Protection and Reinforcement of Tooth Structures by Dental Coating Materials
Abstract
:1. Introduction
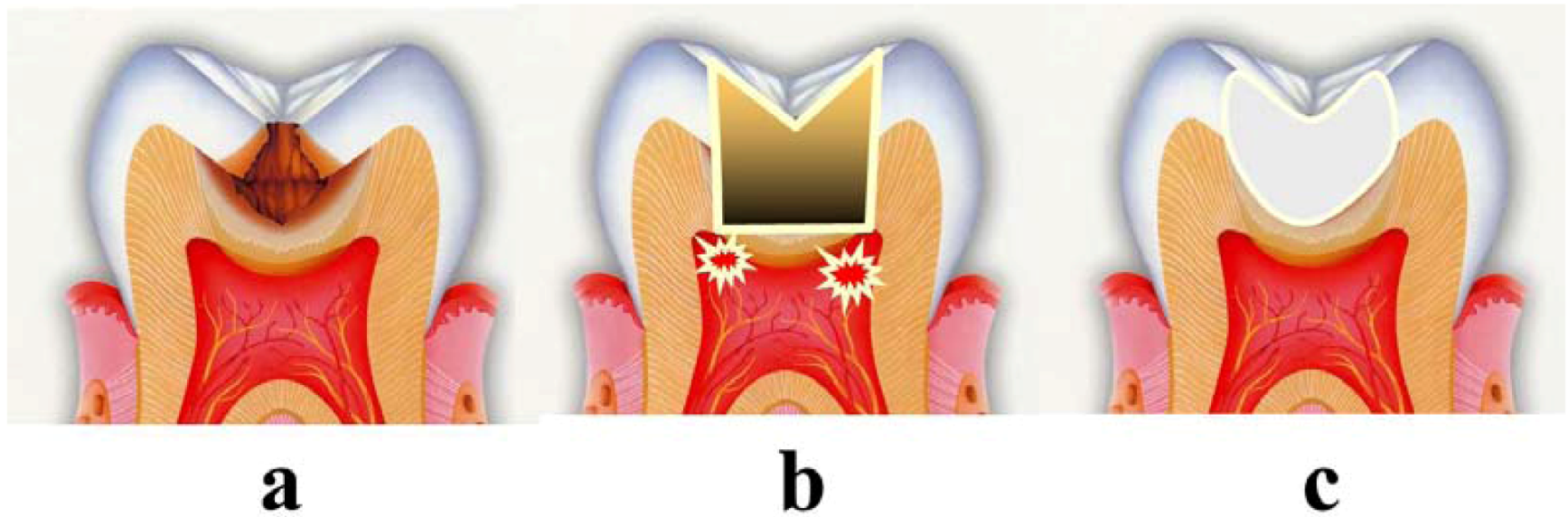
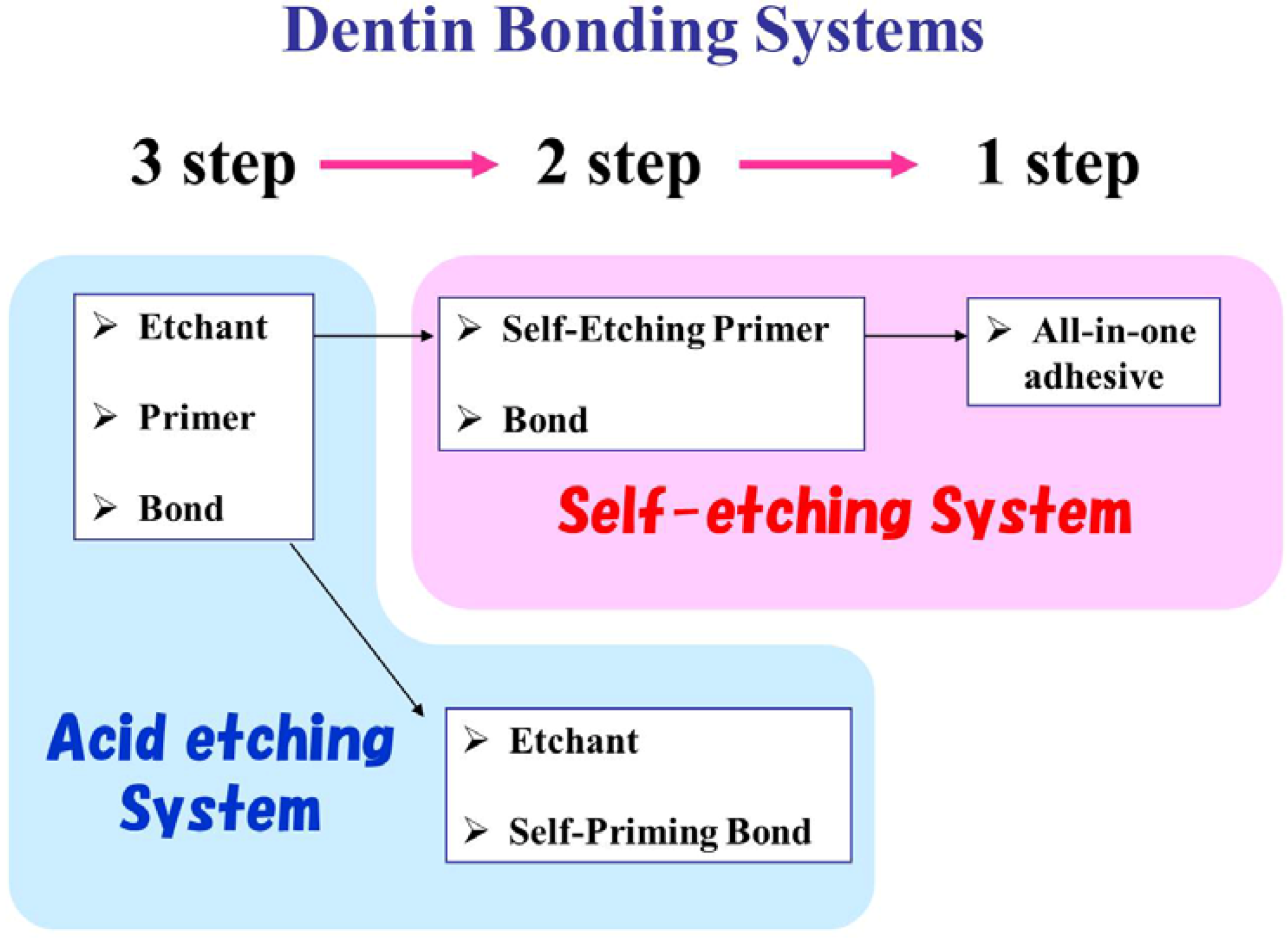
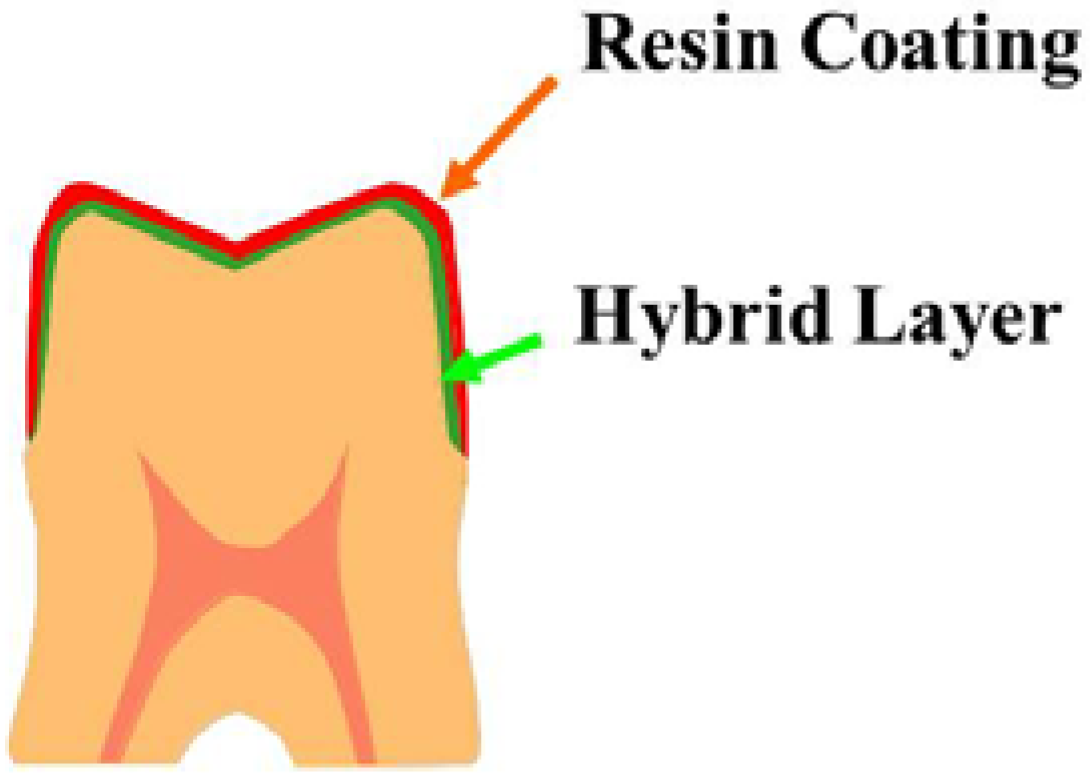
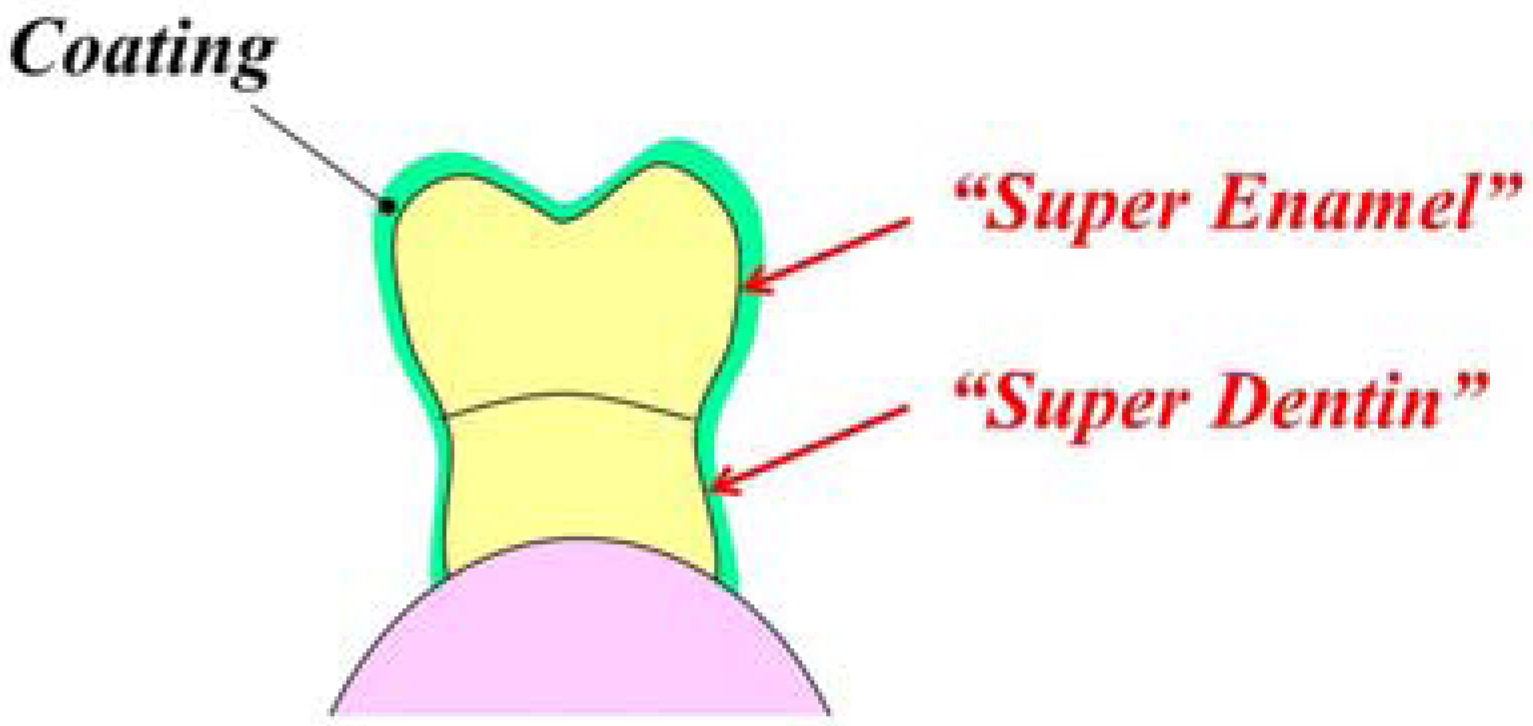
2. Advances in Adhesive Materials


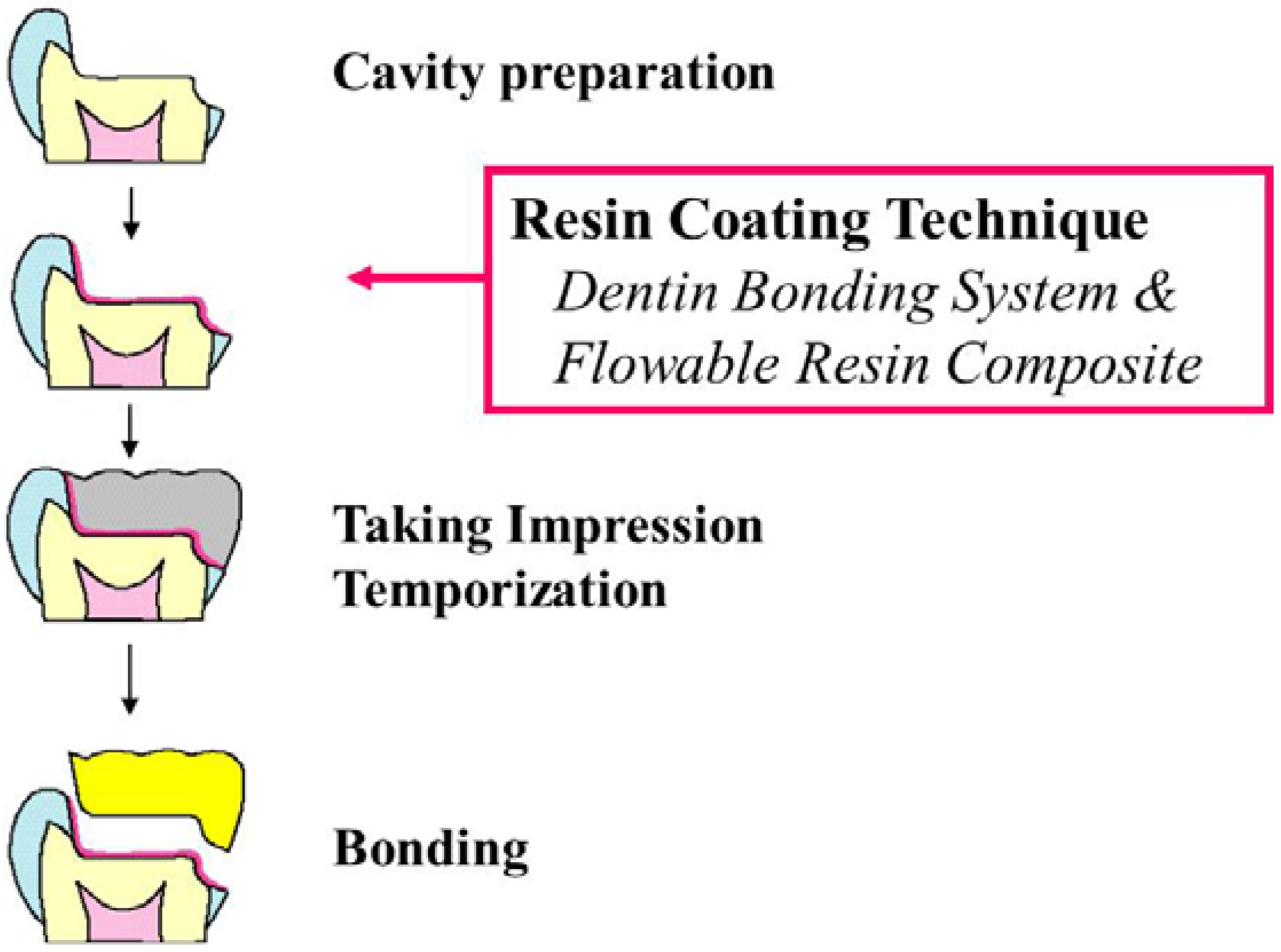
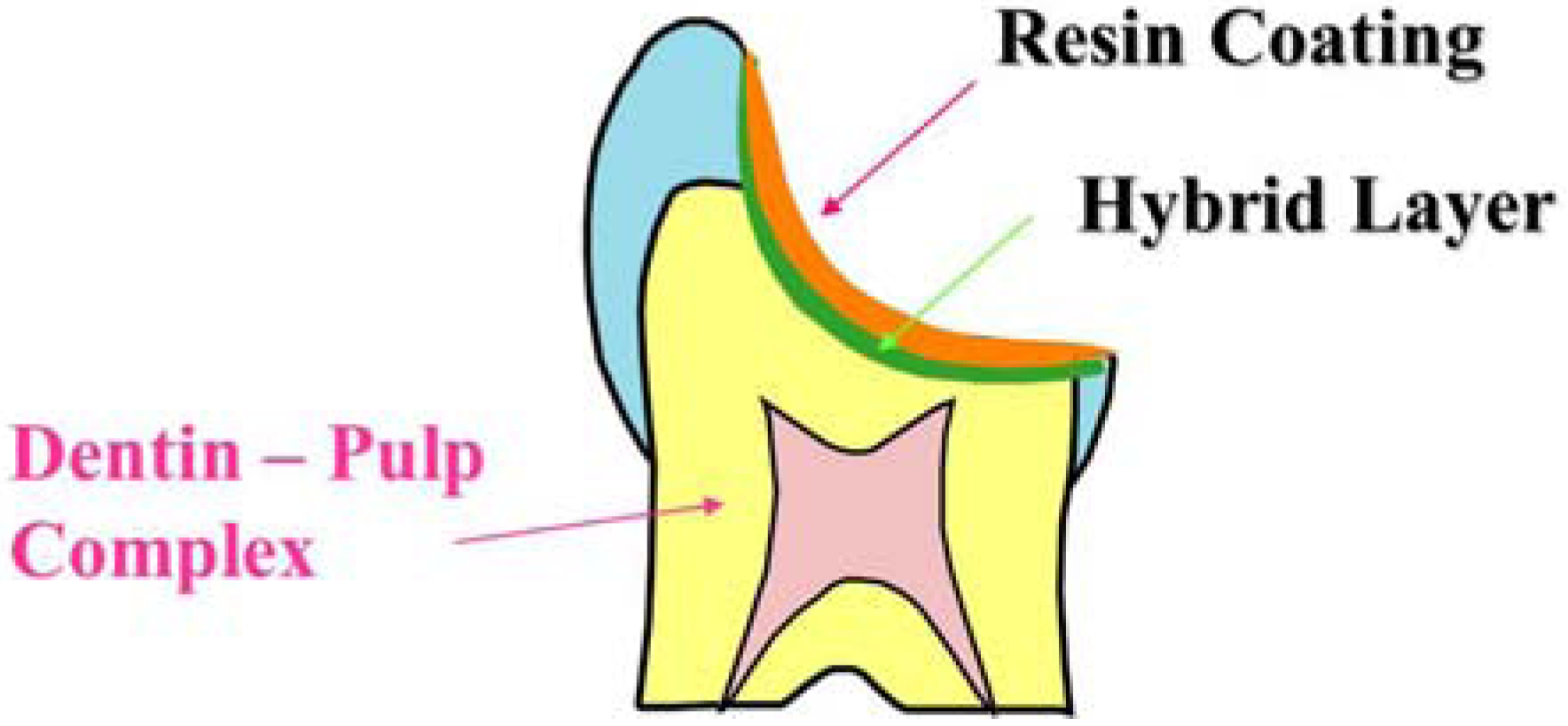
3. Resin Coating Technique in Indirect Restoration
4. Development of Thin Film Coating Materials
5. Dental Coating Materials in the Future

Acknowledgements
References
- Tyas, M.J.; Anusavice, K.J.; Frencken, J.E.; Mount, G.J. Minimal intervention dentistry—A review, FDI Commission Project 1–97. Int. Dent. J. 2000, 50, 1–12. [Google Scholar] [CrossRef]
- Momoi, Y.; Fujitani, M.; Fukushima, M.; Hayashi, M.; Imazato, S.; Kubo, S.; Nikaido, T.; Shimizu, A.; Unemori, M.; Yamaki, M. Clinical guidelines for treating caries in adults following a minimal intervention policy, evidence and consensus based report. J. Dent. 2012, 40, 95–105. [Google Scholar] [CrossRef]
- Nakabayashi, N.; Nakamura, M.; Yasuda, N. Hybrid layer as a dentin bonding mechanism. J. Aesthet. Dent. 1991, 3, 133–138. [Google Scholar] [CrossRef]
