1. Introduction
The World Health Organization (WHO) predicts that six out of ten individuals will live in urban settings by 2030; seven out of ten individuals will live in cities by 2050. Although cities concentrate people, opportunities and services, they also concentrate risks and hazards for health. These include chronic diseases, such as diabetes and heart diseases resulting from reduced physical activity; asthma and other pollution-related diseases; and mental health issues due to stress and poor living conditions [
1]. The aging population further exacerbates the problem, as seniors consume more than twice the healthcare resources of the general population [
2]. In the United States, seniors will approach 20 percent of the entire population by 2030, compared to 13 percent in 2010 [
3].
To meet escalating healthcare needs, planners need to prepare and proactively account for future demands [
4]. In addition to addressing the scarcity of healthcare resources, equity and affordability also come into play, as the median household income of seniors is typically lower than the younger age groups [
5,
6]. Consequently, it is increasingly important for planners to take funding mechanisms into consideration and provide publicly funded options for those in need in both acute care and community care settings. Site selection of resources for community and preventative care (e.g., primary care, public health units, health education centers, community rehabilitation centers) is especially important, as this kind of care can help reduce additional spending on avoidable hospitalizations and disability-related spending, which currently take up a high percentage of state and federal budgets [
7,
8].
This paper discusses the feasibility of our evaluation framework in supporting hospital site selection for an aging population (
i.e., age 65 and older). This is critical because once established and built, hospitals seldom close down, instead often undergoing multiple expensive renovations, restructuring and expansions in attempts to adapt to evolving needs. The average lifespan of non-residential buildings is approximately 50 years, but it is not uncommon for non-residential buildings including hospitals to have a lifespan of over 100 years [
9,
10]. The aging population adds further challenges, not only because of the volume of healthcare consumed, but also because of the specific factors required to support this age group, such as distance to hospital, accessibility, affordability, chronic diseases and palliative support, which all become necessary considerations. The uncertainties associated with these factors could negatively impact healthcare resource planning unless an appropriate framework is in place to guide sustainable planning.
The World Commission on the Environment and Development [
11] defines sustainability as “development that meets the needs of the present without compromising the ability of future generations to meet their own needs.” Addressing both present and future needs in a sustainable manner requires a balance among social, environmental and economic factors, also known as the “triple bottom-line” [
12]. This is especially challenging in the context of an aging population with its high, varying and complex healthcare needs [
13]. Thus, improved capabilities to project and prioritize the future healthcare needs of an aging population are critical for sustainability planning. For instance, prioritization of multiple alternatives (e.g., various locations, hospital size, specialization) during the decision-making and planning process can help minimize costs and maximize impact while providing better publicly funded hospital facilities for the elderly in an economically, environmentally and socially sustainable way. If sustainable solutions are not found, as the baby boomers reach their senior years with multiple chronic conditions, healthcare costs are bound to increase significantly.
The literature points to a limited number of decision frameworks in different jurisdictions for evidence-based hospital site selection and planning. Usiak [
14] analytically considered features such as site size, location, visibility, access and topography in his site selection decision framework. Busselton Hospital and Health Centre in Australia [
15] also employed evidence-based evaluations to assist with site selection decisions. These examples, however, represent exceptions rather than the norm. The existing decision-making processes for site selection lack the ability to take into account the comprehensive criteria required for an aging population in a structured manner to support a systematic planning process and do not consistently evaluate alternatives or transparently represent the evaluation results. The selection and collection of relevant high-quality data for the evaluation can also prove challenging.
Our research team developed an evaluation framework, taking into account comprehensive criteria in a structured way based on an extensive literature review, and transparently interpreted the evaluation results by utilizing Geographic Information System (GIS) tools as the underlying evaluative approach. The framework provides an opportunity for urban planners and decision-makers to systematically reflect on key issues facing aging communities and use urban planning practices to effect positive changes in addressing evolving population health needs. GIS “integrates hardware, software and data for capturing, managing, analyzing and displaying all forms of geographically referenced information” (ESRI). Through its spatial capabilities, GIS enables planners to visualize data in ways that reveal relationships and trends and thus more effectively interpret and evaluate the impact of alternatives on the key factors of site selection.
To assess the applicability of our framework, the team performed a retrospective case study based in Dallas, Texas. An actual planned, publicly funded new hospital, located at the intersection of Record Crossing Road and Harry Hines Boulevard in the northwestern part of Dallas, Texas, was chosen as the study site. Our framework, which includes sustainability criteria, was applied retrospectively to evaluate whether the site selection of the hospital was sufficient to support an aging population. This case study application enabled the team to demonstrate the feasibility of our framework as well as illustrate the evaluative process and types of data required. Part of our results were presented during an expert workshop entitled “Sustainable Cities, Better Health, Better Future,” held on 2 March 2012, at Stanford University.
