Dietary Approaches in the Management of Diabetic Patients with Kidney Disease
Abstract
1. Introduction
2. Clinical Practice Guidelines on the Nutritional Management of Diabetic Kidney Disease
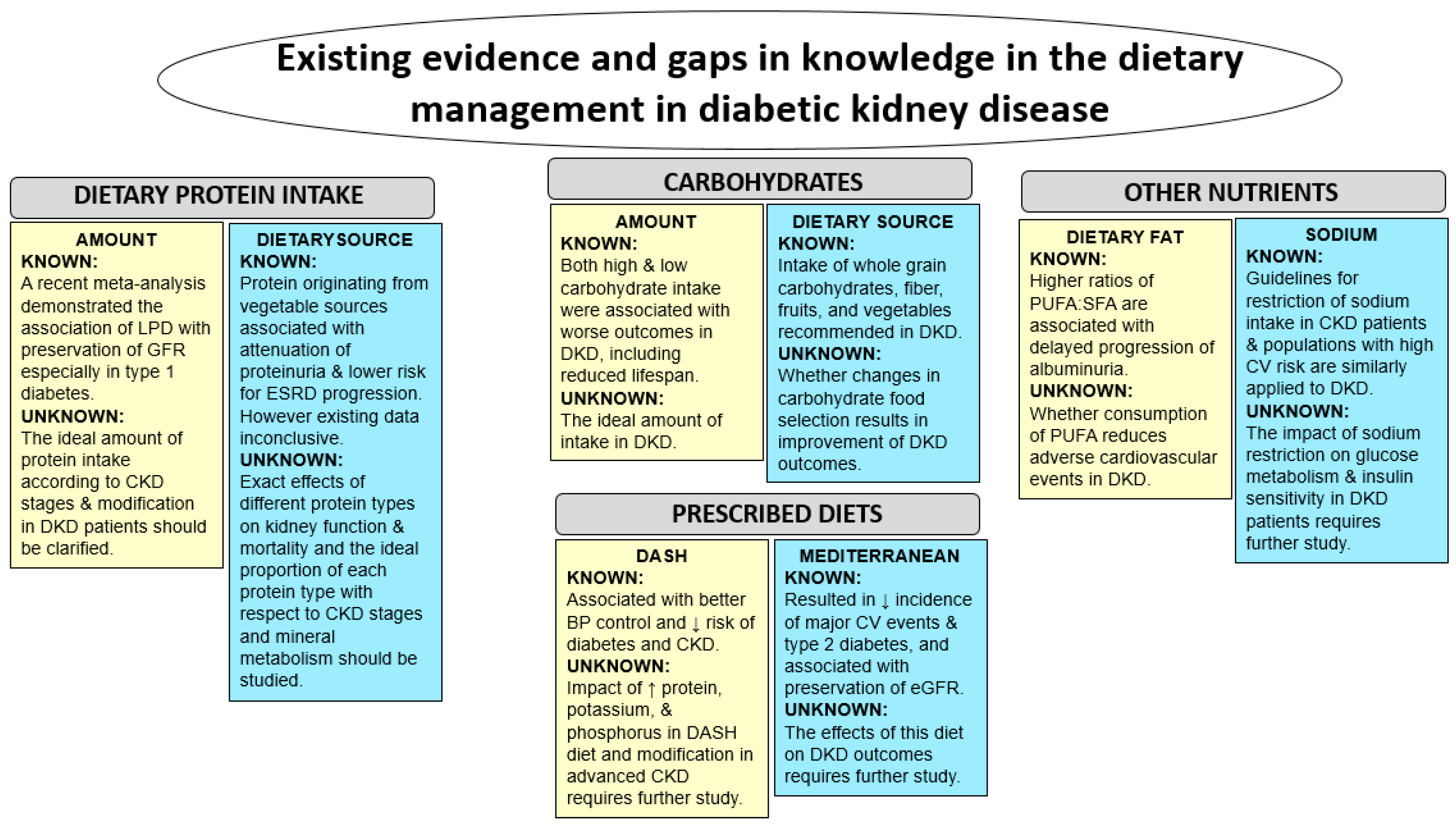
3. Dietary Protein Intake in Diabetic Kidney Disease: Non-Dialysis Dependent Chronic Kidney Disease
3.1. Quantity of Dietary Protein Intake
3.2. Sources of Dietary Protein Intake
4. Dietary Protein Intake in Diabetic Kidney Disease Patients Receiving Dialysis
5. Energy and Carbohydrate Intake in Diabetic Kidney Disease
6. Fat Intake in Diabetic Kidney Disease
7. Sodium Intake in Diabetic Kidney Disease
8. Comparison of Prescribed Diets
9. Practical Implementation of Nutritional Management
10. Future Areas for Research
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States; US Department of Health and Human Services: Atlanta, GA, USA, 2014.