- Fontana, M.; Gonzalez–Cabezas, C. Secondary caries and restoration replacement: An unresolved problem. Compend. Contin. Educ. Dent. 2000, 21, 15–26. [Google Scholar]
- Tsuchiya, S.; Nikaido, T.; Sonoda, H.; Foxton, R.M.; Tagami, J. Ultrastructure of the dentin-adhesive interface after acid-base challenge. J. Adhes. Dent. 2004, 6, 183–190. [Google Scholar]
- Waidyasekera, K.; Nikaido, T.; Weerasinghe, D.S.; Ichinose, S.; Tagami, J. Reinforcement of dentin in self-etch adhesive technology: A new concept. J. Dent. 2009, 37, 604–609. [Google Scholar] [CrossRef]
- Nurrohman, H.; Nikaido, T.; Takagaki, T.; Sadr, A.; Ichinose, S.; Tagami, J. Hydroxyapatite crystal protection against acid-attack beneath resin-dentin interface with four adhesives. TEM and crystallography evidence. Dent. Mater. 2012, 28, e89–e98. [Google Scholar] [CrossRef]
- Nikaido, T.; Weerasinghe, D.D.; Waidyasekera, K.; Inoue, G.; Foxton, R.M.; Tagami, J. Assessment of the nanostructure of acid-base resistant zone by the application of all-in-one adhesive systems: Super dentin formation. Biomed. Mater. Eng. 2009, 19, 163–171. [Google Scholar]
