Increasing the Vaccine Potential of Live M. bovis BCG by Coadministration with Plasmid DNA Encoding a Tuberculosis Prototype Antigen
Abstract
:1. Introduction
2. Experimental
2.1. Animals
2.2. Vaccination Protocol

2.3. Cytokine Production
2.4. In Vivo CTL Activity Assessment by Adoptive Transfer of CFSE-Labelled Target Cells
2.5. IgG Antibody Secretion
2.6. Statistical Analysis
3. Results and Discussion
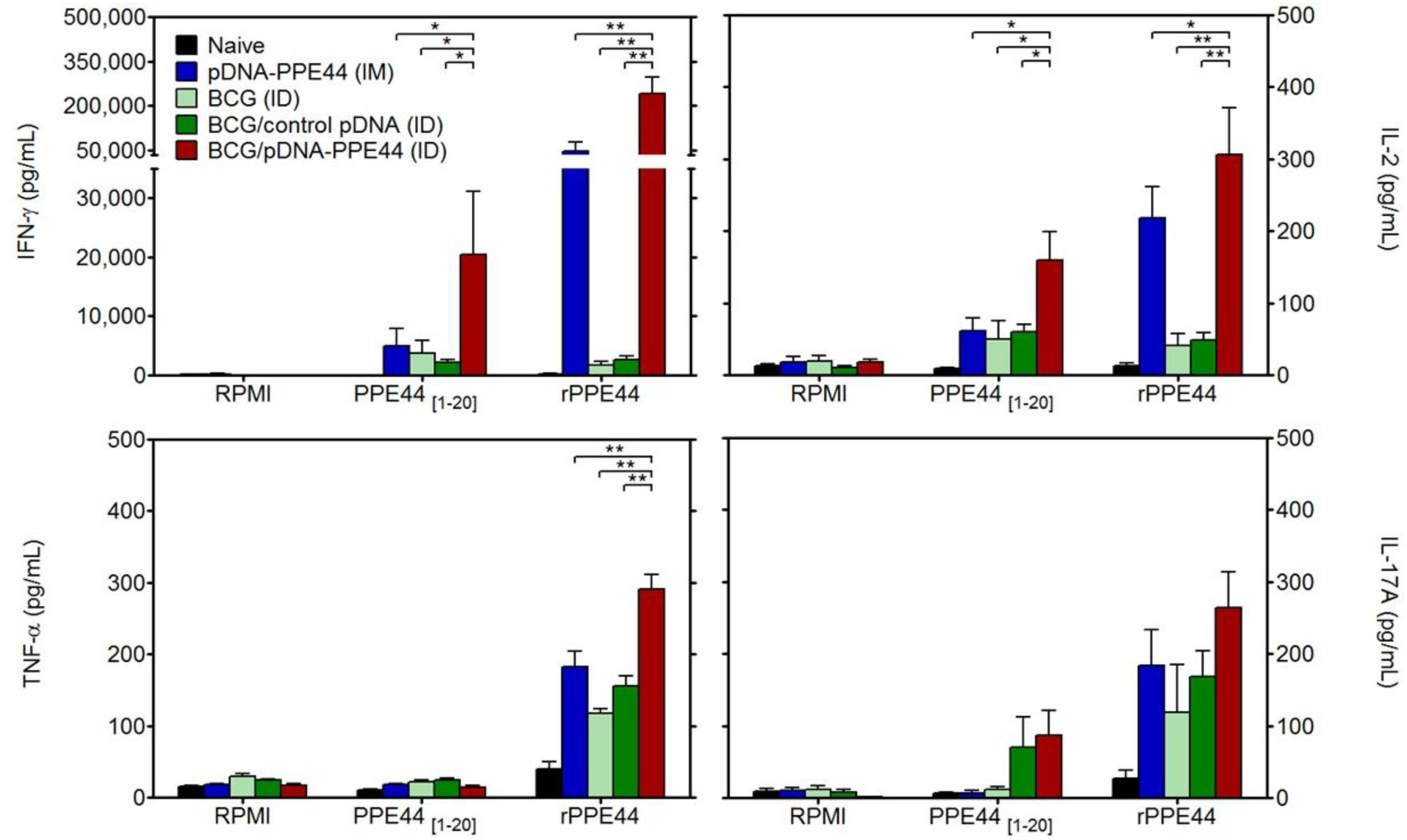
3.1. BCG/PPE44-Encoding pDNA Co-Vaccination Enhances Specific Th1-Type Cytokine Secretion
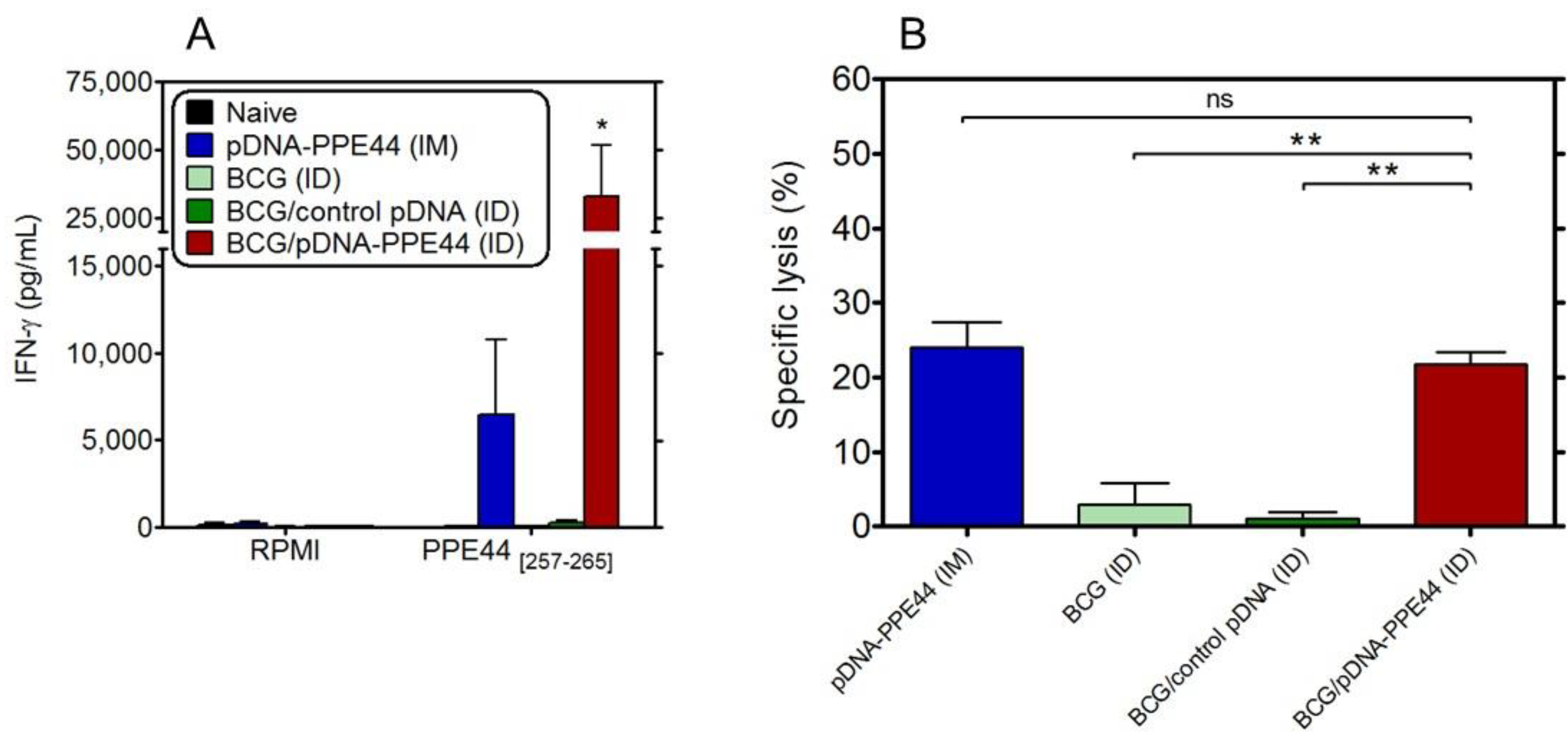
3.2. BCG/PPE44-Encoding pDNA Co-Vaccination Enhances Effective Cytolytic and IFN-γ-Producing CD8+ T-Cell Responses
3.3. BCG/PPE44-Encoding pDNA Co-Vaccination Enhances Mycobacteria-Specific Responses against Non-Plasmid-Encoded but BCG-Expressed Antigens
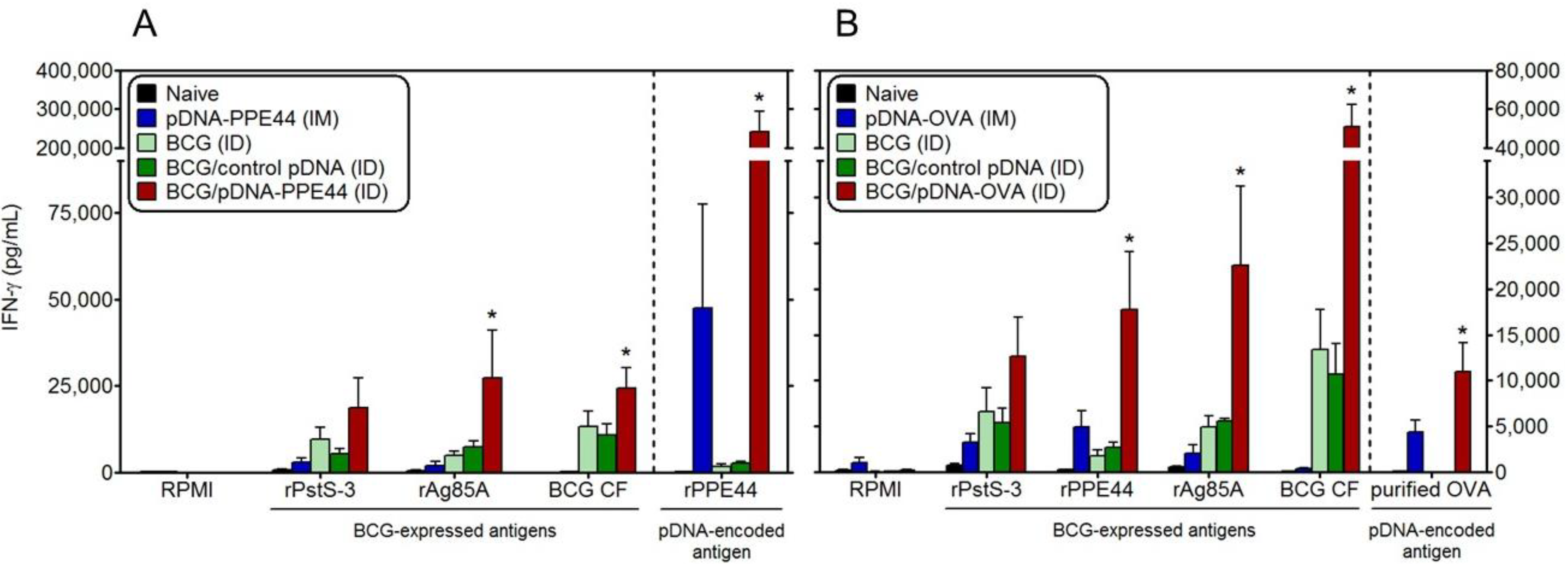
3.4. Bystander Activation of IFN-γ Responses against BCG-Expressed Antigens by BCG/OVA-Encoding pDNA Co-Vaccination
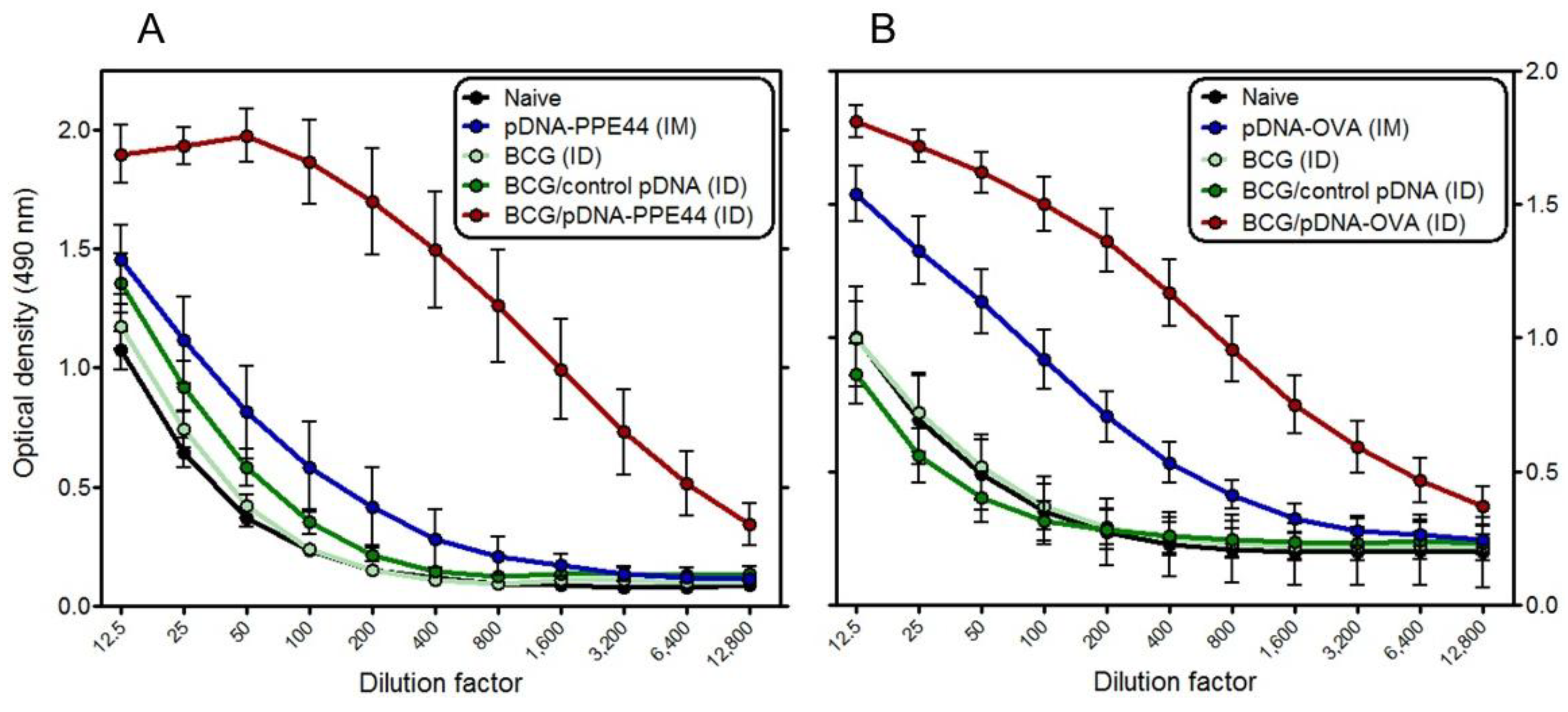
3.5. BCG/PPE44-Encoding pDNA or BCG/pDNA-OVA Co-Vaccination also Enhances Antigen-Specific Antibody Responses
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Trunz, B.B.; Fine, P.; Dye, C. Effect of BCG vaccination on childhood tuberculous meningitis and miliary tuberculosis worldwide: A meta-analysis and assessment of cost-effectiveness. Lancet 2006, 367, 1173–1180. [Google Scholar] [CrossRef]
- Fine, P.E. Variation in protection by BCG: Implications of and for heterologous immunity. Lancet 1995, 346, 1339–1345. [Google Scholar] [CrossRef]
- World Health Organization. Global Tuberculosis Report; Geneva, Switzerland, 2013.
- Weir, R.E.; Gorak-Stolinska, P.; Floyd, S.; Lalor, M.K.; Stenson, S.; Branson, K.; Blitz, R.; Ben-Smith, A.; Fine, P.E.; Dockrell, H.M. Persistence of the immune response induced by BCG vaccination. BMC Infect. Dis. 2008, 8. [Google Scholar] [CrossRef]