- Gregg, E.W.; Li, Y.; Wang, J.; Burrows, N.R.; Ali, M.K.; Rolka, D.; Williams, D.E.; Geiss, L. Changes in diabetes-related complications in the united states, 1990–2010. N. Engl. J. Med. 2014, 370, 1514–1523. [Google Scholar] [CrossRef] [PubMed]
- Satirapoj, B.; Adler, S.G. Prevalence and management of diabetic nephropathy in western countries. Kidney Dis. 2015, 1, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Collins, A.J.; Foley, R.N.; Chavers, B.; Gilbertson, D.; Herzog, C.; Ishani, A.; Johansen, K.; Kasiske, B.L.; Kutner, N.; Liu, J.; et al. US Renal Data System 2013 Annual Data Report. Am. J. Kidney Dis. 2014, 63, A7. [Google Scholar] [CrossRef] [PubMed]
- Goldstein-Fuchs, J.; Kalantar-Zadeh, K. Nutrition intervention for advanced stages of diabetic kidney disease. Diabetes Spectr. 2015, 28, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Whitham, D. Nutrition for the prevention and treatment of chronic kidney disease in diabetes. Can. J. Diabetes 2014, 38, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Ley, S.H.; Hamdy, O.; Mohan, V.; Hu, F.B. Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet 2014, 383, 1999–2007. [Google Scholar] [CrossRef]
- KDOQI. KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am. J. Kidney 2007, 49, S12–154. [Google Scholar]
- Kovesdy, C.P.; Kopple, J.D.; Kalantar-Zadeh, K. Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: Reconciling low protein intake with nutritional therapy. Am. J. Clin. Nutr. 2013, 97, 1163–1177. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Moore, L.W.; Tortorici, A.R.; Chou, J.A.; St-Jules, D.E.; Aoun, A.; Rojas-Bautista, V.; Tschida, A.K.; Rhee, C.M.; Shah, A.A.; et al. North american experience with low protein diet for non-dialysis-dependent chronic kidney disease. BMC Nephrol. 2016, 17, 90. [Google Scholar] [CrossRef] [PubMed]
- Ko, G.J.; Obi, Y.; Tortorici, A.R.; Kalantar-Zadeh, K. Dietary protein intake and chronic kidney disease. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, K.R.; Bakris, G.L.; Bilous, R.W.; Chiang, J.L.; de Boer, I.H.; Goldstein-Fuchs, J.; Hirsch, I.B.; Kalantar-Zadeh, K.; Narva, A.S.; Navaneethan, S.D.; et al. Diabetic kidney disease: A report from an ada consensus conference. Am. J. Kidney Dis. 2014, 64, 510–533. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.W.; Byham-Gray, L.D.; Scott Parrott, J.; Rigassio-Radler, D.; Mandayam, S.; Jones, S.L.; Mitch, W.E.; Osama Gaber, A. The mean dietary protein intake at different stages of chronic kidney disease is higher than current guidelines. Kidney Int. 2013, 83, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.P.; Rains, T.M. Dietary protein is important in the practical management of prediabetes and type 2 diabetes. J. Nutr. 2015, 145, 164S–169S. [Google Scholar] [CrossRef] [PubMed]
- Friedman, A.N. High-protein diets: Potential effects on the kidney in renal health and disease. Am. J. Kidney Dis. 2004, 44, 950–962. [Google Scholar] [CrossRef] [PubMed]
- Hammond, K.A.; Janes, D.N. The effects of increased protein intake on kidney size and function. J. Exp. Biol. 1998, 201, 2081–2090. [Google Scholar] [PubMed]
- Alavi, F.K.; Zawada, E.T.; Simmons, J.L. Renal hemodynamic and histological consequences of diets high in unsaturated fat, protein or sucrose in obese zucker rats. Clin. Nephrol. 1995, 43, 122–130. [Google Scholar] [PubMed]
- Graf, H.; Stummvoll, H.K.; Luger, A.; Prager, R. Effect of amino acid infusion on glomerular filtration rate. N. Engl. J. Med. 1983, 308, 159–160. [Google Scholar] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Comparison of high vs. normal/low protein diets on renal function in subjects without chronic kidney disease: A systematic review and meta-analysis. PLoS ONE 2014, 9, e97656. [Google Scholar] [CrossRef] [PubMed]
