Journal Description
Vaccines
Vaccines
is an international, peer-reviewed, open access journal published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, PMC, Embase, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q1 (Immunology) / CiteScore - Q1 (Pharmacology (medical))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 18.6 days after submission; acceptance to publication is undertaken in 3.3 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
5.2 (2023);
5-Year Impact Factor:
4.9 (2023)
Latest Articles
Dengue Vaccine Development and Deployment into Routine Immunization
Vaccines 2025, 13(5), 483; https://doi.org/10.3390/vaccines13050483 (registering DOI) - 29 Apr 2025
Abstract
Dengue has emerged as a significant global health threat. Despite decades of research, only two dengue vaccines—CYD-TDV (Dengvaxia) and TAK-003 (Qdenga)—have been licensed to date, with limited implementation. This paper explores and outlines strategies for integrating dengue vaccines into routine immunization programs, particularly
[...] Read more.
Dengue has emerged as a significant global health threat. Despite decades of research, only two dengue vaccines—CYD-TDV (Dengvaxia) and TAK-003 (Qdenga)—have been licensed to date, with limited implementation. This paper explores and outlines strategies for integrating dengue vaccines into routine immunization programs, particularly in high-burden regions. TAK-003, a tetravalent live-attenuated vaccine, has demonstrated 61% efficacy against virologically confirmed dengue and 84% efficacy against hospitalizations in endemic settings. However, concerns remain about vaccine-enhanced disease, particularly among seronegative individuals exposed to DENV3 and DENV4. WHO recommends targeted introduction in high-transmission settings without pre-vaccination screening, while ongoing post-introduction studies will further clarify long-term safety and efficacy. Effective vaccine rollout requires a multi-pronged approach, including school-based immunization, integration with adolescent health services, and strong community engagement. Decision-making for vaccine introduction should be guided by National Immunization Technical Advisory Groups (NITAGs), local epidemiological data, and cost-effectiveness assessments. While future vaccines, including mRNA and virus-like particle candidates, are under development, optimizing the use of currently available vaccines is crucial to reducing dengue’s public health impact. Given the continued rise in cases, immediate action—combining vaccination with vector control—is essential to prevent further morbidity and mortality.
Full article
(This article belongs to the Special Issue 50 Years of Immunization—Steps Forward)
Open AccessReview
Overcoming Barriers to Human Papillomavirus Vaccination in Guangdong Province, China
by
Shuaijing Zhang, Shiqi Li, Jingtai Ma, Guiyuan Ji, Zhifeng Li, Siyi Chen, Fenglin Zhang, Xingfen Yang, Jianpeng Xiao, Rong Cao, Chenggang Wu and Wei Wu
Vaccines 2025, 13(5), 482; https://doi.org/10.3390/vaccines13050482 - 29 Apr 2025
Abstract
Human papillomavirus (HPV) infection remains a critical public health challenge in China, particularly in Guangdong Province, where HPV-52, 16, and 58 genotypes predominate, and male infection rates exceed 40%. Despite the successful implementation of a government-funded school-based program that has achieved 88% HPV
[...] Read more.
Human papillomavirus (HPV) infection remains a critical public health challenge in China, particularly in Guangdong Province, where HPV-52, 16, and 58 genotypes predominate, and male infection rates exceed 40%. Despite the successful implementation of a government-funded school-based program that has achieved 88% HPV vaccine coverage among adolescent girls, several persistent barriers, including genotype mismatch (the free HPV vaccine covers < 50% of high-risk local strains), regional disparities (80% vs. 60% for first-dose coverage), and exclusion of males, thwart progress toward herd immunity. Financial sustainability risks pose an even more significant threat to the expansion of HPV vaccination programs, especially in Guangdong province where annual expenditures exceed CNY 200 million. This review delves into Guangdong’s pioneering efforts and proposes practical solutions: accelerating domestic multivalent HPV vaccine development, adopting gender-neutral vaccination policies, and leveraging mobile clinics for remote populations. These strategies not only provide a roadmap for China but also serve as valuable insight for other LMICs striving to overcome HPV-related inequalities.
Full article
(This article belongs to the Special Issue HPV Vaccination Coverage: Problems and Challenges)
Open AccessReview
Challenges and Innovations in Pharmacovigilance and Signal Management During the COVID-19 Pandemic: An Industry Perspective
by
Maria Maddalena Lino, Susan Mather, Marianna Trani, Yan Chen, Patrick Caubel and Barbara De Bernardi
Vaccines 2025, 13(5), 481; https://doi.org/10.3390/vaccines13050481 - 29 Apr 2025
Abstract
Vaccine marketing authorization holders (MAHs) are responsible for the conduction of global vaccine pharmacovigilance on their vaccine products. A safety signal is detected when a new adverse event (AE) or aspect of an AE occurs after exposure to the vaccine and warrants further
[...] Read more.
Vaccine marketing authorization holders (MAHs) are responsible for the conduction of global vaccine pharmacovigilance on their vaccine products. A safety signal is detected when a new adverse event (AE) or aspect of an AE occurs after exposure to the vaccine and warrants further investigation to determine whether a causal association may exist. Signal detection and evaluation (signal management) begins at the start of vaccine development, before an MAH submits an application for authorization to regulatory authorities, continues through the course of all clinical trials, and carries on beyond development into the post-marketing phase. As long as the vaccine remains authorized anywhere in the world, pharmacovigilance continues. During the time that the COVID-19 vaccine became widely available after authorization and approval, clinical trials were also ongoing, and therefore all clinical development and post-authorization safety information was closely monitored for safety by the MAH. MAH pharmacovigilance activities were adapted to manage the unprecedented volume of safety information that became available within a very short timeframe following worldwide vaccination campaigns. No vaccine had previously been administered to such a large number of individuals in such a short time, nor had there previously been a public health vaccine experience that was the subject of so many medical and non-medical writings. The MAH’s COVID-19 vaccine signal detection methods included the continuous review of accruing clinical trial data and the quantitative and qualitative analyses of spontaneously reported experiences. Review of published and unpublished medical literature and epidemiology-based analyses such as observed vs. expected analysis based on reported adverse events following immunization (AEFIs) played key roles in pharmacovigilance and signal management. All methods of signal detection and evaluation have caveats, but when considered in totality, can advance our understanding of a vaccine’s safety profile and therefore the risk–benefit considerations for vaccinating both individuals and large populations of people. All COVID-19 vaccines authorized for use were subject to an unprecedented level of pharmacovigilance by their individual MAHs, national regulatory authorities, public health organizations, and others during the years immediately following regulatory authorization and full approval. The intense worldwide focus on pharmacovigilance and the need for MAHs and regulatory/health authorities to quickly evaluate incoming safety information, spurred frequent and timely communications between national and regional health authorities and between MAHs and regulatory/health authorities, spotlighting a unique opportunity for individuals committed to patient safety to share important accruing safety information in a collegial and less traditionally formal manner than usual. The global pandemic precipitated by the SARS-CoV-2 virus created a significant impetus for MAHs to develop innovative vaccines to change the course of the COVID-19 pandemic. Pharmacovigilance also had to meet unprecedented needs. In this article, unique aspects of COVID-19 vaccine pharmacovigilance encountered by one MAH will be summarized.