- Ritz, N.; Hanekom, W.A.; Robins-Browne, R.; Britton, W.J.; Curtis, N. Influence of BCG vaccine strain on the immune response and protection against tuberculosis. FEMS Microbiol. Rev. 2008, 32, 821–841. [Google Scholar] [CrossRef]
- Lin, M.Y.; Geluk, A.; Smith, S.G.; Stewart, A.L.; Friggen, A.H.; Franken, K.L.; Verduyn, M.J.; van Meijgaarden, K.E.; Voskuil, M.I.; Dockrell, H.M.; et al. Lack of immune responses to Mycobacterium tuberculosis DosR regulon proteins following Mycobacterium bovis BCG vaccination. Infect. Immun. 2007, 75, 3523–3530. [Google Scholar] [CrossRef]
- Weir, R.E.; Black, G.F.; Nazareth, B.; Floyd, S.; Stenson, S.; Stanley, C.; Branson, K.; Sichali, L.; Chaguluka, S.D.; Donovan, L.; et al. The influence of previous exposure to environmental mycobacteria on the interferon-gamma response to bacille Calmette-Guerin vaccination in southern England and northern Malawi. Clin. Exp. Immunol. 2006, 146, 390–399. [Google Scholar] [CrossRef]
- Ryan, A.A.; Nambiar, J.K.; Wozniak, T.M.; Roediger, B.; Shklovskaya, E.; Britton, W.J.; Fazekas de St Groth, B.; Triccas, J.A. Antigen load governs the differential priming of CD8 T cells in response to the bacille Calmette Guerin vaccine or Mycobacterium tuberculosis infection. J. Immunol. 2009, 182, 7172–7717. [Google Scholar] [CrossRef]
- Van Pinxteren, L.A.; Cassidy, J.P.; Smedegaard, B.H.; Agger, E.M.; Andersen, P. Control of latent Mycobacterium tuberculosis infection is dependent on CD8 T cells. Eur. J. Immunol. 2000, 30, 3689–36298. [Google Scholar] [CrossRef]
- Tascon, R.E.; Stavropoulos, E.; Lukacs, K.V.; Colston, M.J. Protection against Mycobacterium tuberculosis infection by CD8+ T cells requires the production of gamma interferon. Infect. Immun. 1998, 66, 830–834. [Google Scholar]
