1. Introduction
In Australia, approximately 2.3% of high-school-aged young people identify as trans or gender diverse (hereafter ‘trans’) (
Fisher et al. 2019). For a subset of these trans youth, incongruence between their experienced gender and their sex assigned at birth can result in significant distress, known as gender dysphoria (
American Psychiatric Association 2013). Australian standards of care and guidelines for treatment in adolescence provide that appropriate treatment can consist of puberty blockers, gender-affirming hormones, and, in some cases, surgery (
Telfer et al. 2021). Australian legal requirements for obtaining valid consent to these treatments can, however, result in significant barriers to treatment. The development of Australian law concerning consent for the medical treatment of trans youth has been slow, haphazard, and remains incomplete. Most notably, Australian law articulating the process for obtaining lawful consent and access to treatment has fallen behind medical knowledge (
Jowett 2022), creating tangible harm for trans youth and families forced to navigate the corridors of the Family Court (
Kelly 2016).
For more than 15 years, medical treatment for trans youth was considered a ‘special medical procedure’ and thus outside the bounds of parental responsibility. Family Court approval was needed before treatment could proceed. However, in 2017, the decision of the Full Court in
Re: Kelvin removed the label of ‘special’ from gender-affirming hormone treatment, meaning that it was no longer necessary for families to appear before the Family Court to obtain approval for treatment.
1 It was also understood by the medical and legal communities that, where a young person was assessed as competent by their treating medical team, it was no longer necessary to obtain parental consent for treatment. However, the 2020 trial decision of
Re: Imogen provided a different interpretation. In
Re: Imogen, Watts J held that
both parents must consent before any gender-affirming medical treatment can occur, even where the young person is assessed as competent.
2 It was also held that, where there is any disagreement between parents about treatment, the matter should come before the Family Court.
This article explores the implications of the decision in
Re: Imogen for trans youth and their families and proposes possible models for reform. It starts by providing the background to
Re: Imogen and explaining the current legal position. It then explores why the law needs to be reformed, highlighting the inconsistent approach to competency in Australian law and the harm the current law does to trans youth. Finally, it explores models for reform. Building on critiques of the law in this area (
Jowett and Kelly 2021;
Jowett and Mathews 2020;
Bell 2015;
France 2014;
Kelly 2014;
Dimopoulos and Taylor-Sands 2021), it reviews various options for law reform and suggests an optimal model.
2. Special Medical Procedures and Trans Youth: From Re: Alex to Re: Imogen
The law on special medical procedures was conceived of in the High Court of Australia’s decision in
Secretary, Department of Health & Community Services v JWB and SMB (Marion’s Case) as a procedural safeguard to protect intellectually disabled young people from non-therapeutic sterilisations maligned with their best interests.
3 Special medical procedures lie outside the bounds of treatments that parents can lawfully consent to within their ‘parental responsibility’.
4 Court approval is required under the Family Court’s welfare jurisdiction, which empowers the Court to make orders relating to the welfare of children, having regard to ‘the best interests of the child’ as ‘the paramount consideration’.
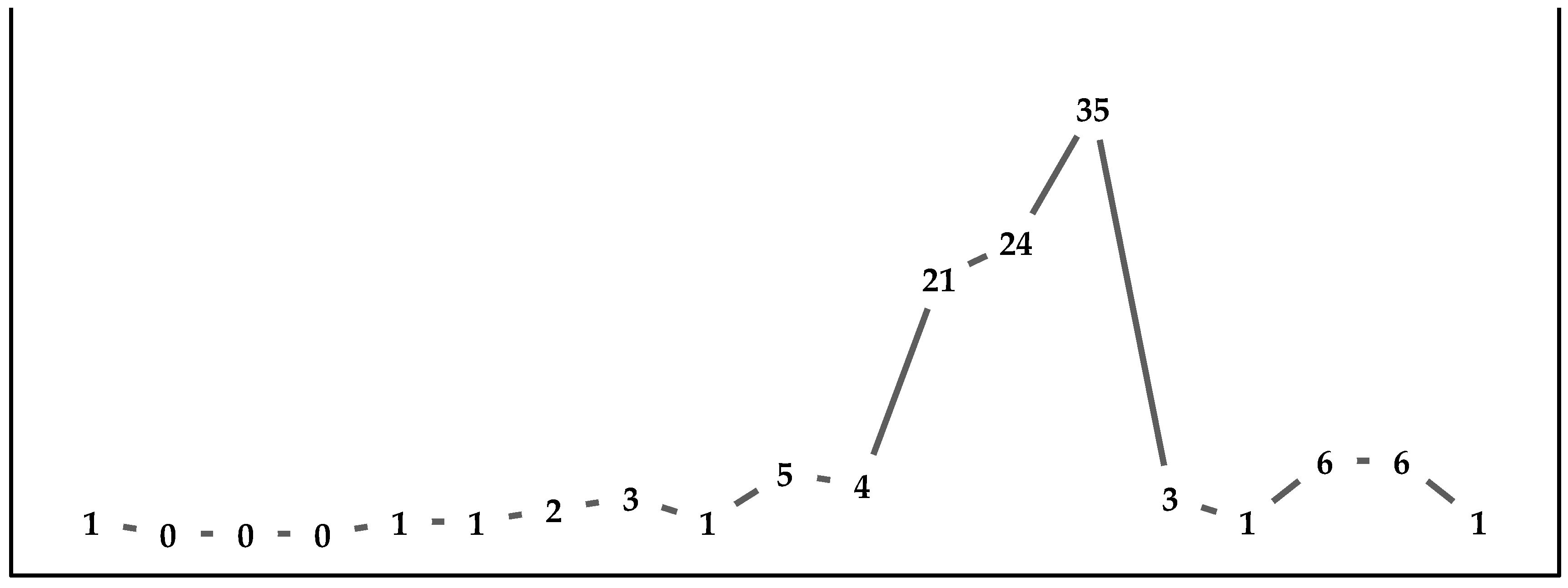
5Cases concerning medical treatment for trans youth have regularly appeared in the Family Court since 2004, peaking with 35 matters in 2017 (see
Figure 1). Because of its designation as a special medical procedure, between the 2004 case of
Re: Alex and 2013, all gender-affirming medical interventions for trans youth, including puberty blockers, gender-affirming hormones and surgery, required Family Court approval.
