The Effects of the Exposure of Musculoskeletal Tissue to Extracorporeal Shock Waves
Abstract
1. Introduction
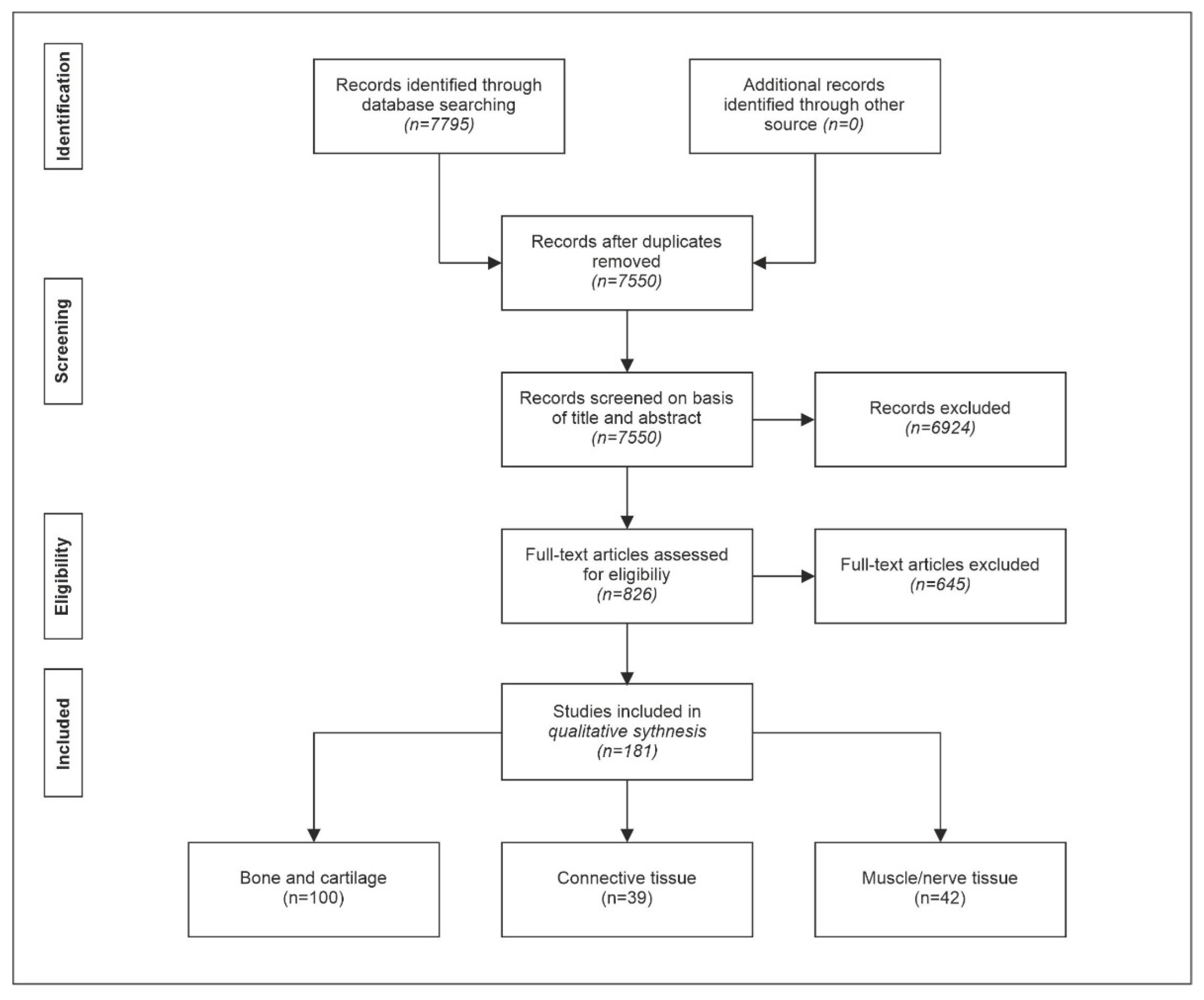
2. Materials and Methods
3. Results
3.1. Effects of the Exposure of Bone and Cartilage Tissue to Extracorporeal Shock Waves
3.2. Effects of Exposure of Connective Tissue to Extracorporeal Shock Waves
3.3. Effects of Exposure of Muscle and Nerve Tissue to Extracorporeal Shock Waves
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jocham, D.; Chaussy, C.; Schmiedt, E. Extracorporeal shock wave lithotripsy. Urol. Int. 1986, 41, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Sauerbruch, T.; Delius, M.; Paumgartner, G.; Holl, J.; Wess, O.; Weber, W.; Hepp, W.; Brendel, W. Fragmentation of gallstones by extracorporeal shock waves. N. Engl. J. Med. 1986, 314, 818–822. [Google Scholar] [CrossRef] [PubMed]
- Sauerbruch, T.; Holl, J.; Sackmann, M.; Werner, R.; Wotzka, R.; Paumgartner, G. Disintegration of a pancreatic duct stone with extracorporeal shock waves in a patient with chronic pancreatitis. Endoscopy 1987, 19, 207–208. [Google Scholar] [CrossRef] [PubMed]
- Sauerbruch, T.; Stern, M. Fragmentation of bile duct stones by extracorporeal shock waves: A new approach to biliary calculi after failure of routine endoscopic measures. Gastroenterology 1989, 96, 146–152. [Google Scholar] [CrossRef]
- Iro, H.; Nitsche, N.; Schneider, H.T.; Ell, C. Extracorporeal shockwave lithotripsy of salivary gland stones. Lancet 1989, 2, 115. [Google Scholar] [CrossRef]
- Graff, J.; Richter, K.D.; Pastor, J. Effect of high energy shock waves on bony tissue. Urol. Res. 1988, 16, 252–258. [Google Scholar]
- Haupt, G.; Haupt, A.; Ekkernkamp, A.; Gerety, B.; Chvapil, M. Influence of shock waves on fracture healing. Urology 1992, 39, 529–532. [Google Scholar] [CrossRef]
- Kertzman, P.; Csaszar, N.B.M.; Furia, J.P.; Schmitz, C. Radial extracorporeal shock wave therapy is efficient and safe in the treatment of fracture nonunions of superficial bones: A retrospective case series. J. Orthop. Surg. Res. 2017, 12, 164. [Google Scholar] [CrossRef]
- Speed, C. A systematic review of shockwave therapies in soft tissue conditions: Focusing on the evidence. Br. J. Sports Med. 2014, 48, 1538–1542. [Google Scholar] [CrossRef]
- Schmitz, C.; Csaszar, N.B.; Milz, S.; Schieker, M.; Maffulli, N.; Rompe, J.D.; Furia, J.P. Efficacy and safety of extracorporeal shock wave therapy for orthopedic conditions: A systematic review on studies listed in the PEDro database. Br. Med. Bull. 2015, 116, 115–138. [Google Scholar] [CrossRef]
- Reilly, J.M.; Bluman, E.; Tenforde, A.S. Effect of shockwave treatment for management of upper and lower extremity musculoskeletal conditions: A narrative review. PM R 2018, 10, 1385–1403. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.P.; Rees, S.; Kalindjian, S.B.; Philpott, K.L. Principles of early drug discovery. Br. J. Pharmacol. 2011, 162, 1239–1249. [Google Scholar] [CrossRef] [PubMed]
- Visco, V.; Vulpiani, M.C.; Torrisi, M.R.; Ferretti, A.; Pavan, A.; Vetrano, M. Experimental studies on the biological effects of extracorporeal shock wave therapy on tendon models. A review of the literature. Muscles Ligaments Tendons J. 2014, 4, 357–361. [Google Scholar] [CrossRef]
- Liu, T.; Shindel, A.W.; Lin, G.; Lue, T.F. Cellular signaling pathways modulated by low-intensity extracorporeal shock wave therapy. Int. J. Impot. Res. 2019, 31, 170–176. [Google Scholar] [CrossRef]
- Auersperg, V.; Trieb, K. Extracorporeal shock wave therapy: An update. EFORT Open. Rev. 2020, 5, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Simplicio, C.L.; Purita, J.; Murrell, W.; Santos, G.S.; Dos Santos, R.G.; Lana, J. Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J. Clin. Orthop. Trauma 2020, 11, S309–S318. [Google Scholar] [CrossRef]
- Rola, P.; Wlodarczak, A.; Barycki, M.; Doroszko, A. Use of the shock wave therapy in basic research and clinical applications-from bench to bedsite. Biomedicines 2022, 10, 568. [Google Scholar] [CrossRef]
- Li, B.; Wang, R.; Huang, X.; Ou, Y.; Jia, Z.; Lin, S.; Zhang, Y.; Xia, H.; Chen, B. Extracorporeal shock wave therapy promotes osteogenic differentiation in a rabbit osteoporosis model. Front. Endocrinol. 2021, 12, 627718. [Google Scholar] [CrossRef]
- Inoue, S.; Hatakeyama, J.; Aoki, H.; Kuroki, H.; Niikura, T.; Oe, K.; Fukui, T.; Kuroda, R.; Akisue, T.; Moriyama, H. Utilization of mechanical stress to treat osteoporosis: The effects of electrical stimulation, radial extracorporeal shock wave, and ultrasound on experimental osteoporosis in ovariectomized rats. Calcif. Tissue Int. 2021, 109, 215–229. [Google Scholar] [CrossRef]
- Inoue, S.; Hatakeyama, J.; Aoki, H.; Kuroki, H.; Niikura, T.; Oe, K.; Fukui, T.; Kuroda, R.; Akisue, T.; Moriyama, H. Effects of ultrasound, radial extracorporeal shock waves, and electrical stimulation on rat bone defect healing. Ann. N. Y. Acad. Sci. 2021, 1497, 3–14. [Google Scholar] [CrossRef]
- Zhao, Z.; Wang, Y.; Wang, Q.; Liang, J.; Hu, W.; Zhao, S.; Li, P.; Zhu, H.; Li, Z. Radial extracorporeal shockwave promotes subchondral bone stem/progenitor cell self-renewal by activating YAP/TAZ and facilitates cartilage repair in vivo. Stem Cell Res. Ther. 2021, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Chijimatsu, R.; Yoshikawa, H.; Yoshida, K. Extracorporeal shock wave therapy accelerates endochondral ossification and fracture healing in a rat femur delayed-union model. Biochem. Biophys. Res. Commun. 2020, 530, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Alshihri, A.; Niu, W.; Kammerer, P.W.; Al-Askar, M.; Yamashita, A.; Kurisawa, M.; Spector, M. The effects of shock wave stimulation of mesenchymal stem cells on proliferation, migration, and differentiation in an injectable gelatin matrix for osteogenic regeneration. J. Tissue Eng. Regen. Med. 2020, 14, 1630–1640. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.L.; Chou, W.Y.; Hsu, C.C.; Ko, J.Y.; Jhan, S.W.; Wang, C.J.; Lee, M.S.; Hsu, T.C.; Cheng, J.H. Shockwave therapy modulates the expression of BMP2 for prevention of bone and cartilage loss in the lower limbs of postmenopausal osteoporosis rat model. Biomedicines 2020, 8, 614. [Google Scholar] [CrossRef] [PubMed]
- Ramesh, S.; Zaman, F.; Madhuri, V.; Savendahl, L. Radial extracorporeal shock wave treatment promotes bone growth and chondrogenesis in cultured fetal rat metatarsal bones. Clin. Orthop. Relat. Res. 2020, 478, 668–678. [Google Scholar] [CrossRef] [PubMed]
- Colbath, A.C.; Kisiday, J.D.; Phillips, J.N.; Goodrich, L.R. Can extracorporeal shockwave promote osteogenesis of equine bone marrow-derived mesenchymal stem cells in vitro? Stem Cells Dev. 2020, 29, 110–118. [Google Scholar] [CrossRef]
- Hashimoto, S.; Ichinose, T.; Ohsawa, T.; Koibuchi, N.; Chikuda, H. Extracorporeal shockwave therapy accelerates the healing of a meniscal tear in the avascular region in a rat model. Am. J. Sports Med. 2019, 47, 2937–2944. [Google Scholar] [CrossRef]
- Senel, E.; Ozkan, E.; Bereket, M.C.; Onger, M.E. The assessment of new bone formation induced by unfocused extracorporeal shock wave therapy applied on pre-surgical phase of distraction osteogenesis. Eur. Oral Res. 2019, 53, 125–131. [Google Scholar] [CrossRef]
- Kim, Y.H.; Bang, J.I.; Son, H.J.; Kim, Y.; Kim, J.H.; Bae, H.; Han, S.J.; Yoon, H.J.; Kim, B.S. Protective effects of extracorporeal shockwave on rat chondrocytes and temporomandibular joint osteoarthritis; preclinical evaluation with in vivo 99m Tc-HDP SPECT and ex vivo micro-CT. Osteoarthr. Cartil. 2019, 27, 1692–1701. [Google Scholar] [CrossRef]
- Buarque de Gusmao, C.V.; Batista, N.A.; Vidotto Lemes, V.T.; Maia Neto, W.L.; de Faria, L.D.; Alves, J.M.; Belangero, W.D. Effect of low-intensity pulsed ultrasound stimulation, extracorporeal shockwaves and radial pressure waves on Akt, BMP-2, ERK-2, FAK and TGF-β1 during bone healing in rat tibial defects. Ultrasound Med. Biol. 2019, 45, 2140–2161. [Google Scholar] [CrossRef]
- Cheng, J.H.; Wang, C.J.; Chou, W.Y.; Hsu, S.L.; Chen, J.H.; Hsu, T.C. Comparison efficacy of ESWT and Wharton’s jelly mesenchymal stem cell in early osteoarthritis of rat knee. Am. J. Transl. Res. 2019, 11, 586–598. [Google Scholar] [PubMed]
- Ginini, J.G.; Emodi, O.; Sabo, E.; Maor, G.; Shilo, D.; Rachmiel, A. Effects of timing of extracorporeal shock wave therapy on mandibular distraction osteogenesis: An experimental study in a rat model. J. Oral Maxillofac. Surg. 2019, 77, 629–638. [Google Scholar] [CrossRef] [PubMed]
- Ginini, J.G.; Maor, G.; Emodi, O.; Shilo, D.; Gabet, Y.; Aizenbud, D.; Rachmiel, A. Effects of extracorporeal shock wave therapy on distraction osteogenesis in rat mandible. Plast. Reconstr. Surg. 2018, 142, 1501–1509. [Google Scholar] [CrossRef] [PubMed]
- Qi, H.; Jin, S.; Yin, C.; Chen, L.; Sun, L.; Liu, Y. Radial extracorporeal shock wave therapy promotes osteochondral regeneration of knee joints in rabbits. Exp. Ther. Med. 2018, 16, 3478–3484. [Google Scholar] [CrossRef] [PubMed]
- Koolen, M.K.E.; Kruyt, M.C.; Zadpoor, A.A.; Oner, F.C.; Weinans, H.; van der Jagt, O.P. Optimization of screw fixation in rat bone with extracorporeal shock waves. J. Orthop. Res. 2018, 36, 76–84. [Google Scholar] [CrossRef]
- Mackert, G.A.; Schulte, M.; Hirche, C.; Kotsougiani, D.; Vogelpohl, J.; Hoener, B.; Fiebig, T.; Kirschner, S.; Brockmann, M.A.; Lehnhardt, M.; et al. Low-energy extracorporeal shockwave therapy (ESWT) improves metaphyseal fracture healing in an osteoporotic rat model. PLoS ONE 2017, 12, e0189356. [Google Scholar] [CrossRef]
- Tan, L.; Zhao, B.; Ge, F.T.; Sun, D.H.; Yu, T. Shockwaves inhibit chondrogenic differentiation of human mesenchymal stem cells in association with adenosine and A2B receptors. Sci. Rep. 2017, 7, 14377. [Google Scholar] [CrossRef]
- Hsu, S.L.; Cheng, J.H.; Wang, C.J.; Ko, J.Y.; Hsu, C.H. Extracorporeal shockwave therapy enhances expression of Pdia-3 which is a key factor of the 1alpha,25-dihydroxyvitamin D 3 rapid membrane signaling pathway in treatment of early osteoarthritis of the knee. Int. J. Med. Sci. 2017, 14, 1220–1230. [Google Scholar] [CrossRef]
- Yilmaz, V.; Karadas, O.; Dandinoglu, T.; Umay, E.; Cakci, A.; Tan, A.K. Efficacy of extracorporeal shockwave therapy and low-intensity pulsed ultrasound in a rat knee osteoarthritis model: A randomized controlled trial. Eur. J. Rheumatol. 2017, 4, 104–108. [Google Scholar] [CrossRef]
- Wang, C.J.; Cheng, J.H.; Huang, C.Y.; Hsu, S.L.; Lee, F.Y.; Yip, H.K. Medial tibial subchondral bone is the key target for extracorporeal shockwave therapy in early osteoarthritis of the knee. Am. J. Transl. Res. 2017, 9, 1720–1731. [Google Scholar]
- Chen, Y.; Xu, J.; Huang, Z.; Yu, M.; Zhang, Y.; Chen, H.; Ma, Z.; Liao, H.; Hu, J. An innovative approach for enhancing bone defect healing using PLGA scaffolds seeded with extracorporeal-shock-wave-treated bone marrow mesenchymal stem cells (BMSCs). Sci. Rep. 2017, 7, 44130. [Google Scholar] [CrossRef] [PubMed]
- Onger, M.E.; Bereket, C.; Sener, I.; Ozkan, N.; Senel, E.; Polat, A.V. Is it possible to change of the duration of consolidation period in the distraction osteogenesis with the repetition of extracorporeal shock waves? Med. Oral. Patol. Oral. Cir. Bucal 2017, 22, e251–e257. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, C.J.; Cheng, J.H.; Chou, W.Y.; Hsu, S.L.; Chen, J.H.; Huang, C.Y. Changes of articular cartilage and subchondral bone after extracorporeal shockwave therapy in osteoarthritis of the knee. Int. J. Med. Sci. 2017, 14, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Lama, A.; Santoro, A.; Corrado, B.; Pirozzi, C.; Paciello, O.; Pagano, T.B.; Russo, S.; Calignano, A.; Mattace Raso, G.; Meli, R. Extracorporeal shock waves alone or combined with raloxifene promote bone formation and suppress resorption in ovariectomized rats. PLoS ONE 2017, 12, e0171276. [Google Scholar]
- Catalano, M.G.; Marano, F.; Rinella, L.; de Girolamo, L.; Bosco, O.; Fortunati, N.; Berta, L.; Frairia, R. Extracorporeal shockwaves (ESWs) enhance the osteogenic medium-induced differentiation of adipose-derived stem cells into osteoblast-like cells. J. Tissue Eng. Regen. Med. 2017, 11, 390–399. [Google Scholar] [CrossRef]