- Bruns, H.; Meinken, C.; Schauenberg, P.; Harter, G.; Kern, P.; Modlin, R.L.; Antoni, C.; Stenger, S. Anti-TNF immunotherapy reduces CD8+ T cell-mediated antimicrobial activity against Mycobacterium tuberculosis in humans. J. Clin. Investig. 2009, 119, 1167–1177. [Google Scholar] [CrossRef]
- Romano, M.; Huygen, K. An update on vaccines for tuberculosis-there is more to it than just waning of BCG efficacy with time. Exp. Opin. Biol. Ther. 2012, 12, 1601–1610. [Google Scholar] [CrossRef]
- Liu, M.A. DNA vaccines: An historical perspective and view to the future. Immunol. Rev. 2011, 239, 62–84. [Google Scholar] [CrossRef]
- Derrick, S.C.; Yang, A.L.; Morris, S.L. A polyvalent DNA vaccine expressing an ESAT6-Ag85B fusion protein protects mice against a primary infection with Mycobacterium tuberculosis and boosts BCG-induced protective immunity. Vaccine 2004, 23, 780–788. [Google Scholar] [CrossRef]
- Lu, J.; Wang, C.; Zhou, Z.; Zhang, Y.; Cao, T.; Shi, C.; Chen, Z.; Chen, L.; Cai, C.; Fan, X. Immunogenicity and protective efficacy against murine tuberculosis of a prime-boost regimen with BCG and a DNA vaccine expressing ESAT-6 and Ag85A fusion protein. Clin. Dev. Immunol. 2011, 2011. [Google Scholar] [CrossRef]
- Cervantes-Villagrana, A.R.; Hernandez-Pando, R.; Biragyn, A.; Castaneda-Delgado, J.; Bodogai, M.; Martinez-Fierro, M.; Sada, E.; Trujillo, V.; Enciso-Moreno, A.; Rivas-Santiago, B. Prime-boost BCG vaccination with DNA vaccines based in beta-defensin-2 and mycobacterial antigens ESAT6 or Ag85B improve protection in a tuberculosis experimental model. Vaccine 2013, 31, 676–684. [Google Scholar] [CrossRef]
