Intensity and Inhalation of Smoking in the Aetiology of Laryngeal Cancer
Abstract
:1. Introduction
2. Methods
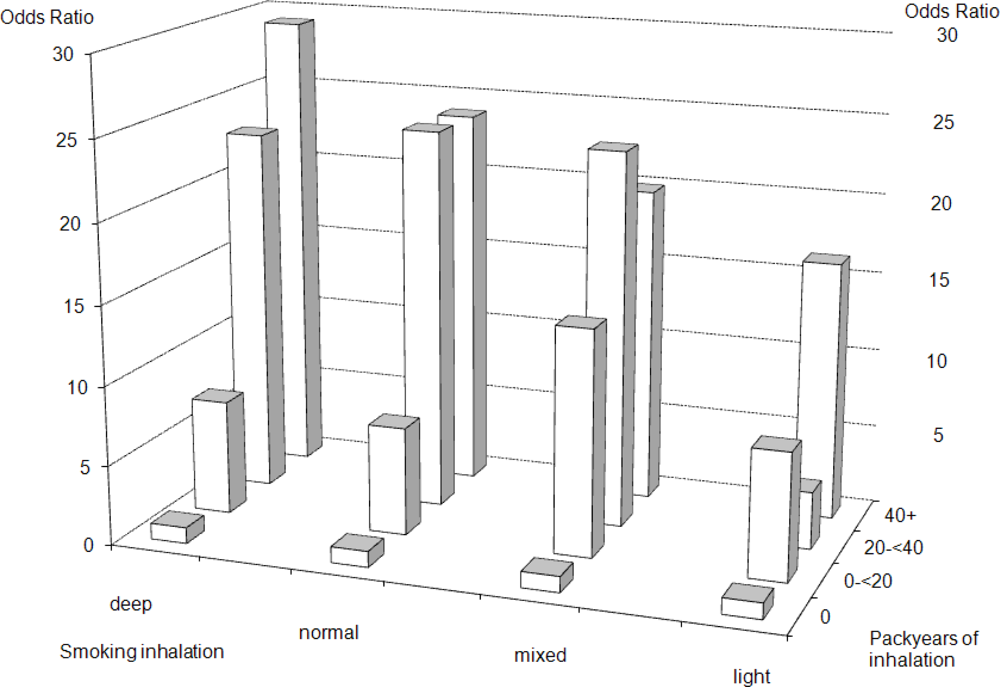
3. Results
4. Discussion
Acknowledgments
References
- Boyle, P. Cancer, cigarette smoking and premature death in Europe: A review including the Recommendations of European Cancer Experts Consensus Meeting, Helsinki, October 1996. Lung Cancer 1997, 17, 1–60. [Google Scholar]
- Kuper, H; Boffetta, P; Adami, HO. Tobacco use and cancer causation: Association by tumour type. J. Intern. Med 2002, 252, 206–224. [Google Scholar]
- Henley, SJ; Thun, MJ; Chao, A; Calle, EE. Association between exclusive pipe smoking and mortality from cancer and other diseases. J. Natl. Cancer Inst 2004, 96, 853–861. [Google Scholar]
- Lange, P; Nyboe, J; Appleyard, M; Jensen, G; Schnohr, P. Relationship of the type of tobacco and inhalation pattern to pulmonary and total mortality. Eur. Respir. J 1992, 5, 1111–1117. [Google Scholar]
- Henschke, CI; Yip, R; Miettinen, OS. Women’s susceptibility to tobacco carcinogens and survival after diagnosis of lung cancer. JAMA 2006, 296, 180–184. [Google Scholar]
- Wynder, EL; Muscat, JE. The changing epidemiology of smoking and lung cancer histology. Environ Health Perspect 1995, 103(Suppl 8), 143–148. [Google Scholar]
- Public Health Service, US Department of Health and Human Services; National Institutes of Health; National Cancer Institute. Preface. Risks Associated with Smoking Cigarettes with Low Maschine-Measured Yields of Tar and Nicotine; Smoking and Tobacco Control Monograph No 13;. National Cancer Institute: Rockville, MD, USA, 2001. Available online: http://cancercontrol.cancer.gov/tcrb/monographs/13/m13_preface.pdf (accessed on 16 December 2010).