6 However, following the 2013 decision of the Full Court of the Family Court of Australia in
Re: Jamie, this requirement was lifted for puberty blockers, as they were stripped of their classification as a special medical procedure, but it was retained for gender-affirming hormones and, impliedly, surgery.
7 Additionally, any young person seeking to provide their own consent to any treatment was required to be assessed as competent by the Court, rather than their doctor as normally occurs in medical practice.
As noted above, in 2017, the decision of the Full Court in
Re: Kelvin removed the requirement for court approval to commence gender-affirming treatment. It was also presumed to have removed the requirement that parental consent be obtained when a child is assessed as competent. Medical guidelines were developed to reflect this new position (
Telfer et al. 2018b). However, in
Re: Imogen, Watts J held that parents must consent to all gender-affirming medical treatment, even where the young person is assessed as competent. It was also held that where there is any disagreement between parents about treatment, the matter should come before the Family Court. This was because both parents must consent to treatment, a practice that the medical community followed in most instances but sometimes dispensed with where a parent posed a risk to the child or the other parent or could not be located (
Kelly et al. 2022).
The decision in
Re: Imogen sent ripples through the medical community. Following
Re: Kelvin, the Australian Standards of Care and Treatment Guidelines for Trans and Gender Diverse Children and Adolescents had been published and endorsed by the Australian Professional Association for Trans Health, the leading national body for professionals involved in the health, rights and wellbeing of trans people—binary and non-binary (
Telfer et al. 2018b). The Guidelines, which were intended to reflect the decision in
Re: Kelvin, stated that, while obtaining consent from parents or guardians before gender-affirming hormone treatment commences is ideal, parental consent is not required when the adolescent is found to be competent. In practice, this meant that, while the consent of both parents was typically secured, where one parent was uninvolved in a competent child’s life or was passively unsupportive, consent was not actively pursued. Thus, it was not uncommon for a doctor to prescribe hormone treatment to a competent trans young person without the express consent of a parent or guardian, and it was presumed that this protocol complied with the law as laid down in
Re: Kelvin. However, in
Re: Imogen, Watts J stated that the treatment guidelines were incorrect; the consent of
both parents was always needed, and, in the case of disagreement between parents, Family Court approval was required. This means that at least some trans youth will find themselves back in the Family Court, even in circumstances where they themselves have been found to be competent to consent.
3. A Case for Reform
There is widespread agreement that the law needs reform, even more so since the decision in
Re: Imogen. Judges involved in these matters have been vocal in their frustration that these cases continue to come to the Family Court (
Bannerman 2014;
Strickland 2014,
2015).
8 Medical practitioners have voiced concern about the law’s impact on trans youth’s health and wellbeing, as well as on their finite clinical resources (
Hewitt et al. 2012;
Telfer et al. 2018a). Legal academics have critiqued the law, highlighting its myriad inconsistencies and failings as well as the economic barriers presented by mandatory Family Court involvement (
France 2014;
Kelly 2014;
Bell 2015;
Jowett and Kelly 2021;
Dimopoulos and Taylor-Sands 2021). Legal barriers to gender-affirming care ‘threaten the health, well-being, and survival of transgender children and young adults’ (
Martin et al. 2021).
Clearly there has been an impetus to bring cases to court in this area, with accompanying optimism for reform. However, this has historically been minimally successful and often only for the young person the subject of the proceedings; anddespite the precedential effect these judgements have on the broader trans community, their support systems, and their healthcare teams. A blunt but apt narrative description of the gender dysphoria case law in Australia is that it has been a game of whack-a-mole for all involved. Every time a judgement is purported to cover the law—or is hoped to by those impacted by it—it does not. By way of example, in 2017, legal advice was given to clinicians at the Royal Children’s Hospital (RCH) in Melbourne that
Re: Kelvin meant that getting the consent of both parents was not necessary for treatment to proceed. The judgement was celebrated for improving access to medical treatment and upholding the rights of trans youth (
Telfer et al. 2018a;
Australian Human Rights Commission 2017;
Fraser and Condello 2017;
Feldman and Dreyfus 2017;
McAllister 2018;
Human Rights Law Centre 2017). The RCH has since had to change its approach following the
Re: Imogen decision, in which Watts J stated that the approach being taken at that hospital was incorrect.
More recently, a more extreme approach was taken by the Perth Children’s Hospital,
9 which was advised to require court applications for
all forms of treatment for trans youth due to the
Bell decision in England (
Pascual Juanola 2021). In that case, the High Court of England and Wales put forth that there would be ‘enormous difficulties in a child under 16’ understanding and weighing the information required to decide whether to consent to puberty blockers.
10 In the High Court’s view, ‘where the consequences of the treatment are profound, the benefits unclear and the long-term consequences to a material degree unknown, it may be that
Gillick competence cannot be achieved, however much information and supportive discussion is undertaken.’
11 As a result, the Court proffered that ‘[g]iven the long-term consequences of the clinical interventions at issue in this case, and given that the treatment is as yet innovative and experimental, we recognise that clinicians may well regard these as cases where the authorisation of the court should be sought prior to commencing the clinical treatment’.
12 While the Perth Children’s Hospital has now retreated from this position, and the
Bell decision was reversed on appeal,
13 there is ongoing concern among doctors in the field that the rules may change at any time.