- Li, N.; Nikaido, T.; Takagaki, T.; Sadr, A.; Makishi, P.; Chen, J.; Tagami, J. The role of functional monomers in bonding to enamel: Acid-base resistant zone and bonding performance. J. Dent. 2010, 38, 722–730. [Google Scholar] [CrossRef]
- Yoshida, Y.; Nagakane, K.; Fukuda, R.; Okazaki, M.; Shintani, H.; Inoue, S.; Tagawa, Y.; Suzuki, K.; De Munck, J.; Van Meerbeek, B. Comparative study on adhesive performance of functional monomers. J. Dent. Res. 2004, 83, 454–458. [Google Scholar] [CrossRef]
- Nikaido, T.; Yoda, A.; Foxton, R.M.; Tagami, J. A resin coating technique to achieve minimal intervention in indirect resin composites: A case report. Int. Chin. J. Dent. 2003, 3, 62–68. [Google Scholar]
- Islam, M.R.; Takada, T.; Weerasinghe, D.S.; Uzzaman, M.A.; Foxton, R.M.; Nikaido, T.; Tagami, T. Effect of resin coating on adhesion of composite crown restoration. Dent. Mater. J. 2006, 25, 272–279. [Google Scholar] [CrossRef]
- Pashley, E.L.; Comer, R.W.; Simpson, M.D.; Horner, J.A.; Pashley, D.H.; Caughman, W.F. Dentin permeability: Sealing the dentin in crown preparations. Oper. Dent. 1992, 17, 13–20. [Google Scholar]
