Correlation between Macular Neovascularization (MNV) Type and Druse Type in Neovascular Age-Related Macular Degeneration (AMD) Based on the CONAN Classification
Abstract: Background
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Study Design
2.3. Data Collection
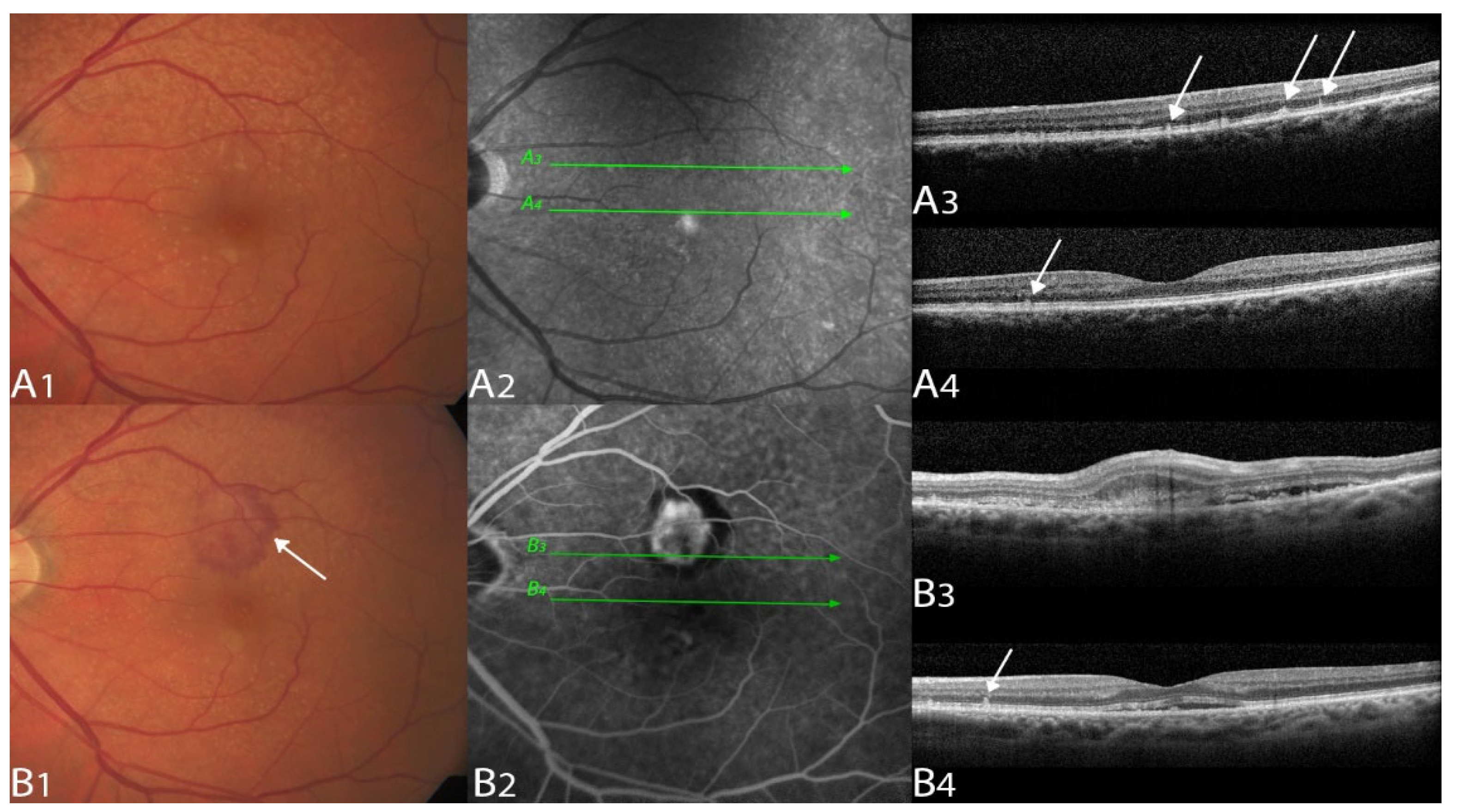
2.4. Image Grading and Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Freund, K.B.; Zweifel, S.A.; Engelbert, M. Do we need a new classification for choroidal neovascularization in age-related macular degeneration? Retina 2010, 30, 1333–1349. [Google Scholar] [CrossRef] [PubMed]
- Grossniklaus, H.E.; Gass, J.D. Clinicopathologic correlations of surgically excised type 1 and type 2 submacular choroidal neovascular membranes. Am. J. Ophthalmol. 1998, 126, 59–69. [Google Scholar] [CrossRef]
- Gass, J.D. Biomicroscopic and histopathologic considerations regarding the feasibility of surgical excision of subfoveal neovascular membranes. Am. J. Ophthalmol. 1994, 118, 285–298. [Google Scholar] [CrossRef]
- Jung, J.J.; Chen, C.Y.; Mrejen, S.; Gallego-Pinazo, R.; Xu, L.; Marsiglia, M.; Boddu, S.; Freund, K.B. The incidence of neovascular subtypes in newly diagnosed neovascular age-related macular degeneration. Am. J. Ophthalmol. 2014, 158, 769–779 e762. [Google Scholar] [CrossRef] [PubMed]
- Spaide, R.F.; Jaffe, G.J.; Sarraf, D.; Freund, K.B.; Sadda, S.R.; Staurenghi, G.; Waheed, N.K.; Chakravarthy, U.; Rosenfeld, P.J.; Holz, F.G.; et al. Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group. Ophthalmology 2020, 127, 616–636. [Google Scholar] [CrossRef]
- Mimoun, G.; Soubrane, G.; Coscas, G. Macular drusen. J. Fr. Ophtalmol. 1990, 13, 511–530. [Google Scholar]
- Zweifel, S.A.; Spaide, R.F.; Curcio, C.A.; Malek, G.; Imamura, Y. Reticular pseudodrusen are subretinal drusenoid deposits. Ophthalmology 2010, 117, 303–312 e301. [Google Scholar] [CrossRef]
- Schmitz-Valckenberg, S.; Alten, F.; Steinberg, J.S.; Jaffe, G.J.; Fleckenstein, M.; Mukesh, B.N.; Hohman, T.C.; Holz, F.G.; Geographic Atrophy Progression (GAP) Study Group. Reticular drusen associated with geographic atrophy in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2011, 52, 5009–5015. [Google Scholar] [CrossRef]
- Steinberg, J.S.; Auge, J.; Jaffe, G.J.; Fleckenstein, M.; Holz, F.G.; Schmitz-Valckenberg, S.; Group, G.A.P.S. Longitudinal analysis of reticular drusen associated with geographic atrophy in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4054–4060. [Google Scholar] [CrossRef]
- Zhou, Q.; Daniel, E.; Maguire, M.G.; Grunwald, J.E.; Martin, E.R.; Martin, D.F.; Ying, G.S.; Comparison of Age-Related Macular Degeneration Treatments Trials Research Group. Pseudodrusen and Incidence of Late Age-Related Macular Degeneration in Fellow Eyes in the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology 2016, 123, 1530–1540. [Google Scholar] [CrossRef]