Full article
(This article belongs to the Special Issue Vaccination, Public Health and Epidemiology)
Open AccessArticle
Antibody Response Against SARS-CoV-2 Spike Protein in People with HIV After COVID-19 Vaccination
by
María José Muñoz-Gómez, Pablo Ryan, Marta Quero-Delgado, María Martin-Vicente, Guillermo Cuevas, Jorge Valencia, Eva Jiménez, Natalia Blanca-López, Samuel Manzano, Juan Ignacio Lazo, Vicente Mas, Mónica Vázquez, Daniel Sepúlveda-Crespo, Juan Torres-Macho, Isidoro Martínez and Salvador Resino
Vaccines 2025, 13(5), 480; https://doi.org/10.3390/vaccines13050480 - 29 Apr 2025
Abstract
Background/Objectives: People with HIV (PWH) often have a suboptimal response to vaccines, raising concerns regarding the efficacy of coronavirus disease 2019 (COVID-19) vaccines in this population. We aimed to evaluate the humoral immune response to the B.1 lineage and Omicron variant in PWH
[...] Read more.
Background/Objectives: People with HIV (PWH) often have a suboptimal response to vaccines, raising concerns regarding the efficacy of coronavirus disease 2019 (COVID-19) vaccines in this population. We aimed to evaluate the humoral immune response to the B.1 lineage and Omicron variant in PWH on antiretroviral therapy (ART) following COVID-19 vaccination. Methods: We conducted a prospective study of 19 PWH on ART who received a two-dose series of the COVID-19 mRNA vaccine and a booster six months later. Participants without HIV infection (n = 25) were included as a healthy control (HC) group. The humoral response to the COVID-19 vaccine (anti-SARS-CoV-2 S IgG levels and ability to block ACE2-S interaction) against both the original B.1 lineage and the Omicron variant was assessed using immunoassays. Results: The humoral response in PWH was very strong (geometric mean fold rise, GMFR > 8) after the second dose and strong (GMFR > 4) after the booster dose for both the B.1 lineage and the Omicron variant. We found comparable humoral responses to the B.1 lineage and Omicron variant between PWH and HC groups after the second and booster doses (q-value > 0.05). The COVID-19 vaccine generated a significantly weaker humoral response against the Omicron variant compared to the B.1 lineage in both groups (q-value < 0.05). However, this response improved after the booster dose, although it remained weaker in PWH. Conclusions: PWH showed a strong humoral response to the COVID-19 vaccine against B.1 and Omicron, though the Omicron response was weaker than B.1. Booster doses in PWH improved the Omicron response, but it stayed lower than B.1. Findings confirm vaccine effectiveness in PWH, stressing the critical role of boosters and potential need for updated vaccines for variants like Omicron.
Full article
(This article belongs to the Special Issue Vaccines and Vaccination: HIV, Hepatitis Viruses, and HPV)
►▼
Show Figures
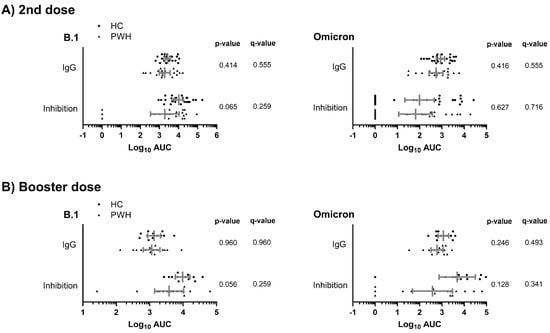
Figure 1
Open AccessOpinion
Value of Vaccinations: A Fundamental Public Health Priority to Be Fully Evaluated
by
Sara Boccalini
Vaccines 2025, 13(5), 479; https://doi.org/10.3390/vaccines13050479 - 29 Apr 2025
Abstract
Introduction: Vaccinations are one of the most impactful public health interventions, saving millions of lives annually and reducing the spread of infectious diseases. Numerous vaccines are expected to become available in the future. Decision-makers will have to thoroughly evaluate them. It is essential
[...] Read more.
Introduction: Vaccinations are one of the most impactful public health interventions, saving millions of lives annually and reducing the spread of infectious diseases. Numerous vaccines are expected to become available in the future. Decision-makers will have to thoroughly evaluate them. It is essential to fully comprehend the value of vaccinations to effectively and efficiently guide decisions. Methods: This work aims to highlight the multifaceted benefits of vaccination, extending beyond clinical outcomes to encompass profound economic and societal advantages. Results: Vaccinations should be considered an investment, not a cost. In comparison to other health expenditures, the vaccine costs can be considered moderate. Vaccinations can also reduce the fiscal burden by avoiding diseases, minimizing lost workdays and absenteeism, lowering disability claims, and increasing workforce productivity. The costs of non-vaccination represent a relevant issue. Vaccination also plays a key role in addressing the global challenge of antimicrobial resistance. Apart from quantifiable economic parameters, vaccines also have intangible benefits reducing pain and avoiding quality of life lost and deaths. Conclusions: Comprehensive Health Technology Assessments are required to understand the overall value of vaccinations.
Full article
(This article belongs to the Special Issue Estimating Vaccines' Value and Impact)
►▼
Show Figures
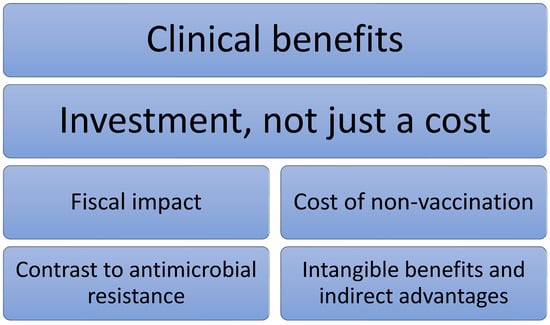
Figure 1
Open AccessReview
EBV Vaccines in the Prevention and Treatment of Nasopharyngeal Carcinoma
by
Weiwei Zhang, Chuang Wang, Yousheng Meng, Lang He and Mingqing Dong
Vaccines 2025, 13(5), 478; https://doi.org/10.3390/vaccines13050478 - 29 Apr 2025
Abstract
Epstein–Barr virus (EBV), a ubiquitous human herpesvirus, has been robustly linked to the pathogenesis of nasopharyngeal carcinoma (NPC). The mechanism of EBV-induced NPC involves complex interactions between viral proteins and host cell pathways. This review aims to comprehensively outline the mechanism of EBV-induced
[...] Read more.
Epstein–Barr virus (EBV), a ubiquitous human herpesvirus, has been robustly linked to the pathogenesis of nasopharyngeal carcinoma (NPC). The mechanism of EBV-induced NPC involves complex interactions between viral proteins and host cell pathways. This review aims to comprehensively outline the mechanism of EBV-induced NPC and the latest advances in targeted EBV vaccines for prophylaxis and treatment. This review explores the intricate molecular mechanisms by which EBV contributes to NPC pathogenesis, highlighting viral latency, genetic and epigenetic alterations, and immune evasion strategies. It emphasizes the pivotal role of key viral proteins, including EBNA1, LMP1, and LMP2A, in carcinogenesis. Subsequently, the discussion shifts towards the development of targeted EBV vaccines, including preventive vaccines aimed at preventing primary EBV infection and therapeutic vaccines aimed at treating diagnosed EBV-related NPC. The review underscores the challenges and future directions in the field, stressing the importance of developing innovative vaccine strategies and combination therapies to improve efficacy. This review synthesizes current insights into the molecular mechanisms of EBV-induced NPC and the development of EBV-targeted vaccines, highlighting the potential use of mRNA vaccines for NPC treatment.