- Ma, H.Z.; Zhou, D.S.; Li, D.; Zhang, W.; Zeng, B.F. A histomorphometric study of necrotic femoral head in rabbits treated with extracorporeal shock waves. J. Phys. Ther. Sci. 2017, 29, 24–28. [Google Scholar] [CrossRef][Green Version]
- Huang, H.M.; Li, X.L.; Tu, S.Q.; Chen, X.F.; Lu, C.C.; Jiang, L.H. Effects of roughly focused extracorporeal shock waves therapy on the expressions of bone morphogenetic protein-2 and osteoprotegerin in osteoporotic fracture in rats. Chin. Med. J. 2016, 129, 2567–2575. [Google Scholar] [CrossRef]
- Notarnicola, A.; Vicenti, G.; Maccagnano, G.; Silvestris, F.; Cafforio, P.; Moretti, B. Extracorporeal shock waves induce osteogenic differentiation of human bone-marrow stromal cells. J. Biol. Regul. Homeost. Agents 2016, 30, 139–144. [Google Scholar]
- Zhai, L.; Sun, N.; Zhang, B.; Liu, S.T.; Zhao, Z.; Jin, H.C.; Ma, X.L.; Xing, G.Y. Effects of focused extracorporeal shock waves on bone marrow mesenchymal stem cells in patients with avascular necrosis of the femoral head. Ultrasound Med. Biol. 2016, 42, 753–762. [Google Scholar] [CrossRef]
- Dias dos Santos, P.R.; De Medeiros, V.P.; Freire Martins de Moura, J.P.; da Silveira Franciozi, C.E.; Nader, H.B.; Faloppa, F. Effects of shock wave therapy on glycosaminoglycan expression during bone healing. Int. J. Surg. 2015, 24, 120–123. [Google Scholar] [CrossRef]
- Wang, C.J.; Huang, C.Y.; Hsu, S.L.; Chen, J.H.; Cheng, J.H. Extracorporeal shockwave therapy in osteoporotic osteoarthritis of the knee in rats: An experiment in animals. Arthritis Res. Ther. 2014, 16, R139. [Google Scholar] [CrossRef] [PubMed]
- Muzio, G.; Martinasso, G.; Baino, F.; Frairia, R.; Vitale-Brovarone, C.; Canuto, R.A. Key role of the expression of bone morphogenetic proteins in increasing the osteogenic activity of osteoblast-like cells exposed to shock waves and seeded on bioactive glass-ceramic scaffolds for bone tissue engineering. J. Biomater. Appl. 2014, 29, 728–736. [Google Scholar] [CrossRef] [PubMed]
- Oktas, B.; Orhan, Z.; Erbil, B.; Degirmenci, E.; Ustundag, N. Effect of extracorporeal shock wave therapy on fracture healing in rat femural fractures with intact and excised periosteum. Eklem Hastalik. Cerrahisi 2014, 25, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Junger, W.G.; Yuan, C.; Zhang, W.; Bao, Y.; Qin, D.; Wang, C.; Tan, L.; Qi, B.; Zhu, D.; et al. Shockwaves induce osteogenic differentiation of human mesenchymal stem cells through atp release and activation of P2X7 receptors. Stem Cells 2013, 31, 1170–1180. [Google Scholar] [CrossRef] [PubMed]
- Suhr, F.; Delhasse, Y.; Bungartz, G.; Schmidt, A.; Pfannkuche, K.; Bloch, W. Cell biological effects of mechanical stimulations generated by focused extracorporeal shock wave applications on cultured human bone marrow stromal cells. Stem Cell Res. 2013, 11, 951–964. [Google Scholar] [CrossRef]
- Lyon, R.; Liu, X.C.; Kubin, M.; Schwab, J. Does extracorporeal shock wave therapy enhance healing of osteochondritis dissecans of the rabbit knee?: A pilot study. Clin. Orthop. Relat. Res. 2013, 471, 1159–1165. [Google Scholar] [CrossRef][Green Version]
- Wang, C.J.; Sun, Y.C.; Siu, K.K.; Wu, C.T. Extracorporeal shockwave therapy shows site-specific effects in osteoarthritis of the knee in rats. J. Surg. Res. 2013, 183, 612–619. [Google Scholar] [CrossRef]
- Wang, C.J.; Hsu, S.L.; Weng, L.H.; Sun, Y.C.; Wang, F.S. Extracorporeal shockwave therapy shows a number of treatment related chondroprotective effect in osteoarthritis of the knee in rats. BMC Musculoskelet. Disord. 2013, 14, 44. [Google Scholar] [CrossRef]
- van der Jagt, O.P.; Waarsing, J.H.; Kops, N.; Schaden, W.; Jahr, H.; Verhaar, J.A.; Weinans, H. Unfocused extracorporeal shock waves induce anabolic effects in osteoporotic rats. J. Orthop. Res. 2013, 31, 768–775. [Google Scholar] [CrossRef]
- Oztemur, Z.; Ozturk, H.; Ozyurek, S.; Kaloglu, C.; Golge, U.H.; Bulut, O. The long-term effects of extracorporeal shock waves on the epiphysis of the adolescent rat. J. Orthop. Sci. 2013, 18, 159–164. [Google Scholar] [CrossRef]
- Gollwitzer, H.; Gloeck, T.; Roessner, M.; Langer, R.; Horn, C.; Gerdesmeyer, L.; Diehl, P. Radial extracorporeal shock wave therapy (reswt) induces new bone formation in vivo: Results of an animal study in rabbits. Ultrasound Med. Biol. 2013, 39, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Altuntas, E.E.; Oztemur, Z.; Ozer, H.; Muderris, S. Effect of extracorporeal shock waves on subcondylar mandibular fractures. J. Craniofac. Surg. 2012, 23, 1645–1648. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Tamma, R.; Moretti, L.; Fiore, A.; Vicenti, G.; Zallone, A.; Moretti, B. Effects of radial shock waves therapy on osteoblasts activities. Musculoskelet. Surg. 2012, 96, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Ji, H.; Jing, R.; Liu, C.; Wang, M.; Zhai, L.; Bai, X.; Xing, G. Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Arch. Orthop. Trauma Surg. 2012, 132, 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Kearney, C.J.; Hsu, H.P.; Spector, M. The use of extracorporeal shock wave-stimulated periosteal cells for orthotopic bone generation. Tissue Eng. Part A 2012, 18, 1500–1508. [Google Scholar] [CrossRef]
- Xu, J.K.; Chen, H.J.; Li, X.D.; Huang, Z.L.; Xu, H.; Yang, H.L.; Hu, J. Optimal intensity shock wave promotes the adhesion and migration of rat osteoblasts via integrin beta1-mediated expression of phosphorylated focal adhesion kinase. J. Biol. Chem. 2012, 287, 26200–26212. [Google Scholar] [CrossRef]
- Wang, C.J.; Sun, Y.C.; Wong, T.; Hsu, S.L.; Chou, W.Y.; Chang, H.W. Extracorporeal shockwave therapy shows time-dependent chondroprotective effects in osteoarthritis of the knee in rats. J. Surg. Res. 2012, 178, 196–205. [Google Scholar] [CrossRef]
- Erturk, C.; Altay, M.A.; Ozardali, I.; Altay, N.; Cece, H.; Isikan, U.E. The effect of extracorporeal shockwaves on cartilage end-plates in rabbits: A preliminary mri and histopathological study. Acta Orthop. Traumatol. Turc. 2012, 46, 449–454. [Google Scholar] [CrossRef]
- Wang, C.J.; Weng, L.H.; Ko, J.Y.; Wang, J.W.; Chen, J.M.; Sun, Y.C.; Yang, Y.J. Extracorporeal shockwave shows regression of osteoarthritis of the knee in rats. J. Surg. Res. 2011, 171, 601–608. [Google Scholar] [CrossRef]
- van der Jagt, O.P.; Piscaer, T.M.; Schaden, W.; Li, J.; Kops, N.; Jahr, H.; van der Linden, J.C.; Waarsing, J.H.; Verhaar, J.A.; de Jong, M.; et al. Unfocused extracorporeal shock waves induce anabolic effects in rat bone. J. Bone Jt. Surg. Am. 2011, 93, 38–48. [Google Scholar] [CrossRef]
- Notarnicola, A.; Tamma, R.; Moretti, L.; Panella, A.; Dell’endice, S.; Zallone, A.; Moretti, B. Effect of shock wave treatment on platelet-rich plasma added to osteoblast cultures. Ultrasound Med. Biol. 2011, 37, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Hausdorf, J.; Sievers, B.; Schmitt-Sody, M.; Jansson, V.; Maier, M.; Mayer-Wagner, S. Stimulation of bone growth factor synthesis in human osteoblasts and fibroblasts after extracorporeal shock wave application. Arch. Orthop. Trauma Surg. 2011, 131, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Huang, K.E.; Sun, Y.C.; Yang, Y.J.; Ko, J.Y.; Weng, L.H.; Wang, F.S. VEGF modulates angiogenesis and osteogenesis in shockwave-promoted fracture healing in rabbits. J. Surg. Res. 2011, 171, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Mayer-Wagner, S.; Ernst, J.; Maier, M.; Chiquet, M.; Joos, H.; Muller, P.E.; Jansson, V.; Sievers, B.; Hausdorf, J. The effect of high-energy extracorporeal shock waves on hyaline cartilage of adult rats in vivo. J. Orthop. Res. 2010, 28, 1050–1056. [Google Scholar] [CrossRef]
- Muzio, G.; Verne, E.; Canuto, R.A.; Martinasso, G.; Saracino, S.; Baino, F.; Miola, M.; Berta, L.; Frairia, R.; Vitale-Brovarone, C. Shock waves induce activity of human osteoblast-like cells in bioactive scaffolds. J. Trauma 2010, 68, 1439–1444. [Google Scholar] [CrossRef]
- Lai, J.P.; Wang, F.S.; Hung, C.M.; Wang, C.J.; Huang, C.J.; Kuo, Y.R. Extracorporeal shock wave accelerates consolidation in distraction osteogenesis of the rat mandible. J. Trauma 2010, 69, 1252–1258. [Google Scholar] [CrossRef]
- Qin, L.; Wang, L.; Wong, M.W.; Wen, C.; Wang, G.; Zhang, G.; Chan, K.M.; Cheung, W.H.; Leung, K.S. Osteogenesis induced by extracorporeal shockwave in treatment of delayed osteotendinous junction healing. J. Orthop. Res. 2010, 28, 70–76. [Google Scholar] [CrossRef]
- van der Jagt, O.P.; van der Linden, J.C.; Schaden, W.; van Schie, H.T.; Piscaer, T.M.; Verhaar, J.A.; Weinans, H.; Waarsing, J.H. Unfocused extracorporeal shock wave therapy as potential treatment for osteoporosis. J. Orthop. Res. 2009, 27, 1528–1533. [Google Scholar] [CrossRef]
- Iannone, F.; Moretti, B.; Notarnicola, A.; Moretti, L.; Patella, S.; Patella, V.; Lapadula, G. Extracorporeal shock waves increase interleukin-10 expression by human osteoarthritic and healthy osteoblasts in vitro. Clin. Exp. Rheumatol. 2009, 27, 794–799. [Google Scholar]
- Tamma, R.; dell’Endice, S.; Notarnicola, A.; Moretti, L.; Patella, S.; Patella, V.; Zallone, A.; Moretti, B. Extracorporeal shock waves stimulate osteoblast activities. Ultrasound Med. Biol. 2009, 35, 2093–2100. [Google Scholar] [CrossRef]
- Lee, T.C.; Yang, Y.L.; Chang, N.K.; Lin, T.S.; Lin, W.C.; Liu, Y.S.; Wang, C.J. Biomechanical testing of spinal fusion segments enhanced by extracorporeal shock wave treatment in rabbits. Chang Gung Med. J. 2009, 32, 276–282. [Google Scholar] [PubMed]
- Tam, K.F.; Cheung, W.H.; Lee, K.M.; Qin, L.; Leung, K.S. Shockwave exerts osteogenic effect on osteoporotic bone in an ovariectomized goat model. Ultrasound Med. Biol. 2009, 35, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, A.; Ritz, U.; Hessmann, M.H.; Alini, M.; Rommens, P.M.; Rompe, J.D. Extracorporeal shock wave-mediated changes in proliferation, differentiation, and gene expression of human osteoblasts. J. Trauma 2008, 65, 1402–1410. [Google Scholar] [CrossRef] [PubMed]
- Tam, K.F.; Cheung, W.H.; Lee, K.M.; Qin, L.; Leung, K.S. Osteogenic effects of low-intensity pulsed ultrasound, extracorporeal shockwaves and their combination-an in vitro comparative study on human periosteal cells. Ultrasound Med. Biol. 2008, 34, 1957–1965. [Google Scholar] [CrossRef]
- Lee, T.C.; Huang, H.Y.; Yang, Y.L.; Hung, K.S.; Cheng, C.H.; Lin, W.C.; Wang, C.J. Application of extracorporeal shock wave treatment to enhance spinal fusion: A rabbit experiment. Surg. Neurol. 2008, 70, 129–134. [Google Scholar] [CrossRef]
- Wang, C.J.; Wang, F.S.; Yang, K.D. Biological effects of extracorporeal shockwave in bone healing: A study in rabbits. Arch. Orthop. Trauma Surg. 2008, 128, 879–884. [Google Scholar] [CrossRef]
- Moretti, B.; Iannone, F.; Notarnicola, A.; Lapadula, G.; Moretti, L.; Patella, V.; Garofalo, R. Extracorporeal shock waves down-regulate the expression of interleukin-10 and tumor necrosis factor-alpha in osteoarthritic chondrocytes. BMC Musculoskelet. Disord. 2008, 9, 16. [Google Scholar] [CrossRef]
- Tischer, T.; Milz, S.; Weiler, C.; Pautke, C.; Hausdorf, J.; Schmitz, C.; Maier, M. Dose-dependent new bone formation by extracorporeal shock wave application on the intact femur of rabbits. Eur. Surg. Res. 2008, 41, 44–53. [Google Scholar] [CrossRef]
- Ozturk, H.; Bulut, O.; Oztemur, Z.; Kaloglu, C.; Kol, I.O. Effect of high-energy extracorporeal shock waves on the immature epiphysis in a rabbit model. Arch. Orthop. Trauma Surg. 2008, 128, 627–631. [Google Scholar] [CrossRef]
- Ma, H.Z.; Zeng, B.F.; Li, X.L. Upregulation of VEGF in subchondral bone of necrotic femoral heads in rabbits with use of extracorporeal shock waves. Calcif. Tissue Int. 2007, 81, 124–131. [Google Scholar] [CrossRef]
- Murata, R.; Nakagawa, K.; Ohtori, S.; Ochiai, N.; Arai, M.; Saisu, T.; Sasho, T.; Takahashi, K.; Moriya, H. The effects of radial shock waves on gene transfer in rabbit chondrocytes in vitro. Osteoarthr. Cartil. 2007, 15, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Benson, B.M.; Byron, C.R.; Pondenis, H.; Stewart, A.A. The effects of radial shock waves on the metabolism of equine cartilage explants in vitro. N. Z. Vet. J. 2007, 55, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Martini, L.; Giavaresi, G.; Fini, M.; Borsari, V.; Torricelli, P.; Giardino, R. Early effects of extracorporeal shock wave treatment on osteoblast-like cells: A comparative study between electromagnetic and electrohydraulic devices. J. Trauma 2006, 61, 1198–1206. [Google Scholar] [CrossRef] [PubMed]
