignani, A.; Maisonneuve, P.; Rossi, S.; Silini, E.; Mondelli, M.U. Hepatitis C virus genotype 1b as a major risk factor associated with hepatocellular carcinoma in patients with cirrhosis: A seventeen-year prospective cohort study. Hepatology 2007, 46, 1350–1356. [Google Scholar] [CrossRef]
- Lok, A.S.; Seeff, L.B.; Morgan, T.R.; Di Bisceglie, A.M.; Sterling, R.K.; Curto, T.M.; Everson, G.T.; Lindsay, K.L.; Lee, W.M.; Bonkovsky, H.L.; et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advancedliver disease. Gastroenterology 2009, 136, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wei, C. Advances in the early diagnosis of hepatocellular carcinoma. Genes Dis. 2020, 7, 308–319. [Google Scholar] [CrossRef]
- Han, L.L.; Lv, Y.; Guo, H.; Ruan, Z.P.; Nan, K.J. Implications of biomarkers in human hepatocellular carcinoma pathogenesis and therapy. World J. Gastroenterol. 2014, 20, 10249–10261. [Google Scholar] [CrossRef]
- Zheng, Z.; Qiu, K.; Huang, W. Long Non-Coding RNA (lncRNA) RAMS11 Promotes Metastatis and Cell Growth of Prostate Cancer by CBX4 Complex Binding to Top2α. Cancer Manag. Res. 2021, 2, 913–923. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Lu, J.; Wang, R.; Cao, W.; Xu, J. TOP2A promotes proliferation and metastasis of hepatocellular carcinoma regulated by miR-144-3p. J. Cancer 2022, 13, 589–601. [Google Scholar] [CrossRef] [PubMed]
- Panvichian, R.; Tantiwetrueangdet, A.; Angkathunyakul, N.; Leelaudomlipi, S. TOP2A Amplification and Overexpression in Hepatocellular Carcinoma Tissues. BioMed Res. Int. 2015, 2015, 381602. [Google Scholar] [CrossRef] [PubMed]
- Watanuki, A.; Ohwada, S.; Fukusato, T.; Makita, F.; Yamada, T.; Kikuchi, A.; Morishita, Y. Prognostic significance of DNA topoisomerase IIalpha expression in human hepatocellular carcinoma. Anticancer Res. 2002, 22, 1113–1119. [Google Scholar]
- Cai, H.; Shao, B.; Zhou, Y.; Chen, Z. High expression of TOP2A in hepatocellular carcinoma is associated with disease progression and poor prognosis. Oncol. Lett. 2020, 20, 232. [Google Scholar] [CrossRef]
- Meng, J.; Wei, Y.; Deng, Q.; Li, L.; Li, X. Study on the expression of TOP2A in hepatocellular carcinoma and its relationship with patient prognosis. Cancer Cell Int. 2022, 22, 29. [Google Scholar] [CrossRef]
- Dong, Y.; Sun, X.; Zhang, K.; He, X.; Zhang, Q.; Song, H.; Xu, M.; Lu, H.; Ren, R. Type IIA topoisomerase (TOP2A) triggers epithelial-mesenchymal transition and facilitates HCC progression by regulating Snail expression. Bioengineered 2021, 12, 12967–12979. [Google Scholar] [CrossRef]
- Wong, N.; Yeo, W.; Wong, W.L.; Wong, N.L.Y.; Chan, K.Y.Y.; Mo, F.K.F.; Chan, S.L.; Chan, A.T.C.; Lai, P.B.S.; Ching, A.K.K.; et al. TOP2A overexpression in hepatocellular carcinoma correlates with early age onset, shorter patients’ survival and chemoresistance. Int. J. Cancer 2009, 124, 644–652. [Google Scholar] [CrossRef]
