Implant Stability of Biological Hydroxyapatites Used in Dentistry
Abstract
:1. Introduction
2. Results
2.1. Graft Implants Characterization
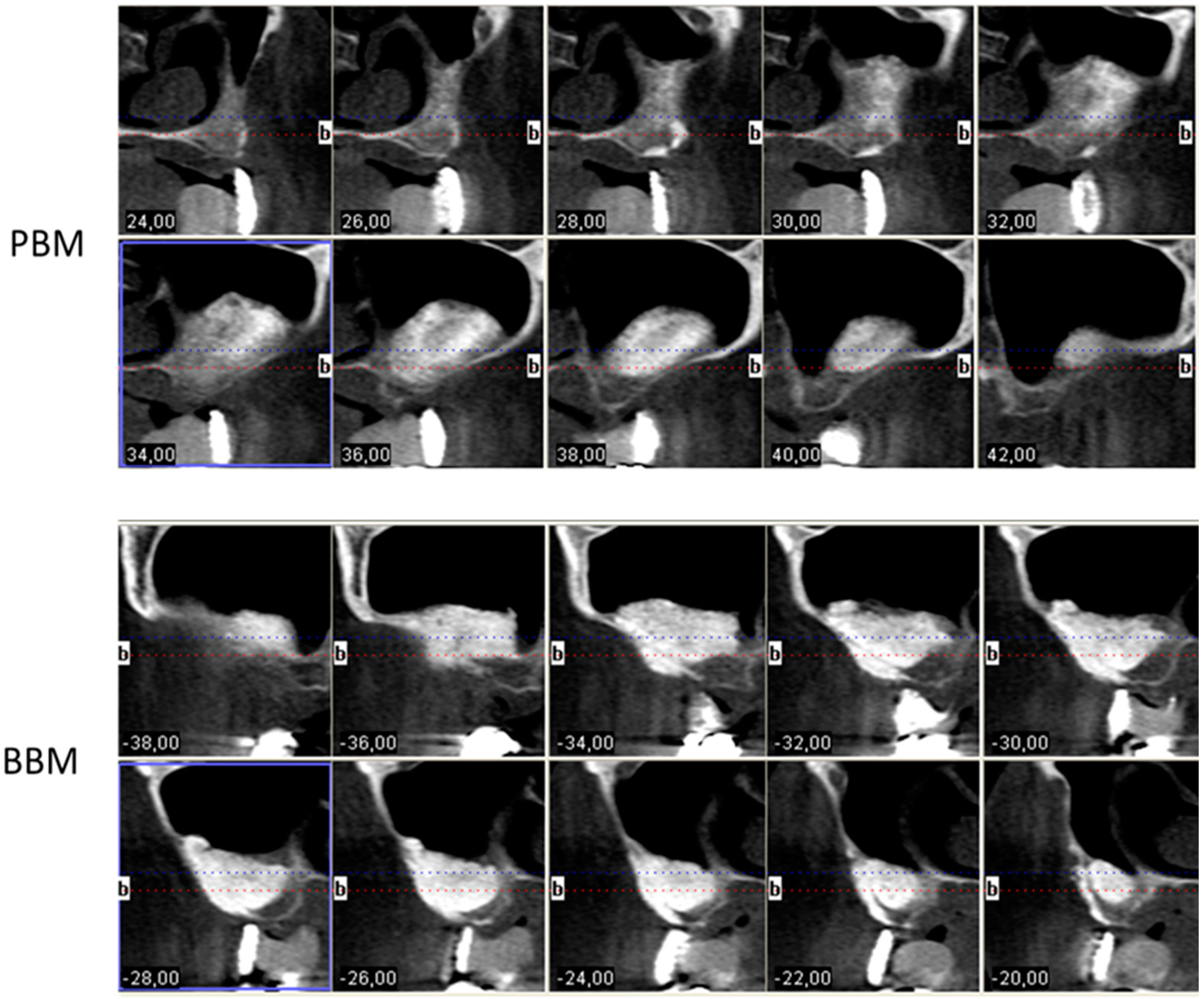
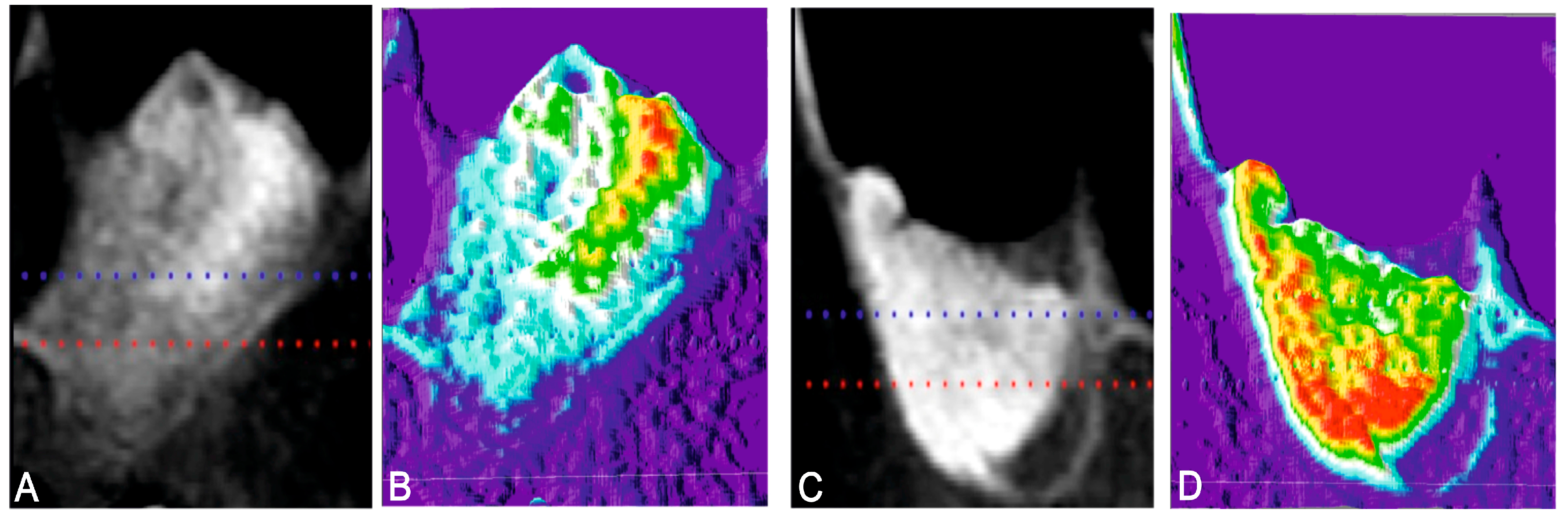
2.2. Radiological and Thermographic Results
2.3. ISQ Results
3. Discussion
4. Materials and Methods
4.1. Commercial Xenograft Materials
4.2. Implant Procedure
4.2.1. Patient Selection and Protocol
4.2.2. Inclusion and Exclusion Criteria
4.2.3. Surgical Procedure. First Phase
4.2.4. Radiographic Thermal Imaging Analysis
4.2.5. Surgical Procedure: Second Phase—Implant Insertion
4.3. Measuring Implant Stability
4.4. Statistical Evaluation
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sharan, A.; Madjar, D. Maxillary sinus pneumatization following extractions: A radiographic study. Int. J. Oral Maxillofac. Implant. 2008, 23, 48–56. [Google Scholar]
- Aghaloo, T.L.; Moy, P.K. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int. J. Oral Maxillofac. Implant. 2007, 22, 49–70. [Google Scholar]
- Corbella, S.; Taschieri, S.; Del Fabbro, M. Long-term outcomes for the treatment of atrophic posterior maxilla: A systematic review of literature. Clin. Implant Dent. Relat. Res. 2015, 17, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Felice, P.; Soardi, E.; Pellegrino, G.; Pistilli, R.; Marchetti, C.; Gessaroli, M.; Esposito, M. Treatment of the atrophic edentulous maxilla: Short implants versus bone augmentation for placing longer implants. Five-month post-loading results of a pilot randomised controlled trial. Eur. J. Oral Implantol. 2011, 4, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Barausse, C.; Pistilli, R.; Sammartino, G.; Grandi, G.; Felice, P. Short implants versus bone augmentation for placing longer implants in atrophic maxillae: One-year post-loading results of a pilot randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 257–268. [Google Scholar] [PubMed]
- Nedir, R.; Nurdin, N.; Abi-Najm, S.; El Hage, M.; Bischof, M. Short implants placed with or without grafting into atrophic sinuses: The 5-year results of a prospective randomized controlled study. Clin. Oral Implant. Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Khouly, I.; Veitz-Keenan, A. Insufficient evidence for sinus lifts over short implants for dental implant rehabilitation. Evid. Based Dent. 2015, 16, 21–22. [Google Scholar] [CrossRef] [PubMed]