- Bulut, O.; Eroglu, M.; Ozturk, H.; Tezeren, G.; Bulut, S.; Koptagel, E. Extracorporeal shock wave treatment for defective nonunion of the radius: A rabbit model. J. Orthop. Surg. 2006, 14, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Martini, L.; Giavaresi, G.; Fini, M.; Torricelli, P.; Borsari, V.; Giardino, R.; De Pretto, M.; Remondini, D.; Castellani, G.C. Shock wave therapy as an innovative technology in skeletal disorders: Study on transmembrane current in stimulated osteoblast-like cells. Int. J. Artif. Organs 2005, 28, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Saisu, T.; Kamegaya, M.; Wada, Y.; Takahashi, K.; Mitsuhashi, S.; Moriya, H.; Maier, M. Acetabular augmentation induced by extracorporeal shock waves in rabbits. J. Pediatr. Orthop. B 2005, 14, 162–167. [Google Scholar] [CrossRef]
- Chen, Y.J.; Wurtz, T.; Wang, C.J.; Kuo, Y.R.; Yang, K.D.; Huang, H.C.; Wang, F.S. Recruitment of mesenchymal stem cells and expression of TGF-beta 1 and VEGF in the early stage of shock wave-promoted bone regeneration of segmental defect in rats. J. Orthop. Res. 2004, 22, 526–534. [Google Scholar] [CrossRef]
- Saisu, T.; Takahashi, K.; Kamegaya, M.; Mitsuhashi, S.; Wada, Y.; Moriya, H. Effects of extracorporeal shock waves on immature rabbit femurs. J. Pediatr. Orthop. B 2004, 13, 176–183. [Google Scholar]
- Chen, Y.J.; Kuo, Y.R.; Yang, K.D.; Wang, C.J.; Sheen Chen, S.M.; Huang, H.C.; Yang, Y.J.; Yi-Chih, S.; Wang, F.S. Activation of extracellular signal-regulated kinase (ERK) and p38 kinase in shock wave-promoted bone formation of segmental defect in rats. Bone 2004, 34, 466–477. [Google Scholar] [CrossRef]
- Pauwels, F.E.; McClure, S.R.; Amin, V.; Van Sickle, D.; Evans, R.B. Effects of extracorporeal shock wave therapy and radial pressure wave therapy on elasticity and microstructure of equine cortical bone. Am. J. Vet. Res. 2004, 65, 207–212. [Google Scholar] [CrossRef]
- Wang, F.S.; Yang, K.D.; Wang, C.J.; Huang, H.C.; Chio, C.C.; Hsu, T.Y.; Ou, C.Y. Shockwave stimulates oxygen radical-mediated osteogenesis of the mesenchymal cells from human umbilical cord blood. J. Bone Miner. Res. 2004, 19, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Da Costa Gomez, T.M.; Radtke, C.L.; Kalscheur, V.L.; Swain, C.A.; Scollay, M.C.; Edwards, R.B.; Santschi, E.M.; Markel, M.D.; Muir, P. Effect of focused and radial extracorporeal shock wave therapy on equine bone microdamage. Vet. Surg. 2004, 33, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Yamazaki, M.; Saisu, T.; Nakajima, A.; Shimizu, S.; Mitsuhashi, S.; Moriya, H. Gene expression for extracellular matrix proteins in shockwave-induced osteogenesis in rats. Calcif. Tissue Int. 2004, 74, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Kuo, Y.R.; Yang, K.D.; Wang, C.J.; Huang, H.C.; Wang, F.S. Shock wave application enhances pertussis toxin protein-sensitive bone formation of segmental femoral defect in rats. J. Bone Miner. Res. 2003, 18, 2169–2179. [Google Scholar] [CrossRef]
- Martini, L.; Fini, M.; Giavaresi, G.; Torricelli, P.; de Pretto, M.; Rimondini, L.; Giardino, R. Primary osteoblasts response to shock wave therapy using different parameters. Artif. Cells Blood Substit. Immobil. Biotechnol. 2003, 31, 449–466. [Google Scholar] [CrossRef]
- Martini, L.; Giavaresi, G.; Fini, M.; Torricelli, P.; de Pretto, M.; Schaden, W.; Giardino, R. Effect of extracorporeal shock wave therapy on osteoblastlike cells. Clin. Orthop. Relat. Res. 2003, 413, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Dorotka, R.; Kubista, B.; Schatz, K.D.; Trieb, K. Effects of extracorporeal shock waves on human articular chondrocytes and ovine bone marrow stromal cells in vitro. Arch. Orthop. Trauma Surg. 2003, 123, 345–348. [Google Scholar] [CrossRef]
- Wang, F.S.; Yang, K.D.; Kuo, Y.R.; Wang, C.J.; Sheen-Chen, S.M.; Huang, H.C.; Chen, Y.J. Temporal and spatial expression of bone morphogenetic proteins in extracorporeal shock wave-promoted healing of segmental defect. Bone 2003, 32, 387–396. [Google Scholar] [CrossRef]
- Maier, M.; Milz, S.; Tischer, T.; Munzing, W.; Manthey, N.; Stabler, A.; Holzknecht, N.; Weiler, C.; Nerlich, A.; Refior, H.J.; et al. Influence of extracorporeal shock-wave application on normal bone in an animal model in vivo. Scintigraphy, MRI and histopathology. J. Bone Jt. Surg. Br. 2002, 84, 592–599. [Google Scholar] [CrossRef]
- Wang, F.S.; Yang, K.D.; Chen, R.F.; Wang, C.J.; Sheen-Chen, S.M. Extracorporeal shock wave promotes growth and differentiation of bone-marrow stromal cells towards osteoprogenitors associated with induction of TGF-beta1. J. Bone Jt. Surg. Br. 2002, 84, 457–461. [Google Scholar] [CrossRef]
- Wang, F.S.; Wang, C.J.; Huang, H.J.; Chung, H.; Chen, R.F.; Yang, K.D. Physical shock wave mediates membrane hyperpolarization and Ras activation for osteogenesis in human bone marrow stromal cells. Biochem. Biophys. Res. Commun. 2001, 287, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Huang, H.Y.; Chen, H.H.; Pai, C.H.; Yang, K.D. Effect of shock wave therapy on acute fractures of the tibia: A study in a dog model. Clin. Orthop. Relat. Res. 2001, 387, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Vaterlein, N.; Lussenhop, S.; Hahn, M.; Delling, G.; Meiss, A.L. The effect of extracorporeal shock waves on joint cartilage--an in vivo study in rabbits. Arch. Orthop. Trauma Surg. 2000, 120, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Peters, N.; Dahmen, G.; Schmidt, W.; Stein, F. Über die Auswirkungen von extrakorporalen Ultraschall-Stossenwellen auf weitentwickelte Embryonen des Knochenfisches Oryzias latipes [Effects of extracorporeal ultrasound shockwaves on the relatively mature embryos of the teleost oryzias latipes]. Ultraschall Med. 1998, 19, 52–58. (In German) [Google Scholar] [CrossRef] [PubMed]
- Augat, P.; Claes, L.; Suger, G. In vivo effect of shock-waves on the healing of fractured bone. Clin. Biomech. 1995, 10, 374–378. [Google Scholar] [CrossRef]
- Forriol, F.; Solchaga, L.; Moreno, J.L.; Canadell, J. The effect of shockwaves on mature and healing cortical bone. Int. Orthop. 1994, 18, 325–329. [Google Scholar] [CrossRef][Green Version]
- Haberal, B.; Simsek, E.K.; Akpinar, K.; Turkbey Simsek, D.; Sahinturk, F. Impact of radial extracorporeal shock wave therapy in post-laminectomy epidural fibrosis in a rat model. Jt. Dis. Relat. Surg. 2021, 32, 162–169. [Google Scholar] [CrossRef]
- Heimes, D.; Wiesmann, N.; Eckrich, J.; Brieger, J.; Mattyasovszky, S.; Proff, P.; Weber, M.; Deschner, J.; Al-Nawas, B.; Kammerer, P.W. In vivo modulation of angiogenesis and immune response on a collagen matrix via extracorporeal shockwaves. Int. J. Mol. Sci. 2020, 21, 7574. [Google Scholar] [CrossRef]
- Lu, C.C.; Chou, S.H.; Shen, P.C.; Chou, P.H.; Ho, M.L.; Tien, Y.C. Extracorporeal shock wave promotes activation of anterior cruciate ligament remnant cells and their paracrine regulation of bone marrow stromal cells’ proliferation, migration, collagen synthesis, and differentiation. Bone Jt. Res. 2020, 9, 458–468. [Google Scholar] [CrossRef]
- Basoli, V.; Chaudary, S.; Cruciani, S.; Santaniello, S.; Balzano, F.; Ventura, C.; Redl, H.; Dungel, P.; Maioli, M. Mechanical stimulation of fibroblasts by extracorporeal shock waves: Modulation of cell activation and proliferation through a transient proinflammatory milieu. Cell Transplant. 2020, 29, 963689720916175. [Google Scholar] [CrossRef]
- Schnurrer-Luke-Vrbanic, T.; Avancini-Dobrovic, V.; Sosa, I.; Cvijanovic, O.; Bobinac, D. VEGF-A expression in soft tissues repaired by shockwave therapy: Differences between modalities. J. Biol. Regul. Homeost. Agents 2018, 32, 583–588. [Google Scholar] [PubMed]
- Cui, H.S.; Hong, A.R.; Kim, J.B.; Yu, J.H.; Cho, Y.S.; Joo, S.Y.; Seo, C.H. Extracorporeal shock wave therapy alters the expression of fibrosis-related molecules in fibroblast derived from human hypertrophic scar. Int. J. Mol. Sci. 2018, 19, 124. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Falkensammer, F.; Andrukhov, O.; Chen, J.; Mittermayr, R.; Rausch-Fan, X. Effects of shock waves on expression of IL-6, IL-8, MCP-1, and TNF-alpha expression by human periodontal ligament fibroblasts: An in vitro study. Med. Sci. Monit. 2016, 22, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Hochstrasser, T.; Frank, H.G.; Schmitz, C. Dose-dependent and cell type-specific cell death and proliferation following in vitro exposure to radial extracorporeal shock waves. Sci. Rep. 2016, 6, 30637. [Google Scholar] [CrossRef]
- Leone, L.; Raffa, S.; Vetrano, M.; Ranieri, D.; Malisan, F.; Scrofani, C.; Vulpiani, M.C.; Ferretti, A.; Torrisi, M.R.; Visco, V. Extracorporeal shock wave treatment (ESWT) enhances the in vitro-induced differentiation of human tendon-derived stem/progenitor cells (hTSPCs). Oncotarget 2016, 7, 6410–6423. [Google Scholar] [CrossRef]
- Kisch, T.; Sorg, H.; Forstmeier, V.; Knobloch, K.; Liodaki, E.; Stang, F.; Mailander, P.; Kramer, R. Remote effects of extracorporeal shock wave therapy on cutaneous microcirculation. J. Tissue Viability 2015, 24, 140–145. [Google Scholar] [CrossRef]
- Waugh, C.M.; Morrissey, D.; Jones, E.; Riley, G.P.; Langberg, H.; Screen, H.R. In vivo biological response to extracorporeal shockwave therapy in human tendinopathy. Eur. Cell Mater. 2015, 29, 268–280. [Google Scholar] [CrossRef]
- de Girolamo, L.; Stanco, D.; Galliera, E.; Vigano, M.; Lovati, A.B.; Marazzi, M.G.; Romeo, P.; Sansone, V. Soft-focused extracorporeal shock waves increase the expression of tendon-specific markers and the release of anti-inflammatory cytokines in an adherent culture model of primary human tendon cells. Ultrasound. Med. Biol. 2014, 40, 1204–1215. [Google Scholar] [CrossRef]
- Chow, D.H.; Suen, P.K.; Huang, L.; Cheung, W.H.; Leung, K.S.; Ng, C.; Shi, S.Q.; Wong, M.W.; Qin, L. Extracorporeal shockwave enhanced regeneration of fibrocartilage in a delayed tendon-bone insertion repair model. J. Orthop. Res. 2014, 32, 507–514. [Google Scholar] [CrossRef]
- Cinar, B.M.; Circi, E.; Balcik, C.; Guven, G.; Akpinar, S.; Derincek, A. The effects of extracorporeal shock waves on carrageenan-induced achilles tendinitis in rats: A biomechanical and histological analysis. Acta Orthop. Traumatol. Turc. 2013, 47, 266–272. [Google Scholar] [CrossRef]
- Contaldo, C.; Hogger, D.C.; Khorrami Borozadi, M.; Stotz, M.; Platz, U.; Forster, N.; Lindenblatt, N.; Giovanoli, P. Radial pressure waves mediate apoptosis and functional angiogenesis during wound repair in apoe deficient mice. Microvasc. Res. 2012, 84, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Chow, D.H.; Suen, P.K.; Fu, L.H.; Cheung, W.H.; Leung, K.S.; Wong, M.W.; Qin, L. Extracorporeal shockwave therapy for treatment of delayed tendon-bone insertion healing in a rabbit model: A dose-response study. Am. J. Sports Med. 2012, 40, 2862–2871. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.D.; Choi, S.; Lee, G.J.; Chon, J.; Jeong, Y.S.; Park, H.K.; Kim, H.S. Effects of extracorporeal shockwave therapy on nanostructural and biomechanical responses in the collagenase-induced achilles tendinitis animal model. Lasers Med. Sci. 2012, 27, 1195–1204. [Google Scholar] [CrossRef] [PubMed]
- Leone, L.; Vetrano, M.; Ranieri, D.; Raffa, S.; Vulpiani, M.C.; Ferretti, A.; Torrisi, M.R.; Visco, V. Extracorporeal shock wave treatment (ESWT) improves in vitro functional activities of ruptured human tendon-derived tenocytes. PLoS ONE 2012, 7, e49759. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Kearney, C.J.; Cheriyan, T.; Schmid, T.M.; Spector, M. Extracorporeal shockwave-induced expression of lubricin in tendons and septa. Cell Tissue Res. 2011, 346, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Penteado, F.T.; Faloppa, F.; Giusti, G.; Moraes, V.Y.; Belloti, J.C.; Santos, J.B. High-energy extracorporeal shockwave therapy in a patellar tendon animal model: A vascularization focused study. Clinics 2011, 66, 1611–1614. [Google Scholar] [CrossRef]
- Kubo, M.; Li, T.S.; Kamota, T.; Ohshima, M.; Shirasawa, B.; Hamano, K. Extracorporeal shock wave therapy ameliorates secondary lymphedema by promoting lymphangiogenesis. J. Vasc. Surg. 2010, 52, 429–434. [Google Scholar] [CrossRef]