- Jain, C.K.; Roychoudhury, S.; Majumder, H.K. Selective killing of G2 decatenation checkpoint defective colon cancer cells by catalytic topoisomerase II inhibitor. Biochim. Biophys. Acta 2015, 1853, 1195–1204. [Google Scholar] [CrossRef]
- Deng, S.P.; Guo, W.L. Identifying key genes of liver cancer by networking of multiple data sets. IEEE/ACM Trans. Comput. Biol. Bioinform. 2019, 16, 792–800. [Google Scholar] [CrossRef]
- Yu, Y.; Ding, S.; Liang, Y.; Zheng, Y.; Li, W.; Yang, L.; Zheng, X.; Jiang, J. Expression of ERCC1, TYMS, TUBB3, RRM1 and TOP2A in patients with esophageal squamous cell carcinoma: A hierarchical clustering analysis. Exp. Ther. Med. 2014, 7, 1578–1582. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xing, C.; Cai, Z.; Gong, J.; Zhou, J.; Xu, J.; Guo, F. Identification of potential biomarkers involved in gastric cancer through integrated analysis of non-coding RNA associated competing endogenous RNAs network. Clin. Lab. 2018, 64, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.M.; Xiong, D.D.; Lin, P.; Yang, H.; Dang, Y.W.; Chen, G. DNA topoisomerase 1 and 2A function as oncogenes in liver cancer and may be direct targets of nitidine chloride. Int. J. Oncol. 2018, 53, 1897–1912. [Google Scholar] [CrossRef] [PubMed]


| HCC (n = 50) | HCV (n = 50) | Control (n = 50) | Test of Sig. | p | |
|---|---|---|---|---|---|
| Age (years) | |||||
| Mean ± SD. | 59.5 ± 5.7 | 58.1 ± 3.3 | 59.7 ± 4 | F = 1.874 | 0.157 |
| Gender | |||||
| Male | 37 (74%) | 36 (72%) | 31 (62%) | χ2 = 1.944 | 0.378 |
| Female | 13 (26%) | 14 (28%) | 19 (38%) | ||
| ALT (IU/L) | |||||
| Median (Min.–Max.) | 38 (11–76) | 50 (6–168) | 22 (9–47) | H = 45.50 * | <0.001 * |
| Sig. bet. Groups | p1 = 0.384, p2 < 0.001 *, p3 < 0.001 * | ||||
| AST (IU/L) | |||||
| Median (Min.–Max.) | 40.5 (16–78) | 52 (8–138) | 23 (9–50) | H = 60.234 * | <0.001 * |
| Sig. bet. Groups | p1 = 0.428, p2 < 0.001 *, p3 < 0.001 * | ||||
| Hb (g/dl) | |||||
| Mean ± SD. | 10.69 ± 1.41 | 12.54 ± 1.33 | 12.96 ± 0.84 | F = 48.796 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 = 0.198 | ||||
| Platelets (×10³/UL) | |||||
| Mean ± SD. | 126.5 ± 53.3 | 173.6 ± 76.7 | 266.9 ± 66.3 | F = 58.421 * | <0.001 * |
| Sig. bet. Groups | p1 = 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| WBCs (×10³/UL) | |||||
| Mean ± SD. | 5.8 ± 1.6 | 6.6 ± 1.9 | 5.9 ± 1.9 | F = 2.670 | 0.073 |
| Serum albumin (g/dl) | |||||
| Median (Min.–Max.) | 3.2 (2.3–3.9) | 3.4 (2.3–4.4) | 4.5 (3.7–5) | H = 93.732 * | <0.001 * |
| Sig. bet. Groups | p1 = 0.007 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| Total Bilirubin (mg/dl) | |||||
| Median (Min.–Max.) | 1.8 (0.4–15.7) | 0.8 (0.2–5) | 0.6 (0.2–1) | H = 63.090 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| Direct bilirubin (mg/dl) | |||||
| Median (Min.–Max.) | 0.7 (0.1–11.2) | 0.2 (0.1–2) | 0.2 (0.1–0.3) | H = 70.297 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 = 0.019 * | ||||
| PT (%) | |||||
| Median (Min.–Max.) | 84.8 (60–95) | 81 (56–97.3) | 98.5 (94–101) | H = 98.201 * | <0.001 * |
