Metabolic Syndrome and Obesity-Related Indices Are Associated with Rapid Renal Function Decline in a Large Taiwanese Population Follow-Up Study
Abstract
:1. Introduction
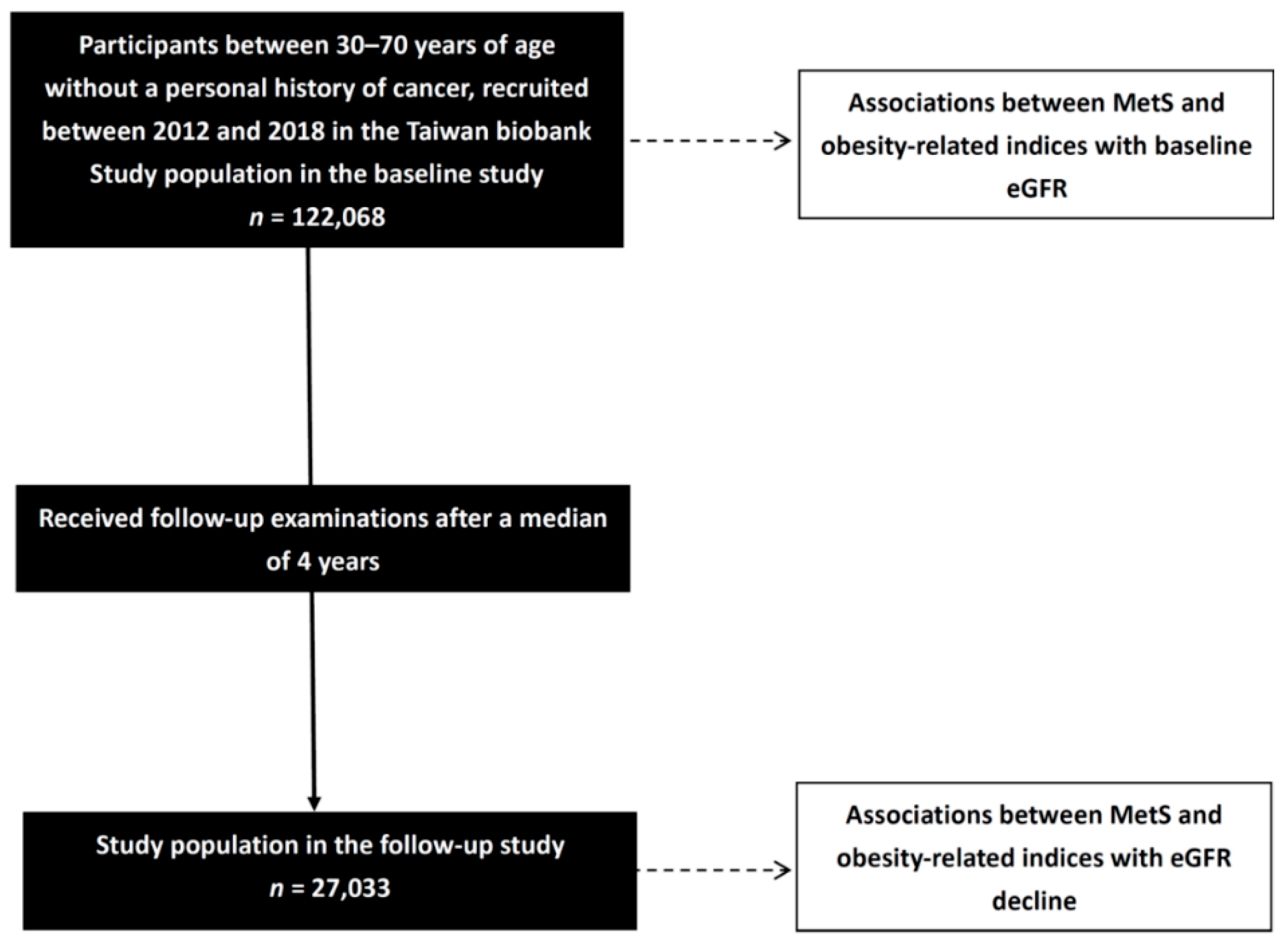
2. Materials and Methods
2.1. The Taiwan Biobank
2.2. Collection of Study Variables
2.3. Definitions of Renal Function Decline (△eGFR) and MetS
2.4. Calculation of Obesity-Related Indices
2.5. Statistical Analysis
2.6. Comparisons of Clinical Characteristics between the Participants with and without MetS at Baseline
3. Results
3.1. Association between MetS and Obesity-Related Indices with Baseline eGFR in All Participants
- (1)
- Adjusted for sex, age, smoking history, hemoglobin, LDL-C, total cholesterol, and uric acid (the significant factors in univariable analysis excluding DM, hypertension, SBP, DBP, fasting glucose, TGs, and HDL-C) for MetS.