- Knight, E.L.; Stampfer, M.J.; Hankinson, S.E.; Spiegelman, D.; Curhan, G.C. The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann. Intern. Med. 2003, 138, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Evert, A.B.; Boucher, J.L.; Cypress, M.; Dunbar, S.A.; Franz, M.J.; Mayer-Davis, E.J.; Neumiller, J.J.; Nwankwo, R.; Verdi, C.L.; Urbanski, P.; et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2013, 36, 3821–3842. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.D.; Bending, J.J.; Dodds, R.A.; Mattock, M.B.; Murrells, T.J.; Keen, H.; Viberti, G.C. Restriction of dietary protein and progression of renal failure in diabetic nephropathy. Lancet 1989, 2, 1411–1415. [Google Scholar] [CrossRef]
- Zeller, K.; Whittaker, E.; Sullivan, L.; Raskin, P.; Jacobson, H.R. Effect of restricting dietary protein on the progression of renal failure in patients with insulin-dependent diabetes mellitus. N. Engl. J. Med. 1991, 324, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Dullaart, R.P.; Beusekamp, B.J.; Meijer, S.; van Doormaal, J.J.; Sluiter, W.J. Long-term effects of protein-restricted diet on albuminuria and renal function in IDDM patients without clinical nephropathy and hypertension. Diabetes Care 1993, 16, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Raal, F.J.; Kalk, W.J.; Lawson, M.; Esser, J.D.; Buys, R.; Fourie, L.; Panz, V.R. Effect of moderate dietary protein restriction on the progression of overt diabetic nephropathy: A 6-mo prospective study. Am. J. Clin. Nutr. 1994, 60, 579–585. [Google Scholar] [PubMed]
- Hansen, H.P.; Tauber-Lassen, E.; Jensen, B.R.; Parving, H.H. Effect of dietary protein restriction on prognosis in patients with diabetic nephropathy. Kidney Int. 2002, 62, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Klahr, S.; Levey, A.S.; Beck, G.J.; Caggiula, A.W.; Hunsicker, L.; Kusek, J.W.; Striker, G. The effects of dietary protein restriction and blood-pressure control on the progression of chronic renal disease. Modification of diet in renal disease study group. N. Engl. J. Med. 1994, 330, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.P.; Kalantar-Zadeh, K.; Kopple, J.D. Is there a role for ketoacid supplements in the management of CKD? Am. J. Kidney Dis. 2015, 65, 659–673. [Google Scholar] [CrossRef] [PubMed]
- Pijls, L.T.; de Vries, H.; van Eijk, J.T.; Donker, A.J. Protein restriction, glomerular filtration rate and albuminuria in patients with type 2 diabetes mellitus: A randomized trial. Eur. J. Clin. Nutr. 2002, 56, 1200–1207. [Google Scholar] [CrossRef] [PubMed]
- Meloni, C.; Morosetti, M.; Suraci, C.; Pennafina, M.G.; Tozzo, C.; Taccone-Gallucci, M.; Casciani, C.U. Severe dietary protein restriction in overt diabetic nephropathy: Benefits or risks? J. Ren. Nutr. 2002, 12, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Dussol, B.; Iovanna, C.; Raccah, D.; Darmon, P.; Morange, S.; Vague, P.; Vialettes, B.; Oliver, C.; Loundoun, A.; Berland, Y. A randomized trial of low-protein diet in type 1 and in type 2 diabetes mellitus patients with incipient and overt nephropathy. J. Ren. Nutr. 2005, 15, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Robertson, L.; Waugh, N.; Robertson, A. Protein restriction for diabetic renal disease. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef]
- Nezu, U.; Kamiyama, H.; Kondo, Y.; Sakuma, M.; Morimoto, T.; Ueda, S. Effect of low-protein diet on kidney function in diabetic nephropathy: Meta-analysis of randomised controlled trials. BMJ. Open 2013, 3, e002934. [Google Scholar] [CrossRef] [PubMed]
- Rughooputh, M.S.; Zeng, R.; Yao, Y. Protein diet restriction slows chronic kidney disease progression in non-diabetic and in type 1 diabetic patients, but not in type 2 diabetic patients: A meta-analysis of randomized controlled trials using glomerular filtration rate as a surrogate. PLoS ONE 2015, 10, e0145505. [Google Scholar] [CrossRef] [PubMed]