- Kitasako, Y.; Murray, P.E.; Tagami, J.; Smith, A.J. Histomorphometric analysis of dentinal bridge formation and pulpal inflammation. Quintessence. Int. 2002, 33, 600–608. [Google Scholar]
- Inokoshi, S. Temporary sealing-pulp and dentin protection using low viscosity composite (in Japanese). Adhes. Dent. 1992, 10, 250. [Google Scholar]
- Sato, M.; Goto, H.; Inai, N.; Nikaido, T.; Tagami, J.; Inokoshi, S.; Yamada, T.; Takatsu, T. How to use “Liner Bond System” as a dentin and pulp protector in indirect restorations (in Japanese). Adhes. Dent. 1994, 12, 41–48. [Google Scholar]
- Otsuki, M.; Yamada, T.; Inokoshi, S.; Takatsu, T.; Hosoda, H. Establishment of a composite resin inlay technique part 7. Use of low viscous resin (in Japanese). Jpn. J. Conserv. Dent. 1993, 36, 1324–1330. [Google Scholar]
- Jayasooriya, P.R.; Pereira, P.N.R.; Nikaido, T.; Tagami, J. Effect of a “Resin-coating” on the interfacial adaptation of composite inlays. Oper. Dent. 2003, 28, 28–35. [Google Scholar]
- Kosaka, S.; Kajihara, H.; Kurashige, H.; Tanaka, T. Effect of resin coating as a means of preventing marginal leakage beneath full cast crowns. Dent. Mater. J. 2005, 24, 117–122. [Google Scholar] [CrossRef]
