Cancers 2023, 15(5), 1576; https://doi.org/10.3390/cancers15051576 - 3 Mar 2023
Cited by 4 | Viewed by 2297
Abstract
Tumor hypoxia can seriously impede the effectiveness of photodynamic therapy (PDT). To address this issue, two approaches, termed in situ oxygen generation and oxygen delivery, were developed. The in situ oxygen generation method uses catalysts such as catalase to decompose excess H2
[...] Read more.
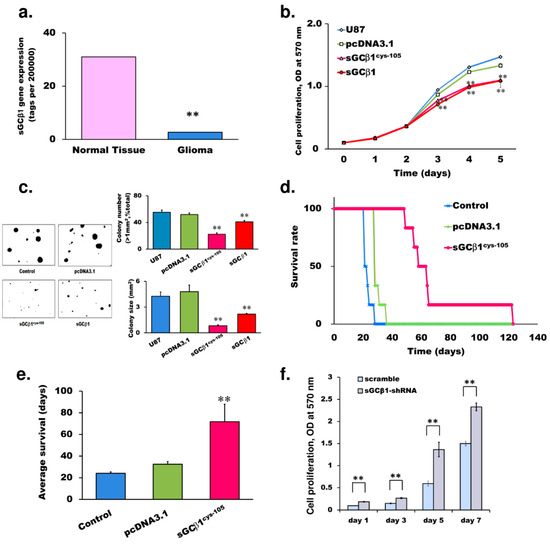
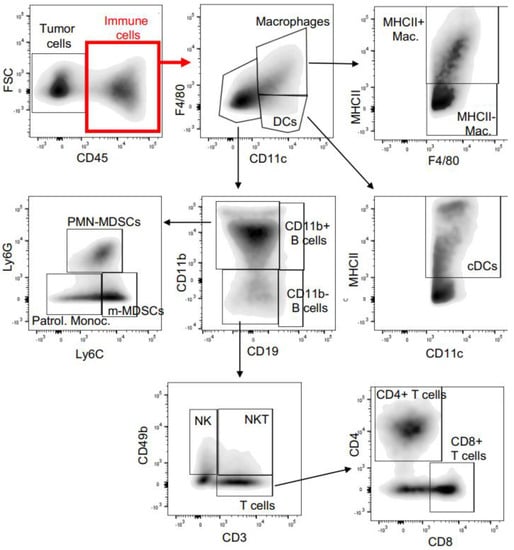
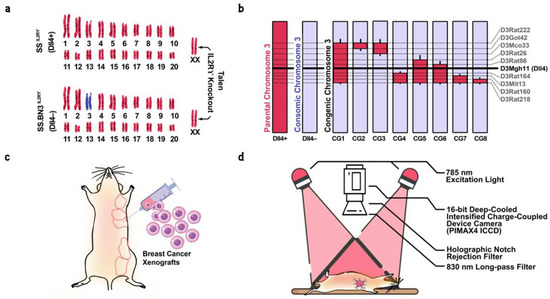
Tumor hypoxia can seriously impede the effectiveness of photodynamic therapy (PDT). To address this issue, two approaches, termed in situ oxygen generation and oxygen delivery, were developed. The in situ oxygen generation method uses catalysts such as catalase to decompose excess H2O2 produced by tumors. It offers specificity for tumors, but its effectiveness is limited by the low H2O2 concentration often present in tumors. The oxygen delivery strategy relies on the high oxygen solubility of perfluorocarbon, etc., to transport oxygen. It is effective, but lacks tumor specificity. In an effort to integrate the merits of the two approaches, we designed a multifunctional nanoemulsion system named CCIPN and prepared it using a sonication-phase inversion composition–sonication method with orthogonal optimization. CCIPN included catalase, the methyl ester of 2-cyano-3,12-dioxooleana-1,9(11)-dien-28-oic acid (CDDO-Me), photosensitizer IR780, and perfluoropolyether. Perfluoropolyether may reserve the oxygen generated by catalase within the same nanoformulation for PDT. CCIPN contained spherical droplets below 100 nm and showed reasonable cytocompatibility. It presented a stronger ability to generate cytotoxic reactive oxygen species and consequently destroy tumor cells upon light irradiation, in comparison with its counterpart without catalase or perfluoropolyether. This study contributes to the design and preparation of oxygen-supplementing PDT nanomaterials.
Full article
(This article belongs to the Special Issue Nanobiomaterials for Cancer Early Detection and Therapy)
►
Show Figures