- Tan, K.; Liang, J.; Teng, X.; Wang, X.; Zhang, J.; Yuan, X.; Fan, X. Comparison of BCG prime-DNA booster and rBCG regimens for protection against tuberculosis. Hum. Vaccin Immunother. 2013. [Google Scholar] [CrossRef]
- Feng, C.G.; Palendira, U.; Demangel, C.; Spratt, J.M.; Malin, A.S.; Britton, W.J. Priming by DNA immunization augments protective efficacy of Mycobacterium bovis Bacille Calmette-Guerin against tuberculosis. Infect. Immun. 2001, 69, 4174–4176. [Google Scholar] [CrossRef]
- Ferraz, J.C.; Stavropoulos, E.; Yang, M.; Coade, S.; Espitia, C.; Lowrie, D.B.; Colston, M.J.; Tascon, R.E. A heterologous DNA priming-Mycobacterium bovis BCG boosting immunization strategy using mycobacterial Hsp70, Hsp65, and Apa antigens improves protection against tuberculosis in mice. Infect. Immun. 2004, 72, 6945–6950. [Google Scholar] [CrossRef]
- Dou, J.; Wang, Y.; Yu, F.; Yang, H.; Wang, J.; He, X.; Xu, W.; Chen, J.; Hu, K. Protection against Mycobacterium tuberculosis challenge in mice by DNA vaccine Ag85A-ESAT-6-IL-21 priming and BCG boosting. Int. J. Immunogenet. 2012, 39, 183–190. [Google Scholar] [CrossRef]
- Romano, M.; D’Souza, S.; Adnet, P.Y.; Laali, R.; Jurion, F.; Palfliet, K.; Huygen, K. Priming but not boosting with plasmid DNA encoding mycolyl-transferase Ag85A from Mycobacterium tuberculosis increases the survival time of Mycobacterium bovis BCG vaccinated mice against low dose intravenous challenge with M. tuberculosis H37Rv. Vaccine 2006, 24, 3353–3364. [Google Scholar] [CrossRef]
- Zhang, S.; Guo, Y.J.; Sun, S.H.; Wang, K.Y.; Wang, K.H.; Zhang, Y.; Zhu, W.J.; Chen, Z.H.; Jiang, L. DNA vaccination using Bacillus Calmette-Guerin-DNA as an adjuvant to enhance immune response to three kinds of swine diseases. Scand. J. Immunol. 2005, 62, 371–377. [Google Scholar] [CrossRef]