- Fan, T.; Li, Y.; Deng, W.W.; Wu, T.; Zhang, W. Short Implants (5 to 8 mm) Versus Longer Implants (>8 mm) with Sinus Lifting in Atrophic Posterior Maxilla: A Meta-Analysis of RCTs. Clin. Implant Dent. Relat. Res. 2017, 19, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Kolerman, R.; Samorodnitzky, G.R.; Barnea, E.; Tal, H. Histomorphometric analysis of newly formed bone after bilateral maxillary sinus augmentation using two different osteoconductive materials and internal collagen membrane. Int. J. Periodontics Restor. Dent. 2012, 32, 21–28. [Google Scholar]
- Wallace, S.S.; Froum, S.J. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann. Periodontol. 2003, 8, 328–343. [Google Scholar] [CrossRef] [PubMed]
- Tuna, T.; Yorgidis, M.; Strub, J.R. Prognosis of implants and fixed restorations after lateral sinus elevation: A literature review. J. Oral Rehabil. 2012, 39, 226–238. [Google Scholar] [CrossRef] [PubMed]
- Traini, T.; Piattelli, A.; Caputi, S.; Degidi, M.; Mangano, C.; Scarano, A.; Perrotti, V.; Iezzi, G. Regeneration of Human Bone Using Different Bone Substitute Biomaterials. Clin. Implant Dent. Relat. Res. 2015, 17, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Baqain, Z.H.; Moqbel, W.Y.; Sawair, F.A. Early dental implant failure: Risk factors. Br. J. Oral Maxillofac. Surg. 2012, 50, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Zinser, M.J.; Randelzhofer, P.; Kuiper, L.; Zöller, J.E.; De Lange, G.L. The predictors of implant failure after maxillary sinus floor augmentation and reconstruction: A retrospective study of 1045 consecutive implants. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 571–582. [Google Scholar] [CrossRef] [PubMed]
- Herliansyah, M.K.; Hamdia, M.; de-Ektessabic, A.I.; Wildanb, M.W.; Toque, J.A. The influence of sintering temperature on the properties of compacted bovine. Mater. Sci. Eng. C 2009, 29, 1674–1680. [Google Scholar] [CrossRef]
- Conz, M.B.; Granjeiro, J.M.; Soares, G.A. Physicochemical characterization of six commercial hydroxyapatites for medical-dental applicatons as bone graft. J. Appl. Oral Sci. 2005, 13, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Barakat, N.A.M.; Khalil, K.A.; Sheikh, F.A.; Omran, A.M.; Gaihre, B.; Khil, S.M.; Kim, H.Y. Physiochemical characterizations of hydroxyapatite extracted from bovine bones by three different methods: Extraction of biologically desirable Hap. Mater. Sci. Eng. C 2008, 28, 1381–1387. [Google Scholar] [CrossRef]
