Haeberle and Zengerle [
23] characterize microfluidic platforms (LOC devices) into capillary-driven systems (RDTs), “microfluidic large-scale integration” systems, electrokinetic platforms, centrifugal microfluidics, and “free scalable non-contact dispensing” devices. The main functions integrated on these platforms are: pumping and valving, mixing, separation, reagent storage and sample preparation [
24]. A 2013 market review of LOC applications showed blood glucose analysis, electrolytes analysis, HIV diagnostics and determination of cardiac markers as some of the main applications of LOC systems by leading companies such as Abbott, Alere, Arkray, Bayer, LifeScan, Menarini Diagnostics, Roche and Siemens [
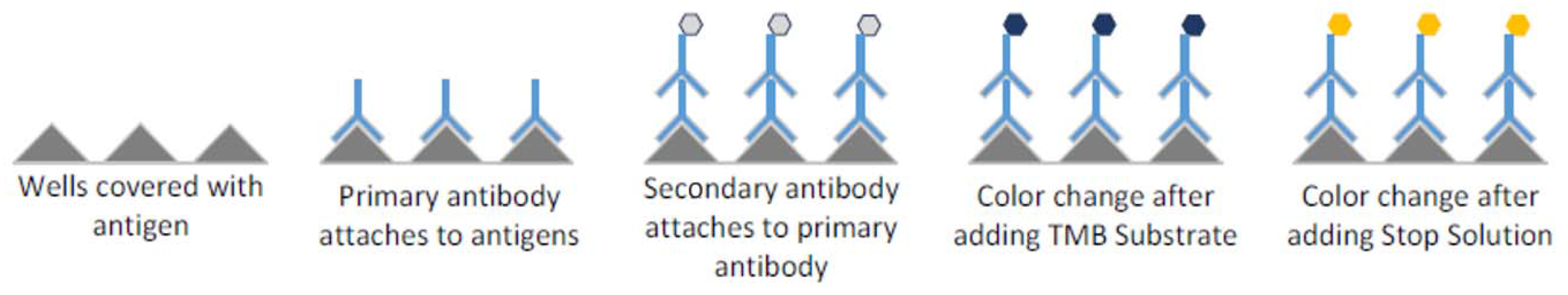
24]. Diagnostic tests that run on microfluidic devices range from immunoassays (based on immune responses to an antigen of a particular pathogen) to molecular diagnostics (detecting and oftentimes amplifying deoxyribose nucleic acid (DNA) or ribose nucleic acid (RNA)) [
25]. While both diagnostics have been implemented on microfluidic devices, implementation of molecular diagnostics is generally more challenging due to more complex assay steps. For example, the use of polymerase chain reaction (PCR) for amplification of nucleic acids requires elaborate sample preparation and complex thermal cycling [
25]. The following section will review some microfluidic devices for POC.
2.1. LOC Devices for POC Based on Molecular Detection and Immunoassays
Liao et al. [
26] implemented POC testing for HSV-2 virus on a portable molecular diagnostic device. The so-called “smart cup” combines capillary fluidics and isothermal amplification to carry out a quantitative fluorescent LAMP assay. The design uses the smartphone flashlight to excite the fluorescent dye and the smartphone camera for quantitative readout. Although the heating technique and the readout are very economic (Mg–Fe pouches are only
$0.15), the design uses a custom-made microfluidic chip consisting of Qiagen silica membrane as entry port, and solvent-bonded, milled polymethyl methacrylate (PMMA) layers containing the microfluidic structures as described in Liu et al. [
26,
27].
In another publication by the same group [
28], two custom-made, layered microfluidic chips were used for plasma separation and detection of nucleic acids via reverse-transcriptase LAMP. The plasma separation chip consisted of machined PMMA, plasma-separation membranes, and double-sided and single-sided adhesives. Another microfluidic chip was used for nucleic acid extraction and amplification [
26,
27,
28]. The sample-to-answer testing would include loading the sample into the first chip, transfer of the plasma to the second chip as well as manual placing of the second chip onto a heating platform [
28]. Besides a number of manual steps in running this assay, the fabrication sequence to produce these platforms is rather involved.