- Agron, E.; Domalpally, A.; Cukras, C.A.; Clemons, T.E.; Chen, Q.; Lu, Z.; Chew, E.Y.; Keenan, T.D.L.; Areds; Groups, A.R. Reticular Pseudodrusen: The Third Macular Risk Feature for Progression to Late Age-related Macular Degeneration: Age-Related Eye Disease Study 2 Report 30. Ophthalmology, 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Zweifel, S.A.; Imamura, Y.; Spaide, T.C.; Fujiwara, T.; Spaide, R.F. Prevalence and significance of subretinal drusenoid deposits (reticular pseudodrusen) in age-related macular degeneration. Ophthalmology 2010, 117, 1775–1781. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.Y.; Dubois, L.; Tadayoni, R.; Delahaye-Mazza, C.; Debibie, C.; Quentel, G. Prevalence of reticular pseudodrusen in age-related macular degeneration with newly diagnosed choroidal neovascularisation. Br. J. Ophthalmol. 2007, 91, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Marsiglia, M.; Boddu, S.; Chen, C.Y.; Jung, J.J.; Mrejen, S.; Gallego-Pinazo, R.; Freund, K.B. Correlation between neovascular lesion type and clinical characteristics of nonneovascular fellow eyes in patients with unilateral, neovascular age-related macular degeneration. Retina 2015, 35, 966–974. [Google Scholar] [CrossRef] [PubMed]
- Cheung, C.M.G.; Gan, A.; Yanagi, Y.; Wong, T.Y.; Spaide, R. Association between Choroidal Thickness and Drusen Subtypes in Age-Related Macular Degeneration. Ophthalmol. Retina 2018, 2, 1196–1205. [Google Scholar] [CrossRef]
- Lee, J.; Kim, M.; Lee, C.S.; Kim, S.S.; Koh, H.J.; Lee, S.C.; Byeon, S.H. Drusen Subtypes and Choroidal Characteristics in Asian Eyes with Typical Neovascular Age-Related Macular Degeneration. Retina 2020, 40, 490–498. [Google Scholar] [CrossRef]
- Lee, J.; Choi, S.; Lee, C.S.; Kim, M.; Kim, S.S.; Koh, H.J.; Lee, S.C.; Byeon, S.H. Neovascularization in Fellow Eye of Unilateral Neovascular Age-related Macular Degeneration According to Different Drusen Types. Am. J. Ophthalmol. 2019, 208, 103–110. [Google Scholar] [CrossRef]
- Wightman, A.J.; Guymer, R.H. Reticular pseudodrusen: Current understanding. Clin. Exp. Optom. 2019, 102, 455–462. [Google Scholar] [CrossRef]
- Spaide, R.F.; Ooto, S.; Curcio, C.A. Subretinal drusenoid deposits AKA pseudodrusen. Surv. Ophthalmol. 2018, 63, 782–815. [Google Scholar] [CrossRef]
- Spaide, R.F. IMPROVING THE AGE-RELATED MACULAR DEGENERATION CONSTRUCT: A New Classification System. Retina 2018, 38, 891–899. [Google Scholar] [CrossRef]
- Wilde, C.; Patel, M.; Lakshmanan, A.; Morales, M.A.; Dhar-Munshi, S.; Amoaku, W.M. Prevalence of reticular pseudodrusen in eyes with newly presenting neovascular age-related macular degeneration. Eur. J. Ophthalmol. 2016, 26, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Rabiolo, A.; Sacconi, R.; Cicinelli, M.V.; Querques, L.; Bandello, F.; Querques, G. Spotlight on reticular pseudodrusen. Clin. Ophthalmol. 2017, 11, 1707–1718. [Google Scholar] [CrossRef]