Full article
(This article belongs to the Special Issue Tumor Antigen-Based Anticancer Vaccine and Immunotherapy)
►▼
Show Figures
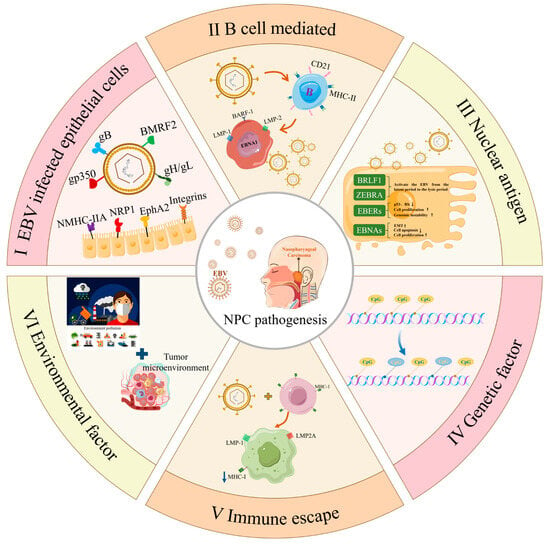
Figure 1
Open AccessReview
Herpes Zoster Vaccination: Insights into Efficacy, Safety, and Guidelines
by
Michał Oleszko, Paweł Zapolnik and Hanna Czajka
Vaccines 2025, 13(5), 477; https://doi.org/10.3390/vaccines13050477 - 28 Apr 2025
Abstract
Background: The varicella–zoster virus (VZV) is a human herpesvirus that primarily causes varicella (chickenpox) as an initial infection, characterized by distinctive skin lesions. It can later reactivate, leading to herpes zoster (shingles). Once reactivated, VZV infection may result in serious complications, the most
[...] Read more.
Background: The varicella–zoster virus (VZV) is a human herpesvirus that primarily causes varicella (chickenpox) as an initial infection, characterized by distinctive skin lesions. It can later reactivate, leading to herpes zoster (shingles). Once reactivated, VZV infection may result in serious complications, the most common being postherpetic neuralgia. Fortunately, vaccination can prevent this condition. Objectives: In this study, we provide a comprehensive analysis of zoster vaccines, including clinical trials, safety profiles, and reimbursement guidelines across various countries. Results: Our findings confirm the vaccine’s effectiveness and safety across diverse populations, aligning with previous clinical trials and real-world data, and summarize global vaccination guidelines.
Full article
(This article belongs to the Special Issue Varicella and Zoster Vaccination)
Open AccessReview
Emerging Immunotherapies in Lung Cancer: The Latest Advances and the Future of mRNA Vaccines
by
Raquel Ramos and Nuno Vale
Vaccines 2025, 13(5), 476; https://doi.org/10.3390/vaccines13050476 - 28 Apr 2025
Abstract
Lung cancer is the most lethal malignancy worldwide, having the highest incidence rate. This is a heterogeneous disease classified according to its histological and molecular characteristics. Depending on these, different therapeutic approaches have already been approved for lung cancer treatment targeting genetic alterations
[...] Read more.
Lung cancer is the most lethal malignancy worldwide, having the highest incidence rate. This is a heterogeneous disease classified according to its histological and molecular characteristics. Depending on these, different therapeutic approaches have already been approved for lung cancer treatment targeting genetic alterations or even the immune system. Nonetheless, other therapies are being studied to continuously improve the care and survival of lung cancer patients. Among them, immunotherapies are one of the main targets of investigation to try and combat the ability of some malignant cells to evade anti-tumor responses mediated by the immune system. Cancer vaccine development has emerged as a promising approach to strengthen the patient’s immune system and combat the disease, especially mRNA vaccines. Currently, there are several ongoing studies investigating the therapeutic efficacy of mRNA vaccines in lung cancer treatment alone or combined with other therapeutic drugs. This review aims to highlight the importance of immunotherapy in lung cancer treatment, presenting the most recent advances particularly in mRNA-based vaccines as well as the challenges and future perspectives.
Full article
(This article belongs to the Special Issue Advances in Cancer Immunotherapy and Vaccines Research: 2nd Edition)
►▼
Show Figures
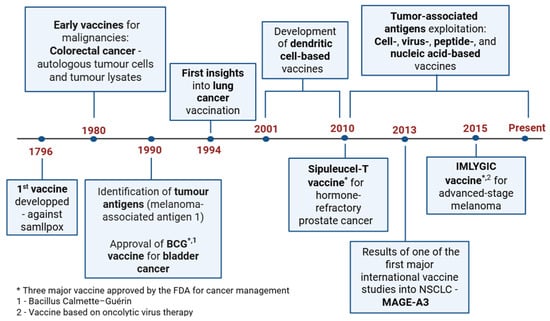
Figure 1
Open AccessArticle
Epidemiological Impact of Increasing Vaccination Coverage Rate and Re-Vaccination on Pneumococcal Disease in Older Adults in Germany
by
Oluwaseun Sharomi, Marion de Lepper, Sarah Mihm-Sippel, Thorsten Reuter, Claudia Solleder, Giulio Meleleo, Tufail M. Malik, Kevin M. Bakker and Rachel J. Oidtman
Vaccines 2025, 13(5), 475; https://doi.org/10.3390/vaccines13050475 - 28 Apr 2025
Abstract
Background/Objectives: The clinical impact of replacing the 23-valent pneumococcal polysaccharide vaccine (PPSV23) for the vaccination of older (≥60 years) and at-risk German adults with either the 20-valent (PCV20) or 21-valent (V116) pneumococcal conjugate vaccine (PCV) was evaluated. Methods: An age- and serotype-specific transmission
[...] Read more.
Background/Objectives: The clinical impact of replacing the 23-valent pneumococcal polysaccharide vaccine (PPSV23) for the vaccination of older (≥60 years) and at-risk German adults with either the 20-valent (PCV20) or 21-valent (V116) pneumococcal conjugate vaccine (PCV) was evaluated. Methods: An age- and serotype-specific transmission model was adapted to Germany to evaluate the impact of V116 versus PCV20 vaccination on pneumococcal disease (PD) incidence, including invasive pneumococcal disease (IPD) and inpatient and outpatient non-bacteremic pneumococcal pneumonia, over 10 years. A reference strategy (PPSV23 vaccination at a constant 30% vaccine coverage rate (VCR)) was compared against eight strategies varying by PCV (PCV20 vs. V116), VCR (30% vs. 60%), with or without the PCV revaccination of previously PPSV23-vaccinated adults (0% vs. 50% revaccination). Results: Vaccination with PCV20 and V116 initially decreased PD incidence, but incidence returned to pre-vaccine levels after five and eight years, respectively. Increasing the VCR to 60% prevented this resurgence. At a 10-year time horizon, V116 with 30% VCR reduced IPD cases by 9%, inpatient NBPP cases by 10%, and outpatient NBPP cases by 7% compared to the reference strategy. PCV20 with 30% VCR reduced these cases by 6%, 5%, and 4%, respectively. Increasing the VCR to 60% and revaccinating 50% of previously PPSV23-vaccinated adults further reduced IPD cases by 14% and 13% for V116, and by 9% and 9% for PCV20. Conclusions: Increasing the vaccination coverage rate to 60% and strategically revaccinating previously PPSV23-vaccinated adults significantly enhanced the effectiveness of pneumococcal vaccines, with V116 showing greater overall reductions in disease incidence compared to PCV20 or PPSV23.