Microfluidic chips produced via injection molding can present a faster fabrication route and could also be a relatively affordable option for production of large numbers of fluidic chips. This fabrication option for enzyme-linked immunosorbent assay (ELISA) LOCs is discussed by Chin et al. [
29]. Injection-molded LOCs were used to run hundreds of samples in Rwanda to detect HIV and syphilis simultaneously from 1 μL of whole blood. While injection molding typically is used to produce features above 100 μm in size, tight control of process parameters allowed for reduction of feature sizes to 1 μm [
29]. The materials used to form the microfluidic chips are polystyrene and cyclic olefin copolymer. Cost and time per chip of
$0.10 and 40 s, respectively [
29], render chip fabrication via injection molding a low-cost and high-throughput manufacturing technique. While highly desirable if large quantities of identical parts are produced, injection molding is not an appropriate fabrication approach for prototyping or production of a limited number of parts, due to high cost of molds.
2.2. 3D Printing for LOC Devices
Most LOC devices are based on microfabrication methods using materials such as glass, plastic or polydimethylsiloxane (PDMS) [
30]. While these fabrication methods require access to highly specialized and expensive microfabrication tools, as well as fabrication of a master for replica molding [
31,
32], recent developments in 3D printing, such as emergence of a wider range of materials and inexpensive printers, open new possibilities for rapid fabrication of affordable highly customizable LOC platforms [
31,
33,
34,
35].
For example, a POC device that implements LAMP for genomic detection of
Escherichia Coli and
Staphylococcus Aureus was fabricated with 3D-printing technology by Stedtfeld et al. [
36]. The overall structure of the device was manufactured using stereolithography (3D printing based on curing liquid photosensitive resin by UV light [
32]), while a channel network on the microfluidic chip was obtained using rubber-assisted hot embossing of polyester film with a 3D-printed mold. The polyester film was then assembled with a hydrophobic membrane and closed off with patterned adhesive [
36]. The developed device is operated through an iPod Touch, which is also utilized for data analysis and Wi-Fi connectivity. A sample is loaded manually using a pipettor, while hydrophobic membranes and manual taping of vents after fill maintain fluid in the channels and free of contamination. [
36].
Material jetting is another 3D-printing technology, and was used by Erkal et al. [
37] to create a microfluidic device which holds electrodes for electrochemical detection of dopamine and nitric oxide. Another 3D-printed fluidic device demonstrated by the same group was used to measure the presence of adenosine triphosphate (ATP) while observing oxygen stimulus concentration in the sample [