- Giordano, M.; Ciarambino, T.; Castellino, P.; Cataliotti, A.; Malatino, L.; Ferrara, N.; Politi, C.; Paolisso, G. Long-term effects of moderate protein diet on renal function and low-grade inflammation in older adults with type 2 diabetes and chronic kidney disease. Nutrition 2014, 30, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Azadbakht, L.; Atabak, S.; Esmaillzadeh, A. Soy protein intake, cardiorenal indices, and c-reactive protein in type 2 diabetes with nephropathy: A longitudinal randomized clinical trial. Diabetes Care 2008, 31, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Lew, Q.J.; Jafar, T.H.; Koh, H.W.; Jin, A.; Chow, K.Y.; Yuan, J.M.; Koh, W.P. Red meat intake and risk of esrd. J. Am. Soc. Nephrol. 2016, 28, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Dunkler, D.; Dehghan, M.; Teo, K.K.; Heinze, G.; Gao, P.; Kohl, M.; Clase, C.M.; Mann, J.F.; Yusuf, S.; Oberbauer, R.; et al. Diet and kidney disease in high-risk individuals with type 2 diabetes mellitus. JAMA Intern. Med. 2013, 173, 1682–1692. [Google Scholar] [CrossRef] [PubMed]
- Moorthi, R.N.; Armstrong, C.L.; Janda, K.; Ponsler-Sipes, K.; Asplin, J.R.; Moe, S.M. The effect of a diet containing 70% protein from plants on mineral metabolism and musculoskeletal health in chronic kidney disease. Am. J. Nephrol. 2014, 40, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wei, G.; Jalili, T.; Metos, J.; Giri, A.; Cho, M.E.; Boucher, R.; Greene, T.; Beddhu, S. The associations of plant protein intake with all-cause mortality in CKD. Am. J. Kidney Dis. 2016, 67, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A. Protein and energy: Recommended intake and nutrient supplementation in chronic dialysis patients. Semin. Dial. 2004, 17, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Obi, Y.; Qader, H.; Kovesdy, C.P.; Kalantar-Zadeh, K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Supasyndh, O.; Lehn, R.S.; McAllister, C.J.; Kopple, J.D. Normalized protein nitrogen appearance is correlated with hospitalization and mortality in hemodialysis patients with Kt/V greater than 1.20. J. Ren. Nutr. 2003, 13, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Ravel, V.A.; Molnar, M.Z.; Streja, E.; Kim, J.C.; Victoroff, A.; Jing, J.; Benner, D.; Norris, K.C.; Kovesdy, C.P.; Kopple, J.D.; et al. Low protein nitrogen appearance as a surrogate of low dietary protein intake is associated with higher all-cause mortality in maintenance hemodialysis patients. J. Nutr. 2013, 143, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- Kopple, J.D. National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. Am. J. Kidney Dis. 2001, 37, S66–S70. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Fouque, D.; Kopple, J.D. Outcome research, nutrition, and reverse epidemiology in maintenance dialysis patients. J. Ren. Nutr. 2004, 14, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.M.; Ahmadi, S.F.; Kalantar-Zadeh, K. The dual roles of obesity in chronic kidney disease: A review of the current literature. Curr. Opin. Nephrol. Hypertens. 2016, 25, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Ou, S.H.; Chen, M.Y.; Huang, C.W.; Chen, N.C.; Wu, C.H.; Hsu, C.Y.; Chou, K.J.; Lee, P.T.; Fang, H.C.; Chen, C.L. Potential role of vegetarianism on nutritional and cardiovascular status in Taiwanese dialysis patients: A case-control study. PLoS ONE 2016, 11, e0156297. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Tortorici, A.R.; Chen, J.L.; Kamgar, M.; Lau, W.L.; Moradi, H.; Rhee, C.M.; Streja, E.; Kovesdy, C.P. Dietary restrictions in dialysis patients: Is there anything left to eat? Semin. Dial. 2015, 28, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A.; Cano, N.J.; Franch, H.; Fouque, D.; Himmelfarb, J.; Kalantar-Zadeh, K.; Kuhlmann, M.K.; Stenvinkel, P.; TerWee, P.; Teta, D.; et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: A consensus statement by the international society of renal nutrition and metabolism. Kidney Int. 2013, 84, 1096–1107. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, X.; Song, Y.; Caballero, B.; Cheskin, L.J. Association between obesity and kidney disease: A systematic review and meta-analysis. Kidney Int. 2008, 73, 19–33. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 4. Lifestyle management. Diabetes Care 2017, 40, S33–S43. [Google Scholar]