Full article
(This article belongs to the Special Issue Pneumococcal Vaccines: Current Status and Future Prospects)
►▼
Show Figures
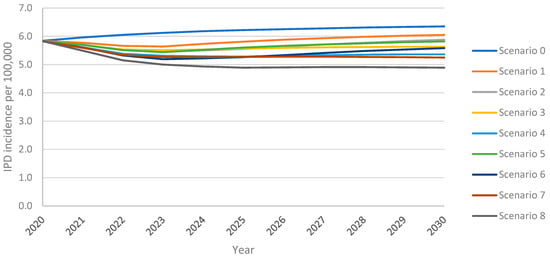
Figure 1
Open AccessArticle
Impact of Chitosan Nanoparticles-Coated Dendritic Cell-Based Vaccine as Cancer Immunotherapy
by
Jehan S. Alrahimi, Najla S. Alotaibi, Alia M. Aldahlawi, Fatemah S. Basingab and Kawther A. Zaher
Vaccines 2025, 13(5), 474; https://doi.org/10.3390/vaccines13050474 - 28 Apr 2025
Abstract
Dendritic cells (DCs) are major contributors to generating an effective immune response due to their ability to present antigens to T cells. Recently, nanoparticles have been widely used in different medical applications, such as drug-delivery systems, to enhance the function of impaired immune
[...] Read more.
Dendritic cells (DCs) are major contributors to generating an effective immune response due to their ability to present antigens to T cells. Recently, nanoparticles have been widely used in different medical applications, such as drug-delivery systems, to enhance the function of impaired immune cells. Objectives: This research aims to develop an effective antitumor DC-based vaccine by adsorption of chitosan-nanoparticles (CH-NPs) onto DCs. Methods: Undifferentiated mouse bone marrow progenitor cells were differentiated into mature DCs using cytokines and lipopolysaccharides. CH-NPs were prepared using the ionic gelation method and subsequently used to coat the stimulated DCs. The MTT assay was employed to assess the cytotoxicity of all formulations. To compare the antitumor effect of CH-NPs, DCs, and DCs-CH-NPs, mice were divided into five groups and injected with the respective vaccine formulations. Following immunization, flow cytometry was used to analyze DC and CD4+ T cell activation in blood and spleen tissues. Histological samples from the spleen and lymph nodes were also collected. Results: Our findings show that co-stimulatory molecules CD80/CD86 and the DC maturation marker CD83 were upregulated in the vaccinated DCs, indicating their maturation. Moreover, CD83, CD11c, and MHC-II were upregulated in blood and spleen samples in vivo. The DC-CH-NPs vaccinated group had a higher mean percentage of CD83 expression in blood samples (76.7 ± 17.1) compared to the DCs group (47.7 ± 11.0) and the CH-NPs group (37.7 ± 8.6). DC markers, particularly CD83, were highly expressed in spleen samples. Additionally, the DC-CH-NPs vaccinated group had a significantly higher number of CD4+ T cells (MFI = 26.1 ± 2.3) compared to the DCs (18.6 ± 1.6) and CH-NPs (13.3 ± 1.4) groups. Conclusions: The present study concludes that the DC-CH-NPs vaccine formulation can induce a potent in vivo immune response. These data may provide valuable insights for developing effective delivery systems for antitumor vaccines.
Full article
(This article belongs to the Special Issue Cutting-Edge Cancer Vaccines Enhanced by Nanotechnology)
►▼
Show Figures
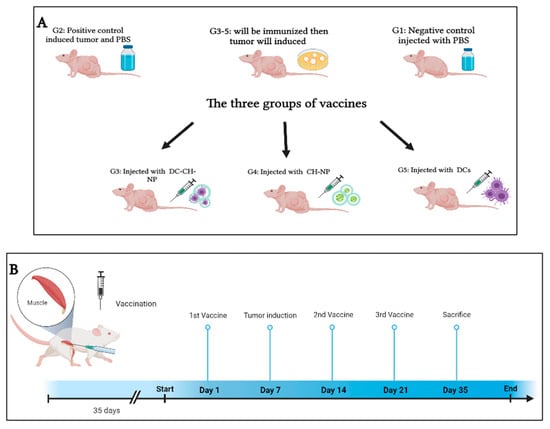
Figure 1
Open AccessReview
Considerations for mRNA Product Development, Regulation and Deployment Across the Lifecycle
by
John H Skerritt
Vaccines 2025, 13(5), 473; https://doi.org/10.3390/vaccines13050473 - 28 Apr 2025
Abstract
With the successful deployment of several mRNA vaccines against SARS-CoV-2, an mRNA vaccine against RSV (respiratory syncytial virus) and a large pipeline of mRNA products against other infectious diseases, cancers and rare diseases, it is important to examine the whole product lifecycle. mRNA
[...] Read more.
With the successful deployment of several mRNA vaccines against SARS-CoV-2, an mRNA vaccine against RSV (respiratory syncytial virus) and a large pipeline of mRNA products against other infectious diseases, cancers and rare diseases, it is important to examine the whole product lifecycle. mRNA technology enables product design, testing and manufacturing systems to be rapidly developed, but these advantages can be lost if other factors that determine public access are not closely considered. This review analyzes key aspects of the mRNA product lifecycle including candidate design, manufacturing, quality systems and product safety and storage. Regulatory thinking is well advanced in some countries but not others, but more thought on the regulation of mRNA vaccines outside of a pandemic situation as well as mRNA therapeutics including individual neoantigen therapies and rare disease treatments is needed. Consumer acceptance—the “social license to operate” around mRNA products—is critical for their uptake, particularly outside of a pandemic.