- (2)
- Adjusted for sex, age, smoking history, DM, hypertension, SBP, DBP, uric acid, fasting glucose, hemoglobin, TGs, HDL-C, LDL-C, and total cholesterol (significant factors in univariable analysis) for WHtR, WHR, CI, BRI, BMI, BAI, AVI, and ABSI.
- (3)
- Adjusted for sex, age, smoking history, DM, hypertension, SBP, DBP, uric acid, fasting glucose, hemoglobin, HDL-C, LDL-C, and total cholesterol (significant factors in the univariable analysis except for TGs) for LAP.
- (4)
- Adjusted for sex, age, smoking history, DM, hypertension, SBP, DBP, uric acid, fasting glucose, hemoglobin, LDL-C, and total cholesterol (significant factors in the univariable analysis except for TGs and HDL-C) for VAI.
3.2. Association between MetS and Obesity-Related Indices with △eGFR in Follow-Up Participants
- (1)
- Adjusted sex, age, hemoglobin, LDL-C, total cholesterol, and uric acid (the significant factors in univariable analysis excluding DM, hypertension, SBP, DBP, fasting glucose, and HDL-C) for MetS.
- (2)
- Adjusted for sex, age, DM, hypertension, SBP, DBP, uric acid, fasting glucose, hemoglobin, HDL-C, LDL-C, and total cholesterol (significant factors in univariable analysis) for WHtR, WHR, CI, BRI, BMI, BAI, AVI, and ABSI.
- (3)
- Adjusted for sex, age, DM, hypertension, SBP, DBP, uric acid, fasting glucose, hemoglobin, LDL-C, and total cholesterol (significant factors in the univariable analysis except for HDL-C) for VAI.
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Mets | metabolic syndrome |
| BMI | body mass index |
| WHR | waist-to-hip ratio |
| WHtR | waist-to-height ratio |
| LAP | lipid accumulation product |
| BRI | body roundness index |
| CI | conicity index |
| BAI | body adiposity index |
| AVI | abdominal volume index |
| VAI | visceral adiposity index |
| ABSI | A body shape index |
References
- Lai, T.S.; Hsu, C.C.; Lin, M.H.; Wu, V.C.; Chen, Y.M. Trends in the incidence and prevalence of end-stage kidney disease requiring dialysis in Taiwan: 2010–2018. J. Formos. Med. Assoc. 2022, 121, S5–S11. [Google Scholar] [CrossRef] [PubMed]
- Yamagata, K.; Yagisawa, T.; Nakai, S.; Nakayama, M.; Imai, E.; Hattori, M.; Iseki, K.; Akiba, T. Prevalence and incidence of chronic kidney disease stage G5 in Japan. Clin. Exp. Nephrol. 2015, 19, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.J.; Raggi, P.; Wolf, M.; Gold, A.M.; Chertow, G.M.; Roe, M.T. Targeting Vascular Calcification in Chronic Kidney Disease. JACC Basic Transl. Sci. 2020, 5, 398–412. [Google Scholar] [CrossRef]
- Chen, T.K.; Knicely, D.H.; Grams, M.E. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA 2019, 322, 1294–1304. [Google Scholar] [CrossRef]
