7.1. OXA-1
The OXA-1 enzyme is also the OXA-30 enzyme, as a result of error in the original OXA-1 sequence [
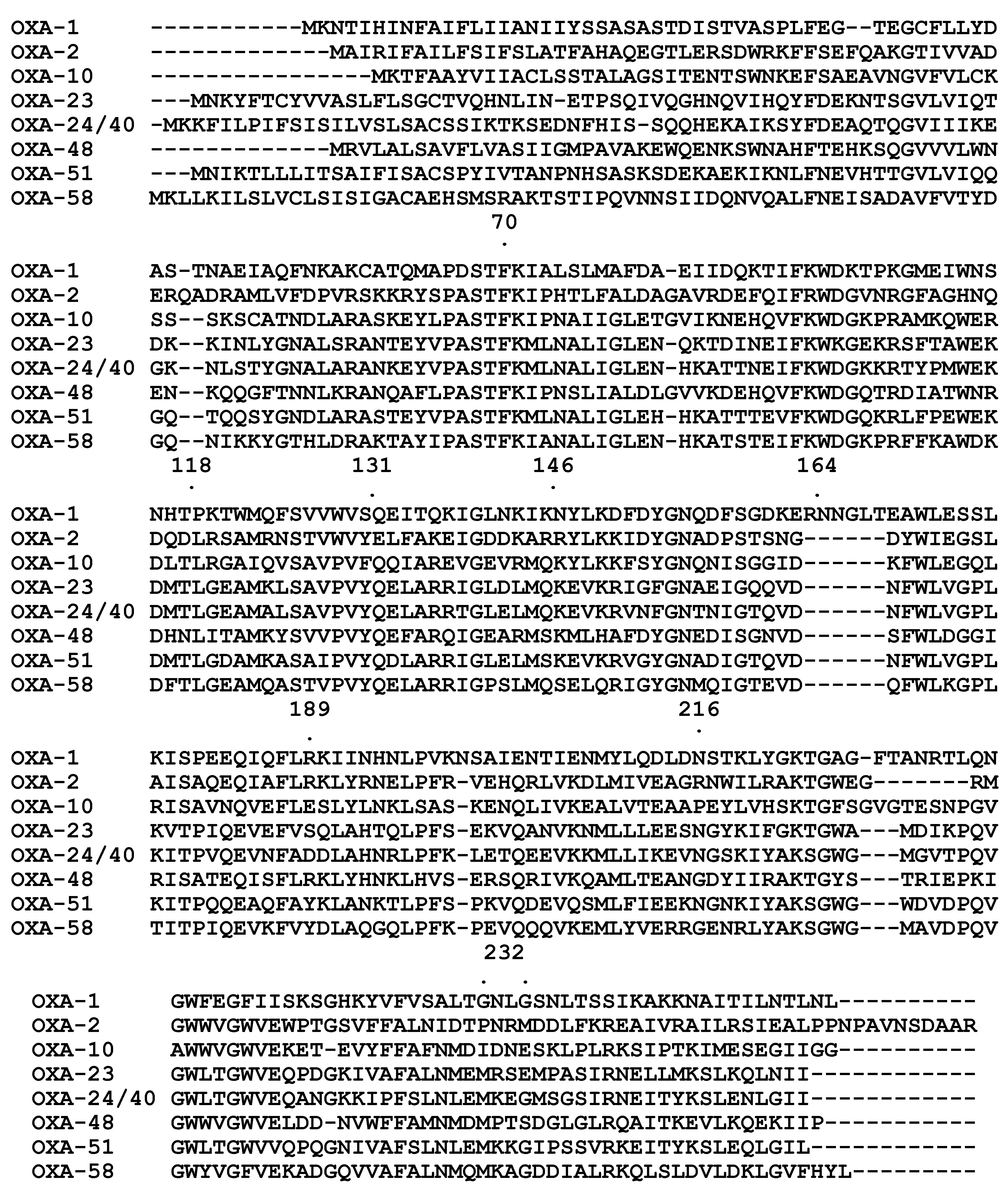
47]. OXA-1 shares less than 30% of homology with other plasmid and chromosomal Class D β-lactamases.
Distribution and hosts. OXA-1-like enzymes are found in several bacterial species such as
P. aeruginosa,
K. pneumoniae and other
Enterobacteriaceae, and in both human and animal isolates [
11,
30,
43]. OXA-1-like enzymes have been described in Europe, Asia and Africa [
30,
43,
48,
49,
50].
Antibiotic susceptibility profile and substrate profile. The wild-type OXA-1 enzyme is a narrow spectrum β-lactamase that confers resistance to penicillins and decreases the susceptibility to cephalothin, cefotaxime and cefepime. The MICs of carbapenem antibiotics and ceftazidime remain unchanged. It is not sensitive to tazobactam. Kinetics made with partially purified enzyme demonstrated that OXA-1 effectively hydrolyzes penicillins and cephalosporins [
30].
Table 5.
MICs for penicillins in the presence and absence of inhibitors against diverse enzymes.
Table 5.
MICs for penicillins in the presence and absence of inhibitors against diverse enzymes.
| Antimicrobial | OXA-1 | OXA-2 | OXA-10 | OXA-18 | OXA-20 | OXA-23 | OXA-24 | OXA-48 | OXA-58 | OXA-69 | OXA-134 |
|---|
| Amoxicillin | >512 | >512 | - | 32 | 512 | >1024 | >512 | >512 | >512 | - | >512 |
| Amoxicillin + clavulanic acid a | 128 | 64 | - | 4 | 32 | >1024 | >512 | >512 | 128 | - | 128 |
| Ticarcillin | >512 | >512 | >512 | 128 | 512 | >1024 | >512 | >512 | >512 | 8 | >512 |
| Ticarcillin + clavulanic acid a | 256 | 32 | 128 | 8 | 32 | 1024 | >512 | >512 | 256 | 8 | 256 |
| Piperacillin | 128 | 64 | 128 | 16 | 4 | 32 | 256 | 128 | 8 | 4 | 8 |
| Piperacillin + tazobactam b | 128 | 2 | 32 | 1 | 1 | 4 | 128 | 128 | 8 | 4 | 8 |
| Reference | [41] | [18] | [51] | [38] | [39] | [52] | [41] | [43] | [44] | [29] | [37] |
Table 6.
IC50 values for selected β-lactamases.
Table 6.