Full article
(This article belongs to the Section DNA and mRNA Vaccines)
►▼
Show Figures
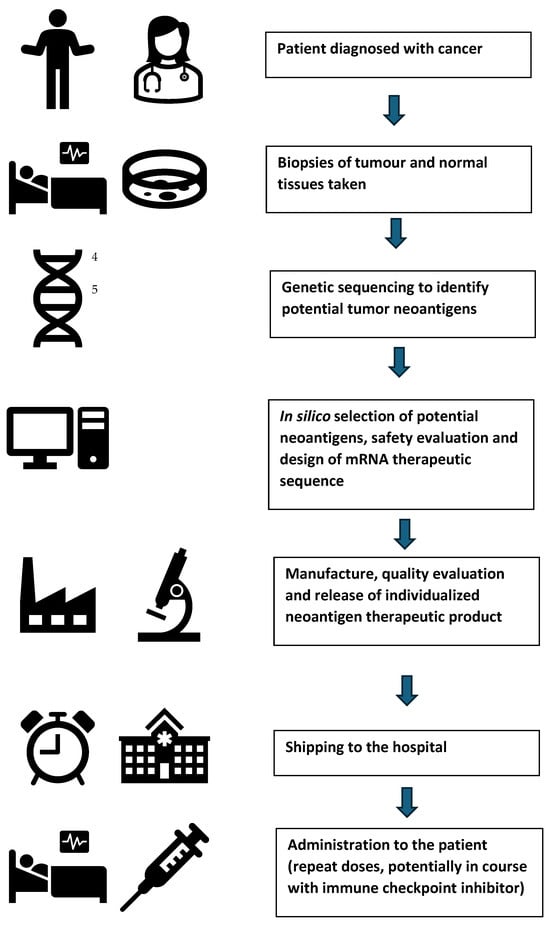
Figure 1
Open AccessArticle
Influenza Vaccination and Cardiovascular Outcomes in Patients with Coronary Artery Diseases: A Placebo-Controlled Randomized Study, IVCAD
by
Mohammadmoein Dehesh, Sharareh Gholamin, Seyed-Mostafa Razavi, Ali Eskandari, Hossein Vakili, Mohammad Rahnavardi Azari, Yunzhi Wang, Ethan K. Gough and Maryam Keshtkar-Jahromi
Vaccines 2025, 13(5), 472; https://doi.org/10.3390/vaccines13050472 - 27 Apr 2025
Abstract
Background/Objectives: Influenza infection is associated with cardiovascular morbidity and mortality; however, the effect of influenza vaccination on cardiovascular outcomes is not fully understood. This clinical trial aimed to investigate the correlation between cardiovascular outcomes and influenza vaccine (FluVac) in coronary artery disease
[...] Read more.
Background/Objectives: Influenza infection is associated with cardiovascular morbidity and mortality; however, the effect of influenza vaccination on cardiovascular outcomes is not fully understood. This clinical trial aimed to investigate the correlation between cardiovascular outcomes and influenza vaccine (FluVac) in coronary artery disease (CAD) subjects. Methods: This was a randomized single-blinded placebo-controlled trial. Enrolled CAD subjects received 0.5 mL of 2007–2008 trivalent FluVac (15 µg hemagglutinin of each of Solomon Islands/3/2006 (H1N1), Wisconsin/67/2005 (H3N2), and Malaysia/2506/2004 (B)). The subjects were followed up at 1 month (hemagglutinin (HA) antibody titers) and at 12 months post-vaccination for evaluation of outcomes (influenza-like episodes, acute coronary syndrome (ACS), myocardial infarction (MI), coronary revascularization, and death). Results: In total, 278 eligible CAD subjects were randomized to receive either FluVac (n = 137) or a placebo (n = 141), of which consequently 131 and 135 subjects completed the study. Cardiovascular deaths (3/131 [2.29%] vs. 3/135 [2.22%]) and all-cause deaths (4/131 [3.05%] vs. 4/135 [2.96%]) were similar in both groups. Adverse cardiovascular events, including ACS, MI, and coronary revascularization, were less frequent in the vaccine group but did not reach statistical significance. The magnitude of the antibody change and serologic response (≥4-fold HI titer rise) of all three antibodies were significantly higher in the vaccine group compared to the placebo but did not correlate with cardiovascular outcomes in the FluVac group. Conclusions: The influenza vaccine may improve cardiovascular outcomes, though this improvement is not correlated with post-vaccination antibody titers. Despite the controversy, influenza vaccination is recommended in the CAD population (clinicaltrials.gov; NCT00607178).
Full article
(This article belongs to the Special Issue The Recent Development of Influenza Vaccine: 2nd Edition)
►▼
Show Figures
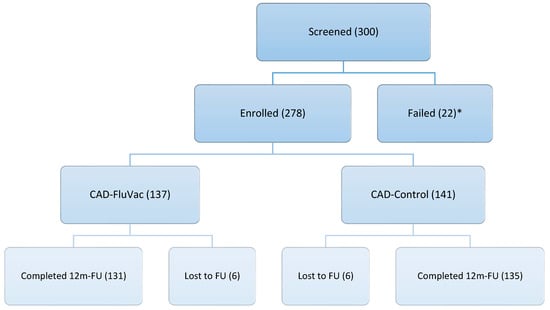
Figure 1
Open AccessArticle
Isolation and Characterization of E8 Monoclonal Antibodies from Donors Vaccinated with Recombinant Vaccinia Vaccine with Efficient Neutralization of Authentic Monkeypox Virus
by
Yutao Shi, Shuhui Wang, Yanling Hao, Xiuli Shen, Jun Zhang, Shuo Wang, Junjie Zhang, Yuyu Fu, Ran Chen, Dong Wang, Yiming Shao, Dan Li and Ying Liu
Vaccines 2025, 13(5), 471; https://doi.org/10.3390/vaccines13050471 - 27 Apr 2025
Abstract
►▼
Show Figures
Background/Objectives: Monkeypox, twice declared a public health emergency of international concern by the WHO, currently lacks approved targeted therapeutics. This study focused on the development of monkeypox virus (MPXV) E8-specific human monoclonal antibodies (mAbs) derived from recipients of the recombinant vaccinia vaccine (rTV),
[...] Read more.
Background/Objectives: Monkeypox, twice declared a public health emergency of international concern by the WHO, currently lacks approved targeted therapeutics. This study focused on the development of monkeypox virus (MPXV) E8-specific human monoclonal antibodies (mAbs) derived from recipients of the recombinant vaccinia vaccine (rTV), with subsequent evaluation of their cross-neutralizing activity against orthopoxviruses, including the vaccinia virus (VACV) and MPXV. Methods: Three mAbs (C5, C9, and F8) were isolated from rTV vaccinees. Structural mapping characterized their binding domains on the MPXV E8 and VACV D8 proteins. Neutralization potency was assessed against the VACV TianTan strain and MPXV clade IIb. A combo was further evaluated in a VACV-infected mice model for clinical recovery and viral load reduction. Complement-dependent enhancement mechanisms were also investigated in vitro. Results: C9 targets the virion surface region of E8 and both the virion surface region and intravirion region of D8, showing cross-neutralization activity against the MPXV (IC50 = 3.0 μg/mL) and VACV (IC50 = 51.1 ng/mL) in vitro. All three antibodies demonstrated potent neutralization against the VACV in vitro: C5 (IC50 = 3.9 ng/mL), C9 (IC50 = 51.1 ng/mL), and F8 (IC50 = 101.1 ng/mL). Notably, complement enhanced neutralization against the VACV by >50-fold, although no enhancement was observed for the MPXV. In vivo administration accelerated clinical recovery by 24 h and achieved significant viral clearance (0.9-log reduction). Conclusions: E8-targeting mAbs exhibited broad-spectrum neutralization against orthopoxviruses, demonstrating therapeutic potential against both historical (VACV) and emerging (MPXV) pathogens. However, MPXV’s resistance to complement-dependent enhancement highlights the necessity for pathogen-adapted optimization. These findings establish E8 as a critical conserved target for pan-poxvirus VACV and MPXV countermeasure development.
