1
Department of Rehabilitation Science, Faculty of Physical Education and Physiotherapy, Vrije Universiteit Brussel, 1050 Brussels, Belgium
2
Pain in Motion International Research Group, Department of Physiotherapy, Human Physiology and Anatomy, Faculty of Physical Education & Physiotherapy, Vrije Universiteit Brussel, 1050 Brussels, Belgium
3
Department of Health Sciences, Faculty of Science, Vrije Universiteit Amsterdam, Amsterdam Movement Sciences Research Institute, 1105 Amsterdam, The Netherlands
4
Department of Epidemiology and Data Science (Amsterdam UMC, Location VUmc), Amsterdam Movement Sciences Research Institute, 1046 Amsterdam, The Netherlands
5
Chronic Pain Rehabilitation, Department of Physical Medicine and Physiotherapy, University Hospital Brussels, 1050 Brussels, Belgium
6
General Practice “Het Homeer”, 9281 Harkema, The Netherlands
7
Transcare, Transdisciplinary Pain Management Center, 9711 Groningen, The Netherlands
J. Clin. Med. 2023, 12(3), 885; https://doi.org/10.3390/jcm12030885 - 22 Jan 2023
Cited by 4 | Viewed by 2779
Abstract
To manage chronic pain, multidisciplinary interventions have been increasingly deployed, mostly in secondary or tertiary care settings. Evidence on the effectiveness of multidisciplinary intervention within primary care is scarce. This study examined the effectiveness of a primary care multidisciplinary treatment for chronic pain
[...] Read more.
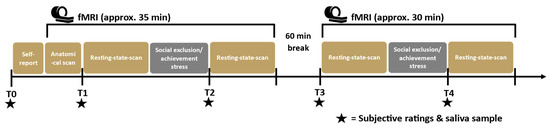
To manage chronic pain, multidisciplinary interventions have been increasingly deployed, mostly in secondary or tertiary care settings. Evidence on the effectiveness of multidisciplinary intervention within primary care is scarce. This study examined the effectiveness of a primary care multidisciplinary treatment for chronic pain compared with treatment as usual (TAU). The intervention consisted of pain neuroscience education and treatment by a GP, psychologist, and physiotherapist. Both groups filled out patient-reported outcome measures at baseline, 6 months, and 12 months. The results indicated there were no statistically significant differences for the primary outcomes of pain intensity, number of pain sites, and health-related quality of life (HR-QoL). There was a statistically significant difference in the secondary outcome perceived health change in favor of the intervention group. None of the other differences were statistically significant. A post-hoc analysis showed that there were statistically significant effects on patients’ illness perceptions in favor of the intervention group. Based on the results, the findings do not support effectiveness of a low intensity outpatient multidisciplinary primary care treatment to treat chronic pain compared with TAU. However, as a result of several study limitations, it is considered unwarranted to conclude that multidisciplinary treatment in primary care is not valuable at all.
Full article
(This article belongs to the Section Anesthesiology)
▼
Show Figures