1
Faculty of Health, Medicine and Life Sciences, School of Nutrition and Translational Research in Metabolism (NUTRIM), Maastricht University, 6200 MD Maastricht, The Netherlands
2
Centre for Healthy Eating & Food Innovation, Faculty of Science & Engineering, Maastricht University Campus Venlo, 5928 SZ Venlo, The Netherlands
3
College of Natural and Health Sciences, Zayed University, Dubai 19282, United Arab Emirates
4
Department of Food and Nutrition, Toronto Metropolitan University, Toronto, ON M5B 2K3, Canada
Metabolites 2022, 12(11), 1051; https://doi.org/10.3390/metabo12111051 - 1 Nov 2022
Cited by 7 | Viewed by 2468
Abstract
Peptide-hormones, including pancreatic peptide-YY(PYY), glucagon-like peptide-1 (GLP-1), cholecystokinin (CCK), insulin, and leptin function as satiety signals, while ghrelin promotes hunger. These hormones are also involved in glucose homeostasis and body-weight regulation. The aim of this cross-sectional analysis was to examine the association of
[...] Read more.
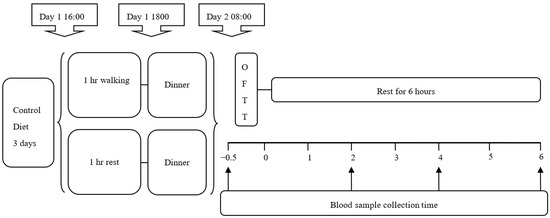
Peptide-hormones, including pancreatic peptide-YY(PYY), glucagon-like peptide-1 (GLP-1), cholecystokinin (CCK), insulin, and leptin function as satiety signals, while ghrelin promotes hunger. These hormones are also involved in glucose homeostasis and body-weight regulation. The aim of this cross-sectional analysis was to examine the association of these peptide-hormones with obesity-markers, insulin-resistance, and dyslipidemia (total-cholesterol (TC), low-density-lipoprotein-cholesterol (LDL-C), high-density-lipoprotein-cholesterol (HDL-C), triglyceride (TG)). Sixteen-obese (OB) adults and 21 normal-weight (NW) age-and gender-matched counterparts were recruited. OB-participants showed significantly higher levels of leptin, insulin, Homeostatic-Model Assessment of Insulin Resistance (HOMA-IR), and TG. NW participants had significantly higher levels of ghrelin. GLP-1 was positively correlated with insulin, HOMA-IR, and obesity-markers except percent body fat. Leptin was positively correlated with all markers (except glucose and dyslipidemia). PYY was positively correlated with BMI, insulin and HOMA-IR. Ghrelin was inversely correlated with all of the markers except glucose, TC, and LDL-C. In the regression analysis model, leptin was positively associated with obesity markers and insulin resistance. Our results indicate a significant difference in peptide hormones among OB and NW Lebanese individuals. Since there is controversial evidence regarding body-weight and peptide-hormones in the literature, this study highlights a step forward towards finding ethnic based strategies to treat obesity and its consequences.
Full article
(This article belongs to the Special Issue Prevention, Diagnosis and Treatment of Metabolic and Hormone-Dependent Disorders)