IC50 values for selected β-lactamases.
| Inhibitor | IC50 |
|---|
| OXA-2 | OXA-10 | OXA-18 | OXA-20 | OXA-24/40 | OXA-48 | OXA-58 | OXA-69 |
|---|
| Clavulanic acid (µM) | 3 | <40 | 0.08 | 2.2 | 300 | 16 | 310 | 100 |
| Tazobactam (µM) | 0.05 | - | 0.123 | - | 180 | 1.7 | 60 | 40 |
| Sulbactam (µM) | 0.1 | <40 | 0.56 | - | 190 | 50 | 2500 | 30 |
| NaCl (mM) | - | 19 | - | - | 3000 | 7 | 12 | 7.5 |
| Reference | [18] | [53] | [38] | [39] | [41] | [43] | [44] | [29] |
Reported clinical mutants. There are five sequences of OXA-1-like enzymes (
Table 7) which share at least 95% amino acid identity. OXA-31 was identified in a multi-drug resistant French isolate of
P. aeruginosa in 1999 in a non-transferrable plasmid. It differs from OXA-1 in three amino acids, but has identical susceptibility and kinetic profiles [
30]. Another plasmid-born variant, OXA-47, was initially identified in Turkey in a
K. pneumoniae isolate that also expressed OXA-48. The sequence of OXA-47 differs from OXA-1 in seven amino acids. OXA-47 confers resistance to amoxicillin and ticarcillin and decreased susceptibility to piperacillin, but does not change the susceptibility to carbapenems and cephalosporins. MICs obtained in the presence of inhibitors show an increased susceptibility to clavulanic acid but not to tazobactam [
43].
Table 7.
OXA-1 like enzymes.
Table 7.
OXA-1 like enzymes.
| β-Lactamase | Subgroup | Spectrum | First Reported Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-1/30 | OXA-1 | Narrow | E. coli | Plasmid | AF255921 | [50] |
| OXA-4 | OXA-1 | Narrow | C. freundii | Plasmid | AY162283 | [54] |
| OXA-31 | OXA-1 | Expanded | P. aeruginosa | Plasmid | AF294653 | [30] |
| OXA-47 | OXA-1 | Narrow | K. pneumoniae | Plasmid | AY237830 | [43] |
| OXA-224 | OXA-1 | - | P. aeruginosa | Plasmid | JN596991 | [55] |
Location and genetic environment. Analysis of the genetic environment of several OXA-1-like enzymes shows the encoding gene to be associated with Class 1 integrons [
11]. The OXA-1 gene was surrounded by an integrase gene and by an aminoglycoside acetyltransferase gene [
56]. A very similar arrangement was observed for the gene encoding OXA-31 [
30,
57]. The genes for OXA-4 and -224 were also located associated with a Class 1 integron, surrounded by an aminoglycoside acetyltransferase and
qacEΔ1 [
54,
57]. A different gene organization is described for the gene encoding OXA-47 [
43].
Structure determination. The crystal structure of the apoenzyme of OXA-1 was determined in 2003 [
57], and later as the complex with doripenem [
58]. A deacylation-deficient OXA-1 mutant structure is also described as apoenzyme and in complex with oxacillin [
59,
60].
7.2. OXA-2
The OXA-2 β-lactamase can be traced to the 1970s. The enzyme is characterized by a hydrolysis rate for oxacillin several times higher than for benzylpenicillin [
61].
Distribution and hosts. OXA-2-like enzymes are described worldwide [
62,
63,
64,
65,
66] and are predominantly, but not exclusively, found in
P. aeruginosa. Other species in which OXA-2 like enzymes have been found are
Salmonella [
64],
K. pneumoniae [
67],
Acinetobacter [
68] and also the Gram-positive
Corynebacterium amycolatum [
10], amongst other species [
10].
Antibiotic susceptibility and substrate profiles. Enzymes from this group were regarded as narrow-spectrum enzymes [
10], but recent experiments demonstrate that this enzyme is in fact a carbapenemase [
28]. When cloned into
E. coli it confers resistance to penicillins and decreases the susceptibility to cephalothin, ceftazidime, and carbapenems. In
A. baumannii background OXA-2 confers resistance to carbapenems with MIC values are very similar to the ones obtained for OXA-58 when tested under the same conditions [
28]. Changes in the MICs determined in the presence of clavulanic acid and tazobactam show that this enzyme is susceptible to their inhibitory activity [
18,
63]. Kinetically, it behaves like a classical CHDL, with low turnover rates for carbapenems but with very high affinities. Its turnover rate for oxacillin is higher than the one obtained for other CHDLs [
28]. The IC
50 values for sulbactam, tazobactam and clavulanic acid are reported as 0.1, 0.05 and 3 μM, respectively [
19].
Reported clinical mutants. Thirteen OXA-2-like enzymes are described, each sharing at least 80% amino acid identity (
Table 8). A cutoff of 95% amino acid identity identifies four subgroups. Although many of the isolates are only clinical findings, some have been studied sufficiently to allow their classification as narrow or expanded-spectrum enzymes.
Table 8.
OXA-2 like enzymes.
Table 8.
OXA-2 like enzymes.
| β-Lactamase | Subgroup | Spectrum a | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-2 | OXA-2 | Carbapenemase | S. Typhimurium | Plasmid | X07260 | [68,69] |
| OXA-3 | OXA-3 | Narrow | P. aeruginosa | Plasmid | L07945 | [9] |
| OXA-15 | OXA-2 | Expanded | P. aeruginosa | Plasmid | U63835 | [63] |
| OXA-21 | OXA-3 | - | A. baumannii | Plasmid | Y10693 | [70] |
| OXA-32 | OXA-2 | Expanded | P. aeruginosa | Plasmid | AF315351 | [18] |
| OXA-34 | OXA-2 | - | P. aeruginosa | - | AF350424 | - |
| OXA-36 | OXA-2 | - | P. aeruginosa | - | AF300985 | - |
| OXA-46 | OXA-46 | Narrow | P. aeruginosa | Plasmid | AF317511 | [71] |
| OXA-53 | OXA-53 | Expanded | S. enterica | Plasmid | AY289608 | [72] |
| OXA-141 | OXA-2 | - | P. aeruginosa | - | EF552405 | - |
| OXA-144 | OXA-2 | - | A. baumannii | - | FJ872530 | - |
| OXA-161 | OXA-2 | Expanded | P. aeruginosa | Plasmid | GQ202693 | [65] |
| OXA-210 | OXA-2 | - | P. aeruginosa | - | JF795487 | - |
OXA-15 is an Asp150Gly mutant found on a transferrable plasmid in a
P. aeruginosa strain isolated in Turkey in 1992 that had a considerable resistance to ceftazidime. When cloned into
E. coli it decreased the susceptibility to ampicillin, ceftazidime, moxalactam and aztreonam, but did not change the MICs for carbenicillin and other cephalosporins. Kinetics performed with a semi-purified enzyme showed that it had an increased activity against ceftazidime and decreased activity against ampicillin when compared to OXA-2 [