The impetus for reform is clear. Alongside harm to young people, court involvement has strained the medical and family systems that support trans youth (
Kelly 2016). The uncertainty of the law has created volatility in clinical practice, while also requiring significant resources that could be spent elsewhere. This is because clinicians must spend considerable time, diverted from their clinical practice, preparing evidentiary reports for court hearings. This is apt to consider at a time when, during a global pandemic, healthcare resources are limited. In addition, there is no suggestion that Family Court involvement had served any significant legal or medical function. A review of case law in the Family Court between 2004 and 2022 reveals that judges have never taken a position contrary to the advice of treating medical practitioners. Continuing Family Court involvement in decision making in this context makes little sense. It is therefore our view that the appropriate response to the issue is legislative. The benefit of legislative reform is that all stakeholder concerns can be considered, and the law can be specifically crafted to respond to trans youth.
4. Minors and Consent to Medical Treatment: What Does the Law Say?
Currently, the Australian legal framework pertaining to minors and consent to medical treatment is comprised of legislation sitting alongside the common law, including a patchwork of decisions by single judges of the Family Court of Australia and two Full Court judgments. Consent for medical treatment is necessary at law to transform something that would otherwise be unlawful into accepted conduct, the absence of which would ordinarily be considered assault.
14 This legal principle stems from the long-recognised right to bodily inviolability or bodily integrity.
15 The requirement for consent is generally uncontroversial where a competent adult is concerned. However, by virtue of their status as minors, children are generally presumed to be unable to consent to their own medical procedures.
16With the exception of South Australia, the age of medical decision making is set by state and territory legislation on the age of majority, age 18, and does not otherwise address children’s capacity to consent below this age.
17 However, in South Australia, the consent given at the age of 16 years or over is as effective as that of an adult.
18 In New South Wales, legislation provides that the consent given by a young person aged 14 and over is sufficient as a defence to a claim of assault and battery, but it has not been interpreted as creating a positive power to give consent at that age.
19 Below the legislative ages of medical decision making, the common law determines whether a young person has the capacity to make their own health decisions. As a general rule, parents are empowered to give consent on behalf of their child by virtue of their parental responsibility derived from the
Family Law Act 1975 (Cth) (‘
Family Law Act’), the common law, and the criminal code.
20The 1992 High Court decision in
Marion’s Case confirmed that young people in Australia can be competent under the common law when they satisfy the precepts of
Gillick competence.
21 Gillick competence is derived from a decision of the United Kingdom House of Lords.
22 In
Gillick, the House of Lords ruled that a young person can be competent to consent to their own healthcare ‘if and when the child achieves sufficient understanding and intelligence to enable him or her to understand fully what is proposed.’
23 South Australia has adopted a version of this principle in its legislation, which provides that, for those under the age of 16, a medical practitioner can administer medical treatment with the child’s consent when they, and another medical practitioner, are of the opinion that: (1) ‘the child is capable of understanding the nature, consequences and risks of the treatment’; and (2) ‘the treatment is in the best interest of the child’s health and well-being’.
24Alongside general principles, a considerable body of case law specifically addresses the lawfulness of consent given by parents and young people to gender-affirming medical treatment. In
Marion’s Case, the High Court was concerned with the non-therapeutic sterilisation of an intellectually disabled child, but indicated wider applicability of the principles to other treatments.
25 The majority in
Marion’s Case outlined the factors present in a non-therapeutic sterilisation case that necessitates it residing outside the scope of parental authority, including that:
The procedure is non-therapeutic in nature;
The procedure is major, irreversible, and invasive;
There is a significant risk of the wrong decision being made, regarding either the child’s present or future capacity to consent, about the best interests of a child who cannot consent, particularly in circumstances where there are independent and possibly conflicting interests of the parents or medical staff in relation to those of the child; and
Grave consequences would flow were a wrong decision made about treatment.
In the 2004 case of
Re: Alex, Nicholson CJ determined that puberty blockers and gender-affirming hormones gave rise to similar concerns and that, accordingly, court approval was required before these treatments could go ahead. This conclusion derived from the legal interpretation of what constitutes therapeutic treatment, with his Honour deciding that, as the aetiology of diverse gender identity had not been definitively established, treatment for gender dysphoria could not be said to ‘cure a disease or correct a malfunction’ and was therefore non-therapeutic in nature.
26In 2013, the law changed substantively when the Full Court in
Re: Jamie held that, because puberty blockers are a reversible form treatment and do not pose significant risk, parents could consent without any court oversight. However, gender-affirming hormones remained a special medical procedure requiring court approval, unless the young person themselves was capable of consenting. The Full Court held, however, that it was the Court, rather than clinicians, who made the competency assessment.
27 The effect of this approach was that all young people seeking hormone treatment needed to make an application to the Family Court.
In the 2017 decision of
Re: Kelvin, the law shifted again as the Full Court moved gender-affirming hormones out of the ‘special medical procedure’ category.
28 Following
Re: Kelvin, parents can consent to hormone treatment, and, where the parents, the young person, and the clinicians all agree about the treatment, the Court no longer has a role to play in determining
Gillick competency.
29 The justification for the change was the desire to align the law with the current state of medicine,
30 which indicated that less risk attends contemporary treatment decisions because: (i) clinicians are now guided by Australian-specific clinical guidelines;
31 (ii) there is evidence of positive outcomes for those who receive treatment; and (iii) there is evidence that not treating a young person with gender dysphoria increases risk.
32 However, by limiting the removal of court approval to situations where parents, doctors, and a competent young person are in agreement, the Full Court left open the opportunity for ongoing Family Court involvement.
In the 2020 case of
Re: Imogen, Watts J held that, in cases where both parents do not provide consent to treatment, a court application is required.
33 This is the case even when the young person’s treating doctors believe them to be
Gillick-competent. Following
Re: Imogen, young people may only consent to treatment without court oversight where there is no dispute about: their
Gillick-competence; the diagnosis of gender dysphoria; or the proposed treatment. The legal basis for this requirement is unclear, as no forms of gender-affirming medical treatment are considered special medical procedures, and there was no indication in
Marion’s Case that there are types of medical treatment to which the principles of
Gillick competency do not apply.