Although by no means exhaustive, this is, to our knowledge, one of the first urban planning and decision support tools in development that proactively addresses population health and resource planning. Through this work, we hope to promote dialogues among various stakeholders and advance this multidisciplinary area that holds the key to urban health sustainability.
3. Evaluation Framework
Based on extensive literature review and interviews with experts (urban planners, architects and healthcare planners), we developed an evaluation framework for determining locations for healthcare facilities for an aging population (
Table 1). The framework took into account existing urban infrastructure, various stakeholders and their intended activities during different project phases (e.g., construction and operation phases). The identified stakeholder groups includes targeted primary users (
i.e., the aging population), decision-makers/owners and neighborhood sub-populations.
Table 1.
The evaluative framework for health care facility locations for an aging population.
Table 1.
The evaluative framework for health care facility locations for an aging population.
| Category | Criteria | Elements exemplified but not restrictive |
|---|
| Needs | Demographics | % of seniors and a projected aging population from census blocks |
| Socio-economics | % of low-income specific for senior households from census blocks |
| Health conditions | % of seniors with chronic diseases (e.g., diabetes) and smoking seniors from census blocks |
| Existing health services | Types of healthcare services provided, size, clientele and funding mechanism |
| Health services utilization | Frequency of visitation for health services, healthcare spending and health insurance payment |
| Capacity | Infrastructure: construction phase | Water and electricity provision |
| Infrastructure: accessibility | Road capacity, volumes and public transport services |
| Infrastructure: other utilities | Capacities of facilities (e.g., power substation) and networks for utilities’ provision |
| Support | Financial support | Funds from government and independent organizations |
| Community support | Community opinion gathered through surveys or focus groups |
We organized our evaluation criteria into three main categories: (1) needs; (2) capacity and (3) support. Because different jurisdictions can provide different available data to evaluate each criterion, the framework allows planners to flexibly select data as elements (i.e., indicators) for their evaluations. Consequently, although we suggest the data collected as elements, they are not restricted for the applications.
The first category (i.e., needs) takes into account the social environment of nearby possible locations and consists of five criteria. First, demographic analyses and trends help planners understand the potential catchment population and related healthcare needs surrounding the proposed healthcare facilities. We recommend data about the percentages of seniors and a projected aging population from census blocks around a proposed site location as elements required to evaluate this criterion. Higher percentages of seniors and a projected aging population make the site more appropriate for a hospital with a geriatric or long-term care focus. Second, it is important to analyze the socio-economic status of seniors around the various possible locations. Our framework recommends data about the percentage of low-income specific for senior households from census blocks around a proposed site location as an element for evaluation. The percentage of low-income households around a possible site location informs the logical funding model necessary (e.g., publicly funded facilities are more appropriate for low-income areas). Third, planners need to analyze the health conditions of an aging population around possible site locations. Both health conditions (e.g., diseases) and lifestyles (e.g., healthy behaviors) are important factors in assessing and projecting overall health status over time. Our framework suggests data about the percentages of seniors with chronic diseases (e.g., diabetes) and smoking seniors from census blocks around a proposed site location as elements for the evaluation of this criterion. Fourth, planners should identify the various health services that already exist in the neighborhood as well as whether the proposed new site would have a complement or substitute effect. The types of services provided, size, clientele and funding mechanism are all relevant considerations. Fifth, planners need to factor in current health services utilization patterns such as frequency of visitation for health services and healthcare spending.
The second category (i.e., capacity) takes into account the physical infrastructure adjacent to alternative locations and includes three criteria. First, an analysis of the location and capacity of infrastructure informs planners as to whether the construction of healthcare facilities is feasible. Second, planners need to analyze accessibility options surrounding the sites of choice, including private and public transportation options, as well as physical and operational conditions of the supporting infrastructure. Third, planners need to analyze the conditions of other utilities’ provisions, either to ensure sufficient provision of utilities for the selected locations or to be prepared to solicit support and/or absorb those costs and efforts as part of the project.
The last category (i.e., support) takes into account general support from owners and third-party stakeholders, and it includes two components. First, planners need to ensure sufficient financial capacity to support the project in the construction as well as the operational phases. Second, planners need to align with the community to ensure support at various levels to best address local needs.