Full article
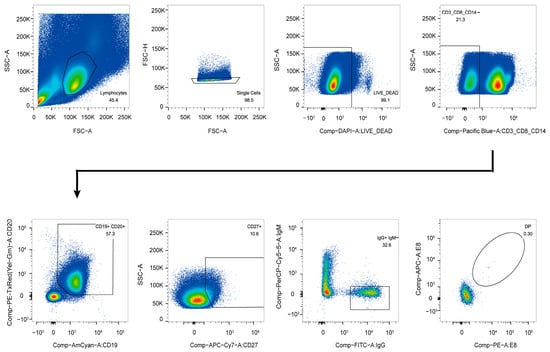
Figure 1
Open AccessReview
Administration of Nirsevimab for RSV Prophylaxis in Infants: A Comprehensive Review
by
Pan-Pan Wu and Fang-Rui Ding
Vaccines 2025, 13(5), 470; https://doi.org/10.3390/vaccines13050470 - 27 Apr 2025
Abstract
Respiratory syncytial virus (RSV) is the primary etiological agent responsible for lower respiratory tract infections (LRTIs) and hospitalizations among infants. Nirsevimab, a novel monoclonal antibody (mAb), offers sustained protection against RSV for a minimum of 5 months in neonates and young children. Extensive
[...] Read more.
Respiratory syncytial virus (RSV) is the primary etiological agent responsible for lower respiratory tract infections (LRTIs) and hospitalizations among infants. Nirsevimab, a novel monoclonal antibody (mAb), offers sustained protection against RSV for a minimum of 5 months in neonates and young children. Extensive clinical trials and real-world evidence have demonstrated that nirsevimab significantly mitigates the incidence and severity of RSV infections in infants, while exhibiting favorable safety profiles and cost-effectiveness. Regulatory authorities in multiple countries have approved nirsevimab, and its implementation is progressively expanding across various healthcare settings. However, several critical issues require further attention. Specifically, a more in-depth investigation into the long-term efficacy and benefits of nirsevimab across diverse populations, particularly neonates, is essential. Additionally, accelerating the introduction and administration of nirsevimab in developing countries remains imperative. Thus, this review comprehensively summarizes the administration of nirsevimab in infants to facilitate its broader application.
Full article
(This article belongs to the Special Issue Immune Response After Respiratory Infection or Vaccination)
►▼
Show Figures
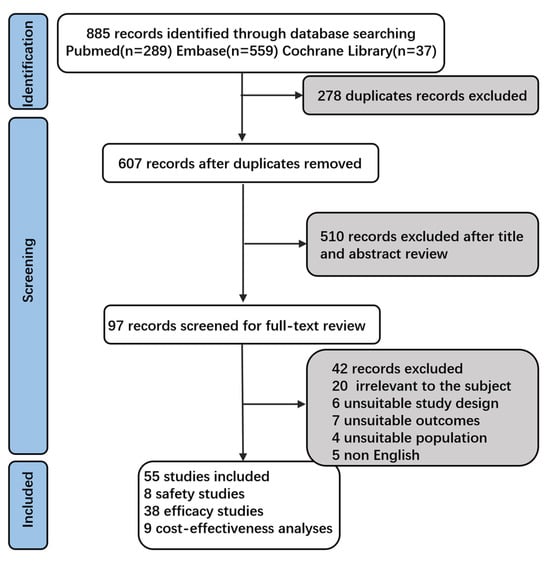
Figure 1
Open AccessReview
Clinical Translation Challenges and Strategies for Tumour Vaccines Considering Multiple Delivery Routes
by
Ruiyun Song, Xiao Li, Junsong Zhu, Jian He and Jintong Na
Vaccines 2025, 13(5), 469; https://doi.org/10.3390/vaccines13050469 - 27 Apr 2025
Abstract
►▼
Show Figures
Background: The high incidence and mortality rates of cancer have kept it at the top of the research agenda for the global healthcare industry, as well as put serious economic pressure on families and society. It has gradually been recognised that reducing the
[...] Read more.
Background: The high incidence and mortality rates of cancer have kept it at the top of the research agenda for the global healthcare industry, as well as put serious economic pressure on families and society. It has gradually been recognised that reducing the incidence of cancer through various interventions and that combining prevention and treatment are the key to alleviating the burden of cancer. Methods: Retrieve and summarize the literature related to the delivery methods of tumor vaccines, and investigate whether these delivery methods have been applied clinically or have been used in clinical trials. Results: there are a variety of methods for cancer vaccine development, but only a very small number of studies have been able to make strides towards implementing these methods in the clinic, which is closely linked to drawbacks with the means of vaccine delivery. Conclusions: This review analyses the reasons why it is difficult to apply these methods in the clinic from the point of view of the delivery method rather than the design of the cancer vaccine. It also describes some of the delivery methods that have not yet been applied for cancer vaccines and, considering this in conjunction with those that are currently used for this purpose, predicts their prospects for future application.
Full article

Graphical abstract
Open AccessArticle
A Cyclic-di-AMP Adjuvanted CPAF Protein Vaccine Is Immunogenic in Swine, but It Fails to Reduce Genital Chlamydia trachomatis Burden
by
Leonie Bettin, Maria Stadler, Christine Unterweger, Maximiliane Dippel, Jonathan M. Harris, Andrea Buzanich-Ladinig, Taylor B. Poston, Toni Darville and Tobias Käser
Vaccines 2025, 13(5), 468; https://doi.org/10.3390/vaccines13050468 - 27 Apr 2025
Abstract
Background/Objectives: Chlamydia trachomatis (Ct) is the leading bacterial cause of sexually transmitted infection globally. If undiagnosed or left untreated, these infections can lead to serious complications such as infertility, ectopic pregnancies, and chronic pelvic pain. Despite the high prevalence and
[...] Read more.
Background/Objectives: Chlamydia trachomatis (Ct) is the leading bacterial cause of sexually transmitted infection globally. If undiagnosed or left untreated, these infections can lead to serious complications such as infertility, ectopic pregnancies, and chronic pelvic pain. Despite the high prevalence and potential for serious health complications, no vaccine has been licensed. Pigs offer a valuable biomedical model for chlamydia research: they have an overall high degree of similarity to humans and serve as natural hosts for Chlamydia suis (Cs), a close relative of Ct. Thus, in this study, the pig model was used to evaluate a vaccine candidate against Ct. Methods: The vaccine candidate consists of chlamydial-protease-like activity factor (CPAF) protein adjuvanted with STING (Stimulator of Interferon Genes) pathway agonist cyclic-di-AMP (c-di-AMP). Pigs received two doses intramuscularly followed by two intranasal doses. Each week, the systemic T cell response was assessed via IFN-γ and IL-17 ELISpots, as well as multi-parameter flow cytometry on 0, 14, and 28 days post vaccination (dpv). The humoral immune response was analyzed by measuring CPAF-specific antibody levels and avidity via ELISAs. Results: Vaccination with c-di-AMP adjuvanted CPAF triggered low-level systemic IFN-γ and multifunctional IFN-γ+TNF-α+ CD4 T cell responses. Despite the rather low systemic effector cytokine production, robust anti-CPAF IgG responses were detected in serum, vaginal swab eluates, and oviduct flushes. Genital Ct challenge 42 dpv resulted in only transient infection, precluding a confident assessment of vaccine efficacy of the tested CPAF/c-di-AMP vaccine candidate. However, after challenge, vaccinated pigs exhibited boosted systemic anti-CPAF IFN-γ and mucosal IgG responses compared to unvaccinated pigs. Conclusions: Thus, while vaccine efficacy remains elusive, the CPAF/c-di-AMP vaccine candidate was immunogenic: it elicited a low-level systemic cell-mediated response and robust humoral immune responses. Future studies will incorporate a STING agonist directly conjugated to CPAF as well as addition of other Th1-inducing adjuvants to enhance cellular immunity.