37]. Both devices were fabricated via an Objet Connex 350 multi-material printer.
Stereolithography and material jetting are well suited for designs requiring leakage-free bonding between adjacent layers, but these technologies are significantly more expensive than alternative 3D technologies such as fused deposition modeling (FDM) [
31]. Prices for low-end FDM printers recently dropped from
$14,000 to
$300 due to expiration of patents, and are expected to decrease further as a large community of hobbyists has evolved around 3D printing, making hardware open source and sharing designs and ideas online [
38].
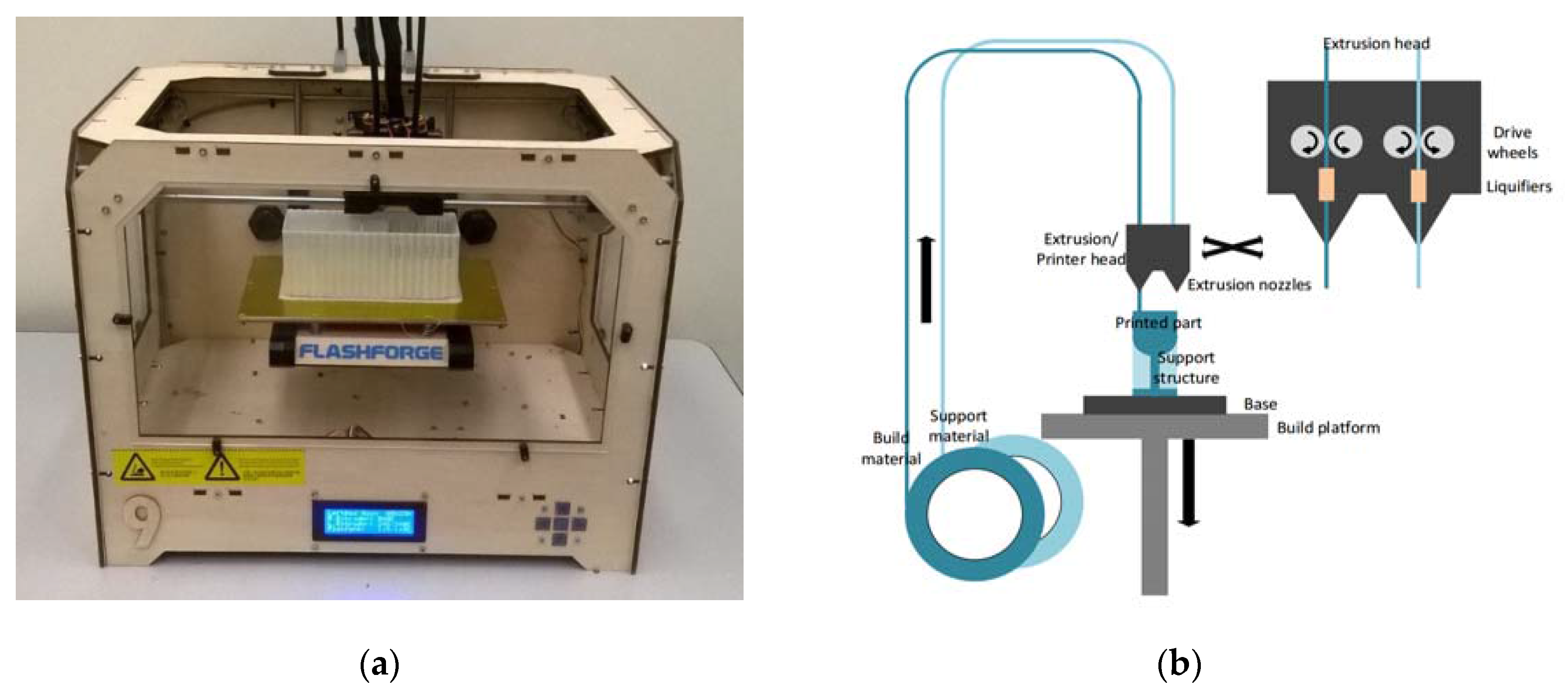
The principle of FDM is based on layered deposition of liquefied material, and is illustrated in
Figure 1. Thermoplastic filaments are stored on spools and extruded through heated nozzles, where the plastic is liquified upon reaching the glass transition temperature. The molten material is then deposited onto the base, where it cools down and solidifies. To deposit a new layer atop of solidified material, the build platform holding the base is lowered. The height of one layer is defined by the lowering distance of the build platform between successive layers, and is as low as 100 µm [
39,
40,
41].
To save material and time, parts are typically not printed solid but filled with a hexagonal honeycomb structure (this so-called infill differs in the various systems and can be of different geometric pattern, such as the square pattern utilized in Airwolf systems). The surface of printed parts consists of the denser shell of material. These shells are made up of about one to four layers (the number can be chosen by the user) of extruded material that give the part its shape and seal the hollow infill.
Waheed et al. [
33] recently analyzed advantages and disadvantages of different FDM systems utilized for the fabrication of microfluidic devices, and found that these systems are simple to use and are able to fabricate affordable microfluidic systems. However, FDM-printed parts present a staircase effect deriving from the layered fabrication method. The extent of this effect is impacted by the layer height and negatively affects the surface texture, as well as limits the resolution of printed parts. The average deviation for features printed in the X and Y directions was reported to be 60.8 and 71.5 µm, respectively [
33].
Among the nine FDM systems analyzed in Waheed et al. [
33] was also the MakerBot Replicator 2X (MakerBot Industries, LLC, New York, NY, USA), which was recently demonstrated by Kadimisetty et al. [
42] to be capable of manufacturing a low-cost ELISA platform for the electrochemiluminescent detection of cancer proteins. The channel height of this fluidic chip was 200 µm, which corresponds to the layer height of the MakerBot Replicator 2X [
42]. To actuate liquids, Kadimisetty et al. [
42] rely on gravity by manually tilting the device.