4. Application and Results
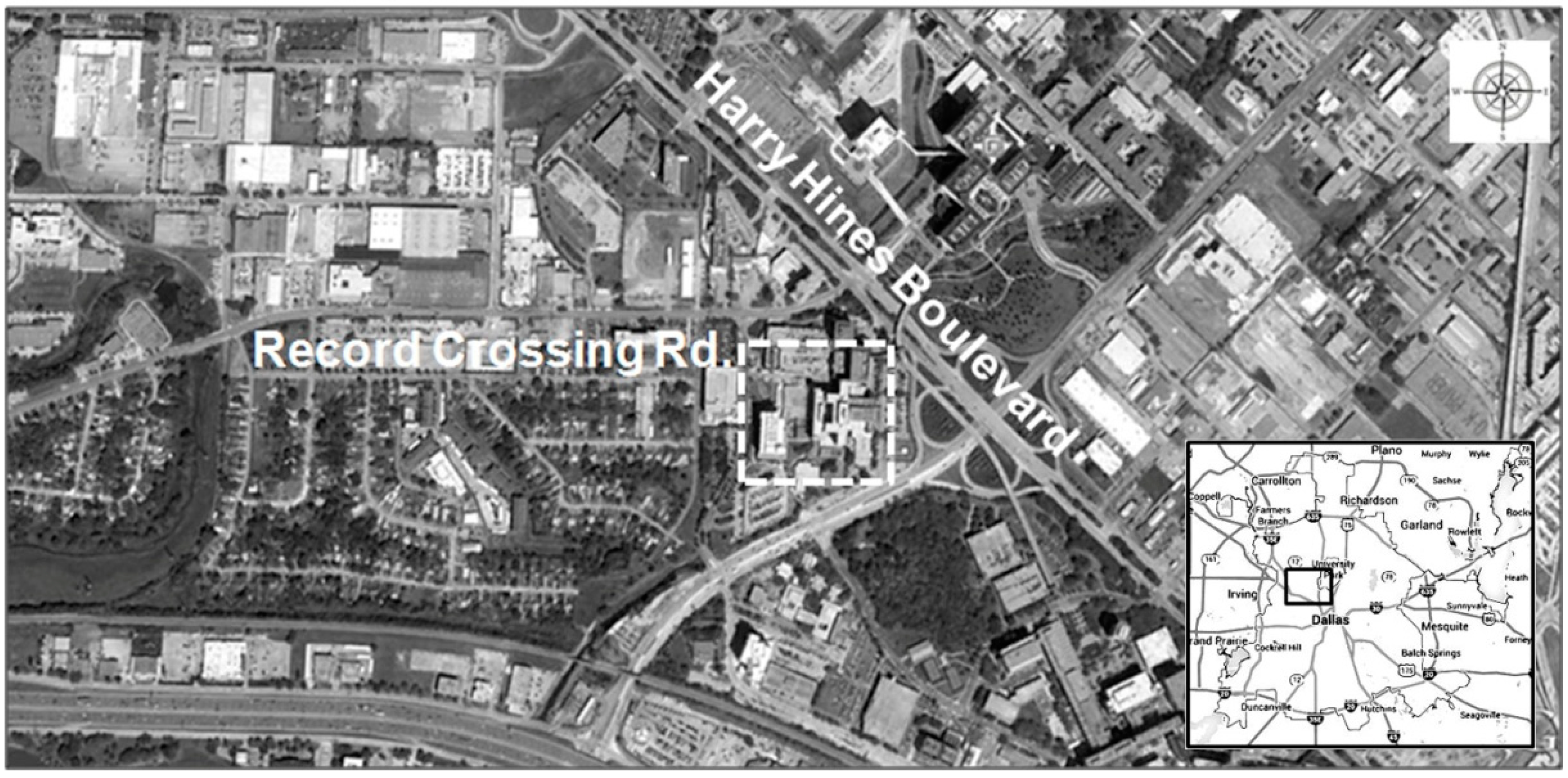
Our research team applied the framework to one specific location in Dallas, Texas and employed web-based GIS tools to display evaluation findings. The study site is located at the intersection of Record Crossing Road and Harry Hines Boulevard in the northwestern part of Dallas, Texas (
Figure 1). It is an actual planned, publicly funded new hospital. We applied our framework retrospectively to evaluate whether the site selection of the hospital was sufficient to support an aging population.
Figure 1.
Study site location (Dallas, Texas).
Figure 1.
Study site location (Dallas, Texas).
To systematically apply our framework, we reviewed formal decision-making processes required for construction projects and found they consist of five decision-enabling phases: the definition, formulation, evaluation, decision and iteration phases [
16,
33]. In the retrospective application of our framework, we focused on the theoretical phases (
i.e., definition, formulation and evaluation). In the definition phase, we needed to define multiple relevant indicators (
i.e., elements) required to evaluate the criteria because some criteria (e.g., health conditions) are complex concepts with multiple contributing factors. We evaluated whether the proposed site could be suitable for a publicly funded hospital for an aging population based on each criterion by using elements defined. The analytical results of our framework application are summarized below.