63]. OXA-32, a Leu164Ile mutant, was described in a ceftazidime-resistant
P. aeruginosa isolate from the French West Indies. The gene was located on a transferrable plasmid.
E. coli cells expressing the gene were less sensitive to ceftazidime, cefotaxime, cefepime, aztreonam, moxalactam, clavulanic acid and tazobactam, but more sensitive to amoxicillin, ticarcillin and cephalothin. It hydrolyzed several penicillins and cephalosporins, with the exception of cefotaxime [
18]. OXA-161, an Asn148Asp single mutant of OXA-2, was described in a
P. aeruginosa isolate from Spain showing an unusual resistance phenotype. When expressed in
P. aeruginosa this mutant conferred less protection to carbenicillin than OXA-2, but the MICs to ceftazidime, aztreonam and cefepime were higher [
65].
Although OXA-46 shares only 80.5% amino acid identity with OXA-2, we include it in the OXA-2 group. It was identified in a multi-drug-resistant
P. aeruginosa isolate from Italy. When cloned in
E. coli, it increased the MICs for penicillins and cephalothin, but not for carbapenems or extended-spectrum cephalosporins. No activity was seen against extended-spectrum cephalosporins or aztreonam [
69].
Location and genetic environment. The genes encoding several OXA-2-like enzymes are associated with Class 1 integrons. The one for OXA-15 was located in a
sulI-associated type transposon, between an aminoglycoside nucleotidyltransferase (
aadB) and
qacEΔ1, an ethidium bromide and quaternary ammonium resistance determinant [
63]. OXA-32 was also located in a Class 1 integron, and was flanked by an integrase gene and an aminoglycoside acetyltransferase [
18]. A very similar arrangement was observed for the genes of OXA-161 and OXA-53 [
65,
72]. The arrangement around the gene encoding OXA-46 was different; it was located in an integron containing two copies of
aacA4 and one of VIM-1 [
69].
Structure determination. The crystal structure for the OXA-2 wild-type enzyme was determined (PDB access number 1K38) but has not yet been published. The structure of OXA-46 is described [
73].
7.3. OXA-10
This enzyme was originally found in
Pseudomonas and called PSE-2 [
74].
Distribution and hosts. OXA-10-like enzymes have been identified in several human and animal isolates worldwide [
46,
66,
75,
76,
77,
78]. Although they are commonly associated with
P. aeruginosa, they have also been reported in
A. baumannii [
79] and in the
Enterobacteriaceae [
75,
80].
Antibiotic susceptibility and substrate profiles. When cloned into
E. coli, OXA-10 conferred resistance to all tested penicillins and to cephalothin. It increased the MICs of expanded-spectrum cephalosporins, aztreonam and carbapenems, without however reaching clinically relevant levels. When cloned in
A. baumannii it behaved as an expanded spectrum β-lactamase conferring resistance to carbapenems [
28]. The enzyme efficiently hydrolyzes penicillins, cephalosporins and (at a low rate) carbapenems [
24,
28]. When compared with the other Class D carbapenemases, the carbapenem kinetics of OXA-10 do not correlate to a significant increase in the MIC values produced by the enzymes. This increase is attributed to greater amount of the OXA-10 enzyme in the periplasm [
28].
Reported clinical mutants. Currently there are twenty-three clinical OXA-10-like enzymes with a widespread distribution in terms of host and geographic localization (
Table 9). Although there are limited data for each, they are traditionally characterized as either narrow spectrum or expanded-spectrum [
11]. OXA-11, a two amino acid mutant of OXA-10, was first described on a transferable plasmid in a Turkish isolate of
P. aeruginosa isolated in 1991. The enzyme conferred higher MICs for cephalosporins, moxalactam and aztreonam than those conferred by OXA-10. Preliminary kinetics indicate that those increases may be predominantly the result of increased relative affinity for the antibiotic [
81].
Table 9.
OXA-10 like enzymes.
Table 9.
OXA-10 like enzymes.
| β-Lactamase | Subgroup | Spectrum | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-10 | OXA-10 | Narrow a | P. aeruginosa | Plasmid | U37105 | [82] |
| OXA-5 | OXA-5 | Narrow | P. aeruginosa | Plasmid | X58272 | [83] |
| OXA-7 | OXA-10 | Narrow | E. coli | Plasmid | X75562 | [80] |
| OXA-11 | OXA-10 | Expanded | P. aeruginosa | Plasmid | Z22590 | [81] |
| OXA-13 | OXA-10 | Expanded | P. aeruginosa | Chromosome | U59183 | [77] |
| OXA-14 | OXA-10 | Expanded | P. aeruginosa | Plasmid | L38523 | [76] |
| OXA-16 | OXA-10 | Expanded | P. aeruginosa | Plasmid | AF043100 | [84] |
| OXA-17 | OXA-10 | Expanded | P. aeruginosa | Plasmid | AF060206 | [85] |
| OXA-19 | OXA-10 | Expanded | P. aeruginosa | Plasmid | AF043381 | [86] |
| OXA-28 | OXA-10 | Expanded | P. aeruginosa | Plasmid | AF231133 | [87] |
| OXA-35 | OXA-10 | Expanded | P. aeruginosa | Chromosome | AF315786 | [51] |
| OXA-56 | OXA-10 | Narrow | P. aeruginosa | - | AY445080 | [88] |
| OXA-74 | OXA-10 | - | P. aeruginosa | Chromosome | AJ854182 | [89] |
| OXA-101 | OXA-10 | - | C. freundii | Plasmid | AM412777 | [75] |
| OXA-128 | OXA-10 | - | A. baumannii | - | EU375515 | [79] |
| OXA-129 | OXA-10 | - | S. enterica | Plasmid | AM932669 | |
| OXA-142 | OXA-10 | - | P. aeruginosa | - | EU358785 | - |
| OXA-145 | OXA-10 | Expanded | P. aeruginosa | Chromosome | FJ790516 | [90] |
| OXA-147 | OXA-10 | Expanded | P. aeruginosa | - | FJ848783 | [91] |
| OXA-183 | OXA-10 | - | P. aeruginosa | - | HQ111474 | - |
| OXA-240 | OXA-10 | - | P. aeruginosa | - | JX089628 | - |
| OXA-251 | OXA-10 | - | P. aeruginosa | - | JN118546 | - |
| OXA-256 | OXA-10 | - | E. cloacae | Plasmid | HE616889 | [92] |
OXA-14, a Gly157Asp mutant of OXA-10, was isolated in
P. aeruginosa in Turkey in 1991. Its susceptibility profile to most tested β-lactams was similar to OXA-10, but OXA-14 was several-fold more resistant to cefepime and ceftazidime [
76]. OXA-16 has two amino acid mutations compared to OXA-10. It was isolated in Turkey in 1993 in a clinical isolate of
P. aeruginosa. OXA-16 increases the MICs of ceftazidime, cefotaxime, ceftriaxone, cefepime and moxalactam as compared to OXA-19 [
84]. OXA-17 was identified in a
P. aeruginosa isolate from Turkey and differs from OXA-10 by an Asn73Ser substitution. When cloned into
E. coli its susceptibility pattern β-lactams was very similar to OXA-10: it increased the MICs for penicillins, carbenicillin, cefotaxime, ceftriaxone, cefepime, cefoperazone, moxalactam and aztreonam, but failed to increase MICs for imipenem and ceftazidime [
85].