- Nikaido, T.; Cho, E.; Nakajima, M.; Tashiro, H.; Toba, S.; Burrow, M.F.; Tagami, J. Tensile bond strengths of resin cements to bovine dentin using resin coating. Am. J. Dent. 2003, 16, 41–46. [Google Scholar]
- Kitasako, Y.; Burrow, M.F.; Nikaido, T.; Tagami, J. Effect of resin coating technique on dentin bond strengths over 3 years. J. Esthet. Restor. Dent. 2002, 14, 115–122. [Google Scholar] [CrossRef]
- Nikaido, T.; Kitasako, Y.; Burrow, M.F.; Umino, A.; Maruoka, R.; Ikeda, M.; Tagami, J. Effect of resin coating on dentin bond durability of a resin cement over 1 year. Am. J. Dent. 2008, 21, 64–68. [Google Scholar]
- Paul, S.J.; Schärer, P. The dual bonding technique: A modified method to improve adhesive luting procedures. Int. J. Periodontics Restor. Dent. 1997, 17, 536–545. [Google Scholar]
- Bertschinger, C.; Paul, S.J.; Lüthy, H.; Schärer, P. Dual application of dentin bonding agents: Effect on bond strength. Am. J. Dent. 1996, 9, 115–119. [Google Scholar]
- Magne, P. Immediate dentin sealing: A fundamental procedure for indirect bonded restorations. J. Esthet. Restor. Dent. 2005, 17, 144–154. [Google Scholar] [CrossRef]