Another device that uses 3D printing for device manufacturing, as well as a smartphone for readout, is described by Berg et al. [
43]. The smartphone is not only used to read out the colorimetric ELISA (supported by a lens in the printed device) from a 96-well plate, but also allows for a custom mobile application with an interactive user interface. To allow for improved data processing, a server was used in conjunction with the device and a smartphone. Smartphones are increasingly used in POC devices [
9,
26,
36,
43] to replace bulky and expensive optical instruments, benefitting from portable dimensions, built-in light source and integration of multiple functions such as imaging, image processing and providing a user interface via touchscreen, as well as Bluetooth and Wi-Fi connectivity. Wireless connectivity is especially important for POC applications as it enables one to remotely analyze data, and provides real-time feedback from specialists in central hospitals to patients in remote areas [
36].
While all microfluidic devices use some type of force propelling liquid through channels, Iwai et al. implemented a human-powered pumping system, allowing for resource-free (no electricity or external components) actuation of fluids through channels. In this design, a human finger pushes down onto an air-filled pressure chamber exerting increased pressure onto fluids in connected microfluidic channels. As the finger releases the dome on the pressure chamber, membrane-type fluidic diodes close, preventing backflow. Cantilever-based diodes are integrated to allow for multiple refills of the channels from fluid inlets. An injection-molding process was developed for low-cost mass production, however, it required increasing channel dimensions from 100 to 300 µm, and introducing the need for oxygen plasma and thermal treatment for bonding of layers [
44]. While the finger-powered microfluidic device does not need external power sources, it is difficult to automate when a sequence of fluidic steps is required.