- Sugioka, K.; Nakagawa, K.; Murata, R.; Ochiai, N.; Sasho, T.; Arai, M.; Tsuruoka, H.; Ohtori, S.; Saisu, T.; Gemba, T.; et al. Radial shock waves effectively introduced NF-kappa b decoy into rat achilles tendon cells in vitro. J. Orthop. Res. 2010, 28, 1078–1083. [Google Scholar] [CrossRef]
- Berta, L.; Fazzari, A.; Ficco, A.M.; Enrica, P.M.; Catalano, M.G.; Frairia, R. Extracorporeal shock waves enhance normal fibroblast proliferation in vitro and activate mRNA expression for TGF-beta1 and for collagen types I and III. Acta Orthop. 2009, 80, 612–617. [Google Scholar] [CrossRef]
- Bosch, G.; de Mos, M.; van Binsbergen, R.; van Schie, H.T.; van de Lest, C.H.; van Weeren, P.R. The effect of focused extracorporeal shock wave therapy on collagen matrix and gene expression in normal tendons and ligaments. Equine Vet. J. 2009, 41, 335–341. [Google Scholar] [CrossRef]
- Han, S.H.; Lee, J.W.; Guyton, G.P.; Parks, B.G.; Courneya, J.P.; Schon, L.C.J. Leonard Goldner award 2008. Effect of extracorporeal shock wave therapy on cultured tenocytes. Foot Ankle Int. 2009, 30, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Byron, C.; Stewart, A.; Benson, B.; Tennent-Brown, B.; Foreman, J. Effects of radial extracorporeal shock wave therapy on radiographic and scintigraphic outcomes in horses with palmar heel pain. Vet. Comp. Orthop. Traumatol. 2009, 22, 113–118. [Google Scholar] [PubMed]
- Chao, Y.H.; Tsuang, Y.H.; Sun, J.S.; Chen, L.T.; Chiang, Y.F.; Wang, C.C.; Chen, M.H. Effects of shock waves on tenocyte proliferation and extracellular matrix metabolism. Ultrasound Med. Biol. 2008, 34, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Qin, L.; Lu, H.B.; Cheung, W.H.; Yang, H.; Wong, W.N.; Chan, K.M.; Leung, K.S. Extracorporeal shock wave therapy in treatment of delayed bone-tendon healing. Am. J. Sports Med. 2008, 36, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Bosch, G.; Lin, Y.L.; van Schie, H.T.; van De Lest, C.H.; Barneveld, A.; van Weeren, P.R. Effect of extracorporeal shock wave therapy on the biochemical composition and metabolic activity of tenocytes in normal tendinous structures in ponies. Equine Vet. J. 2007, 39, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Kersh, K.D.; McClure, S.R.; Van Sickle, D.; Evans, R.B. The evaluation of extracorporeal shock wave therapy on collagenase induced superficial digital flexor tendonitis. Vet. Comp. Orthop. Traumatol. 2006, 19, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Wang, F.S.; Yang, K.D.; Weng, L.H.; Sun, Y.C.; Yang, Y.J. The effect of shock wave treatment at the tendon-bone interface-an histomorphological and biomechanical study in rabbits. J. Orthop. Res. 2005, 23, 274–280. [Google Scholar] [CrossRef]
- Chen, Y.J.; Wang, C.J.; Yang, K.D.; Kuo, Y.R.; Huang, H.C.; Huang, Y.T.; Sun, Y.C.; Wang, F.S. Extracorporeal shock waves promote healing of collagenase-induced achilles tendinitis and increase TGF-beta1 and IGF-I expression. J. Orthop. Res. 2004, 22, 854–861. [Google Scholar] [CrossRef]
- Orhan, Z.; Ozturan, K.; Guven, A.; Cam, K. The effect of extracorporeal shock waves on a rat model of injury to tendo achillis. A histological and biomechanical study. J. Bone Jt. Surg. Br. 2004, 86, 613–618. [Google Scholar] [CrossRef][Green Version]
- Hsu, R.W.W.; Hsu, W.H.; Tai, C.L.; Lee, K.F. Effect of shock-wave therapy on patellar tendinopathy in a rabbit model. J. Orthop. Res. 2004, 22, 221–227. [Google Scholar] [CrossRef]
- Orhan, Z.; Cam, K.; Alper, M.; Ozturan, K. The effects of extracorporeal shock waves on the rat achilles tendon: Is there a critical dose for tissue injury? Arch. Orthop. Trauma Surg. 2004, 124, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Wang, F.-S.; Yang, K.D.; Weng, L.-H.; Hsu, C.-C.; Huang, C.-S.; Yang, L.-C. Shock wave therapy induces neovascularization at the tendon–bone junction. A study in rabbits. J. Orthop. Res. 2003, 21, 984–989. [Google Scholar] [CrossRef]
- Maier, M.; Tischer, T.; Milz, S.; Weiler, C.; Nerlich, A.; Pellengahr, C.; Schmitz, C.; Refior, H.J. Dose-related effects of extracorporeal shock waves on rabbit quadriceps tendon integrity. Arch. Orthop. Trauma Surg. 2002, 122, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Huang, H.-Y.; Pai, C.-H. Shock wave-enhanced neovascularization at the tendon-bone junction: An experiment in dogs. J. Foot Ankle Surg. 2002, 41, 16–22. [Google Scholar] [CrossRef]
- Johannes, E.J.; Kaulesar Sukul, D.M.; Bijma, A.M.; Mulder, P.G. Effects of high-energy shockwaves on normal human fibroblasts in suspension. J. Surg. Res. 1994, 57, 677–681. [Google Scholar] [CrossRef]
- Huang, P.P.; Zhang, Q.B.; Zhou, Y.; Liu, A.Y.; Wang, F.; Xu, Q.Y.; Yang, F. Effect of radial extracorporeal shock wave combined with ultrashort wave diathermy on fibrosis and contracture of muscle. Am. J. Phys. Med. Rehabil. 2021, 100, 643–650. [Google Scholar] [CrossRef]
- Kenmoku, T.; Iwakura, N.; Ochiai, N.; Saisu, T.; Ohtori, S.; Takahashi, K.; Nakazawa, T.; Fukuda, M.; Takaso, M. Influence of different energy patterns on efficacy of radial shock wave therapy. J. Orthop. Sci. 2021, 26, 698–703. [Google Scholar] [CrossRef]
- Park, H.J.; Hong, J.; Piao, Y.; Shin, H.J.; Lee, S.J.; Rhyu, I.J.; Yi, M.H.; Kim, J.; Kim, D.W.; Beom, J. Extracorporeal shockwave therapy enhances peripheral nerve remyelination and gait function in a crush model. Adv. Clin. Exp. Med. 2020, 29, 819–824. [Google Scholar] [CrossRef]
- Matsuda, M.; Kanno, H.; Sugaya, T.; Yamaya, S.; Yahata, K.; Handa, K.; Shindo, T.; Shimokawa, H.; Ozawa, H.; Itoi, E. Low-energy extracorporeal shock wave therapy promotes BDNF expression and improves functional recovery after spinal cord injury in rats. Exp. Neurol. 2020, 328, 113251. [Google Scholar] [CrossRef]
- Langendorf, E.K.; Klein, A.; Drees, P.; Rommens, P.M.; Mattyasovszky, S.G.; Ritz, U. Exposure to radial extracorporeal shockwaves induces muscle regeneration after muscle injury in a surgical rat model. J. Orthop. Res. 2020, 38, 1386–1397. [Google Scholar] [CrossRef]
- Sagir, D.; Bereket, C.; Onger, M.E.; Bakhit, N.; Keskin, M.; Ozkan, E. Efficacy of extracorporeal shockwaves therapy on peripheral nerve regeneration. J. Craniofac. Surg. 2019, 30, 2635–2639. [Google Scholar] [CrossRef] [PubMed]
- Feichtinger, X.; Monforte, X.; Keibl, C.; Hercher, D.; Schanda, J.; Teuschl, A.H.; Muschitz, C.; Redl, H.; Fialka, C.; Mittermayr, R. Substantial biomechanical improvement by extracorporeal shockwave therapy after surgical repair of rodent chronic rotator cuff tears. Am. J. Sports Med. 2019, 47, 2158–2166. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.H.; Yip, H.K.; Chen, H.F.; Yin, T.C.; Chiang, J.Y.; Sung, P.H.; Lin, K.C.; Tsou, Y.H.; Chen, Y.L.; Li, Y.C.; et al. Long-term therapeutic effects of extracorporeal shock wave-assisted melatonin therapy on mononeuropathic pain in rats. Neurochem. Res. 2019, 44, 796–810. [Google Scholar] [CrossRef] [PubMed]
- Mattyasovszky, S.G.; Langendorf, E.K.; Ritz, U.; Schmitz, C.; Schmidtmann, I.; Nowak, T.E.; Wagner, D.; Hofmann, A.; Rommens, P.M.; Drees, P. Exposure to radial extracorporeal shock waves modulates viability and gene expression of human skeletal muscle cells: A controlled in vitro study. J. Orthop. Surg. Res. 2018, 13, 75. [Google Scholar] [CrossRef]
- Yin, T.C.; Wu, R.W.; Sheu, J.J.; Sung, P.H.; Chen, K.H.; Chiang, J.Y.; Hsueh, S.K.; Chung, W.J.; Lin, P.Y.; Hsu, S.L.; et al. Combined therapy with extracorporeal shock wave and adipose-derived mesenchymal stem cells remarkably improved acute ischemia-reperfusion injury of quadriceps muscle. Oxid. Med. Cell. Longev. 2018, 2018, 6012636. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.C.; Ha, K.Y.; Kim, Y.H.; Kim, J.W.; Cho, Y.K.; Kim, S.I. Induction of endogenous neural stem cells by extracorporeal shock waves after spinal cord injury. Spine 2018, 43, E200–E207. [Google Scholar] [CrossRef] [PubMed]
- Luh, J.J.; Huang, W.T.; Lin, K.H.; Huang, Y.Y.; Kuo, P.L.; Chen, W.S. Effects of extracorporeal shock wave-mediated transdermal local anesthetic drug delivery on rat caudal nerves. Ultrasound. Med. Biol. 2018, 44, 214–222. [Google Scholar] [CrossRef]
- Kenmoku, T.; Nemoto, N.; Iwakura, N.; Ochiai, N.; Uchida, K.; Saisu, T.; Ohtori, S.; Nakagawa, K.; Sasho, T.; Takaso, M. Extracorporeal shock wave treatment can selectively destroy end plates in neuromuscular junctions. Muscle Nerve 2018, 57, 466–472. [Google Scholar] [CrossRef]
- Chen, K.H.; Yang, C.H.; Wallace, C.G.; Lin, C.R.; Liu, C.K.; Yin, T.C.; Huang, T.H.; Chen, Y.L.; Sun, C.K.; Yip, H.K. Combination therapy with extracorporeal shock wave and melatonin markedly attenuated neuropathic pain in rat. Am. J. Transl. Res. 2017, 9, 4593–4606. [Google Scholar]
- Yahata, K.; Kanno, H.; Ozawa, H.; Yamaya, S.; Tateda, S.; Ito, K.; Shimokawa, H.; Itoi, E. Low-energy extracorporeal shock wave therapy for promotion of vascular endothelial growth factor expression and angiogenesis and improvement of locomotor and sensory functions after spinal cord injury. J. Neurosurg. Spine 2016, 25, 745–755. [Google Scholar] [CrossRef]
- Schuh, C.M.; Hercher, D.; Stainer, M.; Hopf, R.; Teuschl, A.H.; Schmidhammer, R.; Redl, H. Extracorporeal shockwave treatment: A novel tool to improve schwann cell isolation and culture. Cytotherapy 2016, 18, 760–770. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H. Knee joint angle of intracerebral hemorrhage-induced rats after extracorporeal shock wave therapy. J. Phys. Ther. Sci. 2016, 28, 3122–3124. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kisch, T.; Wuerfel, W.; Forstmeier, V.; Liodaki, E.; Stang, F.H.; Knobloch, K.; Mailaender, P.; Kraemer, R. Repetitive shock wave therapy improves muscular microcirculation. J. Surg. Res. 2016, 201, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, S.G. Effects of extracorporeal shock wave therapy on functional recovery and neurotrophin-3 expression in the spinal cord after crushed sciatic nerve injury in rats. Ultrasound Med. Biol. 2015, 41, 790–796. [Google Scholar] [CrossRef]
- Yamaya, S.; Ozawa, H.; Kanno, H.; Kishimoto, K.N.; Sekiguchi, A.; Tateda, S.; Yahata, K.; Ito, K.; Shimokawa, H.; Itoi, E. Low-energy extracorporeal shock wave therapy promotes vascular endothelial growth factor expression and improves locomotor recovery after spinal cord injury. J. Neurosurg. 2014, 121, 1514–1525. [Google Scholar] [CrossRef]
- Fu, M.; Cheng, H.; Li, D.; Yu, X.; Ji, N.; Luo, F. Radial shock wave therapy in the treatment of chronic constriction injury model in rats: A preliminary study. Chin. Med. J. 2014, 127, 830–834. [Google Scholar]
- Ishikawa, T.; Miyagi, M.; Yamashita, M.; Kamoda, H.; Eguchi, Y.; Arai, G.; Suzuki, M.; Sakuma, Y.; Oikawa, Y.; Orita, S.; et al. In-vivo transfection of the proopiomelanocortin gene, precursor of endogenous endorphin, by use of radial shock waves alleviates neuropathic pain. J. Orthop. Sci. 2013, 18, 636–645. [Google Scholar] [CrossRef]
- Mense, S.; Hoheisel, U. Shock wave treatment improves nerve regeneration in the rat. Muscle Nerve 2013, 47, 702–710. [Google Scholar] [CrossRef]
- Hausner, T.; Pajer, K.; Halat, G.; Hopf, R.; Schmidhammer, R.; Redl, H.; Nogradi, A. Improved rate of peripheral nerve regeneration induced by extracorporeal shock wave treatment in the rat. Exp. Neurol. 2012, 236, 363–370. [Google Scholar] [CrossRef]
- Kenmoku, T.; Ochiai, N.; Ohtori, S.; Saisu, T.; Sasho, T.; Nakagawa, K.; Iwakura, N.; Miyagi, M.; Ishikawa, T.; Tatsuoka, H.; et al. Degeneration and recovery of the neuromuscular junction after application of extracorporeal shock wave therapy. J. Orthop. Res. 2012, 30, 1660–1665. [Google Scholar] [CrossRef]
- Yamashita, M.; Yamauchi, K.; Suzuki, M.; Eguchi, Y.; Orita, S.; Endo, M.; Yamashita, T.; Takahashi, K.; Ohtori, S. Transfection of rat cells with proopiomeranocortin gene, precursor of endogenous endorphin, using radial shock waves suppresses inflammatory pain. Spine 2009, 34, 2270–2277. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.H.; Liang, H.W.; Chen, W.S.; Lai, J.S.; Luh, J.J.; Chong, F.C. Electrophysiological and functional effects of shock waves on the sciatic nerve of rats. Ultrasound Med. Biol. 2008, 34, 1688–1696. [Google Scholar] [CrossRef] [PubMed]