We analyzed the demographic pattern around the hospital site and confirmed that seniors account for a relatively high proportion of the population in the area. To further understand the population base, the socio-economic status (SES) of the hospital catchment population was evaluated. Using Esri Community Analyst (a web-based GIS tool), the percentage of households with incomes less than $15,000 by census block in 2013 (based on the federal poverty line of $11,490 for 2013 [
34]) was mapped (
Figure 2). A high percentage of low-income households that operate on subsistence living standards was found around the hospital site. The pocket of poverty seems to be very specific to the hospital catchment area. The median household income for Dallas in 2012 was $47,301, slightly below the Texas median of $50,740 and the U.S. median of $51,371 [
35]. Note that the income data are not senior-specific but serve as a reasonable proxy (used due to data availability); drilling down into the data to define household and individual income specific for seniors would further confirm our observations. In addition, scoring systems are required for consistent and systematic evaluations.
Figure 2.
Percentage household income less than $10,000 by block in 2013.
Figure 2.
Percentage household income less than $10,000 by block in 2013.
We analyzed the hospital utilization pattern of the hospital catchment population by taking into account the number of visits to physicians and healthcare spending per household. By mapping the percentage of households that visited physicians more than 6 times in the preceding 12 months, a low rate of visitation to doctors was found, despite the high percentage of seniors around the hospital site (
Figure 3). According to the literature, those aged 65 and above average 7.1 hospital visits per year in the U.S., compared to 3.7 average visits by those aged 45–65 [
36]. Seniors in this hospital catchment area currently under-utilize health services compared to the overall U.S. seniors; the reason for this trend is unknown, but is explored further (below). Spending on healthcare-related issues, including health insurance, is another factor related to health service utilization. Individuals over 65 years of age in the U.S. spent, on average, $4843 per annum on healthcare, with a substantial $3085 of the total expenditure being spent on health insurance [
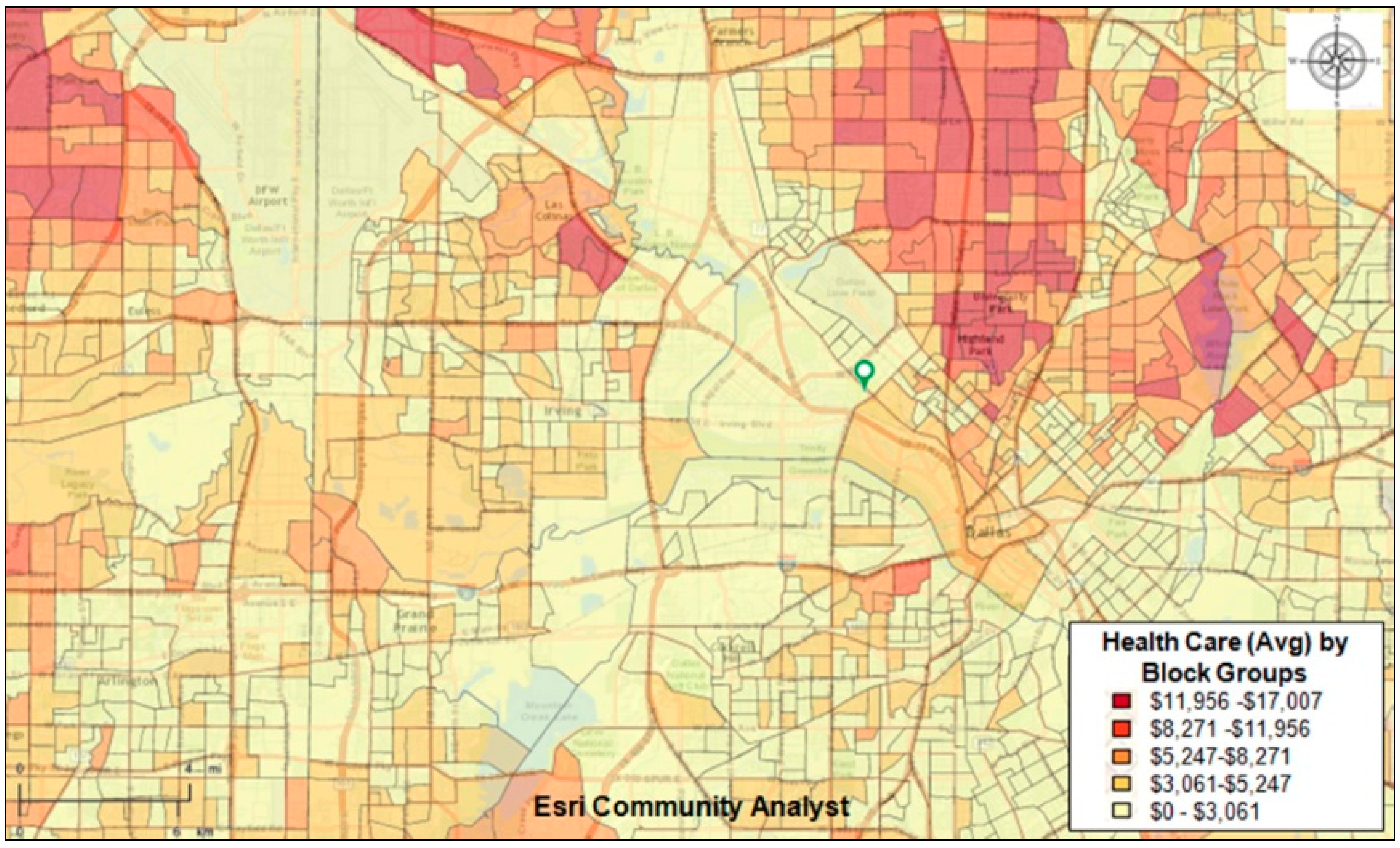
36]. We observed that on average, the hospital catchment population spent significantly less money on healthcare compared to those who lived in areas further out.