- Ahirwar, A.K.; Jain, A.; Singh, A.; Goswami, B.; Bhatnagar, M.K.; Bhatacharjee, J. The study of markers of endothelial dysfunction in metabolic syndrome. Horm. Mol. Biol. Clin. Investig. 2015, 24, 131–136. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [Green Version]
- Cheng, C.H.; Ho, C.C.; Yang, C.F.; Huang, Y.C.; Lai, C.H.; Liaw, Y.P. Waist-to-hip ratio is a better anthropometric index than body mass index for predicting the risk of type 2 diabetes in Taiwanese population. Nutr. Res. 2010, 30, 585–593. [Google Scholar] [CrossRef]
- Maurizi, G.; Della Guardia, L.; Maurizi, A.; Poloni, A. Adipocytes properties and crosstalk with immune system in obesity-related inflammation. J. Cell. Physiol. 2018, 233, 88–97. [Google Scholar] [CrossRef]
- Wu, H.; Ballantyne, C.M. Metabolic Inflammation and Insulin Resistance in Obesity. Circ. Res. 2020, 126, 1549–1564. [Google Scholar] [CrossRef]
- Lin, C.C.; Liu, C.S.; Li, T.C.; Chen, C.C.; Li, C.I.; Lin, W.Y. Microalbuminuria and the metabolic syndrome and its components in the Chinese population. Eur. J. Clin. Investig. 2007, 37, 783–790. [Google Scholar] [CrossRef]
- Lu, J.L.; Molnar, M.Z.; Naseer, A.; Mikkelsen, M.K.; Kalantar-Zadeh, K.; Kovesdy, C.P. Association of age and BMI with kidney function and mortality: A cohort study. Lancet Diabetes Endocrinol. 2015, 3, 704–714. [Google Scholar] [CrossRef] [Green Version]
- Motamed, N.; Rabiee, B.; Hemasi, G.R.; Ajdarkosh, H.; Khonsari, M.R.; Maadi, M.; Keyvani, H.; Zamani, F. Body Roundness Index and Waist-to-Height Ratio are Strongly Associated With Non-Alcoholic Fatty Liver Disease: A Population-Based Study. Hepat. Mon. 2016, 16, e39575. [Google Scholar] [CrossRef] [Green Version]
- Whaley-Connell, A.; Sowers, J.R. Insulin Resistance in Kidney Disease: Is There a Distinct Role Separate from That of Diabetes or Obesity? Cardiorenal. Med. 2017, 8, 41–49. [Google Scholar] [CrossRef]
- Cheng, H.T.; Huang, J.W.; Chiang, C.K.; Yen, C.J.; Hung, K.Y.; Wu, K.D. Metabolic syndrome and insulin resistance as risk factors for development of chronic kidney disease and rapid decline in renal function in elderly. J. Clin. Endocrinol. Metab. 2012, 97, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Yang, J.H.; Chiang, C.W.K.; Hsiung, C.N.; Wu, P.E.; Chang, L.C.; Chu, H.W.; Chang, J.; Song, I.W.; Yang, S.L.; et al. Population structure of Han Chinese in the modern Taiwanese population based on 10,000 participants in the Taiwan Biobank project. Hum. Mol. Genet. 2016, 25, 5321–5331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, C.T.; Hung, T.H.; Yeh, C.K. Taiwan Regulation of Biobanks. J. Law. Med. Ethics 2015, 43, 816–826. [Google Scholar] [CrossRef]
- Directorate General of Budget, Accounting and Statistics, Executive Yuan, Republic of China (Ed.) Social Indicators 2010; Directorate General of Budget, Accounting and Statistics of Executive Yuan: Taipeh, Taiwan, 2011.