- McCormack, VA; Agudo, A; Dahm, CC; Overvad, K; Olsen, A; Tjonneland, A; Kaaks, R; Boeing, H; Manjer, J; Almquist, M; et al. Cigar and pipe smoking and cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Int. J. Cancer 2010, 127, 2402–2411. [Google Scholar]
- Ramroth, H; Dietz, A; Becher, H. Occupational wood dust exposure and the risk of laryngeal cancer: a population based case-control study in Germany. Am. J. Ind. Med 2008, 51, 648–655. [Google Scholar]
- Ramroth, H; Dietz, A; Becher, H. Interaction effects and population-attributable risks for smoking and alcohol on laryngeal cancer and its subsites. A case-control study from Germany. Methods Inf. Med 2004, 43, 499–504. [Google Scholar]
- Neuhauser, M; Becher, H. Improved odds ratio estimation by post hoc stratification of case-control data. Stat. Med 1997, 16, 993–1004. [Google Scholar]
- Batzler, WA; Giersiepen, K; Hentschel, S; Husmann, G; Kaatsch, P; Katalinic, A; Kieschke, J; Kraywinkel, K; Meyer, M; Stabenow, C; Bertz, J; Haberland, J; Wolf, U. Krebs in Deutschland 2003–2004. Haufigkeiten und Trends; Robert Koch-Institut: Berlin, Germany, 2008. [Google Scholar]
- Husmann, G; Kaatsch, P; Katalinic, A; Bertz, J; Haberland, J; Kraywinkel, K; Wolf, U. Krebs in Deutschland 2005/2006. Haufigkeiten und Trends; Robert Koch-Institut: Berlin, Germany, 2010. [Google Scholar]
- Ramroth, H; Dietz, A; Becher, H. Environmental tobacco smoke and laryngeal cancer: Results from a population-based case-control study. Eur. Arch. Otorhinolaryngol 2008, 265, 1367–1371. [Google Scholar]
- Wald, NJ; Watt, HC. Prospective study of effect of switching from cigarettes to pipes or cigars on mortality from three smoking related diseases. BMJ 1997, 314, 1860–1863. [Google Scholar]
| Variable | Category | Cases N (%) | Controls N (%) | Cases vs. Controls Comparison (p-value) |
|---|---|---|---|---|
| Sex | Males | 236 (91.8) | 702 (91.3) | |
| Females | 21 (8.2) | 67 (8.7) | 0.78841 | |
| Age (years) | ... < 50 | 20 ( 7.8) | 64 ( 8.3) | |
| 50 <= … < 60 | 76 (29.6) | 227 (29.5) | ||
| 60 <= … < 70 | 94 (36.6) | 253 (32.9) | ||
| 70 <= … | 67 (26.1) | 225 (29.3) | 0.76522 | |
| Type of Smoking | Never | 13 ( 5.1) | 233 (30.3) | |
| Cigarettes only smoker | 234 (91.0) | 458 (59.5) | ||
| Cigars only smoker | 0 ( 0.0) | 9 ( 1.2) | ||
| Cigarillos only smoker | 0 ( 0.0) | 5 ( 0.7) | ||
| Pipe only smoker | 0 ( 0.0) | 10 ( 1.3) | ||
| mixed | 10 ( 3.9) | 54 ( 7.0) | <0.00011 | |
| Inhalation | Deep inhalers | 170 (66.1) | 320 (41.6) | |
| Normal smoking | 40 (15.6) | 107 (13.9) | ||
| Light inhalation | 7 ( 2.7) | 51 ( 6.6) | ||
| Mixed inhalation | 27 (10.5) | 58 ( 7.5) | <0.00011 | |
| Deep inhalers (packyears) | 0 | 87 (33.9) | 449 (58.4) | |
| 0 < … < 20 | 18 ( 7.0) | 144 (18.7) | ||
| 20 <= … < 40 | 60 (23.3) | 93 (12.1) | ||
| 40 <= … | 92 (35.8) | 83 (10.8) | <0.00012 | |
| Normal smoking (packyears) | 0 | 217 (84.4) | 662 (86.1) | |