Full article
(This article belongs to the Special Issue Challenges to Developing New Vaccines and Improving Existing Platforms)
►▼
Show Figures
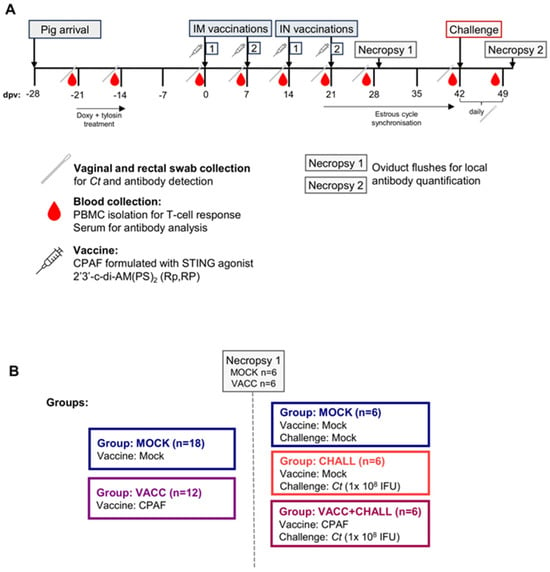
Figure 1
Open AccessArticle
The Safety and Immunogenicity of a Quadrivalent Influenza Subunit Vaccine in Healthy Children Aged 6–35 Months: A Randomized, Blinded and Positive-Controlled Phase III Clinical Trial
by
Lili Huang, Guangfu Li, Yuhui Zhang, Xue Zhao, Kai Wang, Chunyu Jia, Wei Zhang, Jiebing Tan, Xiaofen Chen, Qin Li, Hongyan Jiang, Rui An, Wenna Leng, Yongli Yang, Youcai An, Yanxia Wang and Yaodong Zhang
Vaccines 2025, 13(5), 467; https://doi.org/10.3390/vaccines13050467 - 26 Apr 2025
Abstract
Background: Influenza is a serious contagious disease caused by influenza virus. It is particularly dangerous for children, potentially leading to severe and even fatal complications. The aim of this study was to evaluate the safety and immunogenicity of two candidate quadrivalent influenza
[...] Read more.
Background: Influenza is a serious contagious disease caused by influenza virus. It is particularly dangerous for children, potentially leading to severe and even fatal complications. The aim of this study was to evaluate the safety and immunogenicity of two candidate quadrivalent influenza subunit vaccines in children aged 6–35 months. Methods: The subjects were randomly divided into three groups at a 1:1:1 ratio and received the corresponding vaccines: QIV-Sub-HD (Quadrivalent Influenza Subunit Vaccine, High Dose), QIV-Sub-LD (Quadrivalent Influenza Subunit Vaccine, Low Dose) and QIV-Split-LD (Quadrivalent Influenza Split-Virion Vaccine, Low Dose). Adverse events were recorded at 30 min, 0–7 days and 8–28 and 30 days after each dose of immunization. Serious adverse events (SAEs) were collected and reported within 6 months after the full vaccination. Blood samples were collected before the first dose and on 28 days, 3 months and 6 months after full vaccination for antibody detection to evaluate the immunogenicity and duration of immune responses. Results: The results showed that the relative and absolute criteria met the goals set by the clinical trial protocol, indicating that both vaccines are immunogenic. From the first dose to 30 days after full vaccination, the total incidence of adverse reactions in the QIV-Sub-HD, QIV-Sub-LD and QIV-Split-LD groups was 29.64%, 33.33% and 29.64%, respectively. The main symptoms were fever, cough, diarrhea and vomiting. No new safety concerns were identified. Conclusions: The quadrivalent influenza subunit vaccines candidate, manufactured by Ab&B Bio-tech Co., Ltd. JS., are safe and immunogenic in children aged 6–35 months.
Full article
(This article belongs to the Special Issue Human Immune Responses to Infection and Vaccination)
►▼
Show Figures
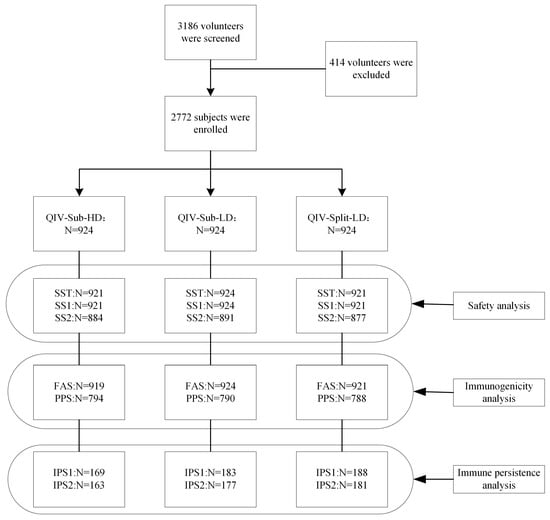
Figure 1
Open AccessReview
Recent Advances in Mpox Epidemic: Global Features and Vaccine Prevention Research
by
Xinling Zhang, Dong-Ang Liu, Yuting Qiu, Ruiyao Hu, Shiyu Chen, Yue Xu, Keyi Chen, Jinghua Yuan and Xiaoping Li
Vaccines 2025, 13(5), 466; https://doi.org/10.3390/vaccines13050466 - 25 Apr 2025
Abstract
Monkeypox (mpox) is a zoonotic disease (zoonose) caused by the monkeypox virus (MPXV). MPXV, a member of the Orthopoxviridae family, is categorized into two clades, Central Africa (I) and West Africa (II), each of which is further subdivided into subclades a and b.
[...] Read more.
Monkeypox (mpox) is a zoonotic disease (zoonose) caused by the monkeypox virus (MPXV). MPXV, a member of the Orthopoxviridae family, is categorized into two clades, Central Africa (I) and West Africa (II), each of which is further subdivided into subclades a and b. Clade I generally causes more serious illness and higher mortality rates, while Clade II results in milder illness. Historically, mpox epidemics were localized to specific regions and countries in Africa. Since 2022, the mpox epidemic, fueled by MPXV Clade IIb, has swiftly spread across various nations and regions, jeopardizing public health and safety. However, starting in 2024, Clade Ib gradually replaced Clade IIb. The notable genetic variation in Clade Ib may provide MPXV with new opportunities to evade the immune system and adapt to hosts. According to the World Health Organization (WHO), from 1 January 2022, to 24 November 2024, there were 117,663 confirmed cases and 2 probable cases, resulting in 263 deaths across 127 Member States in all six WHO regions. As of 9 January 2025, 12 countries outside Africa have reported imported MPXV Clade Ib cases, with secondary cases emerging in the United Kingdom, Germany, and China. Due to the incomplete development of a vaccine specifically for MPXV, the smallpox vaccine remains in use for preventing mpox or for emergency vaccination post-exposure. Therefore, the persistent spread of mpox is still a major concern, requiring greater awareness and vaccination efforts in populations at high risk. This paper aims to summarize the etiological characteristics, epidemic situation, and vaccine prevention efforts for mpox, offering a reference for managing this serious epidemic and ensuring effective scientific prevention and control.