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Isomaa, B.; Henricsson, M.; Almgren, P.; Tuomi, T.; Taskinen, M.R.; Groop, L. The metabolic syndrome influences the risk of chronic complications in patients with type II diabetes. Diabetologia 2001, 44, 1148–1154. [Google Scholar] [CrossRef] [Green Version]
- Kahn, H.S. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disord. 2005, 5, 26. [Google Scholar] [CrossRef] [Green Version]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef] [Green Version]
- Valdez, R. A simple model-based index of abdominal adiposity. J. Clin. Epidemiol. 1991, 44, 955–956. [Google Scholar] [CrossRef]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A better index of body adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Rodríguez-Morán, M. Abdominal volume index. An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch. Med. Res. 2003, 34, 428–432. [Google Scholar] [CrossRef]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef]
- Wu, Z.; Jiang, Y.; Jia, J.; He, D.; Sun, P.; Li, J.; Huo, Y.; Fan, F.; Zhang, Y. Metabolic Syndrome Is Associated With Rapid Estimated Glomerular Filtration Rate Decline In A Chinese Community-Based Population. Diabetes Metab. Syndr. Obes. 2019, 12, 2085–2093. [Google Scholar] [CrossRef] [Green Version]
- Kurella, M.; Lo, J.C.; Chertow, G.M. Metabolic syndrome and the risk for chronic kidney disease among nondiabetic adults. J. Am. Soc. Nephrol. 2005, 16, 2134–2140. [Google Scholar] [CrossRef]
- Song, H.; Wang, X.; Cai, Q.; Ding, W.; Huang, S.; Zhuo, L. Association of metabolic syndrome with decreased glomerular filtration rate among 75,468 Chinese adults: A cross-sectional study. PLoS ONE 2014, 9, e113450. [Google Scholar] [CrossRef]
- Pammer, L.M.; Lamina, C.; Schultheiss, U.T.; Kotsis, F.; Kollerits, B.; Stockmann, H.; Lipovsek, J.; Meiselbach, H.; Busch, M.; Eckardt, K.U.; et al. Association of the metabolic syndrome with mortality and major adverse cardiac events: A large chronic kidney disease cohort. J. Intern. Med. 2021, 290, 1219–1232. [Google Scholar] [CrossRef]
- Tonneijck, L.; Muskiet, M.H.; Smits, M.M.; van Bommel, E.J.; Heerspink, H.J.; van Raalte, D.H.; Joles, J.A. Glomerular Hyperfiltration in Diabetes: Mechanisms, Clinical Significance, and Treatment. J. Am. Soc. Nephrol. 2017, 28, 1023–1039. [Google Scholar] [CrossRef] [Green Version]
- Bae, E.H.; Oh, T.R.; Suh, S.H.; Yang, E.M.; Choi, H.S.; Kim, C.S.; Ma, S.K.; Kim, B.; Han, K.D.; Kim, S.W. Underweight and Weight Change Increases End-Stage Renal Disease Risk in Patients with Diabetes: A Nationwide Population-Based Cohort Study. Nutrients 2021, 14, 154. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, M.; Charchar, F.J.; Maric, C.; McClure, J.; Crawford, L.; Grzeszczak, W.; Sattar, N.; Zukowska-Szczechowska, E.; Dominiczak, A.F. Glomerular hyperfiltration: A new marker of metabolic risk. Kidney Int. 2007, 71, 816–821. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Briffa, J.F.; McAinch, A.J.; Poronnik, P.; Hryciw, D.H. Adipokines as a link between obesity and chronic kidney disease. Am. J. Physiol. Renal Physiol. 