- Azran, Y.M.; Idris, B.; Rusnah, M.; Rohaida, C.H. HAp physical investigation the effect of sintering temperature. Med. J. Malaysia 2004, 59, 79–80. [Google Scholar] [PubMed]
- Danesh-Sani, S.A.; Engebretson, S.P.; Janal, M.N. Histomorphometric results of different grafting materials and effect of healing time on bone maturation after sinus floor augmentation: A systematic review and meta-analysis. J. Periodontal Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Felice, P.; Pistilli, R.; Piattelli, M.; Soardi, E.; Pellegrino, G.; Corvino, V.; Esposito, M. 1-stage versus 2-stage lateral maxillary sinus lift procedures: 4-month post-loading results of a multicenter randomised controlled trial. Eur. J. Oral Implantol. 2013, 6, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Busenlechner, D.; Huber, C.D.; Vasak, C.; Dobsak, A.; Gruber, R.; Watzek, G. Sinus augmentation analysis revised: The gradient of graft consolidation. Clin. Oral Implant. Res. 2009, 20, 1078–1083. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Shimizu, Y.; Asai, S.; Ooya, K. Experimental sinus grafting with the use of deproteinized bone particles of different sizes. Clin. Oral Implant. Res. 2003, 14, 548–555. [Google Scholar] [CrossRef]
- Gupta, R.K.; Padmanabhan, T.V. An evaluation of the resonance frequency analysis device: Examiner reliability and repeatability of readings. J. Oral Implantol. 2013, 39, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Lioubavina-Hack, N.; Lang, N.P.; Karring, T. Significance of primary stability for osseointegration of dental implants. Clin. Oral Implant. Res. 2006, 17, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontology 2000 2008, 47, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.; Vijayaraghavan, V.; Swami, V. Current trends to measure implant stability. J. Indian Prosthodont. Soc. 2016, 16, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Cehreli, M.C.; Karasoy, D.; Akca, K.; Eckert, S.E. Meta-analysis of methods used to assess implant stability. Int. J. Oral Maxillofac. Implant. 2009, 24, 1015–1032. [Google Scholar]
- Atsumi, M.; Park, S.H.; Wang, H.L. Methods used to assess implant stability: Current status. Int. J. Oral Maxillofac. Implant. 2007, 22, 743–754. [Google Scholar] [CrossRef]
- Lundgren, S.; Cricchio, G.; Hallman, M.; Jungner, M.; Rasmusson, L.; Sennerby, L. Sinus floor elevation procedures to enable implant placement and integration: Techniques, biological aspects and clinical outcomes. Periodontology 2000 2017, 73, 103–120. [Google Scholar] [CrossRef] [PubMed]