OXA-13 was isolated from a multi-drug resistant
P. aeruginosa French isolate. It is considered an expanded-spectrum enzyme. It differs from OXA-10 by nine amino acids. OXA-13 increased the MICs of penicillins, cefoperazone, cefotaxime, ceftazidime and aztreonam, but did not change the MIC of imipenem [
77]. OXA-19 differs from OXA-13 by two amino acids. It was isolated in France in 1991 from a
P. aeruginosa strain that was highly resistant to ceftazidime. OXA-19 is less susceptible to penicillins than OXA-13, although the MICs of ceftazidime are nearly identical [
86]. OXA-28 is a two amino acid mutant of OXA-13, identified in
P. aeruginosa. It increased the MICs of penicillins, cefotaxime and aztreonam. Resistance to ceftazidime was observed [
87]. OXA-35 was isolated in France in 1999 in
P. aeruginosa and differs in eight amino acids from OXA-10, but only one from OXA-13. It has almost identical susceptibility and kinetic profiles to β-lactams as OXA-10, with the exception of a higher susceptibility to piperacillin [
51,
86]. OXA-145, an OXA-35 derivative, was isolated in the Reunion Islands in 2008. It differs from OXA-35 by a Leu155 deletion. It is more susceptible to penicillins than OXA-35, but is more resistant to extended spectrum cephalosporins and aztreonam [
86]. A Trp154Leu mutation of OXA-35 gives OXA-147. This enzyme had an increased spectrum of activity against cephalosporins, while becoming more susceptible to penicillins [
87]. Both enzymes were initially identified in
P. aeruginosa.
Location and genetic environment. The genes encoding OXA-10 like enzymes are commonly found associated with Class 1 integrons and in some cases, the genes for OXA-35, OXA-145 and OXA-147 are downstream of an aminoglycoside acetyltransferase [
51,
86,
87].
Structure determination. Multiple OXA-10 structures have been determined at different pH values, and show different levels of carboxylation of the active site lysine [
24,
26,
93]. The structures of OXA-10 Tyr154 mutants have been determined as the apoenzyme and in complex with benzylpenicillin [
94]. The structure of a clinical mutant, OXA-13, was determined as the apoenzyme and in complex with meropenem [
95].
7.4. OXA-23
The first acquired CHDL was described in 1993 in a Scottish clinical
Acinetobacter baumannii strain, first isolated in 1985. The CHDL OXA-23 (formerly known as ARI-1, for
Acinetobacter Resistant to Imipenem) was located on a plasmid [
13].
Distribution and hosts. OXA-23 like enzymes are found currently worldwide [
11,
16,
96,
97,
98,
99] in both human and animals isolates [
100]. The origin of OXA-23 was traced to
Acinetobacter radioresistens, a commensal skin bacterium, where its contribution to carbapenem resistance was negligible due to the absence or low level of expression [
101]. OXA-23-like enzymes were also encountered in a carbapenem-resistant clinical isolate of the environmental bacterium and opportunistic pathogen
A. baylyi, where they were associated with a transposon [
102], and as well in
A. pittii [
96]. They have been found infrequently integrated into the chromosome of clinical
Proteus mirabilis (a member of the Family
Enterobacteriaceae) strains with decreased susceptibility to carbapenems. The genetic environment was identical to the one observed in
A. baumannii, suggesting the acquisition of the enzyme from a plasmid encoding OXA-23 which was suggested to not be able to replicate in
P. mirabilis and that was integrated ultimately into the chromosome [
52].
Antibiotic susceptibility and substrate profiles. In an
E. coli background OXA-23 confers resistance to penicillins and cephalothin and confers decreased susceptibility to moxalactam and carbapenems. A similar outcome is seen in an
A. baumannii background, although the MIC values of carbapenems and moxalactam reach levels considered to correspond to clinical resistance [
28]. MICs obtained in the presence of inhibitors show that clavulanic acid and tazobactam had some inhibitory activity [
52]. It has a low turnover for carbapenems although a very high affinity [
28]. The enzyme hydrolyzes effectively the cephalosporin cefotaxime, as well as oxacillin and other penicillins. It shows low turnover of aztreonam and ceftriaxone, and is unable to hydrolyze ceftazidime [
13,
28,
42].
Reported clinical mutants. Seventeen enzymes share at least 95% sequence identity to OXA-23 (
Table 10). OXA-27, a two amino acid derivative, was identified in a clinical
A. baumannii strain isolated in Singapore in a non-transferrable plasmid. Preliminary kinetic data showed that OXA-27 hydrolyzes penicillins, carbapenems and cephalosporins at a much lower rate. It is sensitive to tazobactam and to a lesser extent clavulanic acid [
103]. The chromosome-encoded OXA-102, OXA-103 and OXA-105 derivatives of OXA-23 have six, three and three amino acid substitutions, respectively. They are described as being less susceptible to the carbapenem ertapenem, but not to the carbapenems meropenem or imipenem [
101]. OXA-146 differs from OXA-23 by duplication of alanine 220. Unlike OXA-23, OXA-146 effectively hydrolyzes ceftazidime, while keeping a very similar substrate profile for other β-lactams [
42].
Table 10.
OXA-23 like enzymes.
Table 10.