- Hausdorf, J.; Lemmens, M.A.; Heck, K.D.; Grolms, N.; Korr, H.; Kertschanska, S.; Steinbusch, H.W.; Schmitz, C.; Maier, M. Selective loss of unmyelinated nerve fibers after extracorporeal shockwave application to the musculoskeletal system. Neuroscience 2008, 155, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Hausdorf, J.; Lemmens, M.A.; Kaplan, S.; Marangoz, C.; Milz, S.; Odaci, E.; Korr, H.; Schmitz, C.; Maier, M. Extracorporeal shockwave application to the distal femur of rabbits diminishes the number of neurons immunoreactive for substance P in dorsal root ganglia L5. Brain Res. 2008, 1207, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.C.; Huang, H.Y.; Yang, Y.L.; Hung, K.S.; Cheng, C.H.; Chang, N.K.; Chung, Y.H.; Hu, M.S.; Wang, C.J. Vulnerability of the spinal cord to injury from extracorporeal shock waves in rabbits. J. Clin. Neurosci. 2007, 14, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, N.; Ohtori, S.; Sasho, T.; Nakagawa, K.; Takahashi, K.; Takahashi, N.; Murata, R.; Takahashi, K.; Moriya, H.; Wada, Y.; et al. Extracorporeal shock wave therapy improves motor dysfunction and pain originating from knee osteoarthritis in rats. Osteoarthr. Cartil. 2007, 15, 1093–1096. [Google Scholar] [CrossRef]
- Wu, Y.H.; Lun, J.J.; Chen, W.S.; Chong, F.C. The electrophysiological and functional effect of shock wave on peripheral nerves. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; Volume 2007, pp. 2369–2372. [Google Scholar]
- Murata, R.; Ohtori, S.; Ochiai, N.; Takahashi, N.; Saisu, T.; Moriya, H.; Takahashi, K.; Wada, Y. Extracorporeal shockwaves induce the expression of ATF3 and GAP-43 in rat dorsal root ganglion neurons. Auton. Neurosci. 2006, 128, 96–100. [Google Scholar] [CrossRef]
- Takahashi, N.; Ohtori, S.; Saisu, T.; Moriya, H.; Wada, Y. Second application of low-energy shock waves has a cumulative effect on free nerve endings. Clin. Orthop. Relat. Res. 2006, 443, 315–319. [Google Scholar] [CrossRef]
- Bolt, D.M.; Burba, D.J.; Hubert, J.D.; Strain, G.M.; Hosgood, G.L.; Henk, W.G.; Cho, D.Y. Determination of functional and morphologic changes in palmar digital nerves after nonfocused extracorporeal shock wave treatment in horses. Am. J. Vet. Res. 2004, 65, 1714–1718. [Google Scholar] [CrossRef]
- Hausdorf, J.; Schmitz, C.; Averbeck, B.; Maier, M. Molekulare Grundlagen zur schmerzvermittelnden Wirkung extrakorporaler Stosswellen [Molecular basis for pain mediating properties of extracorporeal shock waves]. Schmerz 2004, 18, 492–497. (In German) [Google Scholar] [CrossRef]
- Takahashi, N.; Wada, Y.; Ohtori, S.; Saisu, T.; Moriya, H. Application of shock waves to rat skin decreases calcitonin gene-related peptide immunoreactivity in dorsal root ganglion neurons. Auton. Neurosci. 2003, 107, 81–84. [Google Scholar] [CrossRef]
- Maier, M.; Averbeck, B.; Milz, S.; Refior, H.J.; Schmitz, C. Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clin. Orthop. Relat. Res. 2003, 406, 237–245. [Google Scholar] [CrossRef]
- Haake, M.; Thon, A.; Bette, M. Unchanged c-Fos expression after extracorporeal shock wave therapy: An experimental investigation in rats. Arch. Orthop. Trauma Surg. 2002, 122, 518–521. [Google Scholar] [CrossRef] [PubMed]
- Ohtori, S.; Inoue, G.; Mannoji, C.; Saisu, T.; Takahashi, K.; Mitsuhashi, S.; Wada, Y.; Takahashi, K.; Yamagata, M.; Moriya, H. Shock wave application to rat skin induces degeneration and reinnervation of sensory nerve fibres. Neurosci. Lett. 2001, 315, 57–60. [Google Scholar] [CrossRef]
- Haake, M.; Thon, A.; Bette, M. Absence of spinal response to extracorporeal shock waves on the endogenous opioid systems in the rat. Ultrasound Med. Biol. 2001, 27, 279–284. [Google Scholar] [CrossRef]
- Rompe, J.D.; Bohl, J.; Riehle, H.M.; Schwitalle, M.; Krischek, O. Überprüfung der Läsionsgefahr des N. ischiadicus des Kaninchens durch die Applikation niedrig- und mittelenergetischer extrakorporaler Stosswellen [Evaluating the risk of sciatic nerve damage in the rabbit by administration of low and intermediate energy extracorporeal shock waves]. Z. Orthop. Ihre Grenzgeb. 1998, 136, 407–411. (In German) [Google Scholar] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Dakin, S.G.; Newton, J.; Martinez, F.O.; Hedley, R.; Gwilym, S.; Jones, N.; Reid, H.A.B.; Wood, S.; Wells, G.; Appleton, L.; et al. Chronic inflammation is a feature of achilles tendinopathy and rupture. Br. J. Sports Med. 2018, 52, 359–367. [Google Scholar] [CrossRef]
- Vidal, X.; Marti-Fabregas, J.; Canet, O.; Roque, M.; Morral, A.; Tur, M.; Schmitz, C.; Sitja-Rabert, M. Efficacy of radial extracorporeal shock wave therapy compared with botulinum toxin type a injection in treatment of lower extremity spasticity in subjects with cerebral palsy: A randomized, controlled, cross-over study. J. Rehabil. Med. 2020, 52, jrm00076. [Google Scholar] [CrossRef]
- van der Worp, H.; van den Akker-Scheek, I.; van Schie, H.; Zwerver, J. ESWT for tendinopathy: Technology and clinical implications. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1451–1458. [Google Scholar] [CrossRef]
- Cleveland, R.O.; Chitnis, P.V.; McClure, S.R. Acoustic field of a ballistic shock wave therapy device. Ultrasound Med. Biol. 2007, 33, 1327–1335. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.A.; Toth-Kischkat, A.; Schultheiss, R. Principles of shock wave therapy. Clin. Orthop. Relat. Res. 2001, 387, 8–17. [Google Scholar] [CrossRef] [PubMed]
- McClure, S.; Dorfmüller, C. Extracorporeal shock wave therapy: Theory and equipment. Clin. Techn. Equine Pract. 2003, 2, 348–357. [Google Scholar] [CrossRef]
- Maier, M.; Schmitz, C. Shock wave therapy: What really matters. Ultrasound Med. Biol. 2008, 34, 1868–1869. [Google Scholar] [CrossRef] [PubMed]
- Csaszar, N.B.; Angstman, N.B.; Milz, S.; Sprecher, C.M.; Kobel, P.; Farhat, M.; Furia, J.P.; Schmitz, C. Radial shock wave devices generate cavitation. PLoS ONE 2015, 10, e0140541. [Google Scholar] [CrossRef] [PubMed]
- Mandal, C.C.; Ganapathy, S.; Gorin, Y.; Mahadev, K.; Block, K.; Abboud, H.E.; Harris, S.E.; Ghosh-Choudhury, G.; Ghosh-Choudhury, N. Reactive oxygen species derived from Nox4 mediate BMP2 gene transcription and osteoblast differentiation. Biochem. J. 2011, 433, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Wright, H.L.; McCarthy, H.S.; Middleton, J.; Marshall, M.J. RANK, RANKL and osteoprotegerin in bone biology and disease. Curr. Rev. Musculoskelet. Med. 2009, 2, 56–64. [Google Scholar] [CrossRef]
- Lee, T.C.; Staines, A.; Taylor, D. Bone adaptation to load: Microdamage as a stimulus for bone remodelling. J. Anat. 2002, 201, 437–446. [Google Scholar] [CrossRef]
- Shi, L.; Gao, F.; Sun, W.; Wang, B.; Guo, W.; Cheng, L.; Li, Z.; Wang, W. Short-term effects of extracorporeal shock wave therapy on bone mineral density in postmenopausal osteoporotic patients. Osteoporos. Int. 2017, 28, 2945–2953. [Google Scholar] [CrossRef]
- Snijdelaar, D.G.; Dirksen, R.; Slappendel, R.; Crul, B.J. Substance P. Eur. J. Pain 2000, 4, 121–135. [Google Scholar] [CrossRef]
- Mashaghi, A.; Marmalidou, A.; Tehrani, M.; Grace, P.M.; Pothoulakis, C.; Dana, R. Neuropeptide substance P and the immune response. Cell. Mol. Life Sci. 2016, 73, 4249–4264. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.Q.; Mantyh, P.W.; Carlson, E.J.; Gillespie, A.M.; Epstein, C.J.; Basbaum, A.I. Primary afferent tachykinins are required to experience moderate to intense pain. Nature 1998, 392, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Frias, B.; Merighi, A. Capsaicin, nociception and pain. Molecules 2016, 21, 797. [Google Scholar] [CrossRef] [PubMed]
- Gamse, R.; Petsche, U.; Lembeck, F.; Jancso, G. Capsaicin applied to peripheral nerve inhibits axoplasmic transport of substance p and somatostatin. Brain Res. 1982, 239, 447–462. [Google Scholar] [CrossRef]
- Lam, F.Y.; Ferrell, W.R. Capsaicin suppresses substance p-induced joint inflammation in the rat. Neurosci. Lett. 1989, 105, 155–158. [Google Scholar] [CrossRef]
- Anand, P.; Bley, K. Topical capsaicin for pain management: Therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch. Br. J. Anaesth. 2011, 107, 490–502. [Google Scholar] [CrossRef]
- Jones, R. Nonsteroidal anti-inflammatory drug prescribing: Past, present, and future. Am. J. Med. 2001, 110, 4S–7S. [Google Scholar] [CrossRef]
- Santamato, A.; Cinone, N.; Panza, F.; Letizia, S.; Santoro, L.; Lozupone, M.; Daniele, A.; Picelli, A.; Baricich, A.; Intiso, D.; et al. Botulinum toxin type a for the treatment of lower limb spasticity after stroke. Drugs 2019, 79, 143–160. [Google Scholar] [CrossRef]
- Palazon-Garcia, R.; Alcobendas-Maestro, M.; Esclarin-de Ruz, A.; Benavente-Valdepenas, A.M. Treatment of spasticity in spinal cord injury with botulinum toxin. J. Spinal Cord. Med. 2019, 42, 281–287. [Google Scholar] [CrossRef]
- Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society; Delgado, M.R.; Hirtz, D.; Aisen, M.; Ashwal, S.; Fehlings, D.L.; McLaughlin, J.; Morrison, L.A.; Shrader, M.W.; Tilton, A.; et al. Practice parameter: Pharmacologic treatment of spasticity in children and adolescents with cerebral palsy (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2010, 74, 336–343. [Google Scholar]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum neurotoxins: Biology, pharmacology, and toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Cote, T.R.; Mohan, A.K.; Polder, J.A.; Walton, M.K.; Braun, M.M. Botulinum toxin type a injections: Adverse events reported to the US food and drug administration in therapeutic and cosmetic cases. J. Am. Acad. Dermatol. 2005, 53, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Paget, S.P.; Swinney, C.M.; Burton, K.L.O.; Bau, K.; O’Flaherty, S.J. Systemic adverse events after botulinum neurotoxin a injections in children with cerebral palsy. Dev. Med. Child Neurol. 2018, 60, 1172–1177. [Google Scholar] [CrossRef] [PubMed]
- Harris, G.R. Effective treatment of chronic pain by the integration of neural therapy and prolotherapy. J. Prolother. 2010, 2, 377–386. [Google Scholar]
- Dullenkopf, A.; Borgeat, A. Lokalanästhetika. Unterschiede und Gemeinsamkeiten der “-caine” [Local anesthetics. Differences and similarities in the “-cains”]. Anaesthesist 2003, 52, 329–340. (In German) [Google Scholar] [CrossRef]
- Morgan, J.P.M.; Hamm, M.; Schmitz, C.; Brem, M.H. Return to play after treating acute muscle injuries in elite football players with radial extracorporeal shock wave therapy. J. Orthop. Surg. Res. 2021, 16, 708. [Google Scholar] [CrossRef]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef]
- Suputtitada, A.; Chen, C.P.C.; Ngamrungsiri, N.; Schmitz, C. Effects of repeated injection of 1% lidocaine vs. radial extra-corporeal shock wave therapy for treating myofascial trigger points: A randomized controlled trial. Medicina 2022, 58, 479. [Google Scholar] [CrossRef]
- Goats, G.C. Massage--the scientific basis of an ancient art: Part 2. Physiological and therapeutic effects. Br. J. Sports Med. 1994, 28, 153–156. [Google Scholar] [CrossRef]
- Kohrs, R.T.; Zhao, C.; Sun, Y.L.; Jay, G.D.; Zhang, L.; Warman, M.L.; An, K.N.; Amadio, P.C. Tendon fascicle gliding in wild type, heterozygous, and lubricin knockout mice. J. Orthop. Res. 2011, 29, 384–389. [Google Scholar] [CrossRef]
- Willkomm, L.M.; Bickert, B.; Wendt, H.; Kneser, U.; Harhaus, L. Weiterbehandlung und Rehabilitation nach Beugesehnenverletzungen [Postoperative treatment and rehabilitation following flexor tendon injuries]. Unfallchirurg 2020, 123, 126–133. (In German) [Google Scholar] [CrossRef] [PubMed]
- Pavan, P.G.; Stecco, A.; Stern, R.; Stecco, C. Painful connections: Densification versus fibrosis of fascia. Curr. Pain Headache Rep. 2014, 18, 441. [Google Scholar] [CrossRef] [PubMed]
- von Heymann, W.; Stecco, C. Fasziale Dysfunktionen [Fascial dysfunction]. Man. Med. 2016, 54, 303–306. (In German) [Google Scholar] [CrossRef]
- Zhang, L.; Fu, X.B.; Chen, S.; Zhao, Z.B.; Schmitz, C.; Wen, C.S. Efficacy and safety of extracorporeal shock wave therapy for acute and chronic soft tissue wounds: A systematic review and meta-analysis. Int. Wound J. 2018, 15, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Burneikaitė, G.; Shkolnik, E.; Čelutkienė, J.; Zuozienė, G.; Butkuvienė, I.; Petrauskienė, B.; Šerpytis, P.; Laucevičius, A.; Lerman, A. Cardiac shock-wave therapy in the treatment of coronary artery disease: Systematic review and meta-analysis. Cardiovasc. Ultrasound 2017, 15, 11. [Google Scholar] [CrossRef]