- Magne, P.; Kim, T.H.; Cascione, D.; Donovan, T.E. Immediate dentin sealing improves the bond strength of indirect restorations. J. Prosthet. Dent. 2005, 94, 511–519. [Google Scholar] [CrossRef]
- Magne, P.; Nielsen, B. Interaction between impression materials and immediate dentin sealing. J. Prosthet. Dent. 2009, 102, 298–305. [Google Scholar] [CrossRef]
- Nikaido, T.; Nakaoki, Y.; Ogata, M.; Foxton, R.M.; Tagami, J. The resin-coating technique. Effect of a single-step bonding system on dentin bond strengths. J. Adhes. Dent. 2003, 5, 293–300. [Google Scholar]
- Takahashi, R.; Nikaido, T.; Ariyoshi, M.; Kitayama, S.; Sadr, A.; Foxton, R.M.; Tagami, J. Thin resin coating by dual-application of all-in-one adhesives improves dentin bond strength of resin cements for indirect restorations. Dent. Mater. J. 2010, 29, 615–622. [Google Scholar] [CrossRef]
- Horowitz, H.S.; Heifetz, S.B.; Poulsen, S. Retention and effectiveness of a single application of an adhesive sealant in preventing occlusal caries: Final report after five years of a study in Kalispell, Montana. J. Am. Dent. Assoc. 1977, 95, 1133–2119. [Google Scholar]
