Antibiotics 2020, 9(11), 747; https://doi.org/10.3390/antibiotics9110747 - 28 Oct 2020
Cited by 12 | Viewed by 3503
Abstract
The present work was designed to identify and characterize novel antimicrobial peptides (AMPs) from Charybdis pancration (Steinh.) Speta, previously named Urginea maritima, is a Mediterranean plant, well-known for its biological properties in traditional medicine. Polypeptide-enriched extracts from different parts of the plant
[...] Read more.
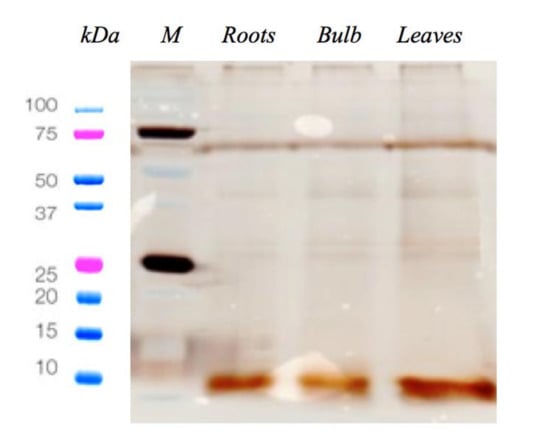
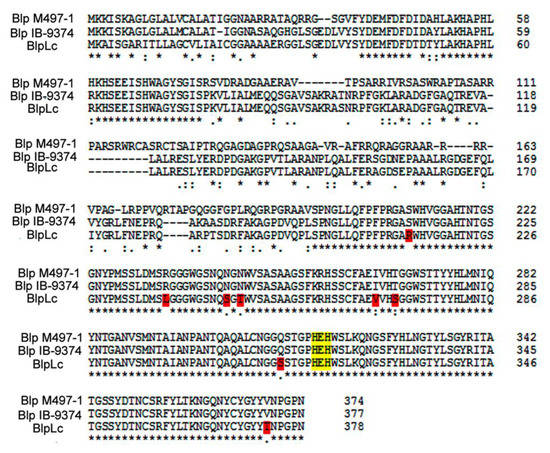
The present work was designed to identify and characterize novel antimicrobial peptides (AMPs) from Charybdis pancration (Steinh.) Speta, previously named Urginea maritima, is a Mediterranean plant, well-known for its biological properties in traditional medicine. Polypeptide-enriched extracts from different parts of the plant (roots, leaves and bulb), never studied before, were tested against two relevant pathogens, Staphylococcus aureus and Pseudomonas aeruginosa. With the aim of identifying novel natural AMPs, peptide fraction displaying antimicrobial activity (the bulb) that showed minimum inhibitory concentration (MICs) equal to 30 µg/mL against the above mentioned strains, was analysed by high-resolution mass spectrometry and database search. Seventeen peptides, related to seven proteins present in the investigated database, were described. Furthermore, we focused on three peptides, which due to their net positive charge, have a better chance to be AMPs and they were investigated by molecular modelling approaches, in order to shed light on the solution properties of their equilibrium structures. Some of new detected peptides could represent a good platform for the development of new antimicrobials in the fight against antibiotic resistance phenomenon.
Full article
(This article belongs to the Special Issue Synthesis and Utility of Antimicrobial Peptides)
►
Show Figures