OXA-23 like enzymes.
| β-Lactamase | Subgroup | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-23 | OXA-23 | A. baumannii | Plasmid | AJ132105 | [104] |
| OXA-27 | OXA-23 | A. baumannii | Plasmid | AF201828 | [103] |
| OXA-49 | OXA-23 | A. baumannii | - | AY288523 | - |
| OXA-102 | OXA-23 | A. radioresistens | Chromosome | - | [101] |
| OXA-103 | OXA-23 | A. radioresistens | Chromosome | - | [101] |
| OXA-105 | OXA-23 | A. radioresistens | Chromosome | - | [101] |
| OXA-133 | OXA-23 | A. radioresistens | - | EU571228 | [105] |
| OXA-146 | OXA-23 | A. baumannii | - | FJ194494 | - |
| OXA-165 | OXA-23 | A. baumannii | Plasmid | HM488986 | - |
| OXA-166 | OXA-23 | A. baumannii | Plasmid | HM488987 | - |
| OXA-168 | OXA-23 | A. baumannii | Plasmid | HM488989 | - |
| OXA-167 | OXA-23 | A. baumannii | Plasmid | HM488988 | - |
| OXA-169 | OXA-23 | A. baumannii | Plasmid | HM488990 | - |
| OXA-170 | OXA-23 | A. baumannii | Plasmid | HM488991 | - |
| OXA-171 | OXA-23 | A. baumannii | Plasmid | HM488992 | - |
| OXA-225 | OXA-23 | A. baumannii | - | JN638887 | - |
| OXA-239 | OXA-23 | A. baumannii | - | JQ837239 | - |
Location and genetic environment. OXA-23-like enzymes genes are usually associated with plasmids, although they are also found on the chromosome [
52,
98,
99,
106]. The most common genetic environment is the presence of IS
Aba1 elements. The IS
Aba1 insertion sequence is predominantly found in
A. baumannii and is associated with increased antibiotic resistance as a result of an increased copy number of the enzyme. IS
Aba1 has an important role in the genetic plasticity of
A. baumannii due to its characteristics as an important mobile element [
107,
108]. In Tn2006 the OXA-23 gene is bracketed by two identical copies of IS
Aba1 in opposite orientations, while in Tn2008 the downstream IS
Aba1 copy is missing [
98,
109]. More recently, Tn2009 was described in China: the OXA-23 gene is bracketed by two copies of IS
Aba1, but they both transcribe in the same direction [
110]. Another insertion sequence found associated with the OXA-23 encoding gene is IS
Aba4, located upstream of the gene, in a transposon denominated Tn2007. The gene is bracketed by IS
Aba4 and a truncated ATPase [
109,
111]. The hybrid promoter IS
Aba10-IS
Aba1 is characterized by the insertion of IS
Aba10 into the IS
Aba1 that precedes the OXA-23 gene, with an ATPase located downstream of the gene. Preliminary data suggest that this insertion sequence may confer additional promoter sequences, thereby increasing the expression level of OXA-23 [
112].
Structure determination. The structure for OXA-23 was determined at several different pH values, and in complex with meropenem. This latter structure is especially interesting as a result of the structural insights it provided with respect to its carbapenemase activity [
113]. The structure of an OXA-23 mutant, OXA-146, has also been recently described [
42].
7.5. OXA-24/40
OXA-24 (OXA-40) was initially identified in the chromosome of a carbapenem-resistant
A. baumannii clinical strain isolated in 1997 in Spain. Later, the reported sequence for the OXA-24 was revised and it turned out to be identical to the one of OXA-40 [
114]. This enzyme is frequently described as “OXA-24/40”.
Distribution and hosts. OXA-24/40-like enzymes have worldwide distribution including Europe [
115,
116], North America [
117,
115], Asia [
16,
116,
118] and South America [
119,
120]. Although this enzyme family is predominantly reported in
A. baumannii strains, OXA-24/40-like enzymes were described in
Acinetobacter haemolyticus [
120],
Acinetobacter pittii [
96],
Acinetobacter baylyi [
121] and
P. aeruginosa [
122].
Antibiotic susceptibility and substrate profiles. OXA-24/40 confers resistance to all penicillins and decreases susceptibility to carbapenems when cloned into an
E. coli background. The MICs for cephalosporins do not change significantly. A similar pattern was seen with OXA-24/40 expressed in
A. baumannii, but the MICs of the carbapenem antibiotics reached levels that would be considered of resistance [
28,
114]. The MIC values are not significantly changed by the presence of clavulanic acid, tazobactam and sulbactam [
114]. Kinetics performed in the presence of a source of carbon dioxide show a high turnover of oxacillin. The turnover for carbapenems is low, but the affinity is in the nanomolar range, which may explain why the enzyme is able to confer a degree of protection against carbapenems [
28]. Kinetics preformed in the absence of a source of carbon dioxide show some activity against penicillins and some cephalosporins, but not against aztreonam, cefepime or cefotaxime. The IC
50 values for clavulanic acid, tazobactam and sulbactam are 300, 180 and 190 μM, respectively. The enzyme was poorly inhibited by NaCl (IC
50 of 3 M) [
41].
Reported clinical mutants. Thirteen OXA-24/40-like enzymes can be sub-divided into four subgroups, each having at least 95% amino acid identity (
Table 11.).
OXA-25 (a two amino acid derivative of OXA-24/40) and OXA-26 (a one amino acid derivative of OXA-24/40) were first identified in European strains of
A. baumannii. Preliminary kinetics demonstrated that they had activity towards penicillins and carbapenems, but not toward cephalosporins [
103]. OXA-72, a Gly224Asp mutant of OXA-24/40, was first reported in Thailand (GenBank: AY739646.1) but is now spread worldwide [
122,
123,
124]. OXA-72 confers slightly decreased MIC values in the presence of carbapenems, but keeps the same susceptibility to aztreonam and cefepime as OXA-24/40 [
125]. OXA-160 is a Pro227Ser mutant of OXA-24/40 that was first described in the USA. Clones expressing this enzyme are more susceptible to carbapenems than those expressing OXA-24/40, but keep similar levels of susceptibility to aztreonam and cefepime [
125].