- Sun, J.; Hou, J.; Li, D.; Liu, Y.; Hu, N.; Hao, Y.; Fu, J.; Hu, Y.; Shao, Y. Enhancement of HIV-1 DNA vaccine immunogenicity by BCG-PSN, a novel adjuvant. Vaccine 2013, 31, 472–479. [Google Scholar] [CrossRef]
- Orme, I.M. Induction of nonspecific acquired resistance and delayed-type hypersensitivity, but not specific acquired resistance in mice inoculated with killed mycobacterial vaccines. Infect. Immun. 1988, 56, 3310–3312. [Google Scholar]
- Sander, L.E.; Davis, M.J.; Boekschoten, M.V.; Amsen, D.; Dascher, C.C.; Ryffel, B.; Swanson, J.A.; Muller, M.; Blander, J.M. Detection of prokaryotic mRNA signifies microbial viability and promotes immunity. Nature 2011, 474, 385–389. [Google Scholar] [CrossRef]
- Rindi, L.; Peroni, I.; Lari, N.; Bonanni, D.; Tortoli, E.; Garzelli, C. Variation of the expression of Mycobacterium tuberculosis ppe44 gene among clinical isolates. FEMS Immunol. Med. Microbiol. 2007, 51, 381–387. [Google Scholar]
- Romano, M.; Rindi, L.; Korf, H.; Bonanni, D.; Adnet, P.Y.; Jurion, F.; Garzelli, C.; Huygen, K. Immunogenicity and protective efficacy of tuberculosis subunit vaccines expressing PPE44 (Rv2770c). Vaccine 2008, 26, 6053–6063. [Google Scholar] [CrossRef]
- Huygen, K.; Content, J.; Denis, O.; Montgomery, D.L.; Yawman, A.M.; Deck, R.R.; DeWitt, C.M.; Orme, I.M.; Baldwin, S.; D’Souza, C.; et al. Immunogenicity and protective efficacy of a tuberculosis DNA vaccine. Nat. Med. 1996, 2, 893–898. [Google Scholar] [CrossRef]
- Stoecklinger, A.; Grieshuber, I.; Scheiblhofer, S.; Weiss, R.; Ritter, U.; Kissenpfennig, A.; Malissen, B.; Romani, N.; Koch, F.; Ferreira, F.; et al. Epidermal langerhans cells are dispensable for humoral and cell-mediated immunity elicited by gene gun immunization. J. Immunol. 2007, 179, 886–893. [Google Scholar]