- Paris, S.; Meyer-Luekel, H.; Mueller, J.; Hummel, M.; Keilbassa, A.M. Progression of sealed initial vovine enamel lesions under demineralizing conditions in vitro. Caries Res. 2006, 40, 124–129. [Google Scholar] [CrossRef]
- Phark, J.H.; Durate, S.J.; Meyer-Lueckel, H.; Paris, S. Caries infiltration with resins: A novel treatment option for interproximal caries. Compend. Contin. Educ. Dent. 2009, 30, 13–17. [Google Scholar]
- Schmidlin, P.R.; Sener, B.; Attin, T.; Wiefand, A. Protection of sound enamel and artificial enamel lesions against demineralization: Caries infiltrant versus adhesive. J Dent. 2012, 40, 851–856. [Google Scholar] [CrossRef]
- Heijnsbroek, M.; Paraskevas, S.; van der Weijden, G.A. Fluoride interventions for root caries: A review. Oral. Health. Prev. Dent. 2007, 5, 145–152. [Google Scholar]
- Kaneshiro, A.V.; Imazato, S.; Ebisu, S.; Tanaka, S.; Tanaka, Y.; Sano, H. Effects of a self-etching resin coating system to prevent demineralization of root surfaces. Dent. Mater. 2008, 24, 1420–1427. [Google Scholar] [CrossRef]
- Daneshmehr, L.; Matin, K.; Nikaido, T.; Tagami, J. Effects of root dentin surface coating with all-in-one adhesive materials on biofilm adherence. J. Dent. 2008, 36, 33–41. [Google Scholar] [CrossRef]