- Ahmed, D.; Stattin, M.; Haas, A.M.; Graf, A.; Krepler, K.; Ansari-Shahrezaei, S. Drusen characteristics of type 2 macular neovascularization in age-related macular degeneration. BMC Ophthalmol. 2020, 20, 381. [Google Scholar] [CrossRef]
- Pauleikhoff, D.; Radermacher, M.; Spital, G.; Muller, C.; Brumm, G.; Lommatzsch, A.; Bird, A.C. Visual prognosis of second eyes in patients with unilateral late exudative age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 2002, 240, 539–542. [Google Scholar] [CrossRef]
- Lavin, M.J.; Eldem, B.; Gregor, Z.J. Symmetry of disciform scars in bilateral age-related macular degeneration. Br. J. Ophthalmol. 1991, 75, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.; Yannuzzi, L.A.; Ladas, I.D.; Guyer, D.R.; Slakter, J.S.; Sorenson, J.A. Choroidal neovascularization in second eyes of patients with unilateral exudative age-related macular degeneration. Ophthalmology 1995, 102, 1380–1386. [Google Scholar] [CrossRef]
- Mann, S.S.; Rutishauser-Arnold, Y.; Peto, T.; Jenkins, S.A.; Leung, I.; Xing, W.; Bird, A.C.; Bunce, C.; Webster, A.R. The symmetry of phenotype between eyes of patients with early and late bilateral age-related macular degeneration (AMD). Graefes Arch. Clin. Exp. Ophthalmol. 2011, 249, 209–214. [Google Scholar] [CrossRef]

| Total patients screened (nscreen) | 1990 (3980 eyes) |
| Patients identified as suitable (npatient) | 268 (536 eyes) |
| Patients removed due to fibrovascular scarring or poor image quality (ndropped) | 77 (154 eyes) (29%) |
| Patients included (npatient) | 191 (382 eyes) (71%) |
| Eyes included (1 per patient) (n) | 191 eyes |
| Localization OD/OS | 97 (51%)/94 (49%) |
| Gender female/male | 117 (61%)/74 (39%) |
| Age mean (years) ± SD | 77.9 ± 7.8 |
| BCVA mean ± SD | 56.6 ± 21.2 ETDRS letters |
| Glaucoma | 22 (12%) |
| Arterial hypertension | 92 (48%) |
| Diabetes mellitus | 17 (9%) |
| Total | MNV 1 | MNV 2 | MNV 3 | MNV Mixed 1/2 | |
|---|---|---|---|---|---|
| Eyes included (n) | 191 (100%) | 80 (42%) | 23 (12%) | 49 (26%) | 39 (20%) |
| Soft drusen only | 38 (20%) | 34 (43%) | 0 (0%) | 1 (2%) | 3 (8%) |
| Predominant soft drusen | 43 (23%) | 32 (40%) | 1 (4%) | 4 (8%) | 6 (15%) |
| SDD only | 39 (20%) | 3 (4%) | 14 (61%) | 13 (27%) | 9 (23%) |
| Predominant SDD | 71 (37%) | 11 (14%) | 8 (35%) | 31 (63%) | 21 (54%) |
| aOR | 95% CI | p | |
|---|---|---|---|
| MNV 1 | |||
| Soft drusen only | 19.0008 | 7.0019; 66.9073 | <0.0001 |
| Predominant soft drusen | 27.9873 | 13.0180; 64.5909 | <0.0001 |
| SDD only | 0.0806 | 0.01867; 0.2395 | <0.0001 |
| Predominant SDD | 0.0357 | 0.0155; 0.0768 | <0.0001 |