Piecemeal changes to the legal framework are inadequate. As
Young (
2019) has suggested, cases concerning medical treatment for trans youth ‘continue to reflect a broader underlying failure by the courts to recognise and respect decisions of mature, competent minors, and fail to engage more deeply with the question of the right of mature minors to decision-making autonomy’. The remainder of this article will consider how the law might be reformed.
5. Contemporary Views on Reform
The Australian legal framework has been subject to significant criticism by legal scholars, medical practitioners, and judges. While the vast majority of critiques by legal scholars engage with issues of legal interpretation of the relevant case law, some venture an opinion on how the law should be reformed.
Bell (
2015, p. 453) observes that ‘[t]he Court’s expansion of its jurisdiction to encompass treatment for gender dysphoria is not fulfilling its stated function of protecting children. Rather, it is causing further distress and harm’. Accordingly, she opines that ‘[f]or legal, medical and social reasons, it would be preferable for the court to revise its approach to gender dysphoria cases and leave this area of decision-making to young people, their families and the medical professionals advising them’ (
Bell 2017, p. 144).
Bell and Bell (
2017, p. 247) aptly cite
Smith v Smith, where the court noted that ‘there are severe limitations in using the judicial system to resolve complex and possibly controversial childrearing and childhood mental health issues’.
France (
2014, p. 246) is similarly in favour of reform through legislation, arguing that ‘[t]he state of medical knowledge has developed to a point where thorough diagnosis provides more than adequate protection for a child’s best interests, arguably better than any protection afforded by the courts’. She notes that ‘[t]he requirement for families of transgender minors to gain court authorisation in order to consent to cross-sex hormone treatments for their child is out of step with the practice in comparable foreign jurisdictions, arguably inconsistent with the common law position in Australia, and against the best interests of transgender children’ (
France 2014, p. 247). In her view, though it poses some difficulties, ‘legislative reform may provide the clearest statement of the law’ (
France 2014, p. 247). This position is also taken by the authors of this article elsewhere (
Jowett and Kelly 2021;
Dimopoulos and Taylor-Sands 2021).
A minority of legal academics is in favour of increased barriers, though not all support judicial oversight. Reviewing the medical evidence regarding the side effects of puberty blockers and gender-affirming hormones,
O’Connor and Madden (
2019) argue that ‘[t]he swing away from oversight by the courts may warrant some reversal, given the subtleties of the medical evidence on the effects of [gender dysphoria] treatment upon which a determination of best interests of a child is based’. Other legal academics have pointed to the importance of providing care only where strict diagnostic criteria, established by a multidisciplinary team, have been met. For example, Patrick Parkinson has argued that blockers and hormone treatment must be a response
only to a clinically diagnosed disorder that is diagnosed after proper assessment. He argues that
Re: Kelvin and
Re: Imogen indicate that assessment and treatment should be conducted by a multidisciplinary team in accordance with internationally recognised standards and guidelines. Parkinson therefore argues that the informed consent model of care, whereby a primary care doctor prescribes treatment without a formal assessment by a mental health practitioner (
Ashley et al. 2021), is unlawful (
Parkinson 2021).
Judges themselves have also expressed support for reforms that remove judicial oversight of medical treatment. Justice Strickland, writing extra-judicially, aptly noted that the ‘pace of appellate jurisprudential development will be leisurely. This leads inexorably to the view that legislative intervention in the arena of young people’s consent to medical treatment is required’ (
Strickland 2015). Accordingly, His Honour put out a call to parliament:
In the face of increasing numbers of young people identifying as gender diverse, and demanding treatment services, it is time that the legislature took responsibility for developing a sensitive, humane and practical system for decision making around their access to potentially life-saving medical treatment.
In
Re: Martin, Bennett J highlighted the redundancy of the law, opining that, in court competency assessments, ‘[i]t is difficult to see, in reality, what the court will do other than to approve of the treatment explained and recommended to it by competent and qualified clinicians.’
34 Speaking to the media, former Chief Justice of the Family Court, Diana Bryant, said that she would ‘like to see the High Court have the opportunity to examine these kinds of cases, these gender identity cases and to decide whether or not the court has to be involved at all’ (
Bannerman 2014). In
Re: Lucas, Tree J noted the slow pace of the development of the common law and that, in his view, ‘there is an urgent need for statutory intervention in order to undo the consequences of
Re Jamie. The sooner that children … and their families do not have to endure the ordeal of litigation in order to get on with their lives, the better.’
35Trans youth have had limited voice in the development of the law (
Dimopoulos 2022). However, Georgie Stone, the subject of the decision in
Re: Jamie, was quoted in the media at age 14 as saying, ‘I don’t think it’s necessary that we have to go back to the court so they can decide if I’m
Gillick competent, ‘cause that’s just up to the parents and doctors I think’. In her view, ‘[t]hey will make just as good a decision as anybody, even better because they’re the experts’ (
Bannerman 2014). In a letter to the judge in
Re: Jamie, she wrote: ‘it frustrates me deeply that I have to go to court to be who I am. It frustrates me that anyone has to endure this. It shouldn’t be the court’s decision. It is my body and I have the right to decide what goes into it.’
36Clinicians working in the field have also been vocal in their criticism of the court approval process. They point to the ill-effects of court intervention that they see in their clinical practice, as well as the patients who never access treatment because of the barriers. Dr Telfer, a clinician and lead author of the
Australian Standards of Care and Treatment Guidelines for Trans and Gender Diverse Children and Adolescents, points out that ‘[i]t’s a highly distressing pathway that is very pathologising, very invasive and potentially very costly’ (
Legge 2015, p. 16). As she explains, a requirement for court approval proves so prohibitive for some that they simply cannot access healthcare, ‘[t]hey have to suffer the down sides for mental health and peer relationships of waiting until they turn 18.’ (
Legge 2015, p. 16). Hewitt et al. have also argued against court involvement because ‘the financial burden of legal involvement is borne by the family and the process itself can be extremely stressful, some families have elected not to pursue hormone treatment, simply to avoid the complicated and costly legal process’ (2012, p. 578). They also note that the court process may actually reduce the robustness of the diagnosis, insofar as ‘a young person observing the distress that court application causes for the parents may feel uncomfortable expressing any doubts they have regarding hormone treatment’ (p. 578). The effects of legal barriers are not insignificant. As Telfer et al. argue, barriers to accessing treatment in the Australian legal system can be expected to result in ‘an ongoing rise in morbidity and mortality amongst transgender youth’ (
Telfer et al. 2015).