- Romano, M.; Roupie, V.; Wang, X.M.; Denis, O.; Jurion, F.; Adnet, P.Y.; Laali, R.; Huygen, K. Immunogenicity and protective efficacy of tuberculosis DNA vaccines combining mycolyl-transferase Ag85A and phosphate transport receptor PstS-3. Immunology 2006, 118, 321–332. [Google Scholar] [CrossRef]
- Romano, M.; Denis, O.; D’Souza, S.; Wang, X.M.; Ottenhoff, T.H.; Brulet, J.M.; Huygen, K. Induction of in vivo functional Db-restricted cytolytic T cell activity against a putative phosphate transport receptor of Mycobacterium tuberculosis. J. Immunol. 2004, 172, 6913–6921. [Google Scholar]
- Lefevre, P.; Braibant, M.; de Wit, L.; Kalai, M.; Roeper, D.; Grotzinger, J.; Delville, J.P.; Peirs, P.; Ooms, J.; Huygen, K.; et al. Three different putative phosphate transport receptors are encoded by the Mycobacterium tuberculosis genome and are present at the surface of Mycobacterium bovis BCG. J. Bacteriol. 1997, 179, 2900–2906. [Google Scholar]
- Tanghe, A.; Lefevre, P.; Denis, O.; D’Souza, S.; Braibant, M.; Lozes, E.; Singh, M.; Montgomery, D.; Content, J.; Huygen, K. Immunogenicity and protective efficacy of tuberculosis DNA vaccines encoding putative phosphate transport receptors. J. Immunol. 1999, 162, 1113–1119. [Google Scholar]
- Chen, C.Y.; Huang, D.; Wang, R.C.; Shen, L.; Zeng, G.; Yao, S.; Shen, Y.; Halliday, L.; Fortman, J.; McAllister, M.; et al. A critical role for CD8 T cells in a nonhuman primate model of tuberculosis. PLoS Pathog. 2009, 5, e1000392. [Google Scholar] [CrossRef]
- Villarreal-Ramos, B.; McAulay, M.; Chance, V.; Martin, M.; Morgan, J.; Howard, C.J. Investigation of the role of CD8+ T cells in bovine tuberculosis in vivo. Infect. Immun. 2003, 71, 4297–4303. [Google Scholar] [CrossRef]