OXA-143 is a plasmid-borne, 31-amino acid mutant of OXA-24/40. It forms the second subgroup of the OXA-24/40 group. OXA-143 was first identified in 2004 in a Brazilian carbapenem-resistant clinical strain of
A. baumannii. When cloned into
E. coli and
A. baumannii backgrounds, this enzyme conferred decreased susceptibility to penicillins and carbapenems but not to cephalosporins. It hydrolyzes penicillins and carbapenems, although these data may underestimate its substrate profile as they were obtained without a carbon dioxide source. OXA-143 is inhibited by NaCl (IC
50 of 25 mM). This enzyme was not associated with integrons or insertion sequences. Analysis of the genetic environment suggested that it was acquired through homologous recombination. The current geographic location of this enzyme is essentially limited to Brazil [
126]. OXA-231 is a single amino acid derivative of OXA-143 that was recently isolated in Brazil. No data regarding the contribution of the enzyme to β-lactam susceptibility are available [
127].
OXA-253 consists of a third subgroup which differs from OXA-143 in 17 amino acids. It has a nearly identical antibiotic susceptibility profile to OXA-143, although it seems to be slightly more active against carbapenem antibiotics [
128].
Table 11.
OXA-24/40 like enzymes.
Table 11.
OXA-24/40 like enzymes.
| β-Lactamase | Subgroup | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-24/40 | OXA-24/40 | A. baumannii | Chromosome | AF509241 | [41] |
| OXA-25 | OXA-24/40 | A. baumannii | Chromosome | AF201826 | [103] |
| OXA-26 | OXA-24/40 | A. baumannii | Chromosome | AF201827 | [103] |
| OXA-72 | OXA-24/40 | A. baumannii | - | EF534256 | [129] |
| OXA-139 | OXA-24/40 | A. baumannii | - | AM991978 | - |
| OXA-143 | OXA-143 | A. baumannii | Plasmid | GQ861437 | [126] |
| OXA-160 | OXA-24/40 | A. baumannii | - | GU199038 | [125] |
| OXA-182 | OXA-182 | A. baumannii | Plasmid | HM640278 | [97] |
| OXA-207 | OXA-24/40 | A. pittii | - | JQ838185 | - |
| OXA-231 | OXA-143 | A. baumannii | Plasmid | JQ326200 | [127] |
| OXA-253 | OXA-253 | A. baumannii | - | KC479324 | - |
| OXA-255 | OXA-253 | A. pittii | - | KC479325 | [96] |
Location and genetic environment. The genes encoding OXA24/40-like enzymes are found both on the chromosome [
114] and on plasmids [
120,
122] and do not appear associated with insertion sequences or integrons. There is a suggestion that they may be acquired through homologous recombination since they are bracketed by two copies of the same replicase gene [
126,
127].
Structure determination. The structures of the OXA-24/40 apo-enzyme and of two deacylation deficient mutants (in complex with doripenem and oxacillin, respectively) have been determined [
54,
130,
131].
7.6. OXA-48
OXA-48 was identified in 2001 in a Turkish strain of multi-drug resistant
Klebsiella pneumoniae. It was located in a transferrable plasmid and was associated with IS
1999 [
43]. OXA-48-like enzymes are now the dominant CHDLs in the
Enterobacteriaceae. They have not yet been found in
Acinetobacter or
Pseudomonas.
Distribution and hosts. The OXA-48 group so far has been found exclusively within the
Enterobacteriaceae (
Citrobacter and
E. coli, among others) [
132]. The progenitor seems to have derived from a waterborne
Shewanella species (itself an opportunistic pathogen) in which chromosome-encoded OXA-48-like enzymes are described [
133,
134]. There are several distinct OXA-48-like genes in the
Enterobacteriaceae and in diverse
Shewanella species that are spread worldwide [
49,
132,
135,
136,
137].
Antibiotic susceptibility and substrate profiles. OXA-48 confers resistance to penicillins (with the exception of piperacillin) and decreases the susceptibility to carbapenems, but fails to change the MICs of expanded-spectrum cephalosporins when expressed in
E. coli. A similar substrate profile is observed in
A. baumannii, where the enzyme also increases the MIC values of piperacillin and carbapenems to levels of clinical resistance [
28]. MIC values obtained in the presence of tazobactam and clavulanic acid did not change [
43]. Kinetics obtained in the presence of sodium bicarbonate as a CO
2 source showed a good turnover for oxacillin and imipenem, but low turnover for other carbapenems. However, the affinity for carbapenems was in the nanomolar range [
27]. In the absence of a source of CO
2 OXA-48 hydrolyzes penicillins and cephalosporins, but not aztreonam [
43,
138]. The IC
50 values for clavulanic acid, tazobactam and sulbactam were 16, 1.7 and 50 μM, respectively. OXA-48 is inhibited by NaCl (IC
50 of 7 mM) [
43].
Reported clinical mutants. Twelve enzymes could be subdivided into two subgroups (OXA-48 and OXA-54), each with at least 95% sequence identity (
Table 12).
Table 12.
OXA-48 like enzymes.
Table 12.
OXA-48 like enzymes.
| β-Lactamase | Subgroup | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-48 | OXA-48 | K. pneumoniae | Plasmid | AY236073 | [43] |
| OXA-54 | OXA-54 | S. oneidensis | Chromosome | AY500137 | [133] |
| OXA-162 | OXA-48 | E. coli | Plasmid | HM015773 | [139] |
| OXA-163 | OXA-48 | E. cloacae | Plasmid | HQ700343 | [140] |
| OXA-181 | OXA-48 | K. pneumoniae | Plasmid | JN205800 | [141] |
| OXA-199 | OXA-48 | S. xiamenensis | Chromosome | JN704570 | [142] |
| OXA-204 | OXA-48 | K. pneumoniae | Plasmid | JQ809466 | [143] |
| OXA-232 | OXA-48 | E. coli | Plasmid | JX423831 | [144] |
| OXA-244 | OXA-48 | K. pneumoniae | Plasmid | JX438000 | [145] |
| OXA-245 | OXA-48 | K. pneumoniae | Plasmid | JX438001 | [145] |
| OXA-247 | OXA-48 | K. pneumoniae | Plasmid | JX893517 | [141] |
| OXA-370 | OXA-48 | Enterobacter sp. | - | KF900153 | - |
OXA-162, a Thr213Ala mutant of OXA-48 found in Turkey, confers resistance to penicillins, including piperacillin, while decreasing the susceptibility to cefepime, ceftazidime and carbapenems. Its kinetic properties are very similar to OXA-48 [
146]. OXA-163, a one amino acid mutant and four amino acids deletion derivative of OXA-48, is more active against penicillins, expanded-spectrum cephalosporins and aztreonam than OXA-48. It is less active against carbapenems and essentially with no increase in MIC values were observed when the enzyme was expressed in
E. coli. OXA-163 was more resistant to inhibition by NaCl. The susceptibility to clavulanate and tazobactam remained similar when compared to OXA-48. The turnover and relative affinity values against most penicillins and carbapenems experienced significant decreases, while the opposite was seen for piperacillin and expanded-spectrum cephalosporins [
140]. OXA-247, a two amino acid derivative of OXA-163 isolated from the same patient after antibiotic therapy, is more susceptible to expanded-spectrum cephalosporins and aztreonam [
147]. OXA-181, identified in
Shewanella siamenensis in India, and OXA-204 in
K. pneumoniae in Tunisia, have four and two amino acid substitutions respectively compared to OXA-48. Both have an almost identical susceptibility and kinetic profiles to those of OXA-48. Kinetically, they behave very similarly to OXA-48 [
141,
143,
148]. OXA-232, an Arg214Ser mutant derivative OXA-181, had a similar susceptibility profile to the one of OXA-181, although the MIC values of piperacillin and cephalothin were higher. In the absence of bicarbonate the turnover of ticarcillin, cephalothin and cefepime were higher than OXA-181 [
144].