The Australian Professional Association for Trans Health (AusPATH) advanced, in their position statement on
Re: Imogen, that they are ‘disturbed’ by the Family Court’s finding that
Gillick-competent youth who have a disputing parent must apply to the Family Court to access gender-affirming treatment and that clinicians cannot commence treatment without first receiving the consent of
both parents (
AusPATH 2020). It is AusPATH’s view that the
Re: Imogen judgment ‘contradicts the principle that the child’s best interests are paramount’. In their view, the judgement
will cause distress across the trans community, to families with trans children, and to the medical professionals and teams providing care to young people seeking such medically necessary care; means that many trans young people will face uncertainty and delays to medically necessary treatment, and their families will face significant or prohibitive costs and, in the cases of an absent or unsupportive parent, a time-consuming court process; and places an additional burden on medical practitioners providing gender affirming healthcare by requiring additional, often complex, processes with families and by being forced to advocate in court for their patients.
AusPATH is in favour of ‘resolutions in the law that advance and protect the best interests, rights and health of trans young people in Australia, and make it possible for the medical practitioners to provide the medically necessary gender affirming treatment and care’ (
AusPATH 2020). In their view, this should be accomplished through legislative reform, preferably via an amendment to the
Family Law Act. This view was echoed by the Sexual Health Society of Queensland, who agreed with AusPath’s call for Parliament to consider amending the
Family Law Act. The Society ‘urges the Family Court of Australia to allow for the provision of lifesaving, gender-affirming hormone therapy…to
Gillick competent trans and gender diverse…minors with the support of their transgender health expert team without the interference of the Family Court or any parent, similar to all other lifesaving paediatric treatments’ (
Sexual Health Society of Queensland 2020).
While not specifically pointing to law reform concerning adolescents, in 2021, the Australian Medical Association acknowledged the health inequities experienced by LGBTQIA+ people and called on the Australian Government to ‘[e]nhance access to beneficial gender-affirming treatment that people who are trans and gender diverse have given consent for’ (
AMA 2021). In the case of trans young people, this requires law reform.
6. What Values Should Underpin Legislative Reform?
Ferguson (
2015, p. 142) has argued that different legal decision-making frameworks for matters affecting children—such as a rights-based approach, a welfare approach, or an approach that focuses on the ‘duties’ that adults owe to children—are ‘simply tools—language descriptors, ways of framing individual considerations, processes and frameworks—for working with the same substantive content’. Given the harmful practical effects of court intervention on trans youth, in our view, the values that underpin such ‘framing’ are significant and must be clearly articulated.
It is our view that legislative reform must be underpinned by a rights-based approach that recognises and respects the evolving autonomy and agency of trans young people to make decisions about their bodies and identities. The nexus between rights and autonomy in this context is that ‘[t]o respect a child’s autonomy is to treat that child as a person, and as a rights-holder’ (
Freeman 1994, p. 323). We take ‘autonomy’ to embrace a young person’s ‘freedom to decide what shall and shall not be done with their body’
37 and their ‘right to be the (part) author of [their] own biography’ such that they ‘can demand that [their] decisions and actions should be respected (in the sense that they are ‘none of your business’) both by social convention and state law’ (
Rossler 2018, p. 138).
To date, court involvement in medical treatment for trans youth has been characterised by a paternalistic approach to the assessment of ‘the best interests of the child’ as ‘the paramount consideration’ in each case. In Re: Alex, Nicholson CJ described the Family Court’s welfare jurisdiction as:
… a protective jurisdiction. It is paternalistic and, in modern thinking about children and young people, must be understood with regard to their rights.38
Former Family Court Chief Justice Diana Bryant has made a similar, extra-curial observation that ‘the “best interests” test is by its very nature paternalistic and protective’ (
Bryant 2009, p. 199). The dominant ‘welfare’ approach to medical treatment for trans youth, underpinned by the ‘best interests’ principle, has involved adults (judges) exercising the power to determine the nature and content of trans young people’s best interests.
39 Court intervention has been driven by assumptions about trans young people’s unique vulnerability and irrationality, and by a purported need to ‘safeguard[] children including … where decisions are sought to be made by loving and caring parents’.
40 Yet, as we have articulated above, court intervention in the medical treatment of trans young people has harmed them rather than helped them.
A rights-based approach stands in contrast to this welfare-based approach in that it requires that children and young people are recognised and respected as active subjects with evolving capacities for decision making (
Dimopoulos 2022). As
Fortin (
2009, p. 402) has argued, ‘[c]hildren’s rights should not be lost somewhere…between parental, medical and judicial paternalism’. A rights-based approach must have a ‘coherent…intellectual foundation’ (
Tobin 2013, citing
Minow 1995) that appreciates
which rights of trans young people have been undermined by court involvement in the medical treatment process and
why those rights are worthy and capable of protection. We submit that this approach should be underpinned by the
United Nations Convention on the Rights of the Child (
1989) (‘
CRC’) as an express normative and legal framework.
While the
CRC has not been incorporated into Australian domestic law, the High Court of Australia has held that, where there is ambiguity in legislation, courts should favour a construction that aligns with Australia’s obligations under a treaty or international convention to which Australia is a party, because Parliament, prima facie, intends to give effect to Australia’s obligations under international law.
41 Some legislation at the federal,
42 state
43, and territory
44 levels in Australia expressly identifies that an object or principle of the legislation is to give effect to Australia’s obligations as a party to the
CRC or to enact provisions that are consistent with the
CRC.