- Iezzi, G.; Scarano, A.; Di Stefano, D.; Arosio, P.; Doi, K.; Ricci, L.; Piattelli, A.; Perrotti, V. Correlation between the bone density recorded by a computerized implant motor and by a histomorphometric analysis: A preliminary in vitro study on bovine ribs. Clin. Implant. Dent. Relat. Res. 2015, 17, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Marquezan, M.; Osório, A.; Sant’Anna, E.; Souza, M.M.; Maia, L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin. Oral Implant. Res. 2012, 23, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.E.; Novaes, A.B.; Haraszthy, V.I.; Bittencourt, M.; Martinelli, C.B.; Luczyszyn, S.M. A clinical study of 406 sinus augmentations with 100% anorganic bovine bone. J. Periodontol. 2009, 80, 1920–1927. [Google Scholar] [CrossRef] [PubMed]
- Ramírez Fernández, M.P.; Gehrke, S.A.; Perrez Albacete Martinez, C.; Calvo Guirado, J.L.; De Aza, P.N. SEM-EDX Study of the degradation process of two xenograft matrials used in sinus lift procedures. Materials 2017, 10, 542. [Google Scholar] [CrossRef]
- Nasr, S.; Slot, D.E.; Bahaa, S.; Dörfer, C.E.; Fawzy El-Sayed, K.M. Dental implants combined with sinus augmentation: What is the merit of bone grafting? A systematic review. J. Craniomaxillofac. Surg. 2016, 44, 1607–1617. [Google Scholar] [CrossRef] [PubMed]
- Rammelsberg, P.; Schmitter, M.; Gabbert, O.; Lorenzo-Bermejo, J.; Eiffler, C.; Schwarz, S. Influence of bone augmentation procedures on the short-term prognosis of simultaneously placed implants. Clin. Oral Implant. Res. 2012, 23, 1232–1237. [Google Scholar] [CrossRef] [PubMed]
- Knöfler, W.; Barth, T.; Graul, R.; Krampe, D. Retrospective analysis of 10,000 implants from insertion up to 20 years-analysis of implantations using augmentative procedures. Int. J. Implant. Dent. 2016, 2, 25. [Google Scholar] [CrossRef]
- Jensen, S.S.; Terheyden, H. Bone augmentation procedures in localized defects in the alveolar ridge: Clinical results with different bone grafts and bone-substitute materials. Int. J. Oral Maxillofac. Implant. 2009, 24, 218–236. [Google Scholar]