- Otoda, T.; Kanasaki, K.; Koya, D. Low-protein diet for diabetic nephropathy. Curr. Diabetes Rep. 2014, 14, 523. [Google Scholar] [CrossRef] [PubMed]
- Solon-Biet, S.M.; McMahon, A.C.; Ballard, J.W.; Ruohonen, K.; Wu, L.E.; Cogger, V.C.; Warren, A.; Huang, X.; Pichaud, N.; Melvin, R.G.; et al. The ratio of macronutrients, not caloric intake, dictates cardiometabolic health, aging, and longevity in ad libitum-fed mice. Cell Metab. 2014, 19, 418–430. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.E.; Suarez, J.A.; Brandhorst, S.; Balasubramanian, P.; Cheng, C.W.; Madia, F.; Fontana, L.; Mirisola, M.G.; Guevara-Aguirre, J.; Wan, J.; et al. Low protein intake is associated with a major reduction in igf-1, cancer, and overall mortality in the 65 and younger but not older population. Cell Metab. 2014, 19, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Evert, A.B.; Boucher, J.L. New diabetes nutrition therapy recommendations: What you need to know. Diabetes Spectr. 2014, 27, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Michas, G.; Micha, R.; Zampelas, A. Dietary fats and cardiovascular disease: Putting together the pieces of a complicated puzzle. Atherosclerosis 2014, 234, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T.J.; Gregoire, J.; Hegele, R.A.; Couture, P.; Mancini, G.B.; McPherson, R.; Francis, G.A.; Poirier, P.; Lau, D.C.; Grover, S.; et al. 2012 Update of the Canadian cardiovascular society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can. J. Cardiol. 2013, 29, 151–167. [Google Scholar] [CrossRef] [PubMed]
- Canadian Diabetes Association Clinical Practice Guidelines Expert Committee; Dworatzek, P.D.; Arcudi, K.; Gougeon, R.; Husein, N.; Sievenpiper, J.L.; Williams, S.L. Nutrition therapy. Can. J. Diabetes 2013, 37 (Suppl. 1), S45–S55. [Google Scholar] [CrossRef] [PubMed]
- Tyson, C.C.; Nwankwo, C.; Lin, P.H.; Svetkey, L.P. The dietary approaches to stop hypertension (DASH) eating pattern in special populations. Curr. Hypertens. Rep. 2012, 14, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, H.; Theilla, M.; Attal-Singer, J.; Singer, P. Effects of polyunsaturated fatty acid consumption in diabetic nephropathy. Nat. Rev. Nephrol. 2011, 7, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Cardenas, C.; Bordiu, E.; Bagazgoitia, J.; Calle-Pascual, A.L.; Diabetes and Nutrition Study Group, Spanish Diabetes Association. Polyunsaturated fatty acid consumption may play a role in the onset and regression of microalbuminuria in well-controlled type 1 and type 2 diabetic people: A 7-year, prospective, population-based, observational multicenter study. Diabetes Care 2004, 27, 1454–1457. [Google Scholar] [PubMed]
- Lee, C.C.; Sharp, S.J.; Wexler, D.J.; Adler, A.I. Dietary intake of eicosapentaenoic and docosahexaenoic acid and diabetic nephropathy: Cohort analysis of the diabetes control and complications trial. Diabetes Care 2010, 33, 1454–1456. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, R.; Cavanaugh, K.L.; Blot, W.J.; Ikizler, T.A.; Lipworth, L.; Kabagambe, E.K. Dietary polyunsaturated fatty acids and incidence of end-stage renal disease in the Southern Community Cohort Study. BMC Nephrol. 2016, 17, 152. [Google Scholar] [CrossRef] [PubMed]