Figure 4 and
Figure 5 depict the spending patterns around the hospital site in question by census blocks in 2013. General population data are utilized as proxies for these analyses; senior-specific healthcare and health insurance data would help validate our findings.
Figure 3.
Visited doctor in last 12 months: 8+ times by block (%) in 2013.
Figure 3.
Visited doctor in last 12 months: 8+ times by block (%) in 2013.
Figure 4.
Average health care spending by block (%) in 2013.
Figure 4.
Average health care spending by block (%) in 2013.
To identify possible reasons for the unusually low health services utilization, we analyzed health behaviors (e.g., smoking rate and exercise rate) of the catchment population as proxies for health status and, in turn, healthcare needs. A high smoking rate and low exercise rate was found among the population in the area; as these are established risk factors for obesity and lung cancer, the inference was made that that the low health services utilization was not due to a lack of need. We also analyzed various healthcare facilities in the proposed hospital catchment area, identifying types of services provided, size and funding mechanism to consider the specialized services provided from the proposed hospital or other existing hospitals. An evaluation of the funding mechanisms of surrounding health facilities indicated that they are mostly privately operated. The observed low utilization rate was most likely due to affordability, and thus an unmet healthcare need seems to exist for our identified group of low-income seniors.
Figure 5.
Average health insurance payment by block (%) in 2013.
Figure 5.
Average health insurance payment by block (%) in 2013.
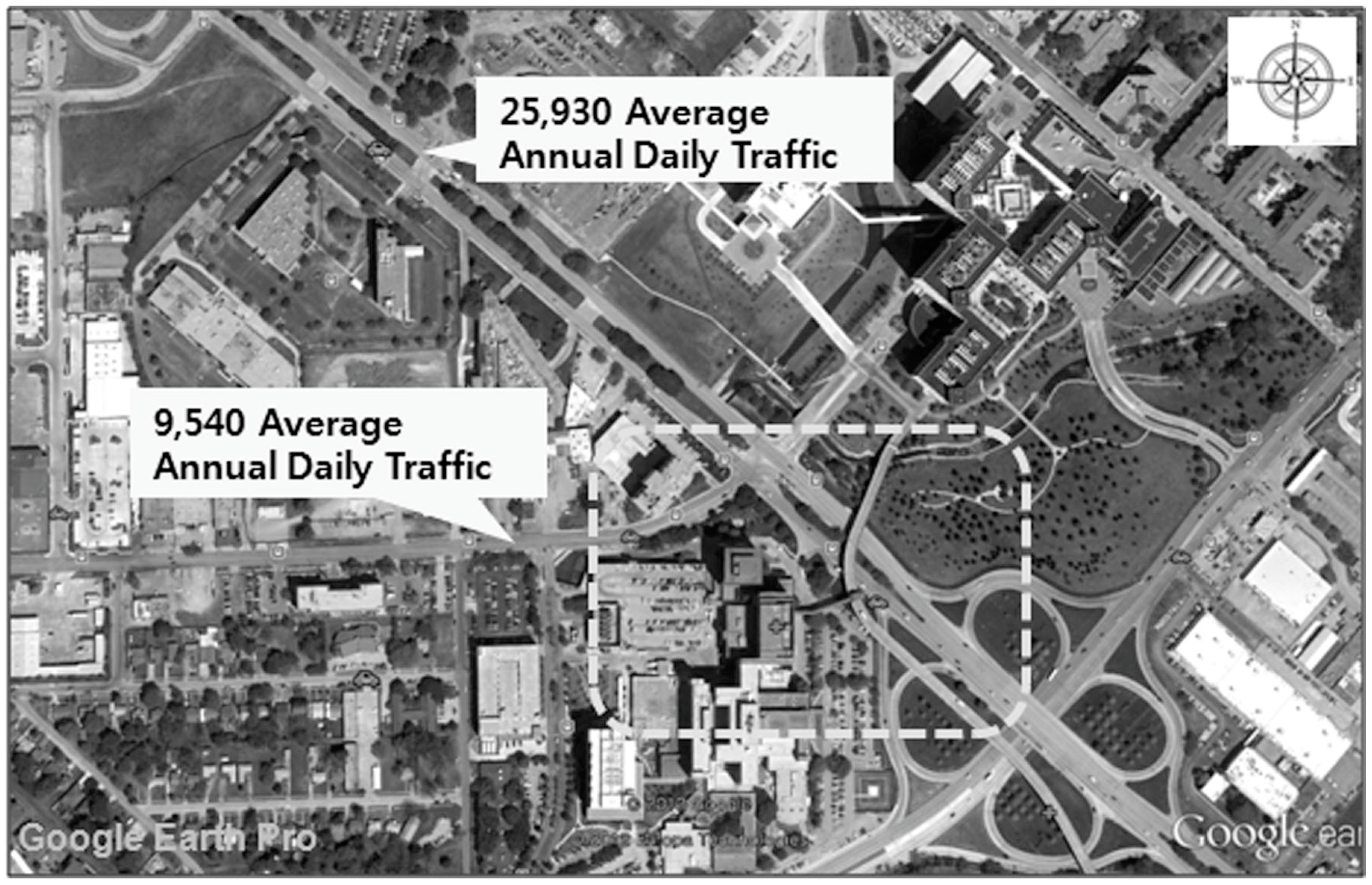
Next, the accessibility of the proposed hospital site was evaluated for both a general population and a specific focus on seniors. Traffic volumes for existing roads leading to the hospital were analyzed using Google Earth Pro, a web-based GIS tool (