- Tajima, K.; Nikaido, T.; Inoue, G.; Ikeda, M.; Tagami, J. Effects of coating root dentin surfaces with adhesive materials. Dent. Mater. J. 2009, 28, 578–586. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Nikaido, T.; Takahashi, R.; Ariyoshi, M.; Sadr, A.; Tagami, J. Protection and Reinforcement of Tooth Structures by Dental Coating Materials. Coatings 2012, 2, 210-220. https://doi.org/10.3390/coatings2040210
Nikaido T, Takahashi R, Ariyoshi M, Sadr A, Tagami J. Protection and Reinforcement of Tooth Structures by Dental Coating Materials. Coatings. 2012; 2(4):210-220. https://doi.org/10.3390/coatings2040210
Chicago/Turabian StyleNikaido, Toru, Rena Takahashi, Meu Ariyoshi, Alireza Sadr, and Junji Tagami. 2012. "Protection and Reinforcement of Tooth Structures by Dental Coating Materials" Coatings 2, no. 4: 210-220. https://doi.org/10.3390/coatings2040210
APA StyleNikaido, T., Takahashi, R., Ariyoshi, M., Sadr, A., & Tagami, J. (2012). Protection and Reinforcement of Tooth Structures by Dental Coating Materials. Coatings, 2(4), 210-220. https://doi.org/10.3390/coatings2040210