The preamble to the
CRC highlights children’s vulnerability and need for ‘special protection’. However, two substantive provisions particularly promote an understanding of children as ‘active participant[s] in the promotion, protection and monitoring of their rights’ (
UNCRC Committee 2006, [14]). Article 5 provides that States must respect the responsibilities, rights and duties of a child’s parents or other caregivers to provide ‘appropriate direction and guidance’ in the child’s exercise of their rights, ‘in a manner consistent with the evolving capacities of the child’. Significantly, the notion of ‘evolving capacities’ in Article 5 is ‘positive and enabling’, recognising that children progressively acquire ‘competencies, understanding and increasing levels of agency’ that enable them ‘to take responsibility and exercise their rights’ (
UNCRC Committee 2016, [17]–[18]).
Article 5 of the
CRC therefore serves to promote children’s increasing agency and autonomy in the exercise of their rights as they mature and develop (
Varadan 2019;
Tobin and Varadan 2019). It has been interpreted to require ‘a transfer of responsibility for decision-making from responsible adults to children, as the child acquires the competence and … willingness to do so’ (
Lansdown 2005, p. 4). In practical terms, the evolving capacities principle means that ‘best interest-based intervention’ by adults, such as the restriction on
Gillick-competent trans youth who have unsupportive parents imposed by the Family Court in
Re: Imogen, is unjustifiable where a young person is found to have reached a level of maturity or competency on a matter equivalent to that expected of an adult (
Tobin 2013, p. 429).
The other
CRC right that we argue must be embraced by legislative reform is the child’s right to express their views and to be heard in decision making. Article 12(1) of the
CRC gives children who are capable of forming a view the right to express their views in all matters affecting them, with the child’s views to be given due weight in accordance with the child’s age and maturity. Article 12(2) gives children the opportunity be heard in judicial and administrative proceedings affecting them, either directly or through a representative or an appropriate body. Together, the rights under Articles 5 and 12 of the
CRC recognise children ‘as having agency and as having a voice that must be listened to’ (
Archard 2004, p. 58).
However, a rights-based approach to young people’s evolving autonomy does not serve to ‘drive a wedge between children and their parents’ (
Tobin 2016, p. 58). Rather, the
CRC adopts a relational (rather than an individualistic) understanding of autonomy (
Herring 2013,
2014). A rights-based approach recognises the importance of the child’s family in decision making and ‘makes it clear that children’s interests are best served when they enjoy a strong and supportive relationship with their parents’ (
Tobin 2016, p. 58). This is consistent with the clinical treatment guidelines for trans young people’s healthcare, which emphasise the importance of providing support to both the young person and their family (
Telfer et al. 2021, p. 9;
Coleman et al. 2012). It is worth noting that the concept of autonomy is also not foreign to clinical treatment guidelines for trans healthcare. The Australian Guidelines recognise ‘the negative contribution treatment delay may have on an adolescent’s sense of autonomy and agency’ (
Telfer et al. 2021, p. 17). In the UK, an objective of the National Health Service (NHS) Service Specification for the Gender Identity Development Service is ‘to promote the development of autonomy’ and to ‘affirm the importance of each person to develop autonomy in relation to treatment decisions’ (
NHS England 2017, p. 24).
Importantly, an approach to legislative reform that respects trans young people’s evolving autonomy accords with the
Gillick principle. Lord Fraser in
Gillick noted that ‘[i]n practice, most wise parents relax their control gradually as the child develops and encourage him or her to become increasingly independent.’
45 Similarly, Lord Scarman observed that:
If the law should impose on the process of ‘growing up’ fixed limits where nature knows only a continuous process, the price would be artificiality and a lack of realism in an area where the law must be sensitive to human development and social change.46
As we explain further below in canvassing various reform options, age-based presumptions of capacity are problematic, for ‘autonomy does not depend on the stage of life that a person has reached’ (
Freeman 1994, p. 322). Rather, legislative reform must recognise that children’s various capacities develop as children mature with age—but not necessarily in a linear fashion (
Lansdown 2005;
Tobin and Varadan 2019). Legislative reform that is guided by the rights under Articles 5 and 12 of the
CRC would acknowledge and respect the evolving capacities of trans young people, their right to meaningfully participate and to be heard in decision making regarding their medical treatment, and the role of adults (parents, caregivers, treating medical practitioners) to support and enable young people’s evolving autonomy.
7. Options for Reforming the Law
One option that could reduce the need for, and the confusion over, competency assessments would be to legislate an age of medical decision making of 16 years. Like the current South Australian statute, such a legislative provision would provide that the consent given by those aged 16 years and older is as effective as that of an adult. The clarity of a status-based approach would reduce clinical discretion and potential inconsistency. It would also align Australia with overseas jurisdictions such as the United Kingdom and New Zealand, where age 16 is the statutory age of medical decision making.
47Several law reform bodies in Australia have considered and made recommendations as to whether the age of medical decision making in Australian states should be below the age of 18. Inquiries in South Australia and Western Australia recommended that young people acquire the ability to consent to their medical treatment at age 16 as though they were of full age (
South Australia Working Party on Consent to Treatment 1983;
Western Australia Law Reform Commission 1988). However, only the South Australian recommendation was made law.
48Recognising that 16 is an age at which a young person is legally able to engage in a number of new activities, such as consent to sex and drive a car, and that this is the legal age of medical decision making in a number of overseas jurisdictions, the South Australian Working Party concluded that 16 was an age at which a young person could appropriately assess information and make a decision based on that information (
South Australia Working Party on Consent to Treatment 1983). We consider that extending this autonomy to medical decision making is appropriate. It is established in the medical literature that young persons aged 16 and over are typically well placed to make decisions concerning their medical treatment. For example, Weithorn and Campbell, in their landmark 1982 study, found that young people aged 14 years were as competent medical decision makers as adult participants (
Weithorn and Campbell 1982). In summarising recent research on the adolescent brain,
Steinberg (
2013) notes that:
Adolescents are indeed less mature than adults when making decisions under conditions that are characterized by emotional arousal and peer pressure, but adolescents aged 15 and older are just as mature as adults when emotional arousal is minimized and when they are not under the influence of peers, conditions that typically characterize medical decision-making.