- Herrero-Climent, M.; Albertini, M.; Rios-Santos, J.V.; Lázaro-Calvo, P.; Fernández-Palacín, A.; Bullon, P. Resonance frequency analysis-reliability in third generation instruments: Osstell mentor®. Med. Oral Patol. Oral Cir. Bucal 2012, 17, 801–806. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Santos-García, R.; Jaramillo-Santos, R.; Romero-Ruiz, M.M.; Fernández-Palacin, A.; Lázaro-Calvo, P.; Bullón, P.; Ríos-Santos, J.V. Assessment of Osstell ISQ’s reliability for implant stability measurement: A cross-sectional clinical study. Med. Oral Patol. Oral. Cir. Bucal 2013, 18, 877–882. [Google Scholar] [CrossRef]
- Degidi, M.; Perrotti, V.; Piattelli, A.; Iezzi, G. Mineralized bone-implant contact and implant stability quotient in 16 human implants retrieved after early healing periods: A histologic and histomorphometric evaluation. Int. J. Oral Maxillofac. Implant. 2010, 25, 45–48. [Google Scholar]
- Al-Khaldi, N.; Sleeman, D.; Allen, F. Stability of dental implants in grafted bone in the anterior maxilla: Longitudinal study. Br. J. Oral Maxillofac. Surg. 2011, 49, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Friberg, B.; Ekestubbe, A.; Sennerby, L. Clinical outcome of Brånemark System implants of various diameters: A retrospective study. Int. J. Oral Maxillofac. Implant. 2002, 17, 671–677. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Maghaireh, H.; Worthington, H.V. Interventions for replacing missing teeth: Different times for loading dental implants. Cochrane Database Syst. Rev. 2013, 28, CD003878. [Google Scholar] [CrossRef]
- Javed, F.; Romanos, G.E. Role of implant diameter on long-term survival of dental implants placed in posterior maxilla: A systematic review. Clin. Oral Investig. 2015, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Schiuma, D.; Plecko, M.; Kloub, M.; Rothstock, S.; Windolf, M.; Gueorguiev, B. Influence of peri-implant bone quality on implant stability. Med. Eng. Phys. 2013, 35, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Anil, S.; Aldosari, A. Impact of bone quality and implant type on the primary stability: An experimental study using bovine bone. J. Oral Implantol. 2015, 41, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Delgado-Ruiz, R.A.; Sacks, D.; Calvo-Guirado, J.L. Influence of the implant diameter and bone quality on the primary stability of porous tantalum trabecular metal dental implants: An in vitro biomechanical study. Clin. Oral Implant. Res. 2016, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, L.; Pagliani, L.; Petersson, A.; Verrocchi, D.; Volpe, S.; Andersson, P. Two different implant designs and impact of related drilling protocols on primary stability in different bone densities: An in vitro comparison study. Int. J. Oral Maxillofac. Implant. 