- Von, E.K.; Morrison, R.; Braun, M.; Ofori-Anyinam, O.; De Kock, E.; Pavithran, P.; Koutsoukos, M.; Moris, P.; Cain, D.; Dubois, M.C.; et al. The candidate tuberculosis vaccine Mtb72F/AS02A: Tolerability and immunogenicity in humans. Hum. Vaccin. 2009, 5, 475–482. [Google Scholar]
- Spertini, F.; Audran, R.; Lurati, F.; Ofori-Anyinam, O.; Zysset, F.; Vandepapeliere, P.; Moris, P.; Demoitie, M.A.; Mettens, P.; Vinals, C.; et al. The candidate tuberculosis vaccine Mtb72F/AS02 in PPD positive adults: A randomized controlled phase I/II study. Tuberculosis 2013, 93, 179–188. [Google Scholar] [CrossRef]
- Skeiky, Y.A.; Alderson, M.R.; Ovendale, P.J.; Lobet, Y.; Dalemans, W.; Orme, I.M.; Reed, S.G.; Campos-Neto, A. Protection of mice and guinea pigs against tuberculosis induced by immunization with a single Mycobacterium tuberculosis recombinant antigen, MTB41. Vaccine 2005, 23, 3937–3945. [Google Scholar] [CrossRef]
- Bonanni, D.; Rindi, L.; Lari, N.; Garzelli, C. Immunogenicity of mycobacterial PPE44 (Rv2770c) in Mycobacterium bovis BCG-infected mice. J. Med. Microbiol. 2005, 54, 443–448. [Google Scholar] [CrossRef]
- Russell, M.S.; Iskandar, M.; Mykytczuk, O.L.; Nash, J.H.; Krishnan, L.; Sad, S. A reduced antigen load in vivo, rather than weak inflammation, causes a substantial delay in CD8+ T cell priming against Mycobacterium bovis (Bacillus Calmette-Guerin). J. Immunol. 2007, 179, 211–220. [Google Scholar]
- Henrickson, S.E.; Perro, M.; Loughhead, S.M.; Senman, B.; Stutte, S.; Quigley, M.; Alexe, G.; Iannacone, M.; Flynn, M.P.; Omid, S.; et al. Antigen availability determines CD8+ T cell-dendritic cell interaction kinetics and memory fate decisions. Immunity 2013, 39, 496–507. [Google Scholar] [CrossRef]
- Bruffaerts, N.; Vandermeulen, G.; Romano, M.; Préat, V.; Stockhofe-Zurwieden, N.; Huygen, K.; Scientific Institute of Public Health (WIV-ISP), Brussels, Belgium. Unpublished data. 2014.