| Ref. | First Author | Year | M | Morphological, Functional and Radiological Findings | ||
|---|---|---|---|---|---|---|
| Findings of Molecular Biological Investigations | ||||||
| Findings of Histological Investigations | ||||||
| [18] | Li | 2021 | F | Increased mineral apposition rates, trabecular bone volume, number, thickness; decreased trabecular separation | ||
| Increased expressions of ALP, OCN, RUNX2, OPG, SMAD2 | ||||||
| [19] | Inoue | 2021 | R | Increased trabecular bone microarchitecture and bone strength | ||
| Decreased RANKL | ||||||
| [20] | Inoue | 2021 | R | Increased bone/tissue volumes | ||
| Increased osteoblast surface, decreased number of sclerostin-positive osteocytes | ||||||
| [21] | Zhao | 2021 | R | Unaltered expressions of OCN, RUNX2, COL2, SOX9; decreased expressions of CEBPα and PPARγ; increased expression of YAP | ||
| Increased proliferation | ||||||
| [22] | Kobayashi | 2020 | F | Increased bone union rate, radiographic score | ||
| Increased enchondral ossification, chondrogenic differentiation without inhibited proliferation | ||||||
| [23] | Alshihri | 2020 | F | Unaltered cell migration; increased proliferation and osteogenic differentiation | ||
| [24] | Hsu | 2020 | F | Increased bone strength, bone mineral density, trabecular thickness, bone /tissue volumes, porosity | ||
| Increased expressions of BMP2, BMP4 and Wnt3a signaling; unaltered expression of IGF1 | ||||||
| [25] | Ramesh | 2020 | R | Increased bone length | ||
| Increased number of proliferative chondrocytes of growth plate’s cartilage and diameter of hypertrophic chondrocytes; activation of IGF1 and NFkb; increased levels of BCL2 and BCL-xL | ||||||
| [26] | Colbath | 2020 | F | Increased expression of ALP, decreased expressions of TGFb and VEGF | ||
| [27] | Hashimoto | 2019 | F | Increased expressions of COL2a1, ACAN, CCN2, SOX9 | ||
| Increased meniscal healing score and BrdU/CCN2 ratio | ||||||
| [28] | Senel | 2019 | F | Bone mineral density, bone mineral content | ||
| [29] | Kim | 2019 | F | Increased structure and bone quality | ||
| Decreased expressions of TNFa, IL1b, IL6, MMP3, MMP13, BMP7 | ||||||
| Increased cell viability; decreased number of apoptotic cells and pro-inflammatory, cartilage degradation markers | ||||||
| [30] | Buarque de Gusmao | 2019 | F/R | F: increased Akt and FAK activity and TGFb1 expression R: increased FAK activity, decreased Akt expression | ||
| [31] | Cheng | 2019 | F | Enhanced bone volume and trabecular thickness | ||
| Reduced synovitis and cartilage damage; decreased expression of MMP-13; enhanced expressions of RUNX2, SOX-9 and COL10A1; enhanced expressions of IGF1, TGFb1 and COL2 and decreased TUNEL activity | ||||||
| [32] | Ginini | 2019 | F | Increased mineral density, enhanced bone formation | ||
| Higher collagen orientation index, increased expressions of COL1 and OCN | ||||||
| [33] | Ginini | 2018 | F | Higher degree of bone formation and mature bone; increased bone mineral density, bone volume fraction, and trabecular thickness | ||
| Enhanced expressions of BMP2, VEGF and PCNA | ||||||
| [34] | Qi | 2018 | R | Improved International Cartilage Repair Society (ICRS) score and macroscopic osteochondral appearance | ||
| [35] | Koolen | 2018 | F | Cortical screws: increased bone formation and screw fixation. Cancellous screws: no alterations | ||
| [36] | Mackert | 2017 | F | Improved average stiffness and yield load | ||
| Increased expressions of COL1a1, NR3A1, IGF1, OCN, TRAP | ||||||
| Improved average ventral, dorsal and endosteal callus formation | ||||||
| [37] | Tan | 2017 | F | ESWT alone: increased levels of A2B receptors; ESWT in combination with adenosine and A2BR agonists downregulated ACAN, COL1A2, COL2A1, SOX9 and SOX6 | ||
| ESWT + adenosine and A2BR agonists: inhibited chondrogenic differentiation | ||||||
| [38] | Hsu | 2017 | n.s. | Increased expressions of ERK1, OPG, ALP, MMP13; potential activation of the 1α,25-Dihydroxyvitamin D3 Rapid Membrane Signaling Pathway | ||
| Increased expression of PDIA3 | ||||||
| [39] | Yilmaz | 2017 | F | Increased osteoblastic activity, improved pain score | ||
| Lower modified Mankin score | ||||||
| [40] | Wang | 2017 | F | Improved OARSI score and gross pathological changes, less cartilage defects, higher bone mineral density and bone volume, improved bone porosity and yield stress | ||
| Increased expressions PCNA and OCN, decreased expression of TUNEL | ||||||
| [41] | Chen | 2017 | F | In vivo: improved bone volume, trabecular volume, BV/TV, bone thickness and bone mineral density | ||
| In vitro: increased expressions of COL1, RUNX2, OSX and ALP | ||||||
| In vitro: enhanced proliferation and osteogenic differentiation; in vivo: increased bone formation and expressions of RUNX2 and OSX | ||||||
| [42] | Onger | 2017 | F | 500 impulses per treatment: unaltered bone volume/bone density 1000 impulses per treatment: enhanced bone volume/bone density | ||
| 500 impulses per treatment: enhanced capillary volume, decreased connective tissue volume 1000 impulses per treatment: enhanced capillary volume; more positive areas of staining with VEGF, collagen antibody, BMP7 compared to control, but decreased capillary volume compared to 500 impulses; unaltered connective tissue volume | ||||||
| [43] | Wang | 2017 | F | Improved OARSI score and gross pathological changes, less cartilage defects, improved BV/TV ratio, improved bone porosity and trabecular thickness | ||
| Decreased expression of TUNEL; higher amount of PCNA-positive cells and increased vascular density; increased cartilage thickness and sectional cartilage area; decreased modified Mankin score | ||||||
| [44] | Lama | 2017 | F | Prevention of bone-weight reduction and trabecular microarchitecture deterioration; restored serum parameters of ALP, RANKL, OPG and PTH due to illness | ||
| Reduced cathepsin k, TNF-α levels, PPARγ and adiponectin transcription; increased RUNX2 and BMP2 expressions | ||||||
| [45] | Catalano | 2017 | F | Increased ERK phosphorylation, ROS formation, RUNX2, ALP, BMP2 | ||
| [46] | Ma | 2017 | F | Higher bone volume per tissue volume, trabecular thickness, trabecular number, osteoblast surface/bone surface, osteoid surface/bone surface, osteoid thickness, mineralizing surface/bone surface, mineralizing apposition rate and bone formation rate as well as a reduced trabecular separation | ||
| [47] | Huang | 2016 | F | Increased expressions of OPG and BMP-2 | ||
| [48] | Notarnicola | 2016 | F | Increased expressions of BMP, ALP, OCN, COL1A1 and RUNX2 | ||
| Enhanced cell adhesion and proliferation | ||||||
| [49] | Zhai | 2016 | F | Increased expression of OCN, core-binding factor α1 and decreased PPARγ | ||
| Increased ALP content | ||||||
| [50] | Dias dos Santos | 2015 | F | Increased contents of sulfated glycosaminoglycans and hyaluronic acid | ||
| [51] | Wang | 2014 | F | Reduced arthritic area of injury joint, enhanced bone mineral density and bone strength, improved subchondral plate thickness and bone porosity, reduced cartilage damage | ||
| Increased Mankin and Safranin O scores, improved alterations of the molecular levels due to the illness of Dickkopf-1, PCNA, VEGF and BMP-2 | ||||||
| [52] | Muzio | 2014 | F | Decreased ALP and OCN | ||
| Increased cell growth | ||||||
| Increased SMAD phosphorylation | ||||||
| [53] | Oktas | 2014 | F | No radiologic differences | ||
| Excised periosteum group: positive effect on bone healing | ||||||
| [54] | Sun | 2013 | F | Shockwave-dependent ATP release that activated P2X7 receptors and downstream signaling events, which induced the differentiation | ||
| [55] | Suhr | 2013 | F | Extended growth rate, proliferation, migration, cell tracking and wound healing; ameliorated cell migration meditated by active remodeling of the actin cytoskeleton as indicated by increased directed stress fiber formations | ||
| [56] | Lyon | 2013 | F | Increased bony density | ||
| More mature bone formation, better healing, higher density of the cartilage | ||||||
| [57] | Wang | 2013 | F | Increased bone mineral density | ||
| Improved Mankin and Safranin O scores; increased COL2; decreased MMP13 | ||||||
| [58] | Wang | 2013 | F | Treatment 1–2 times per week: improved Makin and Safranin O scores; increased COL2; decreased MMP13; increased vWF, VEGF, BMP-2 and osteocalcin; deteriorated effects after 3 treatments per week | ||
| [59] | van der Jagt | 2013 | F | Increased cortical volume (CtV), higher trabecular connectivity and more plate-like and thicker trabeculae, increased trabecular bone volume fraction | ||
| [60] | Oztemur | 2013 | R | No changes in bone length | ||
| Increased blood vessel density, highly basophilic matrix and abundance of the differentiating chondrocytes | ||||||
| [61] | Gollwitzer | 2013 | R | New bone formation | ||
| [62] | Altuntas | 2012 | R | Higher specimens’ mean scores in bone fracture healing | ||
| [63] | Notarnicola | 2012 | F | Reduction in COL1, OSX, bone sialoprotein and RANKL expressions, OCN and osteopontin; in summary: inhibiting effect on osteoclastogenesis | ||
| [64] | Zhao | 2012 | R | Decreased NO level, and severity of cartilage lesions | ||
| Decreased chondrocyte apoptosis, enhanced Mankin score | ||||||
| [65] | Kearney | 2012 | F | Increased cambium cell number, cambium cell thickness, osseous tissue and callus area, larger amount of osteoprogenitor tissue; improved results in combination with a bioactive scaffold | ||
| [66] | Xu | 2012 | F | Promotion of Integrin alpha-5 and beta-1 expressions; induction of phosphorylation of FAK, which led to increased adhesion and migration of osteoblasts | ||
| [67] | Wang | 2012 | F | Improved Mankin and Safranin O scores, increased COL2, VEGF, BMP2 and OCN expressions | ||
| [68] | Erturk | 2012 | F | No alterations in MRI | ||
| Edema, increased fibroblastic activity, neovascularization | ||||||
| [69] | Wang | 2011 | F | Increased BMD, bone strength, modulus of elasticity | ||
| Decreased Mankin score; improved Safranin O staining results; increased expressions of VWF, VEGF, BMP2, OCN and ALP; decreased expression of CTXII, cartilage oligomeric matrix protein | ||||||
| [70] | van der Jagt | 2011 | F | Increased 99mTc-MDP uptake, increased trabecular and cortical bone volume, higher bone stiffness; no alterations in microcrack analysis | ||
| Soft tissue damage, no periosteal damage, de novo bone with active osteoblasts and osteoids | ||||||
| [71] | Notarnicola | 2011 | F | Increased expressions of RUNX2, COL1, OCN, IGF1, IGFBP3; decreased expressions of IGFBP-4 and -5 | ||
| [72] | Hausdorf | 2011 | F | Increased basic fibroblast growth factor; no significant alterations in TGFb | ||
| [73] | Wang | 2011 | F | Increased bone mineral content | ||
| Increased bone tissue; decreased fibrous tissue; increased expressions of VEGF, VWF, PCNA, OCN and BMP2; decreased expression of TUNEL | ||||||
| [74] | Mayer-Wagner | 2010 | F | Increased COL2A1 expression | ||
| Ultrastructural expansion of the rough-surfaced endoplasmatic reticulum, detachment of the cell membrane and necrotic chondrocytes; increased tenascin-C and Chitinase-3-like protein 1; no alterations in Mankin score | ||||||
| [75] | Muzio | 2010 | F | Increased expressions of ALP, COL1, BMP-4, OCN | ||
| Increased osteoblast activity as well as number and size of calcium deposits | ||||||
| [76] | Lai | 2010 | F | Treatment with 14kV: increased mineral density, biomechanical bone strength, intense osteoblastic cell recruitment, new bone formation | ||
| Treatment with 14kV: intense osteoblastic cell recruitment, new bone formation, neovascularization, increased PCNA, VEGF, BMP-2; opposite effects after treatment with 21kV | ||||||
| [77] | Qin | 2010 | F | Higher fraction of new bone | ||
| Increased VEGF expression in hypertrophic chondrocytes, promotion of regeneration of the fibrocartilage zone | ||||||
| [78] | van der Jagt | 2009 | F | Diminished bone loss, higher trabecular bone-volume fraction | ||
| No differences in mineralization or osteoid appearance | ||||||
| [79] | Iannone | 2009 | F | Increased expression of IL10; no alterations in TGFa, CD29 and CD105 expressions | ||