Unlike a presumption of capacity, the New South Wales Law Reform Commission recommended that legislation provide that ‘a young person who is aged 16 or over is presumed to be competent to make a decision about his or her health care’ but that the presumption could be rebutted if ‘in the opinion of the health practitioner, the young person does not understand the information that is relevant to making a decision about the healthcare and does not appreciate the reasonably foreseeable consequences of the decision’ (
New South Wales Law Reform Commission 2008, p. 127). That recommendation was never acted upon.
Whether it is a presumption of capacity (like that in South Australia and recommended in Western Australia) or a presumption of competency (like that recommended in New South Wales), a presumption that 16- and 17-year-old young people are capable of making their own medical decisions would increase access to care for trans youth, decrease doubt, and increase the clarity of clinical decision making.
49 A legislative presumption of capacity at age 16 would be useful for improving access to gender-affirming hormones and surgery but would not assist those seeking puberty blockers, which are sought at a much younger age. Further, while older clinical treatment guidelines indicated age 16 as a minimum age for gender-affirming hormones, more recent clinical guidelines, including the Australian Guidelines, indicate that gender-affirming hormones may be appropriate and desirable before age 16. Thus, while a legislative presumption of capacity at age 16 would benefit some trans youth, it would likely need to be accompanied by other law reform addressing the situation for those aged under 16. Another potential barrier is that it could be argued that gender-affirming healthcare is somehow still ‘special’ and falls outside a provision of general application. (See, e.g.,
Taylor-Sands and Dimopoulos 2022;
Giordano and Holm 2020).
Currently, the law in South Australia provides a legislative test for competency. While the
Gillick test requires ‘sufficient maturity and intelligence to fully understand’, the South Australian legislation requires the adolescent to be ‘capable of understanding the nature, consequences and risks of the treatment.’
50 This is also accompanied by the requirement that it be in the best interests of the child’s health and wellbeing. The treating doctor’s opinion as to competency and best interests must be supported in writing by another medical practitioner.
51 The South Australian provision, or a similar version of it, could be legislated in other Australian states and territories. A benefit of this approach is that it could clarify some of the inherent ambiguities of the
Gillick test that have plagued this area for some time. These include whether it is sufficient or a full understanding that is required, as well as whether it is actual understanding or a capacity to understand that is needed (
Cave 2014).
In Western Australia, the Law Reform Commission recommended that children under 16 be able to give ‘valid and sufficient consent to medical treatment to the same extent as if of full age if they are “mature”, that is, if they are of sufficient intelligence and understanding to comprehend the nature and implications of the proposed treatment. The implications include the consequences of having the treatment performed without parental consultation or agreement’ (
Western Australia Law Reform Commission 1988, p. 45). In New South Wales, the Law Reform Commission recommended a recognition of competency when a young person ‘understands the information that is relevant to making a decision about the health care, and appreciates the reasonably foreseeable consequences of that decision’ (
New South Wales Law Reform Commission 2008, p. 126). The Queensland Law Reform Commission’s test was more general, providing that a person could authorise their own healthcare if they understand the nature and consequences of the particular healthcare (
Queensland Law Reform Commission 1996). Insofar as it more clearly provides that only ‘relevant’ information needs be understood and ‘reasonably foreseeable’ consequences as opposed to ‘full’ understanding or possibly remote risks and implications, we prefer the formulation by the New South Wales Law Reform Commission over that recommended in Western Australia, South Australia and Queensland.
In our view, the requirement for a best interests assessment, as in the South Australian legislation, is not desirable because, as stated by the Western Australia Law Reform Commission, ‘tests based on “best interests” do not really recognise any degree of patient autonomy. They give the adult who decides the question a great deal of power, and permit the invalidation of children’s decisions on discretionary and subjective grounds’ (
Western Australia Law Reform Commission 1988, p. 41). This issue has heightened importance for gender-affirming treatment decisions because, as pointed out by Bryant CJ in
Re: Jamie, ‘one might think that, of all the medical treatments that might arise, treatment for something as personal and essential as the perception of one’s gender and sexuality would be the very exemplar of when the rights of the Gillick-competent child should be given full effect.’
52 We also do not consider it desirable to require two medical practitioners to assess competency, as exists in the South Australian legislation. The requirement for a second written opinion as to competency is both impractical and a rubber-stamping exercise that would, as noted by the Queensland Law Reform Commission, present a significant barrier to care in rural and remote areas (1996, p. 258).
To change the current requirements imposed by the Family Court’s decision in
Re: Imogen, the legislation would ideally clarify that the consent of a young person who passes the competency test is sufficient as lawful consent to treatment, and there is no additional need to seek parental consent. The New South Wales Law Reform Commission recommendations contain a useful adjunct to the competency test in this regard. They provide that ‘a competent young person may accept or refuse health care and it is not necessary to obtain an acceptance or refusal of the health care from the young person’s parent or other legal guardian’ (
New South Wales Law Reform Commission 2008, p. 126). The New South Wales recommendations also explicitly address whether there are concurrent powers and how they interact with the exercise of autonomous decision making of a competent young person:
The legislation should provide that a health practitioner must not rely on the acceptance or refusal of health care of a parent or guardian on a young person’s behalf if that acceptance or refusal conflicts with the young person’s decision where the young person is competent to make a decision about his or her health care (p. 126).