Figure 6). Generally, roadways are in good operating conditions without congestion when Average Annual Daily Traffic (AADT) per lane is 10,000 or less. Since the AADT for the four-lane road is 25,930 and 9540 for the two-lane road, existing roads have not reached their capacities and will be able to provide appropriate service levels for the proposed hospital site.
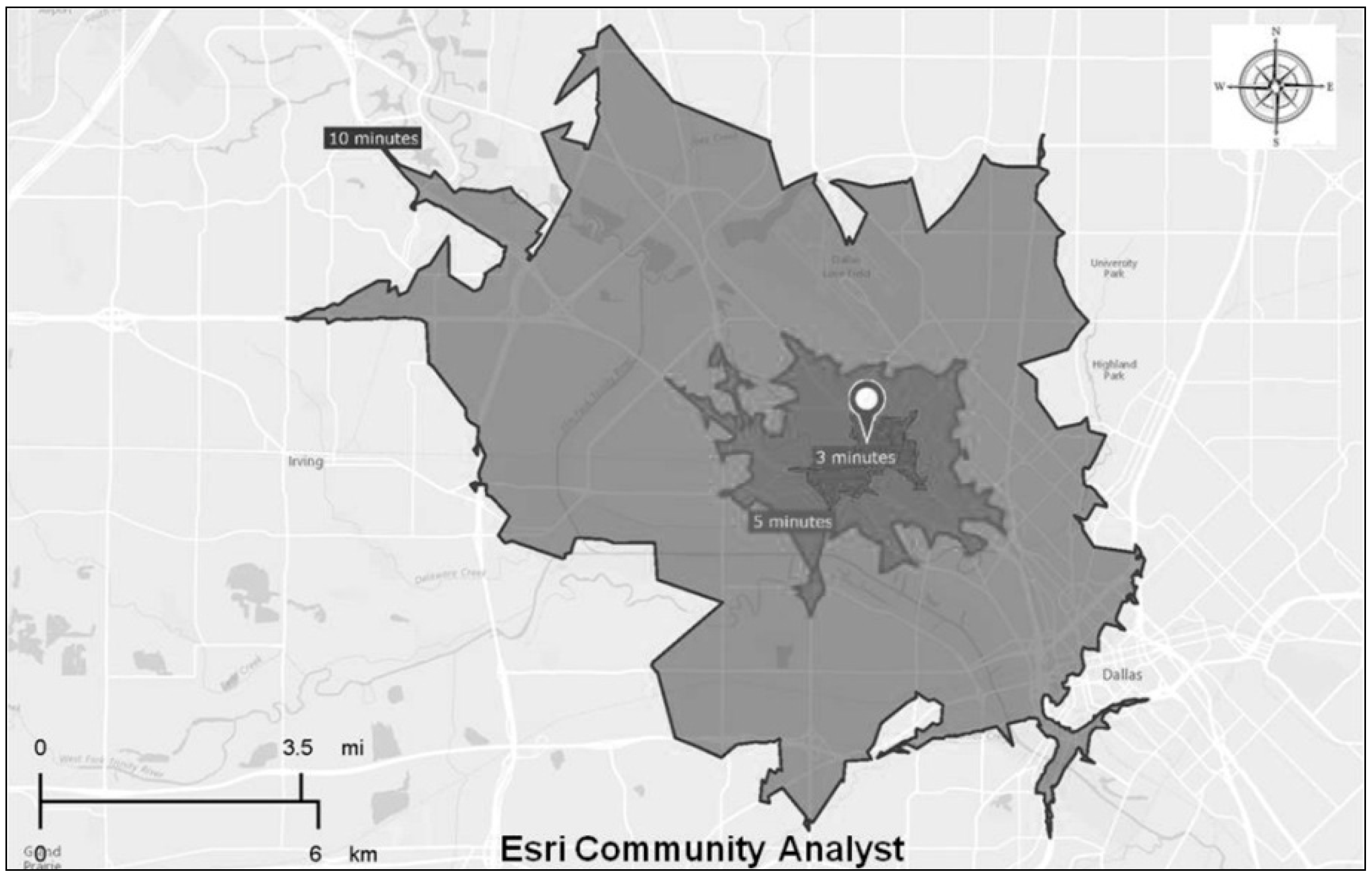
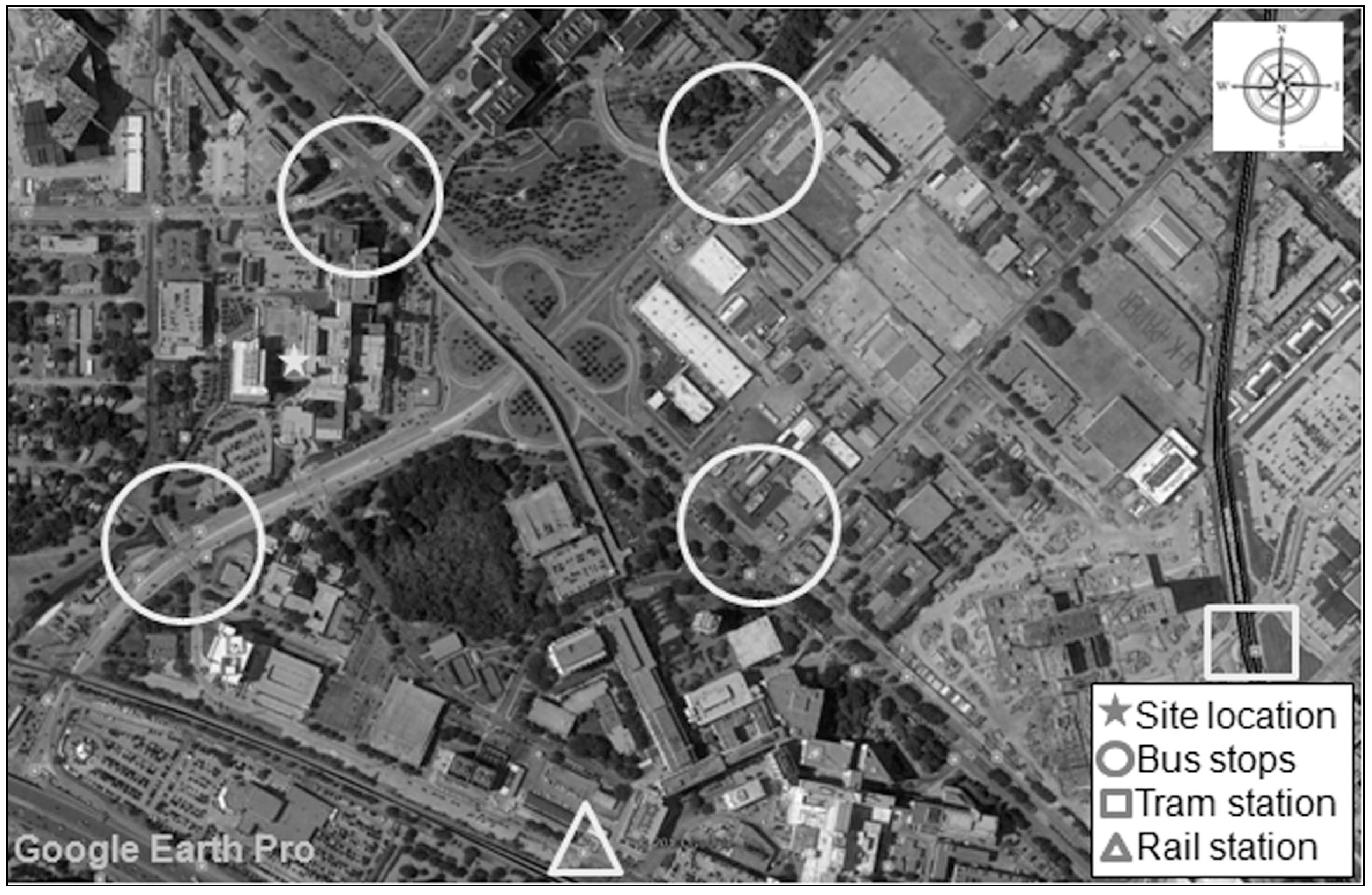
Figure 7 shows the boundaries of three-, five- and ten-minute driving times from/to the proposed hospital site under normal speed. Expected travel time by ambulance could be even shorter due to higher speed and yielding traffic. In addition, we analyzed public transport services around the site and identified comprehensive and high-frequency service to the area by different types of public transport services (e.g., bus, tram and rail) (
Figure 8). Several bus stops are located within 500 m of the facility, in addition to a railway station within 750 meters and a tram station within 1300 m.