2015, 30, 564–568. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; da Silva, U.T.; Del Fabbro, M. Does Implant Design Affect Implant Primary Stability? A Resonance Frequency Analysis-Based Randomized Split-Mouth Clinical Trial. J. Oral Implantol. 2015, 41, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Piattelli, A.; Iezzi, G.; Carinci, F. Do longer implants improve clinical outcome in immediate loading? Int. J. Oral Maxillofac. Surg. 2007, 36, 1172–1176. [Google Scholar] [CrossRef] [PubMed]
- Balleri, P.; Cozzolino, A.; Ghelli, L.; Momicchioli, G.; Varriale, A. Stability measurements of osseointegrated implants using Osstell in partially edentulous jaws after 1 year of loading: A pilot study. Clin. Implant. Dent. Relat. Res. 2002, 4, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Ostman, P.O.; Hellman, M.; Wendelhag, I.; Sennerby, L. Resonance frequency analysis measurements of implants at placement surgery. Int. J. Prosthodont. 2006, 19, 77–83. [Google Scholar] [PubMed]
- O’Sullivan, D.; Sennerby, L.; Meredith, N. Measurements comparing the initial stability of five designs of dental implants: A human cadaver study. Clin. Implant. Dent. Relat. Res. 2000, 2, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Ciornei, G.; Jucan, A.; Malmstrom, H.; Gupta, B. In vitro assessment of primary stability of Straumann® implant designs. Clin. Implant. Dent. Relat. Res. 2014, 16, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.S.; Aaboe, M.; Janner, S.F.; Saulacic, N.; Bornstein, M.M.; Bosshardt, D.D.; Buser, D. Influence of particle size of deproteinized bovine bone mineral on new bone formation and implant stability after simultaneous sinus floor elevation: A histomorphometric study in minipigs. Clin. Implant. Dent. Relat. Res. 2015, 17, 274–285. [Google Scholar] [CrossRef] [PubMed]
- Browaeys, H.; Bouvry, P.; De Bruyn, H. A literature review on biomaterials in sinus augmentation procedures. Clin. Implant. Dent. Relat. Res. 2007, 9, 166–177. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Piattelli, A. RFA values of implants placed in sinus grafted and nongrafted sites after 6 and 12 months. Clin. Implant. Dent. Relat. Res. 2009, 11, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Jensen, O.T.; Sennerby, L. Histologic analysis of clinically retrieved titanium microimplants placed in conjunction with maxillary sinus floor augmentation. Int. J. Oral Maxillofac. Implant. 1998, 13, 513–521. [Google Scholar]