This is accompanied by the proviso that limited residual parental powers to consent survive, with parents being able to give ‘consent to health care on behalf of or in relation to a young person who is not competent to give consent or to decide to accept or refuse health care for reasons other than immaturity, such as unconsciousness or cognitive impairment’ (p. 127). The Western Australia Law Reform Commission recommendations are similarly worded (
Western Australia Law Reform Commission 1988, p. 44). The Queensland Law Reform Commission recommended that once a young person aged over 12 years is found to be competent to make their own healthcare decisions, parental refusals are irrelevant (1996, p. 247).
These recommendations are consistent with a recent judgment of the High Court of England and Wales,
AB v CD, which directly concerned the provision of puberty blockers to trans youth.
53 In that case, Lieven J opined that ‘[t]he very essence of
Gillick is, in my view, that a parent’s right to consent or “determine” treatment cannot trump or overbear the decision of the child.’
54 In her Honour’s opinion, parents retain a power to consent concurrently with their
Gillick-competent child, but the exercise of that power is limited to situations in which the child is unable or chooses not to make the decision themselves.
55 Codification of this stance, as has been recommended by multiple law reform bodies, is desirable.
Legislative reform that codifies a competency test—ideally similar in form to that recommended by the New South Wales Law Reform Commission—would appropriately clarify the law for clinicians and trans young people alike. Importantly, a coexistent provision that parental consent is not required once a patient is assessed as competent would remove a significant legal barrier to care for trans youth. Like a statutory presumption of capacity, however, a provision of general application may leave room for the argument that gender-affirming healthcare is somehow still ‘special’ and not captured.
Rather than applying to medical treatment broadly, a specific provision that applies to trans youth consenting to gender-affirming healthcare is another possible approach. As Shield notes, ‘adolescents in certain situations both have greater need to make their own decisions and may have greater capacity to make those decisions than other adolescents without similar experience’ (
Shield 2007). In one empirical study on the capacity and authority of trans youth to consent to hormone therapy in Canada, trans youth aged 14 to 18 demonstrated understanding and abilities characteristic of the capacity to make decisions about hormone therapy initiation (
Clark and Virani 2021). The youth, parents, and healthcare providers interviewed generally agreed that young people in that age range can possess the capacity to consent to that healthcare. Most healthcare providers felt that the majority of youth who presented for care were well-informed and had sufficient insight to consent to their own treatment. One commented on how trans youth may be in a better position to consent than others their age due to their lived experience:
I actually find most of these kids that have had to ask this question to themselves are way more reflective than their peers of the same age, because they have had to look at questions that other youth may never have had to answer … we see just a breadth of introspection and reflection that is well beyond their years.
Trans young people are likely to have engaged in extensive independent research, deliberation, and decision making prior to discussing their wishes about medical care with other people (
Clark et al. 2020). Even when making their own healthcare decisions, they are likely to seek parental support and assistance with decision making prior to accessing care.
Medical treatment related to gender affirmation would not be the first type of medical treatment singled out under legislation as attracting different rules. New South Wales legislation requires that treatment for children under 16 years of age that is intended to, or is reasonably likely to, render a child infertile be authorised by a tribunal.
56 Similar legislation exists in Queensland, though it is confined to the sterilisation of children with ‘cognitive, intellectual, neurological or physical impairment.’
57 Unlike the New South Wales legislation, the Queensland legislation provides a mechanism for consent by a tribunal but does not require it, noting that where consent is given by an order of the tribunal, the child’s sterilisation is not unlawful.
58 Additionally, in Queensland, the
Public Health Act 2005 (Qld) addresses situations in which it is lawful to provide a young person with cosmetic surgery. The legislation makes it an offence for a person to perform a cosmetic procedure on a child unless the person believes, on reasonable grounds, that it is in the best interests of the child.
59 While not requiring authorisation by a court or tribunal, the legislation curbs decision making about children’s medical treatment for reasons similar to those cited for special medical procedure cases and the New South Wales legislation.
60While introducing legislative reform for gender-affirming healthcare specifically may entrench the notion that the treatment is ‘special’, it may be warranted as a means to reduce the harms created by the current legal framework. The practical benefit of a provision that directly addresses gender-affirming medical care is that it would remove any doubt about the intended effects of the law and remove the possibility of further debate.
9. Proposal for Reform
Accounting for the relative benefits and risks of the above approaches, we consider that the optimal solution, which best takes account of stakeholder concerns in this area, is a combination of the three options discussed above:
- (1)
A statutory presumption of capacity that treats the decisions of those aged 16 years and over the same as those of adults;
- (2)
A statutory test for competency that overcomes the practical challenges attending the Gillick test and clarifies the role of parents once a young person is competent; and
- (3)
A statutory provision that specifically clarifies that the law pertaining to access to gender-affirming healthcare is not different from that pertaining to other forms of healthcare.
It is important to note that these are not revolutionary proposals—they have been implemented in other jurisdictions and in relation to other areas of healthcare. In our view, this multi-pronged approach would remove significant barriers to healthcare for trans young people that result from recent case law.
A specific provision that addresses how lawful consent may be obtained for gender-affirming care is necessary in the face of case law that has painted it as different and special. This is desirable for clarity and also to remove any vestiges of the law on special medical procedures. Such a provision would necessarily encompass a competency test, which expressly provides that the consent of one parent is sufficient.
The law on concurrent consent powers must also be clearly elucidated, making clear that parental consent is not needed when a young person is competent to make their own decisions. It should clarify that parental consent can only be given for medical procedures when a competent young person is unable to or would prefer not to actively exercise their capacity to consent, rather than as a tool to subvert or override the young person’s wishes. A statutory presumption of capacity at age 16 would be a useful adjunct to such provisions. It is desirable from the perspectives of respecting the evolving capacities of young people, ensuring consistency with overseas approaches, and ensuring simplicity in clinical decision making.
Given that our suggested reforms address broad aspects of consent for medical treatment, including the authority of a young person to consent to their own treatment, they are best located in a specific consent to medical treatment statute rather than the Family Law Act. They would ideally take the form of either uniform laws in each state and territory or a national statute. As discussed above, the latter would require a referral of powers from the states to the Commonwealth.