| MNV 2 | |||
| Soft drusen only | n.s. | n.s. | 0.8700 |
| Predominant soft drusen | 0.0427 | 0.0023; 0.2165 | 0.0025 |
| SDD only | 9.2945 | 3.6536; 24.9841 | <0.0001 |
| Predominant SDD | 23.4453 | 4.6190; 429.4434 | 0.0025 |
| MNV 3 | |||
| Soft drusen only | 0.0661 | 0.0037; 0.3243 | 0.00853 |
| Predominant soft drusen | 0.1145 | 0.0376; 0.2849 | <0.0001 |
| SDD only | n.s. | n.s. | 0.3198 |
| Predominant SDD | 8.7374 | 0.5105; 26.5916 | <0.0001 |
| MNV 1/2 mixed | |||
| Soft drusen only | 0.2816 | 0.0650; 0.8484 | 0.0455 |
| Predominant soft drusen | 0.3284 | 0.1364; 0.7268 | 0.0084 |
| SDD only | n.s. | n.s. | 0.6690 |
| Predominant SDD | 0.3284 | 0.1364; 0.7268 | 0.0084 |
| Coeff. | 95% CI | p | |
|---|---|---|---|
| MNV type vs. Glaucoma | 0.0757 | 0.0000; 0.0966 | 0.9063 |
| MNV type vs. Hypertension | 0.1153 | 0.0000; 0.1677 | 0.5471 |
| MNV type vs. Diabetes | 0.0726 | 0.0000; 0.0887 | 0.9221 |
| Druse type vs. Glaucoma | 0.0788 | 0.0000; 0.1048 | 0.8828 |
| Druse type vs. Hypertension | 0.1091 | 0.0000; 0.1321 | 0.6556 |
| Druse type vs. Diabetes | 0.1269 | 0.0000; 0.1591 | 0.4171 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muth, D.R.; Toro, M.D.; Bajka, A.; Jonak, K.; Rieder, R.; Kohler, M.M.; Gunzinger, J.M.; Souied, E.H.; Engelbert, M.; Freund, K.B.; et al. Correlation between Macular Neovascularization (MNV) Type and Druse Type in Neovascular Age-Related Macular Degeneration (AMD) Based on the CONAN Classification. Biomedicines 2022, 10, 2370. https://doi.org/10.3390/biomedicines10102370
Muth DR, Toro MD, Bajka A, Jonak K, Rieder R, Kohler MM, Gunzinger JM, Souied EH, Engelbert M, Freund KB, et al. Correlation between Macular Neovascularization (MNV) Type and Druse Type in Neovascular Age-Related Macular Degeneration (AMD) Based on the CONAN Classification. Biomedicines. 2022; 10(10):2370. https://doi.org/10.3390/biomedicines10102370
Chicago/Turabian StyleMuth, Daniel Rudolf, Mario Damiano Toro, Anahita Bajka, Kamil Jonak, Roman Rieder, Myrtha Magdalena Kohler, Jeanne Martine Gunzinger, Eric H. Souied, Michael Engelbert, K. Bailey Freund, and et al. 2022. "Correlation between Macular Neovascularization (MNV) Type and Druse Type in Neovascular Age-Related Macular Degeneration (AMD) Based on the CONAN Classification" Biomedicines 10, no. 10: 2370. https://doi.org/10.3390/biomedicines10102370
APA StyleMuth, D. R., Toro, M. D., Bajka, A., Jonak, K., Rieder, R., Kohler, M. M., Gunzinger, J. M., Souied, E. H., Engelbert, M., Freund, K. B., & Zweifel, S. A. (2022). Correlation between Macular Neovascularization (MNV) Type and Druse Type in Neovascular Age-Related Macular Degeneration (AMD) Based on the CONAN Classification. Biomedicines, 10(10), 2370. https://doi.org/10.3390/biomedicines10102370