| [80] | Tamma | 2009 | F | Increased expressions of BCL-2-associated X protein, RUNX2, OPN, bone sialoprotein, OCN and COL1; decreased RANKL/OPG ratio suggesting inhibition of osteoclastogenesis | ||
| [81] | Lee | 2009 | F | Increased callus formation and both extension and flexion stiffness | ||
| [82] | Tam | 2009 | F | Enhanced trabecular bone mineral density, trabecular bone-volume fraction, trabecular thickness | ||
| Increased mineral apposition rate | ||||||
| [83] | Hofmann | 2008 | F | Altered expression of several genes involved in bone formation, osteoblast differentiation and skeletal development; no alterations in RUNX2, OSX, osteopontin, osteonectin, OC, TGFb1 expressions | ||
| Enhanced mineralization and number of ALP-positive osteoblasts | ||||||
| [84] | Tam | 2008 | F | Decreased cell viability 6 days after treatment; increased viability 18 days after treatment; increased cell proliferation 18 days after treatment | ||
| Enhanced mineralization 35 days after treatment and AP activity 18 days after treatment | ||||||
| [85] | Lee | 2008 | F | New bone formation | ||
| Superior fusion mass | ||||||
| [86] | Wang | 2008 | F | Increased bone strength | ||
| Increased cortical bone formation; higher number of newly formed vessels; increased expression of VEGF, nitric oxide synthase 3, PCNA and BMP-2 | ||||||
| [87] | Moretti | 2008 | F | Decreased expression of IL10 and TNFa in both groups; no alteration in b1-integrin expression | ||
| [88] | Tischer | 2008 | F | Dose-dependent new bone formation | ||
| Dose-dependent new bone formation | ||||||
| [89] | Ozturk | 2008 | F | Increased epiphyseal plaque thickness and number of chondrocytes | ||
| [90] | Ma | 2007 | F | Increased VEGF expression | ||
| Increased bone and osteoblast number; increased VEGF expression and microvessel density | ||||||
| [91] | Murata | 2007 | R | Augmented uniform gene transfection and increased activity of vector-expressed genes | ||
| [92] | Benson | 2007 | R | Decreased synthesis of GAG; no alterations in NO or Prostaglandin E2 synthesis | ||
| [93] | Martini | 2006 | F | Dose- and device-dependent cell viability and expression of ALP, Capicua Transcriptional Repressor Pseudogene, OCN and TGFb | ||
| [94] | Bulut | 2006 | F | Increased callus volume | ||
| Advanced bone healing | ||||||
| [95] | Martini | 2005 | F | Enhanced transmembrane current and voltage dependence of Ca-activated/K channels | ||
| [96] | Saisu | 2005 | F | Increased breadth of the acetabular roof and transient woven bone formation on the lateral margin | ||
| [97] | Chen | 2004 | F | Increased TGFb1 and VEGF-A expressions | ||
| Increased cell density and cell number of RP59-positive mesenchymal stem cells, subsequently enhanced differentiation into chondrocytes and osteocytes | ||||||
| [98] | Saisu | 2004 | F | Enhanced bone mineral content, long-bone length and width | ||
| [99] | Chen | 2004 | F | Increased ALPase, COL1, COL2 and OCN expressions and [3H]-thymidine uptake; increased expressions and phosphorylations of ERK and p38 | ||
| Activated ERK and p38 expressions | ||||||
| [100] | Pauwels | 2004 | F | No alterations in bone elasticity | ||
| [101] | Wang | 2004 | n.s. | Induced superoxide production; enhanced TGFb1, RUNX2, OCN and COL1 expressions; increased bone alkaline phosphatase activity | ||
| Increase in bone nodule formations, promotion of the CFU-stroma formation but not CFU-mix formation | ||||||
| [102] | da Costa Gomez | 2004 | F/R | R: increased microcrack length, fESWT: increased microcrack density | ||
| [103] | Takahashi | 2004 | F | Increased cortical thickening, bone mineral density, bone mineral content | ||
| Enhanced expressions of COL1A1, COL2A1, OC and OPN; no alterations in expression of COL10A1 | ||||||
| [104] | Chen | 2003 | F | Increased callus size and calcium content, bone mineral density | ||
| Increased ALP activity, OCN production, PCNA, TGFb1 and BMP-2 expressions | ||||||
| Increased bone-tissue formation, progressive mesenchymal aggregation, enchondral ossification and hard callus formation | ||||||
| [105] | Martini | 2003 | F | High intensity treatment (28 kV): decreased viability; reduced cell respiration; depressed ALP and NO synthesis; decreased expressions of OCN, TGFb and Procollagen-type I carboxy-terminal propeptide (PICP); low intensity treatment (14 kV) showed contrary effects with increased viability and cell respiration, increased ALP and NO synthesis as well as OCN and PICP expressions; generally negative affection of PICP production | ||
| [106] | Martini | 2003 | F | Increased NO, OCN and TGFb1 production after low energy application (14kV); decreased cell viability and expression of all examined proteins at high application intensities (28 kV) | ||
| [107] | Dorotka | 2003 | F | Increased cytotoxity in both chondrocytes and BMSCs at high application intensities (0.17mJ/mm2), compared to lower energy levels and control; unaltered cell proliferation at all energy levels | ||
| [108] | Wang | 2003 | F | Increased expressions of BMP2, BMP3, BMP4 and BMP7 | ||
| Intensive mesenchymal cell aggregation, hypertrophic chondrogenesis and endochondral/intramembrane ossification; increased levels of PCNA, BMP2, BMP3 and BMP4 | ||||||
| [109] | Maier | 2002 | F | Decreased bone metabolism after 10 days (detected by scintigraphy), but increased metabolism after 28 days; signs of soft-tissue oedema, epiperiosteal fluid and bone marrow oedema on MRI | ||
| Epiperiostal deposits of hemosiderin | ||||||
| [110] | Wang | 2002 | F | Increased ALP activity and TGFb1 expression | ||
| Promotion of bone marrow stromal, but not hematopoietic cell growth; dose-dependent effect on formation of CFU osteoprogenitors | ||||||
| [111] | Wang | 2001 | F | Induction of cell membrane hyperpolarization and consecutive Ras activation; induction of RUNX2; increased activity of bone ALP; increased expressions of OCN and COL1 | ||
| Increased bone-nodule formations | ||||||
| [112] | Wang | 2001 | F | More callus formations | ||
| More cortical bone and thicker, denser and heavier bone tissues | ||||||
| [113] | Vaterlein | 2000 | F | Neither macroscopic nor radiological alterations after high-intensity treatments | ||
| No histological alterations after high-intensity treatments | ||||||
| [114] | Peters | 1998 | F | Several damages to tissues after low-intensity treatment | ||
| [115] | Augat | 1995 | F | Neither alterations in biomechanical outcomes nor altered radiological results; tendency to deterioration of facture healing with increasing application intensities | ||
| [116] | Forriol | 1994 | F | No effect on the periosteal surface of mature cortical bone, but on the endosteal surface induction of some new trabecular bone; delayed bone healing | ||
| [6] | Graff | 1988 | F | Soft-tissue bleeding | ||
| Bone marrow hemorrhage and osteocyte damage 48 h after ESWT; increased callus and bone formation, focal regeneration, apposition of new bone, bone remodeling | ||||||
| Ref. | First Author | Year | M | Morphological, Functional and Radiological Findings | ||
|---|---|---|---|---|---|---|
| Findings of Molecular Biological Examinations | ||||||
| Findings of Histological Examinations | ||||||
| [117] | Haberal | 2021 | R | Decreased epidural fibrosis; unaltered acute/chronic inflammation and vascular proliferation | ||
| [118] | Heimes | 2020 | R | Increased expression of MMP-9; decreased expression of MMP-13; unaltered expression of inducible nitric oxide synthase 2, HIF1α, VEGF | ||
| Increased coverage of the transplant by vasculature, percentage of the vascularized area, increase in the vascularized area and number of vessel junctions | ||||||
| [119] | Lu | 2020 | F | Increased ACL remnant cell viability; BMSC: increased expressions of Ki67, COL1 and COL3; unaltered expressions of TGFb and VEGF | ||
| ACL cells: increased expression of COL1A1, TGFb and VEGF; BMSC: increased migration and expression of 5-Ethynyl-2’-deoxyuridine, COL1 and COL3; unaltered expression of VEGF and TGFb | ||||||
| [120] | Basoli | 2020 | F | Increased proliferation, ATP release, ROS production, expressions of IL8, MCP1, HSP90 and HSP27; unaltered expression of IL6 | ||
| [121] | Schnurrer-Luke-Vrbanić | 2018 | R | Higher multiplication of collagen fibers; faster organization of muscle fibers and vascularization by treatment with radial shockwaves | ||
| [122] | Cui | 2018 | F | Decreased expression of TGFb, a-SMA, vimentin, COL1A1, N-CAD and twist; increased expression of DNA-binding protein inhibitor ID1/2, E-CAD and FN after 24 h, but decreased expression of FN after 72 h | ||
| Decreased cell migration | ||||||
| [123] | Cai | 2016 | F | Initially decreased expression of IL6, IL8, MCP1 and TNFa; after 4 and more hours: increased expression of IL6 and IL8, unaltered expression of MCP1 and TNFa | ||
| [124] | Hoch-strasser | 2016 | R | Induced mechanical cell destruction, dose-dependent decreased cell viability, increased growth potential of fibroblasts (not of JEG-3 cells), shift in proportion from G0/G1 to G2/M phase in fibroblasts (not in JEG-3 cells) | ||
| Cellular detachments, holes in monolayers, disruption of actin filaments | ||||||
| [125] | Leone | 2016 | F | Increased expressions of COL2A, SOX9, ALP and PPARy; unaltered expressions of OCN and RUNX2 | ||
| Increased expression of differentiation markers in cells grown in specific differentiation media | ||||||
| [126] | Kisch | 2015 | F | Increased capillary blood velocity; unaltered postcapillary venous filling pressure | ||
| [127] | Waugh | 2015 | R | Increased expressions of IL6, IL8, MMP2 complex and ProMMP9; unaltered expressions of IL1b, IL2, IL4, IL10, IL12p70, IL17A, VEGF, interferon-γ, active MMP9, ProMMP2 and active MMP2 | ||
| [128] | de Girolamo | 2014 | F | Increased expressions of SCX, IL1b, IL6, IL10, TGFb and VEGF; unaltered expressions of MMP3, MMP13, COL1A1, COL3A1 and TNFa; reduced NO synthesis | ||
| [129] | Chow | 2014 | F | Increased fibrocartilage area and thickness, proteoglycan deposition, expression of SOX9 and COLII and Vickers hardness; unaltered expression of COL1 | ||
| [130] | Cinar | 2013 | R | Decreased load to failure | ||
| Decreased collagen fiber density | ||||||
| [131] | Contaldo | 2012 | R | Enhanced expressions of caspase-3, PCNA and eNOS; increase in functional angiogenetic density and total wound score | ||
| [132] | Chow | 2012 | F | Increased load to failure, new bone area and new bone volume | ||
| Increased fibrocartilage zone and ratio of bone forming | ||||||
| [133] | Yoo | 2012 | F | Increased fibrillary diameter, vascularity, fibroblast activity, lymphocyte and plasma cell infiltration, dense histocytes; transient disorganization of collagen fibers | ||
| [134] | Leone | 2012 | F | Ruptured tenocytes: decreased expressions of COL1 and SCX; unaltered COL3, tenomodulin, tenascin-C | ||
| Healthy tenocytes: increased cell proliferation and migration | ||||||
| [135] | Zhang | 2011 | F | Increased lubricine expression | ||
| [136] | Penteado | 2011 | F | Unaltered blood-vessel number | ||
| [137] | Kubo | 2010 | F | Reduced ear thickness | ||
| Increased expressions of VEGF-C and VEGF-R3 | ||||||
| Increased density of lymphatic vessels | ||||||
| [138] | Sugioka | 2010 | R | Increased introduction of NFkb decoy-FITC, activation of NFkb; decreased activation of NFkb after pretreatment with ESW+NFkb decoy-FITC | ||
| [139] | Berta | 2009 | F | Decreased viability; increased expression of TGFb1; increase in COL1 and COL3 expressions after 6 days after a primary decreased expression | ||
| [140] | Bosch | 2009 | F | Increased expressions of COL1 and MMP14; decreased expression of MMP3 | ||
| Unaltered total collagen content, disorganization of normal collagen structure; decreased percentage of degraded collagen 6 weeks after treatment after an increase 3 h after treatment | ||||||
| [141] | Han | 2009 | F | Healthy: increased expression of IL1; unaltered expressions of MMP1, MMP2, MMP9, MMP13, IL6 and IL13 Diseased: decreased expressions of MMP1, MMP13 and IL6; unaltered expressions of MMP2, MMP9, IL1 and IL13 | ||
| Decreased cell viability | ||||||
| [142] | Byron | 2009 | R | Radiographic scores, scintigraphic navicular pool phase, delayed-phase region of interest density ratios | ||
| [143] | Chao | 2008 | F | Increased total collagen concentration, NO production, expressions of PCNA, COL1, COL3 and TGFb | ||