OXA-54, identified in
Shewanella oneidensis, differs from OXA-48 by 20 amino acids and constitutes a subgroup of the OXA-48-like enzymes. The susceptibility profile conferred by this enzyme is very similar to that of OXA-48, with the exception of piperacillin and cephalothin, for which the MICs are lower. Kinetics obtained in the absence of CO
2 show comparable activity towards penicillins, carbapenems and cephalosporins but no activity against ceftazidime [
133].
Location and genetic environment. While the genes encoding OXA-48 enzymes are mostly associated with plasmids, they have been found in the chromosome of diverse species [
49,
148]. Several genetic environments have been described for these genes. In the first report of OXA-48, the insertion sequence IS
1999 (in Tn
1999, Tn
1999.2, Tn
1999.3 and Tn
1999.4) was found before the gene (under different arrangements) and was suggested to provide promoter sequences and to contribute to the mobilization of the gene. The initial transposon was made of two copies of IS
1999 bracketing the OXA-48 gene and
lysR. The arrangement of Tn
1999.2 is very similar, but the first IS
1999 is interrupted by IS
1R. On a third arrangement, Tn
1999.3, a variant of Tn
1999.2, a second IS
1R is found in between the gene for OXA-48 and
lysR. More recently, Tn
1999.4 was described as a mosaic transposon that also encodes CTX-M-15 β-lactamase [
43,
149]. The gene of OXA-163 Tn
1999.4 was associated with the IS
Ecl4 element [
142], while the ones encoding OXA-204 and OXA-181 were associated with IS
Ecp1 in Tn
2016 and Tn
2013 [
142,
143].
Structure determination. The structure of the apoenzyme of OXA-48 was determined at basic pH [
138].
7.7. OXA-58
This enzyme was described in 2005 on a plasmid in a multidrug resistant
A. baumannii strain, isolated in France in 2003 [
42].
Distribution and hosts. OXA-58-like genes are now disseminated worldwide [
10,
15,
96,
115,
137,
150,
151,
152,
153]. A collection of
Acinetobacter spp. isolates collected in several countries shows that OXA-58 like enzymes were present in clinical isolates for at least 10 years before their first description [
154]. Although OXA-58-like genes/enzymes are most frequently encountered in
A. baumannii strains, the genes have also been described in other species, such as
Acinetobacter nosocomialis in Taiwan and Spain [
155,
156],
A. pittii in Scotland, Taiwan, Spain [
155,
157,
158],
Acinetobacter haemolyticus in China [
121], and
Acinetobacter junii and
A. radioresistens in India [
105].
Antibiotic susceptibility profile and enzyme kinetics. When cloned in
E. coli and
A. baumannii OXA-58 confers resistance to penicillins and cephalothin, and decreased susceptibility to moxalactam and carbapenems, without affecting the susceptibility to other cephalosporins or monobactams [
28]. MIC values determined in the presence of tazobactam did not change, but some inhibitory effect was seen with clavulanic acid [
44]. In agreement with observations with other CHDLs, this enzyme has a low turnover for carbapenems (especially meropenem, doripenem and ertapenem) but with affinities in the nanomolar range (with the exception of imipenem) [
28]. OXA-58 turns over several penicillins and cephalothin fast [
28,
36]. Inhibition assays performed in the absence of a source of carbon dioxide showed respective IC
50 values for clavulanic acid, tazobactam and sulbactam of 310, 60 and 2.5 μM. OXA-58 is inhibited weakly by NaCl (IC
50 of 12 mM) [
44].
Reported clinical mutants. Four OXA-58 like enzymes are currently known and belong to the same subgroup (
Table 13.).
Table 13.
OXA-58 like enzymes.
Table 13.
OXA-58 like enzymes.
| β-Lactamase | Subgroup | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-58 | OXA-58 | A. baumannii | Plasmid | AY665723 | [44] |
| OXA-96 | OXA-58 | A. baumannii | Plasmid | DQ519090 | [159] |
| OXA-97 | OXA-58 | A. baumannii | Plasmid | EF102240 | [153] |
| OXA-164 | OXA-58 | A. baumannii | plasmid | GU831575 | [160] |
OXA-164, a Phe114Leu mutant of OXA-58, seems to be more sensitive to meropenem, but not imipenem, than OXA-58 [
160]. OXA-97, a Ala54Gly mutant of OXA-58 isolated in Tunisia, confers the same antimicrobial susceptibility profile as OXA-58 [
153].
Location and genetic environment. OXA-58-like enzymes encoding genes are usually associated with plasmids in
Acinetobacter species. The analysis of their genetic environment has shown that they are usually bracketed by two IS
Aba3 insertion sequences, upstream and downstream of the gene [
44]. Several arrangements, however, have been described. All have IS
Aba3 downstream of the gene, but upstream there is variability. Combinations of IS
Aba3 with IS
Aba1, IS
Aba2, IS
Aba125, IS
Aba825, IS
Aba8, IS
1008 and IS
1006 are described [
81,
152,
156,
159,
161,
162,
163]. Poirel
et al., give a detailed analysis of the genetic structures surrounding OXA-58-like genes [
159]. These sequences have promoter sequences, and when two insertion sequences are together they may generate a hybrid promoter which can increase gene expression [
162,
163,
164]. There have also been reports of multiple copies of the OXA-58 gene in the same plasmid, which also contributes to an increased copy number of the enzyme [
165].
Structure determination. The structure of the OXA-58 apoenzyme recently was described [
27].