2013, 305, F1629–F1636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huh, J.H.; Yadav, D.; Kim, J.S.; Son, J.W.; Choi, E.; Kim, S.H.; Shin, C.; Sung, K.C.; Kim, J.Y. An association of metabolic syndrome and chronic kidney disease from a 10-year prospective cohort study. Metabolism 2017, 67, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Sarafidis, P.A.; Ruilope, L.M. Insulin resistance, hyperinsulinemia, and renal injury: Mechanisms and implications. Am. J. Nephrol. 2006, 26, 232–244. [Google Scholar] [CrossRef]
- Sarafidis, P.A.; Lasaridis, A.N. Insulin resistance and endothelin: Another pathway for renal injury in patients with the cardiometabolic syndrome? J. Cardiometab. Syndr. 2008, 3, 183–187. [Google Scholar] [CrossRef]
- Lee, S.J.; Lee, H.J.; Oh, H.J.; Go, T.; Kang, D.R.; Kim, J.Y.; Huh, J.H. Metabolic syndrome status over 2 years predicts incident chronic kidney disease in mid-life adults: A 10-year prospective cohort study. Sci. Rep. 2018, 8, 12237. [Google Scholar] [CrossRef]
- Bamba, R.; Okamura, T.; Hashimoto, Y.; Hamaguchi, M.; Obora, A.; Kojima, T.; Fukui, M. The Visceral Adiposity Index Is a Predictor of Incident Chronic Kidney Disease: A Population-Based Longitudinal Study. Kidney Blood Press. Res. 2020, 45, 407–418. [Google Scholar] [CrossRef]
- Mousapour, P.; Barzin, M.; Valizadeh, M.; Mahdavi, M.; Azizi, F.; Hosseinpanah, F. Predictive performance of lipid accumulation product and visceral adiposity index for renal function decline in non-diabetic adults, an 8.6-year follow-up. Clin. Exp. Nephrol. 2020, 24, 225–234. [Google Scholar] [CrossRef]
- Kim, B.; Kim, G.; Kim, E.; Park, J.; Isobe, T.; Sakae, T.; Oh, S. The A Body Shape Index Might Be a Stronger Predictor of Chronic Kidney Disease Than BMI in a Senior Population. Int. J. Environ. Res. Public Health 2021, 18, 12874. [Google Scholar] [CrossRef]
- Ou, Y.L.; Lee, M.Y.; Lin, I.T.; Wen, W.L.; Hsu, W.H.; Chen, S.C. Obesity-related indices are associated with albuminuria and advanced kidney disease in type 2 diabetes mellitus. Ren. Fail. 2021, 43, 1250–1258. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.F.; Al Mamun, A.; Huang, M.C.; Long, K.Z.; Huang, Y.F.; Shin, S.J.; Hwang, S.J.; Hsu, C.C. Obesity, weight change, and chronic kidney disease in patients with type 2 diabetes mellitus: A longitudinal study in Taiwan. J. Diabetes 2017, 9, 983–993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, S.; Tian, Z.; Torigoe, D.; Zhao, J.; Xie, P.; Sugizaki, T.; Sato, M.; Horiguchi, H.; Terada, K.; Kadomatsu, T.; et al. Aging- and obesity-related peri-muscular adipose tissue accelerates muscle atrophy. PLoS ONE 2019, 14, e0221366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nankivell, B.J.; Nankivell, L.F.J.; Elder, G.J.; Gruenewald, S.M. How unmeasured muscle mass affects estimated GFR and diagnostic inaccuracy. eClinicalMedicine 2020, 29, 100662. [Google Scholar] [CrossRef] [PubMed]