| Decreased cell viability; increased cell proliferation | ||||||
| [144] | Wang | 2008 | F | Increased new bone formation, bone mineral status, tensile load and strength | ||
| Increased remodeling/alignment of collagen fibers, thicker and mature regenerated fibrocartilage zone | ||||||
| [145] | Bosch | 2007 | F | Unaltered DNA content, 3 h after treatment: increased GAG, total protein synthesis; 6 weeks after treatment: decreased GAG, collagen synthesis, noncollagenous protein synthesis, total protein synthesis | ||
| Unaltered total collagen content, disorganization of normal collagen structure; decreased percentage of degraded collagen 6 weeks after treatment after an increase 3 h after treatment | ||||||
| [146] | Kersh | 2006 | F | Unaltered percentage lesion, percentage disruption and gray scale, external width, fibroblast and tenocyte number, increased capillary density | ||
| [147] | Wang | 2005 | F | Increased trabecular bone around the tendons and tensile strength of tendon/bone interface, better bone/tendon contact | ||
| [148] | Chen | 2004 | F | Increased load to failure | ||
| Decreased edema, swelling, inflammatory cell infiltration; increased expressions of TGFb, IGF1, tenocyte proliferation, neovascularization and progressive tendon tissue regeneration | ||||||
| [149] | Orhan | 2004 | F | Higher force to rupture | ||
| Less adhesion formation, increased number of capillaries | ||||||
| [150] | Hsu | 2004 | F | Increased ultimate tensile load | ||
| Increased hydroxyproline concentration; decreased pyridinoline concentration; unaltered number of blast-like tenocytes (4 weeks); increased number of mature tenocytes (16 weeks) | ||||||
| [151] | Orhan | 2004 | F | Disorganization of collagen fibers | ||
| [152] | Wang | 2003 | F | Increased number of neo-vessels and expressions of eNOS, VEGF and PCNA | ||
| [153] | Maier | 2002 | F | Exposure of tendons with high intensity ESWT: increased staining affinity, nuclear and fibrillar appearance paratendon: increased thickness, edema, capillary density | ||
| [154] | Wang | 2002 | F | New capillary and muscularized vessels, newly appeared myofibroblasts; no alterations in bone matrix, bone vascularization and osteocyte activity | ||
| [155] | Johannes | 1994 | F | Decreased cell viability, no alterations in cell growth | ||
| Ref | First Author | Year | M | Morphological, Functional and Radiological Findings | ||
|---|---|---|---|---|---|---|
| Findings of Molecular Biological Examinations | ||||||
| Findings of Histological Examinations | ||||||
| [156] | Huang | 2021 | R | Decreased total contracture angle, muscle contracture angle | ||
| Decreased expressions of TGFb and HIF1a | ||||||
| Decreased proportion of collagen fiber area | ||||||
| [157] | Kenmoku | 2021 | R | Energy flux density- and total energy-dependent decrease in CMAP, unaltered CMAP latency | ||
| [158] | Park | 2020 | F | Increased print width, print area | ||
| Tendential increased expression of myelin basic protein | ||||||
| [159] | Matsuda | 2020 | F | Improved BBB locomotor function, increased withdrawal threshold, abbreviated latency of MEPs, no alterations in MEP amplitude | ||
| Increased expressions of BDNF and TRKB | ||||||
| Increased expression of BDNF, reduced myelin damage and oligodendrocyte loss, decreased axonal damage | ||||||
| [160] | Langendorf | 2020 | R | Increased expressions of MyoD and myosin | ||
| Initially higher amount of mononucleated cells; at day 7, newly formed muscle fibers with less MNCs; unaltered number of cells immunopositive for CD31 | ||||||
| [161] | Sagir | 2019 | F | Decreased EMG amplitude, increased EMG latency, improved sciatic functional index | ||
| Decreased myelin thickness, axon area and number | ||||||
| [162] | Feichtinger | 2019 | F | Improved load-to-failure testing results, intensity measurements in functional gait analysis | ||
| Unaltered expressions of stromal cell-derived factor 1, TGFb1, TGFb3 and VEGFR2 | ||||||
| [163] | Yang | 2019 | n.s. | Improved mechanical paw withdrawal threshold and thermal paw withdrawal latency | ||
| Decreased TNFa, NFkb, MMP9, IL1b, NOX1, NOX2, NOX4, oxidized protein, cleaved caspase 3, cleaved PARP, γ-H2AX, (p)-p38, p-JNK, p-ERK1/2, Nav.1.3, Nav.1.8 and Nav.1.9 | ||||||
| [164] | Mattya-szovszky | 2018 | R | Dose-dependent increase in myogenic factor 5, MyoD, PAX7 and NCAM; downregulation of these proteins at double exposure of the highest energy flux density | ||
| Increased cell viability at low energy flux densities, no alterations at higher energy flux densities | ||||||
| [165] | Yin | 2018 | F | Increased angiogenesis, decreased serum myoglobin/creatine phosphokinase | ||
| Decreased NOX1, NOX2, cleaved caspase 3, cleaved PARP, TGFb, (p-)SMAD3, ICAM1, MMP9, TNFa, NFkb, chemokine (C-C motif) ligand 5, TLR2, TLR4, IL1b, cytosolic cytochrome C, γ-H2AX; increased Bcl-2, p-SMAD1/5, BMP-2, mitochondrial cytochrome C | ||||||
| Decreased muscle-damaged/fibrosis/collagen-deposition areas | ||||||
| [166] | Shin | 2018 | R | Increased expressions of DCX, SOX2, GAP43 and MAP2 | ||
| Increased expressions of DCX, SOX2, GAP43 and MAP-2 | ||||||
| [167] | Luh | 2018 | F | Enhanced amplitude and latency of sensory nerve action potentials in combination with EMLA, compared to single EMLA and ultrasound+EMLA application | ||
| [168] | Kenmoku | 2018 | R | Decreased CMAP amplitude, unaltered CMAP latency | ||
| Irregular end plates, unchanged axon terminals and muscle fibers, increased mean interjunctional fold interval | ||||||
| [169] | Chen | 2017 | n.s. | Improved mechanical paw withdrawal threshold and thermal paw withdrawal latency | ||
| Decreased expressions of TNFa, NFkb, MMP9, IL1b, GFAP, ox42, NOX1, NOX2, NOX4, oxidized protein, γ-H2AX, cytosolic mitochondria, cleaved capase-3, PARP, p-P38, p-JNK, p-ERK1/2, Nav.1.3, Nav.1.8 and Nav.1.9 | ||||||
| Decreased expressions of p-P38+, peripherin+ cells, P38+ and NF200+ cells | ||||||
| [170] | Yahata | 2016 | F | Improved BBB locomotor score, withdrawal latency, 50% withdrawal threshold | ||
| Increased expressions of VEGF, CD31, a-SMA and 5-HT; increased area of spared white matter; decreased number of TUNEL-positive cells | ||||||
| [171] | Schuh | 2016 | F | Increased cell yield, BrdU assays, population doublings, S100b, c-Jun, GFAP and P75 expression; decreased P0 and P16 expressions, increased extracellular ATP levels immediately after application | ||
| [172] | Lee | 2016 | n.s. | Decreased knee-joint angle | ||
| [173] | Kisch | 2016 | F | Increased muscular blood flow | ||
| [174] | Lee | 2015 | n.s. | Increased ankle angles (toe off + foot contact), improved sciatic functional index | ||
| Increased expression of NT3 | ||||||
| [175] | Yamaya | 2014 | F | Improved BBB locomotor score | ||
| Increased expressions of VEGF and VEGF-receptor 1 | ||||||
| Increased NeuN-positive cells, VEGF staining | ||||||
| [176] | Fu | 2014 | F | Improved mechanical withdrawal threshold, thermal withdrawal latency | ||
| [177] | Ishikawa | 2013 | R | Transfection of POMC gene | ||
| [178] | Mense | 2013 | F | Decreased pressure pain threshold, improved locomotor activity | ||
| Increased number of PGP 9.5-IR nerve fibers | ||||||
| [179] | Hausner | 2012 | F | Increased amplitude, CMAP area | ||
| Increased number of myelinated axons, unaltered number of endoneural vessels | ||||||
| [180] | Kenmoku | 2012 | R | Decreased amplitude, unaltered CMAP latency | ||
| Decreased number of acetylcholine receptors | ||||||
| [181] | Yamashita | 2009 | R | Decreased mechanical allodynia | ||
| Increased ratio of β-endorphin-IR muscle cells and number of β-endorphin-IR muscle fibers; decreased number of CGRP-IR DRG neurons | ||||||
| [182] | Wu | 2008 | F | Decreased motor nerve conduction velocity; unaltered sciatic functional index and withdrawal reflex latency | ||
| Damage to the myelin sheath of large-diameter myelinated fibers | ||||||
| [183] | Hausdorf | 2008 | F | Decreased number of unmyelinated nerve fibers of femoral nerve; unaltered number of unmyelinated nerve fibers of sciatic nerve; unaltered size, number and myelin sheet of myelinated nerve fibers | ||
| [184] | Hausdorf | 2008 | F | Decreased number of neurons immunoreactive for substance P | ||
| [185] | Lee | 2007 | F | No changes in motor and vegetative functions | ||
| Decreased number of neurons during high-intensity treatment, dose-dependent myelin damage | ||||||
| [186] | Ochiai | 2007 | F | Increased walking duration | ||
| Decreased ratio of CGRP-positive dorsal root ganglion neurons | ||||||
| [187] | Wu | 2007 | F | Decreased motor nerve conduction velocity, unaltered sciatic functional index | ||
| [188] | Murata | 2006 | F | Increased number of ATF3 and ATF-3/GAP-43 dual-IR neurons | ||
| [189] | Takahashi | 2006 | F | Decreased number of epidermal nerve fibers | ||
| [190] | Bolt | 2004 | R | Decreased sensory nerve conduction velocity | ||
| Disruption of myelin sheet | ||||||
| [191] | Hausdorf | 2004 | F | Increased substance-P release 6 and 24 h after treatment, decreased substance-P release 6 weeks after treatment; unaltered prostaglandin-E2 release | ||
| [192] | Takahashi | 2003 | F | Decreased percentage of CGRP-immunoreactive dorsal root ganglion neurons | ||
| [193] | Maier | 2003 | F | Increased substance-P release after 6 and 24 h; decreased SP release after 6 weeks; no alterations in prostaglandin-E2 release | ||
| [194] | Haake | 2002 | F | Unaltered c Fos expression | ||
| Unaltered c Fos expression | ||||||
| [195] | Ohtori | 2001 | F | Decreased number of nerve fibers immunoreactive for PGP 9.5 and CGRP | ||
| [196] | Haake | 2001 | F | Unaltered expressions of met-enkephalin and dynorphin | ||
| [197] | Rompe | 1998 | F | Vacuolic swelling of axons, no disruption of nerve’s continuity | ||
| No. | Take-Home Message |
|---|---|
| 1 | Compared to the effects of many other forms of therapy, the clinical benefit of extracorporeal shock wave therapy does not appear to be based on a single mechanism. |
| 2 | Different tissues respond to the same mechanical stimulus in different ways. |
| 3 | Just because a mechanism of action of extracorporeal shock wave therapy was described in a study does not automatically mean that this mechanism was relevant to the observed clinical effect. |
| 4 | Focused and radial extracorporeal shock wave therapy seem to act in a similar way. |
| 5 | Extracorporeal shock wave therapy stimulates both progenitor and differentiated cells, and has positive effects on pathologies of bone and cartilage. |
| 6 | Extracorporeal shock wave therapy apparently mimics the effect of capsaicin by reducing substance-P concentration. |
| 7 | Extracorporeal shock wave therapy apparently mimics effects of injection of Botulinum toxin A by destroying endplates in the neuromuscular junction. |
| 8 | Extracorporeal shock wave therapy apparently imitates certain mechanisms of action of neural therapy. |
| 9 | Extracorporeal shock wave therapy apparently imitates certain mechanisms of manual therapy treatments. |
| 10 | Even the most sophisticated research into the effects of exposure of musculoskeletal tissue to extracorporeal shock waves cannot substitute clinical research in order to determine the optimum intensity, treatment frequency and localization of extracorporeal shock wave therapy. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wuerfel, T.; Schmitz, C.; Jokinen, L.L.J. The Effects of the Exposure of Musculoskeletal Tissue to Extracorporeal Shock Waves. Biomedicines 2022, 10, 1084. https://doi.org/10.3390/biomedicines10051084
Wuerfel T, Schmitz C, Jokinen LLJ. The Effects of the Exposure of Musculoskeletal Tissue to Extracorporeal Shock Waves. Biomedicines. 2022; 10(5):1084. https://doi.org/10.3390/biomedicines10051084
Chicago/Turabian StyleWuerfel, Tobias, Christoph Schmitz, and Leon L. J. Jokinen. 2022. "The Effects of the Exposure of Musculoskeletal Tissue to Extracorporeal Shock Waves" Biomedicines 10, no. 5: 1084. https://doi.org/10.3390/biomedicines10051084
APA StyleWuerfel, T., Schmitz, C., & Jokinen, L. L. J. (2022). The Effects of the Exposure of Musculoskeletal Tissue to Extracorporeal Shock Waves. Biomedicines, 10(5), 1084. https://doi.org/10.3390/biomedicines10051084