- Tough, D.F.; Borrow, P.; Sprent, J. Induction of bystander T cell promiferation by viruses and type I interferon in vivo. Science 1996, 272, 1947–1950. [Google Scholar]
- Zhang, X.; Sun, S.; Hwang, I.; Tough, D.F.; Sprent, J. Potent and selective stimulation of memory-phenotype CD8+ T cells in vivo by IL-15. Immunity 1998, 8, 591–599. [Google Scholar] [CrossRef]
- Di Genova, G.; Savelyeva, N.; Suchaki, A.; Thirdborough, S.M.; Stevenson, F.K. Bystander stimulation of activated CD4+ T cells of unrelated specificity following a booster vaccination with tetanus toxoid. Eur. J. Immunol. 2010, 40, 976–985. [Google Scholar] [CrossRef]
- Bruffaerts, N.; Romano, M.; Denis, O.; Jurion, F.; Huygen, K.; Scientific Institute of Public Health (WIV-ISP), Brussels, Belgium. Unpublished data. 2014.
- Von Meyenn, F.; Schaefer, M.; Weighardt, H.; Bauer, S.; Kirschning, C.J.; Wagner, H.; Sparwasser, T. Toll-like receptor 9 contributes to recognition of Mycobacterium bovis Bacillus Calmette-Guerin by Flt3-ligand generated dendritic cells. Immunobiology 2006, 211, 557–565. [Google Scholar] [CrossRef]
- Desmet, C.J.; Ishii, K.J. Nucleic acid sensing at the interface between innate and adaptive immunity in vaccination. Nat. Rev. Immunol. 2012, 12, 479–491. [Google Scholar] [CrossRef]
- Bafica, A.; Scanga, C.A.; Feng, C.G.; Leifer, C.; Cheever, A.; Sher, A. TLR9 regulates Th1 responses and cooperates with TLR2 in mediating optimal resistance to Mycobacterium tuberculosis. J. Exp. Med. 2005, 202, 1715–1724. [Google Scholar] [CrossRef]
- De Brito, C.; Tomkowiak, M.; Ghittoni, R.; Caux, C.; Leverrier, Y.; Marvel, J. CpG promotes cross-presentation of dead cell-associated antigens by pre-CD8α+ dendritic cells. J. Immunol. 2011, 186, 1503–1511. [Google Scholar] [CrossRef]
- Pavlenko, M.; Leder, C.; Moreno, S.; Levitsky, V.; Pisa, P. Priming of CD8+ T-cell responses after DNA immunization is impaired in TLR9- and MyD88-deficient mice. Vaccine 2007, 25, 6341–6347. [Google Scholar] [CrossRef]
- Elnekave, M.; Furmanov, K.; Hovav, A.H. Intradermal naked plasmid DNA immunization: Mechanisms of action. Exp. Rev. Vaccines 2011, 10, 1169–1182. [Google Scholar] [CrossRef]
- Heath, W.R.; Carbone, F.R. The skin-resident and migratory immune system in steady state and memory: Innate lymphocytes, dendritic cells and T cells. Nat. Immunol. 2013, 14, 978–985. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Bruffaerts, N.; Romano, M.; Denis, O.; Jurion, F.; Huygen, K. Increasing the Vaccine Potential of Live M. bovis BCG by Coadministration with Plasmid DNA Encoding a Tuberculosis Prototype Antigen. Vaccines 2014, 2, 181-195. https://doi.org/10.3390/vaccines2010181
Bruffaerts N, Romano M, Denis O, Jurion F, Huygen K. Increasing the Vaccine Potential of Live M. bovis BCG by Coadministration with Plasmid DNA Encoding a Tuberculosis Prototype Antigen. Vaccines. 2014; 2(1):181-195. https://doi.org/10.3390/vaccines2010181
Chicago/Turabian StyleBruffaerts, Nicolas, Marta Romano, Olivier Denis, Fabienne Jurion, and Kris Huygen. 2014. "Increasing the Vaccine Potential of Live M. bovis BCG by Coadministration with Plasmid DNA Encoding a Tuberculosis Prototype Antigen" Vaccines 2, no. 1: 181-195. https://doi.org/10.3390/vaccines2010181