Full article
(This article belongs to the Section Epidemiology)
►▼
Show Figures

Figure 1
Open AccessReview
COVID-19 Vaccination in Patients with Hematological Malignances
by
Massimo Franchini, Fabrizio Maggi and Daniele Focosi
Vaccines 2025, 13(5), 465; https://doi.org/10.3390/vaccines13050465 - 25 Apr 2025
Abstract
Patients with hematologic malignancies (HM) represent a population particularly vulnerable to infections due to their cancer-related immune deficiency and the immunosuppressive treatment they are administered. Accordingly, a high hospitalization and mortality rate has been consistently reported in such a frail population during the
[...] Read more.
Patients with hematologic malignancies (HM) represent a population particularly vulnerable to infections due to their cancer-related immune deficiency and the immunosuppressive treatment they are administered. Accordingly, a high hospitalization and mortality rate has been consistently reported in such a frail population during the first COVID-19 pandemic waves. After a brief description of the clinical impact of SARS-CoV-2 infection in patients with blood cancers, this narrative review is focused on the protective effect of COVID-19 vaccines in patients with HM. All in all, the results from the literature analysis indicate that booster shots in fully vaccinated HM patients are significantly able to increase seroconversion rates, which represent the best surrogate of vaccine efficacy. Despite these encouraging data, concerns still remain regarding the lower immune responses to COVID-19 vaccines, even to booster doses, in severely immunosuppressed HM patients, such as those receiving anti-CD20 monoclonal antibody therapies and hematopoietic stem cell transplants.
Full article
(This article belongs to the Special Issue Immunization of Immunosuppressed Patients)
Open AccessArticle
Immunogenicity of an Intranasal Dual (Core and Surface)-Antigen Vaccine Against Hepatitis B Virus Enhanced by Carboxyl-Vinyl Polymer Excipients
by
Md Haroon Or Rashid, Fumihiko Yasui, Takahiro Sanada, Risa Kono, Tomoko Honda, Bouchra Kitab, Lipi Akter, Masashi Utsunomiya, Risa Sato, Osamu Yoshida, Yoichi Hiasa, Yasunori Oda, Yasumasa Goh, Takashi Miyazaki, Michinori Kohara and Kyoko Tsukiyama-Kohara
Vaccines 2025, 13(5), 464; https://doi.org/10.3390/vaccines13050464 - 25 Apr 2025
Abstract
Background: Hepatitis B virus (HBV) is a major cause of morbidity and mortality globally, and chronic infections are associated with cirrhosis and hepatocellular carcinoma. Issues with conventional treatments and vaccines mean there is a need for new therapeutic vaccines, which must elicit a
[...] Read more.
Background: Hepatitis B virus (HBV) is a major cause of morbidity and mortality globally, and chronic infections are associated with cirrhosis and hepatocellular carcinoma. Issues with conventional treatments and vaccines mean there is a need for new therapeutic vaccines, which must elicit a strong and sustainable immune response. Here, we evaluated the immunogenicity of dual-antigen vaccines containing hybrid surface (hy-LHBs) and core (HBc) antigens, combined with a carboxyl-vinyl polymer (CVP) as a mucoadhesive excipient, following intranasal administration in mice. Methods: Mice were intranasally administered a mixed vaccine (10 µg of hy-LHBs and 2.5 or 10 µg of HBc) with or without a CVP excipient, and they were assessed for their immune response (levels of IgGs or IgA antibodies in an ELISA, IFN-γ level in splenocytes in an ELISpot assay, and cytokine/chemokine levels in a BioPlex assay). A protein stability assay was also conducted for vaccine formulations with and without excipients. Results: Significantly enhanced IgG production was noted targeting hy-LHBs and (less markedly) HBc at 10 µg/antigen, but only a non-significant elevation was noted with the vaccine containing 2.5 µg HBc. The BioPlex assay showed a significant increase in IL-2 (#00-07, 0B), IL-12(p40)(#00), eotaxin (#00), MIP1α (#00, #00-07, 0B), and MCP-1 (#00-07, 0B) in mice that received treatment compared to those of untreated mice. The endpoint titers of IgG1 and IgG2a were measured, which were higher with CVP excipients than without. From the IgG2a/IgG1 ratio, a higher IgG1 response was induced by CVPs to hy-LHBs and a higher IgG2a response was induced to HBc. Th2-dominant phenotype to hy-LHBs was induced with CVP#00 in an ELISpot assay. The highest anti-hy-LHBs antibody titer was noted with the conventional CVP#00 excipient. Consistent with these results, a higher amount of neutralizing antibodies of HBV was induced with CVP#00 treatment and followed by #00-03 and #14-00. Conclusions: We consider that the addition of CVP excipients to vaccine formulation enhances immunogenicity and HBV antigen stability for intranasal vaccines. This effect was seen for both humoral and cell-mediated immune responses, indicating the potential of CVPs as excipients in intranasal HBV vaccines.
Full article
(This article belongs to the Section Hepatitis Virus Vaccines)
►▼
Show Figures
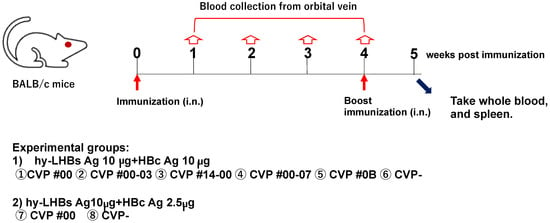
Figure 1

Journal Menu
► ▼ Journal Menu-
- Vaccines Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
2 April 2025
MDPI INSIGHTS: The CEO's Letter #21 - Annual Report, Swiss Consortium, IWD, ICARS, Serbia
MDPI INSIGHTS: The CEO's Letter #21 - Annual Report, Swiss Consortium, IWD, ICARS, Serbia
1 April 2025
Meet us at the 11th Congress of the European Academy of Neurology, 21–24 June 2025, Helsinki, Finland
Meet us at the 11th Congress of the European Academy of Neurology, 21–24 June 2025, Helsinki, Finland

Topics
Topic in
Animals, Arthropoda, Insects, Vaccines, Veterinary Sciences, Pathogens
Ticks and Tick-Borne Pathogens: 2nd Edition
Topic Editors: Alina Rodriguez-Mallon, Alejandro Cabezas-CruzDeadline: 31 March 2026

Conferences
Special Issues
Special Issue in
Vaccines
Current Development of Vaccines for Respiratory Viral Infection
Guest Editor: Ting ShiDeadline: 30 April 2025
Special Issue in
Vaccines
HPV Vaccination Coverage: Problems and Challenges
Guest Editors: Shillpa Naavaal, Zheng Quan Toh, Paul LicciardiDeadline: 30 April 2025
Special Issue in
Vaccines
Advances in DNA Vaccine Research
Guest Editor: Dabbu JaijyanDeadline: 30 April 2025
Special Issue in
Vaccines
Recent Advances in Vaccine Adjuvants and Formulation
Guest Editors: Aihua Zhao, Junli LiDeadline: 30 April 2025
Topical Collections
Topical Collection in
Vaccines
COVID-19 Vaccines and Vaccination
Collection Editors: Ralph Tripp, Scott Anthony
Topical Collection in
Vaccines
Factors Associated with Vaccine Hesitancy
Collection Editor: Brian D. Poole
Topical Collection in
Vaccines
COVID-19 Vaccine Hesitancy: Correlates and Interventions
Collection Editors: Manoj Sharma, Kavita Batra