7.8. OXA-134
Distribution and hosts. OXA-134 is found in diverse
Acinetobacter species including
A. baumannii,
A. lwoffii and
A. schindleri [
96]. Its origin has been linked to
Acinetobacter lwoffii, a human commensal and occasional pathogen [
30].
A. schindleri also encodes an OXA-134-like β-lactamase, but it seems to be from a different cluster [
166]. The only members of this group that have been found in plasmids belong to the OXA-235 subgroup, and are the focus of our discussion [
167].
Antibiotic susceptibility and substrate profiles. OXA-235 is the representative of the OXA-235 subgroup and was responsible for a decreased susceptibility to carbapenems when expressed in
A. baumannii and
A. baylyi. Kinetically, it showed a fast turnover of oxacillin, but surprisingly the turnover for ampicillin and carbapenems was very low. While a slow turnover for carbapenems is not unexpected, the reduced value for ampicillin turnover may be due to the lack of a source of carbon dioxide in the assay [
167].
Reported clinical mutants. There are several clinical mutants comprising three distinct subgroups (
Table 14.), but only the only plasmid encoded protein that has been studied is OXA-235.
Table 14.
OXA-134 like enzymes.
Table 14.
OXA-134 like enzymes.
| β-Lactamase | Subgroup | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-134 | OXA-134 | A. lwoffii | Chromosome | HQ122933 | [31] |
| OXA-186 | OXA-134 | A. lwoffii | Chromosome | - | [31] |
| OXA-187 | OXA-187 | A. lwoffii | Chromosome | - | [31] |
| OXA-188 | OXA-187 | A. lwoffii | Chromosome | - | [31] |
| OXA-189 | OXA-187 | A. lwoffii | Chromosome | - | [31] |
| OXA-190 | OXA-187 | A. lwoffii | Chromosome | - | [31] |
| OXA-191 | OXA-187 | A. lwoffii | Chromosome | - | [158] |
| OXA-235 | OXA-235 | A. baumannii | Plasmid | JQ820240 | [167] |
| OXA-236 | OXA-235 | A. baumannii | Plasmid | JQ820242 | [167] |
| OXA-237 | OXA-235 | A. baumannii | Plasmid | JQ820241 | [167] |
Location and genetic environment. In
A. baumannii, the OXA-235 subgroup genes are associated with two copies of IS
Aba1 [
167].
Structure Determination. No structure of any of members of the OXA-134 group is available.
7.9. Other OXA Groups
Several other less important groups have been described (
Table 15).
OXA-9. This enzyme was initially described associated with a transposon in a
K. pneumoniae strain [
168]. The enzyme has been described worldwide, and is considered a narrow spectrum β-lactamase [
10] which is not inhibited by sodium chloride [
169].
OXA-18. OXA-18, an extended-spectrum Class D β-lactamase, was described in France in 1995 in a
P. aeruginosa isolate [
32]. Later reports demonstrate its spread [
170,
171]. It increases the MIC values of penicillins, expanded spectrum cephalosporins and aztreonam. It is sensitive to inhibition by clavulanic acid. The kinetic data correlate with the MIC data, and the IC
50 values for the inhibitors are in the nanomolar range [
32]. This enzyme had a chromosomal location, where it was bracketed by two copies of the insertion sequence IS
CR19 [
170].
OXA-20. OXA-20 is a narrow-spectrum enzyme identified in
P. aeruginosa in France in 1995 which has disseminated in Europe and is now found in
A. baumannii [
10]. OXA-20 is located in the chromosome in an integron that encodes an aminoglycoside acetyltransferase. When cloned in
E. coli OXA-20 increased the MIC values for penicillins, cephalothin and imipenem but not those of extend-spectrum cephalosporins. It was inhibited by clavulanic acid. OXA-20 hydrolyzes penicillins, cephalothin and aztreonam [
33]. One mutant of this enzyme, OXA-37, is known [
172].
OXA-45. OXA-45 was initially identified in a multidrug resistant
P. aeruginosa isolate from Texas. No other OXA enzymes shares more than 80% sequence identity with OXA-45. It has an expanded-spectrum profile: it confers resistance to ceftazidime and ampicillin and increases the MIC values of piperacillin and of expanded-spectrum cephalosporins. The MIC values of carbapenems were not significantly changed. OXA-45 is sensitive to clavulanic acid [
173].
OXA-51. OXA-51 was described for the first time in 2004, in carbapenem-resistant strains isolated in Argentina between 1993–1994 [
174]. This is a predominantly chromosome-encoded CHDL from
Acinetobacter baumannii that has been recently described as associated with mobile elements in several
Acinetobacter species [
175,
176]. Although there are multiple OXA-51 mutants, little is known about their activity. Members of this family behave as poor penicillinases and very weak carbapenemases, without activity against cephalosporins. They are also resistant to inhibition by clavulanic acid and tazobactam [
29,
173,
177].
OXA-198. OXA-198 was identified on a Class 1 integron in a
P. aeruginosa strain resistant to several antimicrobials. It decreased susceptibility to penicillins, but it did not change the MICs of cephalosporins. It was resistant to tazobactam [
178].
LCR-1. LCR-1 was first described in 1982 in
P. aeruginosa strain from the United States. It hydrolyzed various penicillins, but neither cefotaxime nor imipenem [
179,
180]. Another member of this group having a similar kinetic behavior, NPS-1, was also found in
P. aeruginosa in the United Kingdom. When expressed in
P. aeruginosa LCR-1 it did not change the susceptibility to cephalosporins, monobactams or carbapenems [
181].
Table 15.
Other OXA groups.
Table 15.
Other OXA groups.
| β-Lactamase | Subgroup | Spectrum | First Report Host | Chromosome/Plasmid | GenBank Accession Number | Ref. |
|---|
| OXA-9 | - | Narrow | K. pneumoniae | Plasmid | M55547 | [168] |
| OXA-18 | - | Extended | P. aeruginosa | Chromosome | U85514 | [32] |
| OXA-20 | - | Narrow | P. aeruginosa | Chromosome | AF024602 | [33] |
| OXA-45 | - | Expanded | P. aeruginosa | Plasmid | AJ519683 | [173] |
| OXA-51 | - | Carbapenemase | A. baumannii | Chromosome | AJ309734 | [174] |
| OXA-198 | - | Narrow | P. aeruginosa | Plasmid | HQ634775 | [178] |
| LCR-1 | - | Narrow | P. aeruginosa | Plasmid | Q00983 | [89] |