- Matsuzawa, Y.; Funahashi, T.; Nakamura, T. The concept of metabolic syndrome: Contribution of visceral fat accumulation and its molecular mechanism. J. Atheroscler. Thromb. 2011, 18, 629–639. [Google Scholar] [CrossRef] [Green Version]
- Chiu, T.H.; Huang, Y.C.; Chiu, H.; Wu, P.Y.; Chiou, H.C.; Huang, J.C.; Chen, S.C. Comparison of Various Obesity-Related Indices for Identification of Metabolic Syndrome: A Population-Based Study from Taiwan Biobank. Diagnostics 2020, 10, 1081. [Google Scholar] [CrossRef]
- Chang, A.R.; Grams, M.E.; Ballew, S.H.; Bilo, H.; Correa, A.; Evans, M.; Gutierrez, O.M.; Hosseinpanah, F.; Iseki, K.; Kenealy, T.; et al. Adiposity and risk of decline in glomerular filtration rate: Meta-analysis of individual participant data in a global consortium. BMJ 2019, 364, k5301. [Google Scholar] [CrossRef] [Green Version]
- Malkina, A.; Katz, R.; Shlipak, M.G.; Ix, J.H.; de Boer, I.H.; Sarnak, M.J.; Allison, M.; Kramer, H.J.; Lin, J.; Siscovick, D.; et al. Association of Obesity and Kidney Function Decline among Non-Diabetic Adults with eGFR > 60 ml/min/1.73 m (2): Results from the Multi-Ethnic Study of Atherosclerosis (MESA). Open J. Endocr. Metab. Dis. 2013, 3, 103–112. [Google Scholar] [CrossRef] [Green Version]
- Yan, P.; Xu, Y.; Miao, Y.; Tang, Q.; Wu, Y.; Bai, X.; Zhang, Z.; Li, Q.; Wan, Q. Association of lipid accumulation product with chronic kidney disease in Chinese community adults: A report from the REACTION study. Lipids Health Dis. 2021, 20, 131. [Google Scholar] [CrossRef]
- Zhang, K.; Li, Q.; Chen, Y.; Wang, N.; Lu, Y. Visceral adiposity and renal function: An observational study from SPECT-China. Lipids Health Dis. 2017, 16, 205. [Google Scholar] [CrossRef] [Green Version]
- Straznicky, N.E.; Grima, M.T.; Lambert, E.A.; Eikelis, N.; Dawood, T.; Lambert, G.W.; Nestel, P.J.; Masuo, K.; Sari, C.I.; Chopra, R.; et al. Exercise augments weight loss induced improvement in renal function in obese metabolic syndrome individuals. J. Hypertens. 2011, 29, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.S.; Do Han, K.; Kim, M.K.; Kim, E.S.; Lee, M.K.; Nam, G.E.; Hong, O.K.; Kwon, H.S. Changes in metabolic syndrome status affect the incidence of end-stage renal disease in the general population: A nationwide cohort study. Sci. Rep. 2021, 11, 1957. [Google Scholar] [CrossRef] [PubMed]
| Item | Calculation Formula |
|---|---|
| BMI | BW (kg)/BH2 (m) |
| WHR | WC (cm)/HC (cm) |
| WHtR | WC (cm)/BH (cm) |
| LAP | in females [22] |
| BRI | [23] |
| CI | [24] |
| BAI | [25] |
| AVI | [26] |
| VAI | in females [27] |
| ABSI | WC (m)/[BMI2/3(kg/m2) × BH1/2(m)] [28] |
| Characteristics | MetS (−) (n = 100,519) | MetS (+) (n = 21,549) | p |
|---|---|---|---|
| Age (year) | 49.1 ± 11.0 | 53.6 ± 10.2 | <0.001 |
| Male gender (%) | 34.5 | 42.8 | <0.001 |
| DM (%) | 2.2 | 19.1 | <0.001 |
| Hypertension (%) | 7.5 | 31.6 | <0.001 |
| Smoking history (%) | 25.8 | 33.9 | <0.001 |
| SBP (mmHg) | 116.8 ± 16.9 | 132.6 ± 18.2 | <0.001 |
| DBP (mmHg) | 71.8 ± 10.4 | 80.5 ± 11.4 | <0.001 |