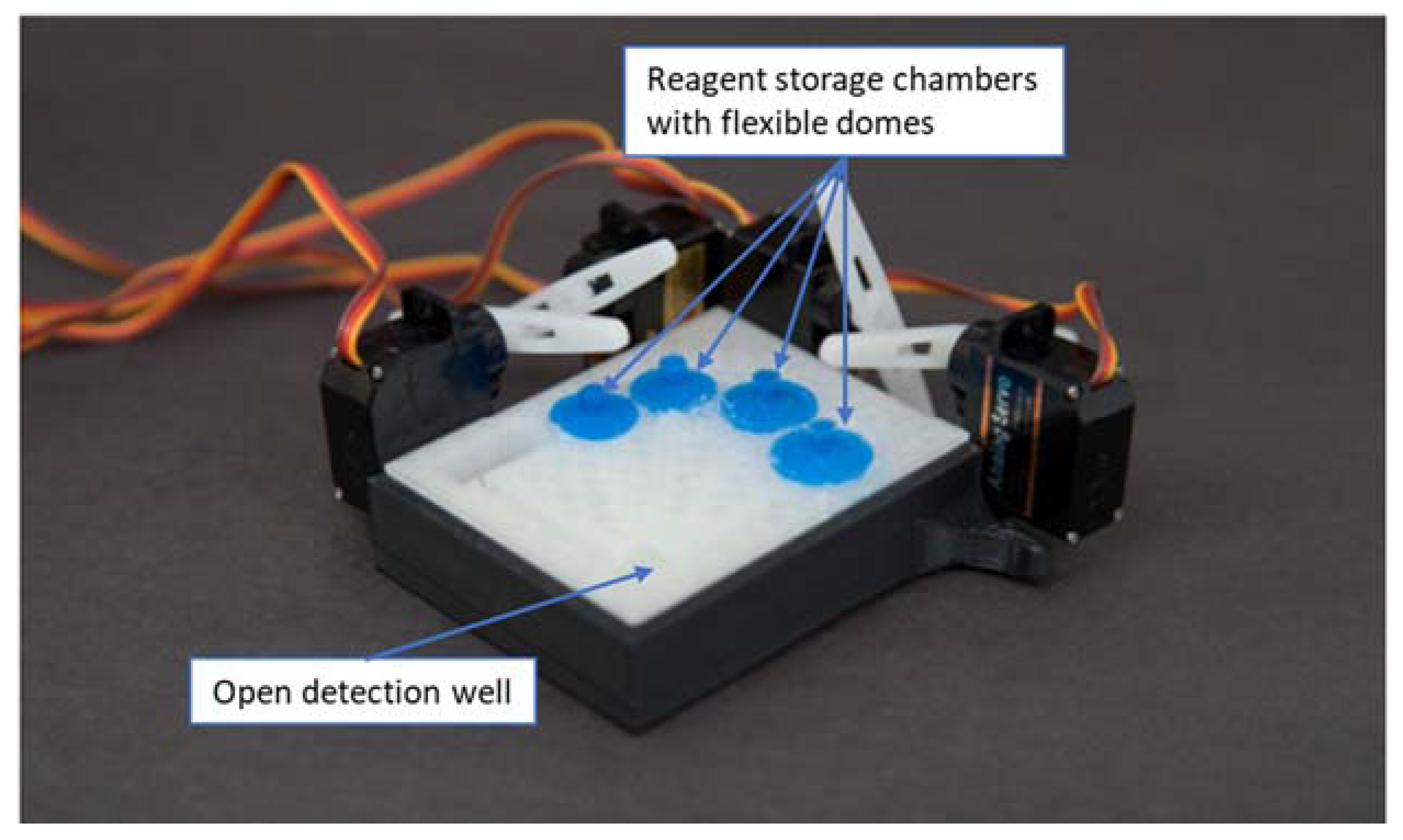
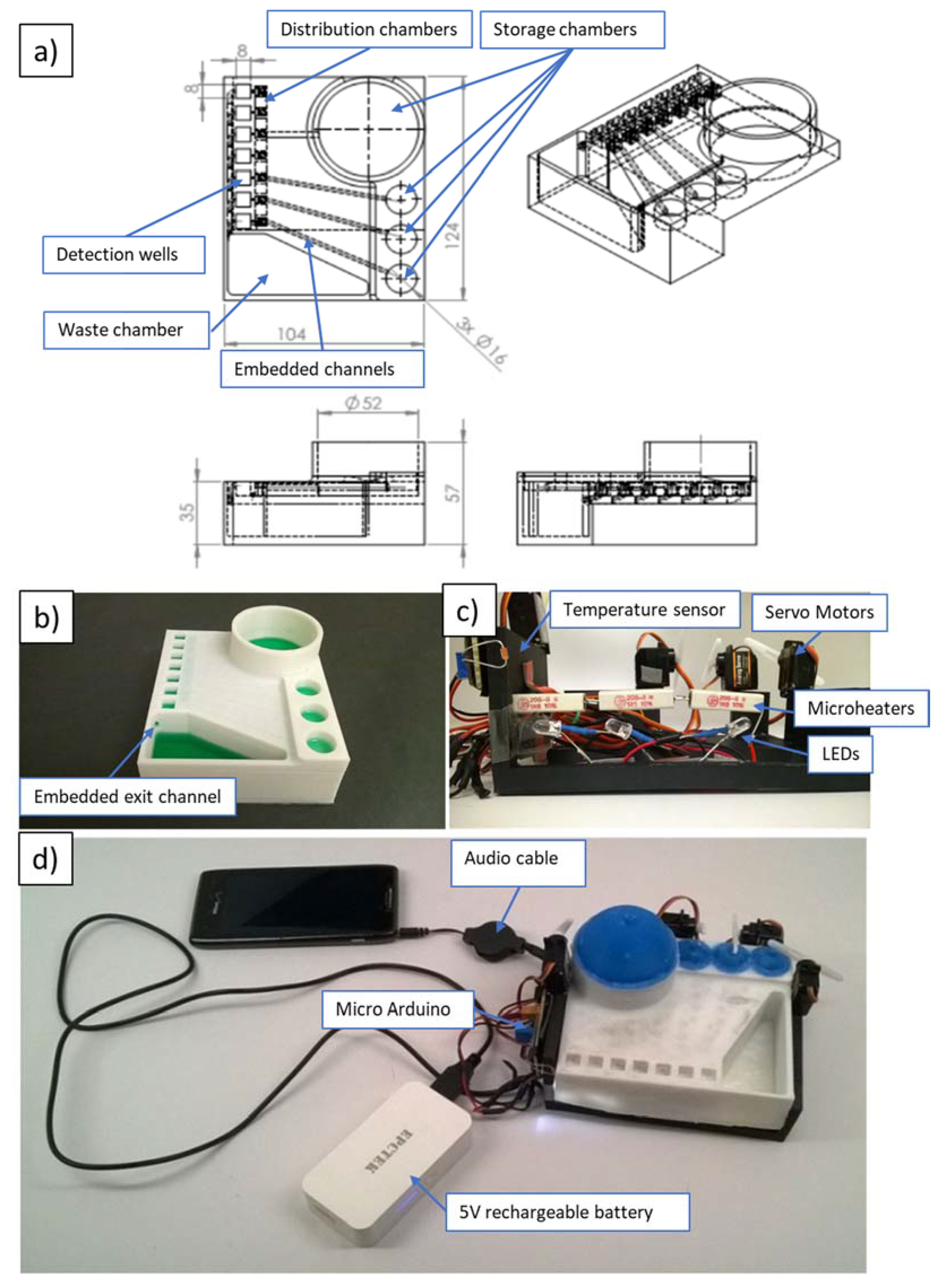
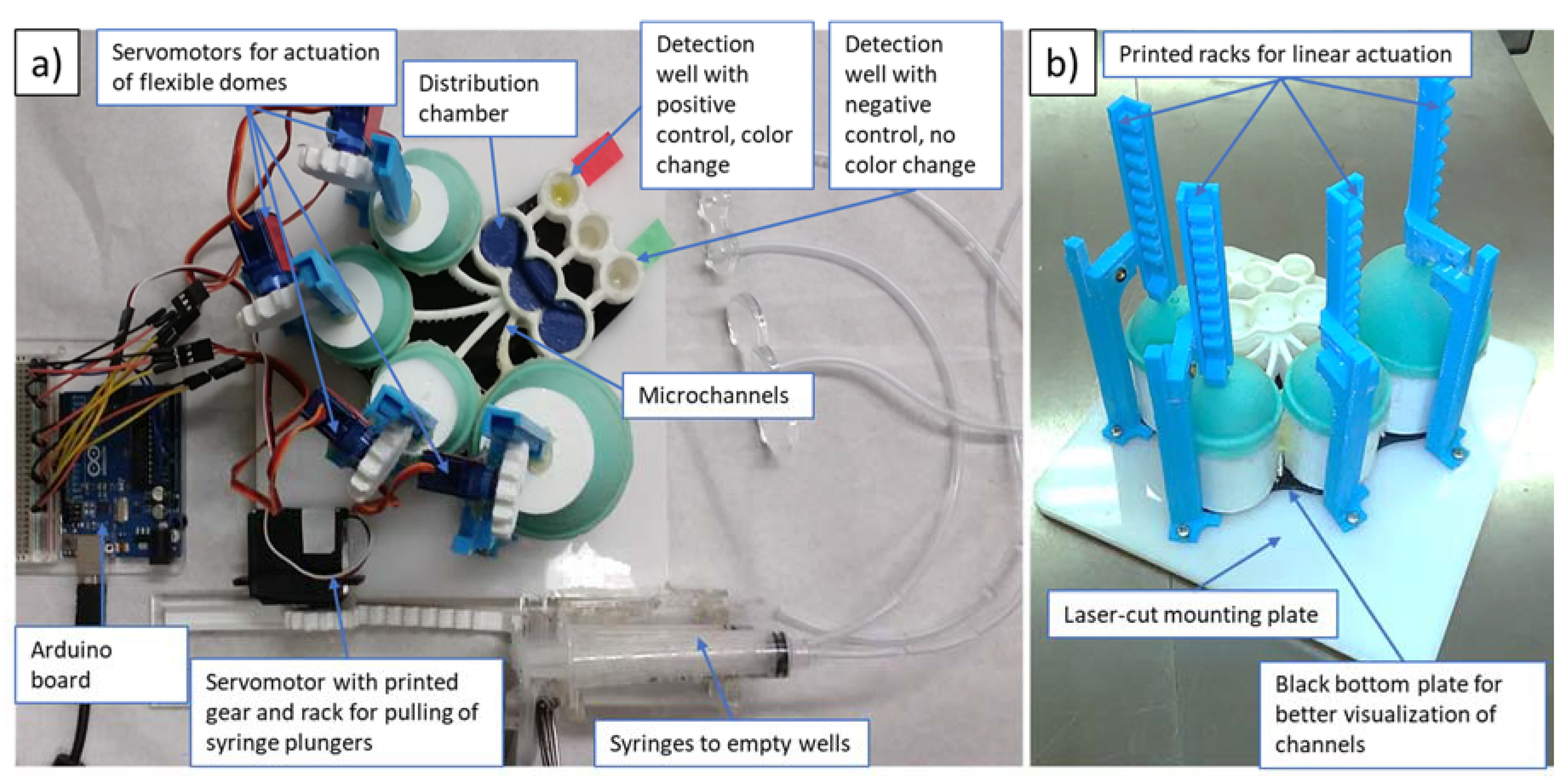
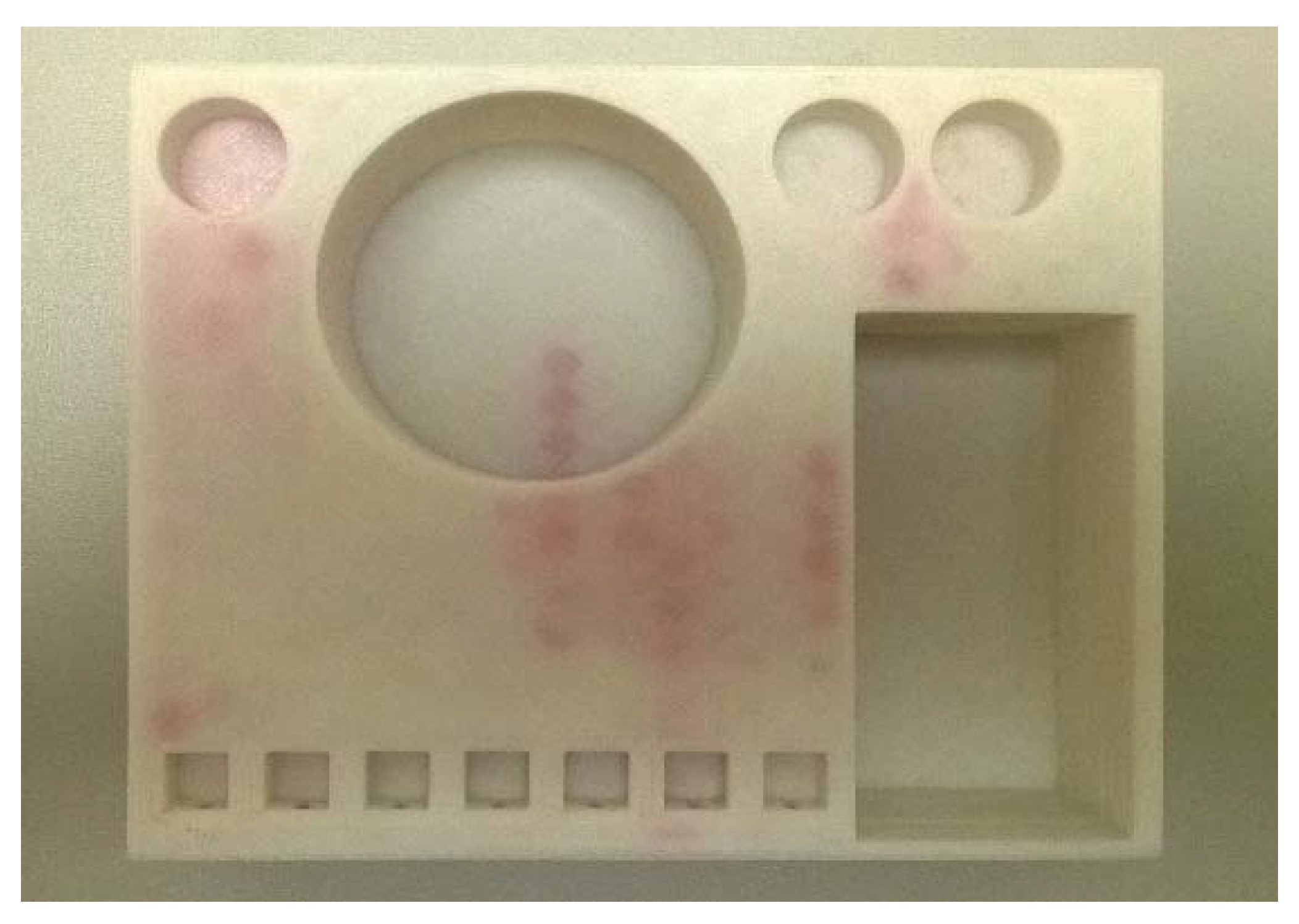
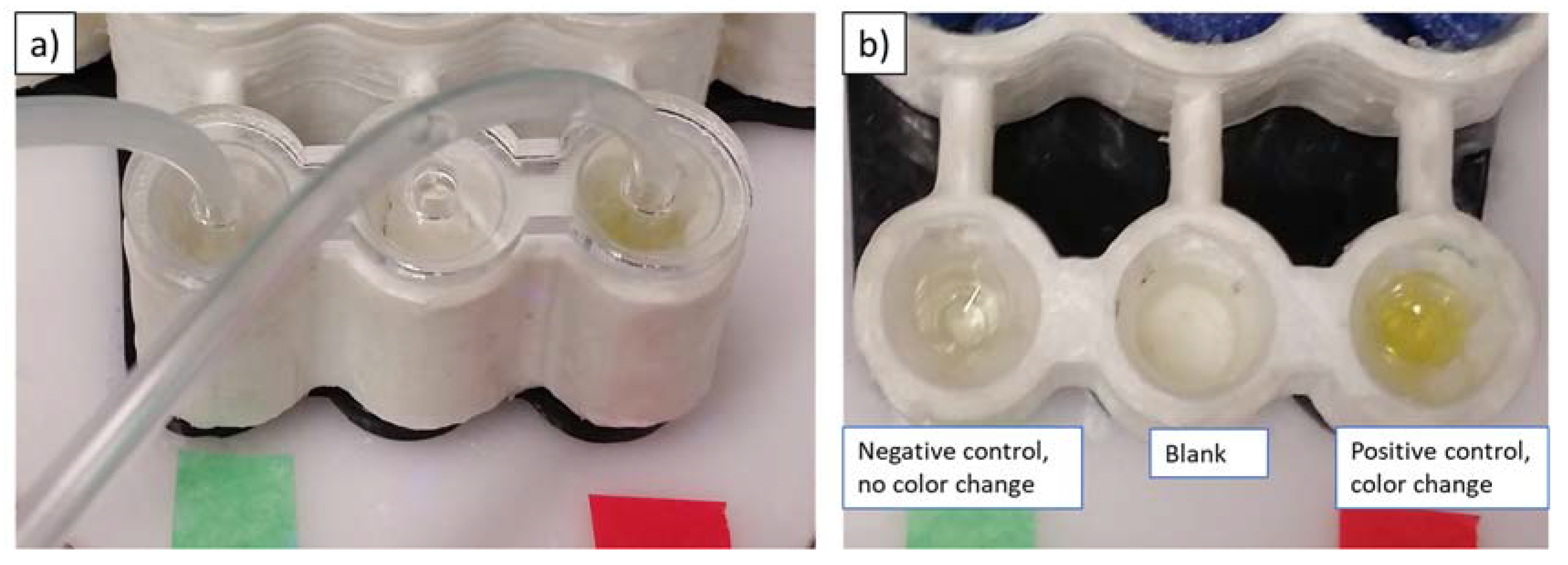
The device suggested by the authors of this work employs 3D-printed (FDM) microfluidics and actuation of reagents via servomotors, mounted onto a reusable case. For production of these devices, printers could be placed in remote hospitals of developing countries to allow on-demand manufacturing of the devices. Implementing electronics onto a reusable case not only allows one to reduce costs, but also affords higher adaptability of the reusable part to different types of immunoassays. Together with control of electronics and processing readout via a smartphone, the design enables the automation of complicated ELISA procedures with multiple steps, including multiple usages of fluid from the same reservoir, flow reciprocation, repeated emptying of the wells, and various incubation steps. Online distribution of print files as well as of control sequences (Arduino C-files or audio files as presented below), and increasingly ready access to 3D printing and disposable syringes and servomotors, allows for worldwide dissemination and access to an automated bioassay technology that does not need laboratory settings or trained personnel to function.