- Lai, H.C.; Zhang, Z.Y.; Wang, F.; Zhuang, L.F.; Liu, X. Resonance frequency analysis of stability on ITI implants with osteotome sinus floor elevation technique without grafting: A 5-month prospective study. Clin. Oral Implant. Res. 2008, 19, 469–475. [Google Scholar] [CrossRef] [PubMed]
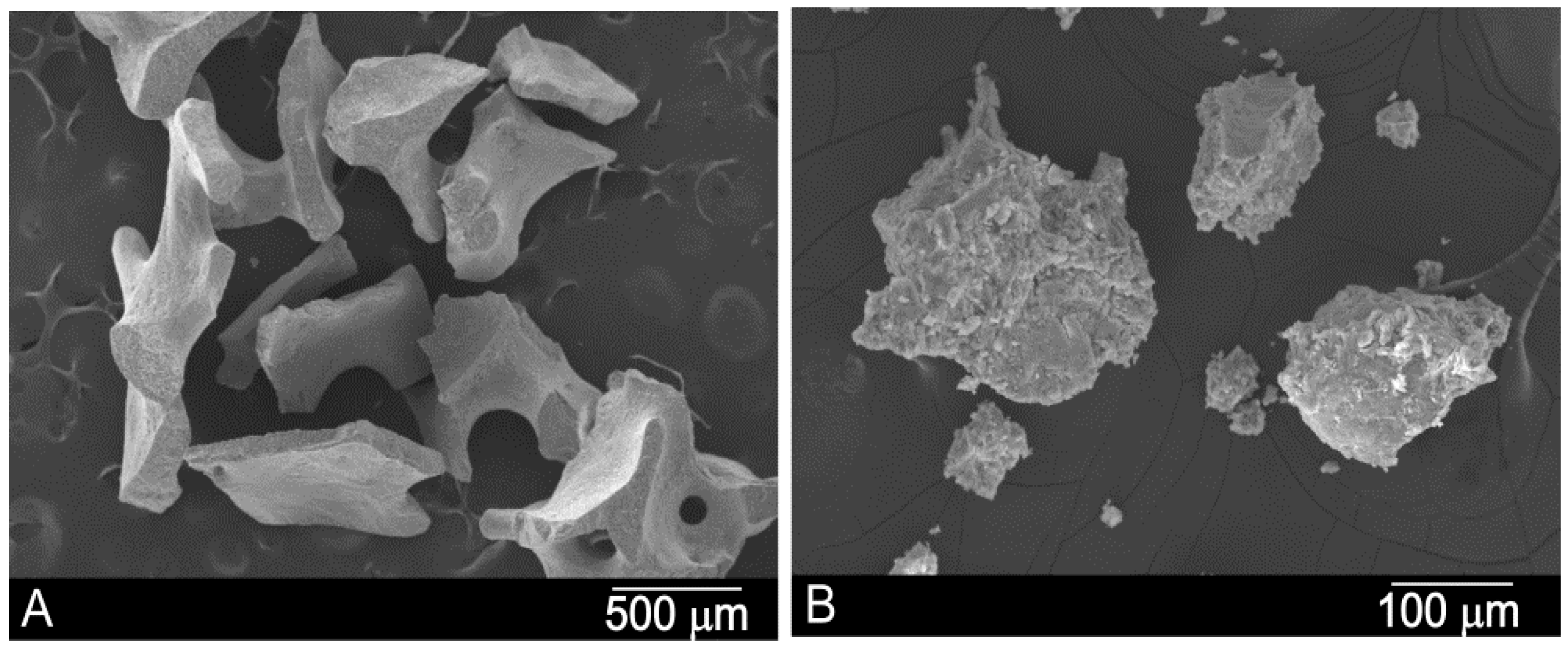





| Material | Phase/s | Ca/P Ratio | Particle Size (μm) | Crystal Size (nm) | Real Density (g/cc) | Porosity (%) | Surface Area (m2/g) |
|---|---|---|---|---|---|---|---|
| PBM | HA+Coll | 2.22 ± 0.08 | 600–1000 | 325 | 2.85 | 59.90 | 97.84 |
| BBM | HA | 2.31 ± 0.09 | 500–1000 | 732 | 2.98 | 49.13 | 2.77 |
| Number of Patients (Total) | 10 | |||||
| Number of Implants (Total) | 60 | |||||
| Osseointegrated (%) | 57 (95) | |||||
| Non Osseointegrated | 3 (5) | |||||
| Vestibule-Lingual (ISQ Values) | T1 | T2 | T3 | |||
| PBM | BBM | PBM | BBM | PBM | BBM | |
| Mean | 62.4 | 63.4 | 66.9 | 73.9 | 72.6 | 73.8 |
| SD | 2.92 | 2.88 | 2.67 | 4.11 | 7.67 | 2.99 |
| Median | 62.5 | 63.2 | 66.6 | 70.6 | 73.7 | 74 |
| Mesio-Distal (ISQ Values) | T1 | T2 | T3 | |||
| PBM | BBM | PBM | BBM | PBM | BBM | |
| Mean | 62.8 | 64.2 | 67.1 | 75.2 | 74.2 | 74.2 |
| SD | 3.23 | 3.18 | 2.33 | 4.29 | 7.59 | 3.01 |
| Median | 62.5 | 64.8 | 69.1 | 72.4 | 75.8 | 75.5 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramírez Fernández, M.P.; Gehrke, S.A.; Mazón, P.; Calvo-Guirado, J.L.; De Aza, P.N. Implant Stability of Biological Hydroxyapatites Used in Dentistry. Materials 2017, 10, 644. https://doi.org/10.3390/ma10060644
Ramírez Fernández MP, Gehrke SA, Mazón P, Calvo-Guirado JL, De Aza PN. Implant Stability of Biological Hydroxyapatites Used in Dentistry. Materials. 2017; 10(6):644. https://doi.org/10.3390/ma10060644
Chicago/Turabian StyleRamírez Fernández, Maria Piedad, Sergio A. Gehrke, Patricia Mazón, Jose L. Calvo-Guirado, and Piedad N. De Aza. 2017. "Implant Stability of Biological Hydroxyapatites Used in Dentistry" Materials 10, no. 6: 644. https://doi.org/10.3390/ma10060644
APA StyleRamírez Fernández, M. P., Gehrke, S. A., Mazón, P., Calvo-Guirado, J. L., & De Aza, P. N. (2017). Implant Stability of Biological Hydroxyapatites Used in Dentistry. Materials, 10(6), 644. https://doi.org/10.3390/ma10060644