| Sig. bet. Groups | p1 = 0.496, p2 < 0.001 *, p3 < 0.001 * | ||||
| α FP (ng/mL) | |||||
| Median (Min.–Max.) | 123.5 (7–2600) | 23.4 (2.1–614) | 3 (1–6) | H = 100.311 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| HCC (n = 50) | HCV (n = 50) | χ2 | p | |
|---|---|---|---|---|
| Loss of Weight | 34 (68%) | 34 (68%) | 0.0 | 1.000 |
| Jaundice | 13 (26%) | 11 (22%) | 0.219 | 0.640 |
| Hepatic Encephalopathy | 10 (0%) | 4 (8%) | 2.990 | 0.084 |
| Splenomegaly | 34 (68%) | 32 (64%) | 0.178 | 0.673 |
| Ascites | ||||
| No | 12 (24%) | 19 (38%) | 10.082 * | 0.018 * |
| Minimal | 21 (42%) | 23 (46%) | ||
| Moderate | 6 (12%) | 7 (14%) | ||
| Tense | 11 (22%) | 1 (2%) | ||
| Comorbidity | ||||
| DM | 14 (28%) | 21 (42%) | 2.154 | 0.142 |
| HTN | 16 (32%) | 16 (32%) | 0.0 | 1.000 |
| Heart Disease | 1 (2%) | 1 (2%) | 0.0 | FE p = 1.000 |
| Child Pugh Class | ||||
| A | 12 (24%) | 19 (38%) | 6.422 * | 0.040 * |
| B | 25 (50%) | 27 (54%) | ||
| C | 13 (26%) | 4 (8%) |
| HCC (n = 50) | HCV (n = 50) | Control (n = 50) | H | p | |
|---|---|---|---|---|---|
| CBX4 | |||||
| Median (Min.–Max.) | 1.882 (0.180–8.900) | 0.300 (0.007–2.915) | 0.062 (0–1.035) | 96.277 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| LINC01564 | |||||
| Median (Min.–Max.) | 2.081 (0.117–12.040) | 0.431 (0.002–4.158) | 0.056 (0–1.024) | 95.376 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| RAMS11 | |||||
| Median (Min.–Max.) | 1.872 (0.172–9.520) | 0.381 (0.000–1.306) | 0.049 (0.001–1.003) | 99.748 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| TOP2A | |||||
| Median (Min.–Max.) | 1.932 (0.050–10.800) | 0.269 (0.000–2.400) | 0.046 (0.001–1.009) | 91.454 * | <0.001 * |
| Sig. bet. Groups | p1 < 0.001 *, p2 < 0.001 *, p3 < 0.001 * | ||||
| AUC | p | 95% C.I | Cut off | Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|---|---|---|---|
| LINC01564 | 0.84 | <0.001 | 0.763–0.917 | >1.3046 | 80 | 78 | 78.4 | 79.6 |
| RAMS11 | 0.911 | <0.001 | 0.854–0.969 | >1.006 | 86 | 86 | 86 | 86 |
| CBX4 | 0.923 | <0.001 | 0.871–0.975 | >1.012 | 86 | 88 | 87.8 | 86.3 |
| TOP2A | 0.908 | <0.001 | 0.850–0.967 | >1.0521 | 82 | 88 | 87.2 | 83 |
| CBX4 | LINC01564 | RAMS11 | TOP2A | ||
|---|---|---|---|---|---|
| Age (years) | rs | 0.081 | 0.093 | 0.109 | −0.070 |
| p | 0.576 | 0.522 | 0.451 | 0.630 | |
| ALT | rs | 0.366 | 0.341 | 0.381 | 0.354 |
| p | 0.009 | 0.015 | 0.006 | 0.012 | |
| AST | rs | 0.362 | 0.305 | 0.373 | 0.334 |
| p | 0.010 | 0.031 | 0.008 | 0.018 | |
| Hb | rs | 0.156 | 0.025 | 0.052 | 0.028 |
| p | 0.280 | 0.861 | 0.719 | 0.850 | |
| Platelets | rs | −0.141 | 0.056 | 0.030 | −0.080 |
| p | 0.329 | 0.697 | 0.835 | 0.580 | |
| WBCS | rs | 0.013 | 0.061 | 0.043 | −0.138 |
| p | 0.928 | 0.673 | 0.768 | 0.340 | |
| Serum albumin | rs | −0.186 | −0.139 | 0.055 | −0.096 |
| p | 0.195 | 0.337 | 0.702 | 0.507 | |
| Total Bilirubin | rs | 0.011 | 0.043 | −0.008 | 0.120 |
| p | 0.938 | 0.768 | 0.957 | 0.405 | |
| Direct bilirubin | rs | 0.027 | 0.042 | −0.006 | 0.148 |