Our application results demonstrate that the proposed new hospital site will be able to support the currently unmet needs of seniors: (1) there is a relatively high percentage of seniors in the hospital catchment area; (2) these seniors have low SES; (3) they currently under-utilize health service due to affordability; (4) although there are several hospitals in the same area, they are small and mostly private and do not address all acute healthcare needs or the affordability issue of low-income seniors; and (5) the hospital site is accessible in general as well as to seniors because it is well-supported by roads and public transport services. The newly proposed hospital site will thus provide a nice complement to existing services and meet the current needs of seniors as well as expected increased future needs as the catchment population ages.
Figure 6.
Average Annual Daily Traffic (AADT) of adjacent roads.
Figure 6.
Average Annual Daily Traffic (AADT) of adjacent roads.
Figure 7.
Boundaries of three-, five- and ten-minute driving times from/to the proposed hospital site.
Figure 7.
Boundaries of three-, five- and ten-minute driving times from/to the proposed hospital site.
Figure 8.
Public transport services around the site studied.
Figure 8.
Public transport services around the site studied.
5. Discussion
This section describes the strengths and weaknesses of the framework as well as web-based GIS tools used for our case study. Based on these, we propose future work required to enhance the decision-making process for hospital site selection for an aging population.
5.1. Strengths and Weaknesses
Our case study demonstrates the meaningful application of our framework to support evidence-based hospital site selection for an aging population. The evaluation framework provides an opportunity for urban planners and decision-makers to systematically reflect on key issues facing aging communities and use urban planning practices to effect positive changes and address evolving population health needs. To our knowledge, this is one of the first urban planning and decision support tools in development that attempts to proactively address a population health issue. GIS tools have the power to display complex analysis results in an easy-to-comprehend, visual manner; their use as a decision support tool should be widely promoted. This will help the planners and decision-makers transparently prioritize multiple alternative healthcare facility and resource plans for an aging population.
In building our framework, we tried to encompass the most critical elements based on the literature review and feedback from industrial experts and subsequently illustrate each criterion with one or two relevant factors. At this point, the framework is by no means definitive, and because of the complex and multidisciplinary nature of the issue, more extensive consultations and refinements are critical to ensure that future iterations encompass all the salient elements to be considered in making a decision about where a healthcare facility should be optimally located. Our current application is also limited due to the lack of availability of senior-specific data for some of the criteria. Drilling down into these data elements will improve the study’s validity. The methodology used for quantitatively scoring each evaluation element (
i.e., each sub-section of evaluation criteria) to create benchmarks for prioritized decision-making can be further enhanced by applying existing research about spatial-relation analysis, such as Moran’s I and distance-based weighing methods [
22,
29,
37]. In addition, to account for trade-offs among evaluation categories and their criteria, the methodology used for weighing each evaluation category and its criteria can be also refined using data-driven approaches and expanded focus group discussions.
Notwithstanding the history and politics of urban planning in America, the authors of this paper believe that it is high time to introduce an evidence-based tool with multidisciplinary contributions to inform politically contextualized discussions, help direct public sector contributions and help move the status quo toward the WHO’s recommendations of building global, age-friendly cities.
We further recommend that hospital planners continue to enhance and specialize in senior services as well as improve senior-friendliness through accessible designs (high contrast colors for better visualization, signal colors correlated with organizational functions, good signage for the elderly), density optimization (efficient distances within hospital for improved accessibility), and resource-efficient, flexible and modular construction methods for adaptability of the facility to necessary changes (new treatments, new technologies, etc.).
5.2. Future Works
Collecting and analyzing senior-specific data is an immediate next step that will improve the validity of the study. Furthermore, additional rigor can be achieved by expanding the scope of each criterion to include more elements, taking into account the data availability of the jurisdiction in question. In addition, case studies with more than two potential sites will be further required to test validity of the framework. The methodology used to quantitatively determine weights (i.e., trade-offs) and scores for each factor based on monetary values will enhance the framework’s ability to prioritize multiple factors and systematically compare multiple alternatives.