- ORIGIN Trial Investigators. Cardiovascular and other outcomes postintervention with insulin glargine and omega-3 fatty acids (originale). Diabetes Care 2016, 39, 709–716. [Google Scholar]
- Wright, J.A.; Cavanaugh, K.L. Dietary sodium in chronic kidney disease: A comprehensive approach. Semin. Dial. 2010, 23, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Kong, Y.W.; Baqar, S.; Jerums, G.; Ekinci, E.I. Sodium and its role in cardiovascular disease—The debate continues. Front. Endocrinol. 2016, 7, 164. [Google Scholar] [CrossRef] [PubMed]
- Cutler, J.A.; Obarzanek, E. Nutrition and blood pressure: Is protein one link? Toward a strategy of hypertension prevention. Ann. Intern. Med. 2005, 143, 74–75. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Nichols, M.; Sun, X.; D′Agostino, R.B., Jr.; Haffner, S.M. Adherence to the dash diet is inversely associated with incidence of type 2 diabetes: The insulin resistance atherosclerosis study. Diabetes Care 2009, 32, 1434–1436. [Google Scholar] [CrossRef] [PubMed]
- Rebholz, C.M.; Crews, D.C.; Grams, M.E.; Steffen, L.M.; Levey, A.S.; Miller, E.R., III; Appel, L.J.; Coresh, J. Dash (dietary approaches to stop hypertension) diet and risk of subsequent kidney disease. Am. J. Kidney Dis. 2016, 68, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Asghari, G.; Yuzbashian, E.; Mirmiran, P.; Azizi, F. The association between dietary approaches to stop hypertension and incidence of chronic kidney disease in adults: The Tehran lipid and glucose study. Nephrol. Dial. Transplant. 2017, 32 (Suppl. 2), ii224–ii230. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P.; Kalantar-Zadeh, K. Dash-ing toward improved renal outcomes: When healthy nutrition prevents incident chronic kidney disease. Nephrol. Dial. Transplant. 2017, 32 (Suppl. 2), ii231–ii233. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.R., Jr.; Gross, M.D.; Steffen, L.; Steffes, M.W.; Yu, X.; Svetkey, L.P.; Appel, L.J.; Vollmer, W.M.; Bray, G.A.; Moore, T.; et al. The effects of dietary patterns on urinary albumin excretion: Results of the dietary approaches to stop hypertension (DASH) trial. Am. J. Kidney Dis. 2009, 53, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvado, J.; Covas, M.I.; Corella, D.; Aros, F.; Gomez-Gracia, E.; Ruiz-Gutierrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvado, J.; Bullo, M.; Babio, N.; Martinez-Gonzalez, M.A.; Ibarrola-Jurado, N.; Basora, J.; Estruch, R.; Covas, M.I.; Corella, D.; Aros, F.; et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: Results of the predimed-reus nutrition intervention randomized trial. Diabetes Care 2011, 34, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, K.R.; Shuler, L.A.; Packard, D.P.; Milton, J.E.; Daratha, K.B.; Bibus, D.M.; Short, R.A. Comparison of low-fat versus mediterranean-style dietary intervention after first myocardial infarction (from the heart institute of spokane diet intervention and evaluation trial). Am. J. Cardiol. 2008, 101, 1523–1530. [Google Scholar] [CrossRef] [PubMed]
- Nafar, M.; Noori, N.; Jalali-Farahani, S.; Hosseinpanah, F.; Poorrezagholi, F.; Ahmadpoor, P.; Samadian, F.; Firouzan, A.; Einollahi, B. Mediterranean diets are associated with a lower incidence of metabolic syndrome one year following renal transplantation. Kidney Int. 2009, 76, 1199–1206. [Google Scholar] [CrossRef] [PubMed]
- Khatri, M.; Moon, Y.P.; Scarmeas, N.; Gu, Y.; Gardener, H.; Cheung, K.; Wright, C.B.; Sacco, R.L.; Nickolas, T.L.; Elkind, M.S. The Association between a Mediterranean-Style Diet and Kidney Function in the Northern Manhattan Study Cohort. Clin. J. Am. Soc. Nephrol. 2014, 9, 1868–1875. [Google Scholar] [CrossRef] [PubMed]
- Tirosh, A.; Golan, R.; Harman-Boehm, I.; Henkin, Y.; Schwarzfuchs, D.; Rudich, A.; Kovsan, J.; Fiedler, G.M.; Bluher, M.; Stumvoll, M.; et al. Renal function following three distinct weight loss dietary strategies during 2 years of a randomized controlled trial. Diabetes Care 2013, 36, 2225–2232. [Google Scholar] [CrossRef] [PubMed]