| p | 0.854 | 0.771 | 0.966 | 0.305 | |
| PT | rs | 0.106 | −0.106 | −0.107 | −0.104 |
| p | 0.463 | 0.463 | 0.458 | 0.471 | |
| α FP | rs | 0.068 | −0.007 | −0.037 | 0.077 |
| p | 0.638 | 0.963 | 0.800 | 0.597 | |
| Overall survival time (months) | rs | −0.470 | −0.572 | −0.622 | −0.573 |
| p | 0.001 | <0.001 | <0.001 | <0.001 |
| Univariate | # Multivariate | |||
|---|---|---|---|---|
| p | HR (LL–UL 95% C.I) | p | HR (LL–UL 95% C.I) | |
| Age (years) | 0.511 | 1.032 (0.939–1.134) | ||
| Gender (female) | 0.446 | 0.611 (0.172–2.168) | ||
| ALT | 0.108 | 1.026 (0.994–1.059) | ||
| AST | 0.294 | 1.016 (0.986–1.046) | ||
| Hb | 0.370 | 0.837 (0.567–1.235) | ||
| Platelets | 0.378 | 1.004 (0.995–1.013) | ||
| WBCS | 0.476 | 0.878 (0.614–1.255) | ||
| Serum albumin | 0.695 | 1.240 (0.423–3.635) | ||
| Total Bilirubin | 0.017 * | 1.143 (1.024–1.275) | 0.733 | 1.296 (0.293–5.727) |
| Direct bilirubin | 0.024 * | 1.185 (1.023–1.373) | 0.986 | 0.982 (0.127–7.621) |
| PT | 0.592 | 1.017 (0.957–1.080) | ||
| α FP | 0.032 * | 1.001 (1.0–1.001) | 0.444 | 1.000 (0.999–1.001) |
| Vascular invasion | 0.262 | 1.852 (0.631–5.437) | ||
| LN metastasis | 0.023 * | 3.259 (1.176–9.032) | 0.044 * | 13.077 (1.065–160.525) |
| Tumor Number | 0.751 | 1.204 (0.383–3.781) | ||
| Tumor Size | 0.529 | 1.386 (0.502–3.822) | ||
| TNM Staging (III + IV) | 0.189 | 30.688 (0.186–5072.267) | ||
| BCLC (C) | 0.003 * | 5.556 (1.759–17.550) | 0.786 | 0.711 (0.061–8.323) |
| CBX4 | 0.002 * | 1.299 (1.101–1.533) | 0.524 | 0.864 (0.552–1.354) |
| LINC01564 | <0.001 * | 1.345 (1.165–1.553) | 0.035 * | 1.297 (1.019–1.651) |
| RAMS11 | <0.001 * | 1.385 (1.184–1.620) | 0.730 | 0.916 (0.555–1.510) |
| TOP2A | <0.001 * | 1.580 (1.301–1.919) | 0.004 * | 2.543 (1.345–4.809) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badr, E.A.E.; Elmongy, E.I.; Mostafa, R.G.; El-Sayed, I.E.-T.; Abd El-Ati Gad Allah, A.E.-N.; Khairy Ahmed, A.; Elghobashy, Y.A.S. The Role of LINC01564, RAMS11, CBX4 and TOP2A in Hepatocellular Carcinoma. Biomedicines 2023, 11, 56. https://doi.org/10.3390/biomedicines11010056
Badr EAE, Elmongy EI, Mostafa RG, El-Sayed IE-T, Abd El-Ati Gad Allah AE-N, Khairy Ahmed A, Elghobashy YAS. The Role of LINC01564, RAMS11, CBX4 and TOP2A in Hepatocellular Carcinoma. Biomedicines. 2023; 11(1):56. https://doi.org/10.3390/biomedicines11010056
Chicago/Turabian StyleBadr, Eman A. E., Elshaymaa I. Elmongy, Rasha Galal Mostafa, Ibrahim El-Tantawy El-Sayed, Abd El-Naser Abd El-Ati Gad Allah, Asmaa Khairy Ahmed, and Yasser A. S. Elghobashy. 2023. "The Role of LINC01564, RAMS11, CBX4 and TOP2A in Hepatocellular Carcinoma" Biomedicines 11, no. 1: 56. https://doi.org/10.3390/biomedicines11010056
APA StyleBadr, E. A. E., Elmongy, E. I., Mostafa, R. G., El-Sayed, I. E.-T., Abd El-Ati Gad Allah, A. E.-N., Khairy Ahmed, A., & Elghobashy, Y. A. S. (2023). The Role of LINC01564, RAMS11, CBX4 and TOP2A in Hepatocellular Carcinoma. Biomedicines, 11(1), 56. https://doi.org/10.3390/biomedicines11010056