| Body height (cm) | 161.8 ± 8.2 | 162.3 ± 8.8 | <0.001 |
| Body weight (kg) | 61.8 ± 11.6 | 73.0 ± 13.9 | <0.001 |
| Waist circumference (cm) | 81.3 ± 9.3 | 92.7 ± 9.2 | <0.001 |
| Hip circumference (cm) | 95.0 ± 6.6 | 100.5 ± 7.8 | <0.001 |
| Laboratory parameters | |||
| Fasting glucose (mg/dL) | 92.7 ± 13.7 | 110.9 ± 35.9 | <0.001 |
| Hemoglobin (g/dL) | 13.7 ± 1.6 | 14.2 ± 1.6 | <0.001 |
| Triglyceride (mg/dL) | 95.9 ± 59.1 | 207.6 ± 153.1 | <0.001 |
| Total cholesterol (mg/dL) | 195.1 ± 35.0 | 198.3 ± 39.5 | <0.001 |
| HDL cholesterol (mg/dL) | 57.1 ± 13.0 | 42.8 ± 8.6 | <0.001 |
| LDL cholesterol (mg/dL) | 120.6 ± 31.2 | 122.3 ± 34.1 | <0.001 |
| eGFR (mL/min/1.73 m2) | 110.9 ± 25.1 | 104.5 ± 26.9 | <0.001 |
| Uric acid (mg/dL) | 5.3 ± 1.4 | 6.2 ± 1.5 | <0.001 |
| Obesity-related indices | |||
| BMI (kg/m2) | 23.5 ± 3.4 | 27.6 ± 3.9 | <0.001 |
| WHR (%) | 85.4 ± 6.5 | 92.2 ± 6.0 | <0.001 |
| WHtR (%) | 50.3 ± 5.6 | 57.2 ± 5.5 | <0.001 |
| LAP | 23.5 ± 18.7 | 73.3 ± 56.3 | <0.001 |
| BRI | 6.4 ± 1.7 | 8.6 ± 1.9 | <0.001 |
| CI | 1.21 ± 0.08 | 1.27 ± 0.07 | <0.001 |
| BAI | 28.3 ± 4.0 | 30.8 ± 4.6 | <0.001 |
| AVI | 13.5 ± 3.1 | 17.4 ± 3.6 | <0.001 |
| VAI | 1.3 ± 1.1 | 3.7 ± 3.4 | <0.001 |
| ABSI | 0.078 ± 0.004 | 0.080 ± 0.005 | <0.001 |
| Characteristics | Univariable | |
|---|---|---|
| Unstandardized Coefficient β (95% Confidence Interval) | p | |
| Age (per 1 year) | −0.682 (−0.695, −0.670) | <0.001 |
| Female (vs. male) | 15.777 (15.491, 16.062) | <0.001 |
| DM | −5.852 (−6.498, −5.206) | <0.001 |
| Hypertension | −12.369 (−12.800, −11.937) | <0.001 |
| Smoking history | −8.112 (−8.431, −7.794) | <0.001 |
| SBP (per 1 mmHg) | −0.298 (−0.306, −0.290) | <0.001 |
| DBP (per 1 mmHg) | −0.443 (−0.456, −0.431) | <0.001 |
| Laboratory parameters | ||
| Fasting glucose (per 1 mg/dL) | −0.072 (−0.079, −0.065) | <0.001 |
| Hemoglobin (per 1 g/dL) | −3.864 (−3.951, −3.777) | <0.001 |
| Triglyceride (per 1 mg/dL) | −0.031 (−0.033, −0.029) | <0.001 |
| Total cholesterol (per 1 mg/dL) | −0.071 (−0.075, −0.067) | <0.001 |
| HDL cholesterol (per 1 mg/dL) | 0.216 (0.205, 0.227) | <0.001 |
| LDL cholesterol (per 1 mg/dL) | −0.082 (−0.086, −0.077) | <0.001 |
| Uric acid (per 1 mg/dL) | −7.101 (−7.193, −7.009) | <0.001 |
| Obesity-Related Indices | Multivariable | |
|---|---|---|
| Unstandardized Coefficient β (95% Confidence Interval) | p | |
| MetS a | 2.190 (1.848, 2.532) | <0.001 |
| BMI (per 1 kg/m2) b | 0.245 (0.205, 0.284) | <0.001 |
| WHR (per 1%) b | 0.384 (0.362, 0.407) | <0.001 |
| WHtR (per 1%) b | 0.427 (0.403, 0.451) | <0.001 |
| LAP (per 1) c | 0.042 (0.036, 0.048) | <0.001 |
| BRI (per 1) b | 1.149 (1.074, 1.225) | <0.001 |
| CI (per 0.1) b | 3.197 (3.029, 3.365) | <0.001 |
| BAI (per 1) b | 0.473 (0.437, 0.509) | <0.001 |
| AVI (per 1) b | 0.425 (0.381, 0.468) | <0.001 |
| VAI (per 1) d | 0.567 (0.495, 0.639) | <0.001 |
| ABSI (per 0.01) b | 4.722 (4.452, 4.992) | <0.001 |
| Characteristics | Univariable | |
|---|---|---|
| Unstandardized Coefficient β (95% Confidence Interval) | p | |