- Milas, N.C.; Nowalk, M.P.; Akpele, L.; Castaldo, L.; Coyne, T.; Doroshenko, L.; Kigawa, L.; Korzec-Ramirez, D.; Scherch, L.K.; Snetselaar, L. Factors associated with adherence to the dietary protein intervention in the modification of diet in renal disease study. J. Am. Diet. Assoc. 1995, 95, 1295–1300. [Google Scholar] [CrossRef]
- Fouque, D.; Horne, R.; Cozzolino, M.; Kalantar-Zadeh, K. Balancing nutrition and serum phosphorus in maintenance dialysis. Am. J. Kidney Dis. 2014, 64, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Pisani, A.; Riccio, E.; Bellizzi, V.; Caputo, D.L.; Mozzillo, G.; Amato, M.; Andreucci, M.; Cianciaruso, B.; Sabbatini, M. 6-tips diet: A simplified dietary approach in patients with chronic renal disease. A clinical randomized trial. Clin. Exp. Nephrol. 2016, 20, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Kovesdy, C.P.; Bross, R.; Benner, D.; Noori, N.; Murali, S.B.; Block, T.; Norris, J.; Kopple, J.D.; Block, G. Design and development of a dialysis food frequency questionnaire. J. Ren. Nutr. 2011, 21, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Paes-Barreto, J.G.; Silva, M.I.; Qureshi, A.R.; Bregman, R.; Cervante, V.F.; Carrero, J.J.; Avesani, C.M. Can renal nutrition education improve adherence to a low-protein diet in patients with stages 3 to 5 chronic kidney disease? J. Ren. Nutr. 2013, 23, 164–171. [Google Scholar] [CrossRef] [PubMed]
- D′Alessandro, C.; Rossi, A.; Innocenti, M.; Ricchiuti, G.; Bozzoli, L.; Sbragia, G.; Meola, M.; Cupisti, A. Dietary protein restriction for renal patients: Don′t forget protein-free foods. J. Ren. Nutr. 2013, 23, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.M.; Leung, A.M.; Kovesdy, C.P.; Lynch, K.E.; Brent, G.A.; Kalantar-Zadeh, K. Updates on the management of diabetes in dialysis patients. Semin. Dial. 2014, 27, 135–145. [Google Scholar] [CrossRef] [PubMed]

| Nutrient | Guidance for Quantity | Guidance for Quality | Special Considerations |
|---|---|---|---|
| Protein | <15% of total calories, or RDA of 0.8 g/kg BW/day for patients with DKD. | Emphasize vegan protein sources, and non-fat or low-fat dairy products are recommended. | Modified to >1.2 g/kg BW/day in patients with ESRD treated with dialysis. |
| Carbohydrate | Specific recommendation was not provided. | Choice of high fiber fruits and vegetables. No more than 10% of daily calories as simple sugars. | Monitor potassium and phosphatelevels. |
| Fat | Specific recommendation was not provided. | Recommend omega-3 and omega-9 polyunsaturated fatty acid consumption. | Within meal plan for calories and palatability. |
| Sodium | 1.5–2.3 g of sodium/day. | Use non-processed fresh food, and utilize sodium-free herbs and spices. | Sodium restrictions should be individualized. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, G.J.; Kalantar-Zadeh, K.; Goldstein-Fuchs, J.; Rhee, C.M. Dietary Approaches in the Management of Diabetic Patients with Kidney Disease. Nutrients 2017, 9, 824. https://doi.org/10.3390/nu9080824
Ko GJ, Kalantar-Zadeh K, Goldstein-Fuchs J, Rhee CM. Dietary Approaches in the Management of Diabetic Patients with Kidney Disease. Nutrients. 2017; 9(8):824. https://doi.org/10.3390/nu9080824
Chicago/Turabian StyleKo, Gang Jee, Kamyar Kalantar-Zadeh, Jordi Goldstein-Fuchs, and Connie M. Rhee. 2017. "Dietary Approaches in the Management of Diabetic Patients with Kidney Disease" Nutrients 9, no. 8: 824. https://doi.org/10.3390/nu9080824
APA StyleKo, G. J., Kalantar-Zadeh, K., Goldstein-Fuchs, J., & Rhee, C. M. (2017). Dietary Approaches in the Management of Diabetic Patients with Kidney Disease. Nutrients, 9(8), 824. https://doi.org/10.3390/nu9080824