| Age (per 1 year) | −0.058 (−0.079, −0.038) | <0.001 |
| Female (vs. male) | −0.699 (−1.148, −0.249) | 0.002 |
| DM | −4.052 (−5.011, −3.093) | <0.001 |
| Hypertension | −1.842 (−2.479, −1.204) | <0.001 |
| Smoking history | 0.341 (−0.152, 0.833) | 0.175 |
| SBP (per 1 mmHg) | −0.067 (−0.079, −0.055) | <0.001 |
| DBP (per 1 mmHg) | −0.051 (−0.071, −0.032) | <0.001 |
| Laboratory parameters | ||
| Fasting glucose (per 1 mg/dL) | −0.034 (−0.045, −0.023) | <0.001 |
| Hemoglobin (per 1 g/dL) | 0.444 (0.305, 0.582) | <0.001 |
| Triglyceride (per 1 mg/dL) | 0 (−0.003, 0.002) | 0.751 |
| Total cholesterol (per 1 mg/dL) | 0.009 (0.003, 0.015) | 0.004 |
| HDL cholesterol (per 1 mg/dL) | 0.019 (0.003, 0.036) | 0.020 |
| LDL cholesterol (per 1 mg/dL) | 0.022 (0.015, 0.029) | <0.001 |
| Uric acid (per 1 mg/dL) | 1.061 (0.910, 1.211) | <0.001 |
| Obesity-Related Indices | Multivariable | |
|---|---|---|
| Unstandardized Coefficient β (95% Confidence Interval) | p | |
| MetS a | −1.972 (−2.569, −1.374) | <0.001 |
| BMI (per 1 kg/m2) b | −0.064 (−0.135, 0.007) | 0.075 |
| WHR (per 1%) b | −0.030 (−0.068, 0.008) | 0.126 |
| WHtR (per 1%) b | −0.058 (−0.100, −0.016) | 0.007 |
| LAP (per 1) b | 0.022 (0.011, 0.033) | <0.001 |
| BRI (per 1) b | −0.206 (−0.339, −0.072) | 0.002 |
| CI (per 0.1) b | −0.452 (−0.740, −0.163) | 0.002 |
| BAI (per 1) b | −0.060 (−0.123, 0.004) | 0.066 |
| AVI (per 1) b | −0.129 (−0.206, −0.051) | 0.001 |
| VAI (per 1) c | −0.174 (−0.318, −0.031) | 0.017 |
| ABSI (per 0.01) b | −0.585 (−1.046, −0.125) | 0.013 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, W.-Y.; Chen, I.-H.; Gau, Y.-C.; Wu, P.-Y.; Huang, J.-C.; Tsai, Y.-C.; Chen, S.-C.; Chang, J.-M.; Hwang, S.-J.; Chen, H.-C. Metabolic Syndrome and Obesity-Related Indices Are Associated with Rapid Renal Function Decline in a Large Taiwanese Population Follow-Up Study. Biomedicines 2022, 10, 1744. https://doi.org/10.3390/biomedicines10071744
Su W-Y, Chen I-H, Gau Y-C, Wu P-Y, Huang J-C, Tsai Y-C, Chen S-C, Chang J-M, Hwang S-J, Chen H-C. Metabolic Syndrome and Obesity-Related Indices Are Associated with Rapid Renal Function Decline in a Large Taiwanese Population Follow-Up Study. Biomedicines. 2022; 10(7):1744. https://doi.org/10.3390/biomedicines10071744
Chicago/Turabian StyleSu, Wei-Yu, I-Hua Chen, Yuh-Ching Gau, Pei-Yu Wu, Jiun-Chi Huang, Yi-Chun Tsai, Szu-Chia Chen, Jer-Ming Chang, Shang-Jyh Hwang, and Hung-Chun Chen. 2022. "Metabolic Syndrome and Obesity-Related Indices Are Associated with Rapid Renal Function Decline in a Large Taiwanese Population Follow-Up Study" Biomedicines 10, no. 7: 1744. https://doi.org/10.3390/biomedicines10071744
APA StyleSu, W.-Y., Chen, I.-H., Gau, Y.-C., Wu, P.-Y., Huang, J.-C., Tsai, Y.-C., Chen, S.-C., Chang, J.-M., Hwang, S.-J., & Chen, H.-C. (2022). Metabolic Syndrome and Obesity-Related Indices Are Associated with Rapid Renal Function Decline in a Large Taiwanese Population Follow-Up Study. Biomedicines, 10(7), 1744. https://doi.org/10.3390/biomedicines10071744