| 0 < … < 20 | 8 ( 3.1) | 68 ( 8.8) | ||
| 20 <= … < 40 | 14 ( 5.4) | 21 ( 2.7) | ||
| 40 <= … | 18 ( 7.0) | 18 ( 2.3) | <0.00012 | |
| Light inhalation (packyears) | 0 | 250 (97.3) | 718 (93.4) | |
| 0 < … < 20 | 3 ( 1.2) | 40 ( 5.2) | ||
| 20 <= … < 40 | 1 ( 0.4) | 9 ( 1.2) | ||
| 40 <= … | 3 ( 1.2) | 2 ( 0.3) | 0.0032 | |
| Mixed inhalation (packyears) | 0 | 230 (89.5) | 711 (92.5) | |
| 0 < … < 20 | 3 ( 1.2) | 16 ( 2.1) | ||
| 20 <= … < 40 | 12 ( 4.7) | 24 ( 3.1) | ||
| 40 <= … | 12 ( 4.7) | 18 ( 2.3) | 0.11662 | |
| Smoking duration (years) | 0 | 13 ( 5.1) | 233 (30.3) | |
| 0 < … < 20 | 14 ( 5.4) | 152 (19.8) | ||
| 20 <= … < 40 | 99 (38.5) | 249 (32.4) | ||
| 40 <= … | 131 (51.0) | 135 (17.6) | <0.00012 | |
| Quitting smoking (years) | Within the last 2 years | 176 (68.5) | 383 (49.8) | |
| More than 2 years ago | 81 (31.5) | 386 (50.2) | <0.00011 | |
| Alcohol consumption (ml Ethanol) | 0 | 18 ( 7.1) | 39 ( 5.1) | |
| 0 < … < 25 | 49 (19.2) | 303 (39.5) | ||
| 25 <= … < 50 | 47 (18.4) | 178 (23.2) | ||
| 50 <= ... < 75 | 43 (16.9) | 127 (16.5) | ||
| 75 <= … | 98 (38.4) | 121 (15.8) | <0.00012 | |
| Years of Education (years) | <9 | 224 (87.2) | 479 (62.3) | |
| 9 | 18 ( 7.0) | 120 (15.6) | ||
| 10+ | 15 ( 5.8) | 170 (22.1) | <0.00012 | |
| Variable | Category | Cases N (%) | Controls N (%) | OR1 | CI1 | OR2 | CI2 |
|---|---|---|---|---|---|---|---|
| Smoker (yes/no) | Non-Smoker | 13 (5.1) | 233 (30.3) | 1 | - | 1 | - |
| Smoker | 244 (94.9) | 536 (69.7) | 17.1 | (9.2, 31.5) | 17.1 | (8.8, 33.4) | |
| Smoking duration * (years) | 0 | 13 (5.1) | 233 (30.3) | 1 | - | 1 | - |
| 0 < ... < 20 | 14 (5.4) | 152 (19.8) | 3.7 | (1.5, 8.8) | 4.5 | (1.8, 11.4) | |
| 20 <= ... < 40 | 99 (38.5) | 249 (32.4) | 11.7 | (6.0, 22.7) | 12.7 | (6.2, 25.8) | |
| 40 <= ... | 131 (51.0) | 135 (17.6) | 22.7 | (12.0, 42.8) | 21.6 | (10.9, 43.0) | |
| Inhalation * | deep | 170 (66.1) | 320 (41.6) | 1 | - | 1 | - |
| middle/mixed | 67 (26.1) | 165 (21.5) | 0.67 | (0.47, 0.97) | 0.73 | (0.50, 1.1) | |
| light | 7 (2.7) | 51 (6.6) | 0.23 | (0.10, 0.53) | 0.22 | (0.09, 0.55) | |
| Non-smoker | 13 (5.1) | 233 (30.3) | 0.05 | (0.02, 0.09) | 0.05 | (0.02, 0.10) | |
| Variable | Category | Cases N (%) | Controls N (%) | OR1 | CI1 | OR2 | CI2 |
|---|---|---|---|---|---|---|---|
| Non-Smokers | 13 (5.1) | 233 (30.3) | 1 | - | 1 | - | |
| Inhalation (per 10 packyears) | light | 51 (6.6) | 7 (2.7) | 1.3 | (1.0, 1.8) | 1.2 | (0.85, 1.6) |
| normal | 107 (13.9) | 40 (15.6) | 1.5 | (1.3, 1.7) | 1.4 | (1.2, 1.6) | |
| deep | 320 (41.6) | 170 (66.1) | 1.5 | (1.4, 1.6) | 1.4 | (1.3, 1.5) | |
| mixed | 58 (7.5) | 27 (10.5) | 1.4 | (1.2, 1.6) | 1.3 | (1.1, 1.5) | |
| Quitting smoking | <2 years | 383 (49.8) | 176 (68.5) | 1 | - | 1 | - |
| 2+ years | 386 (50.2) | 81 (31.5) | 0.43 | (0.30, 0.61) | 0.43 | (0.29, 0.62) | |
| Alcohol consumption | 2 drinks per day | - | - | - | - | 1.3 | (1.2, 1.5) |
| Years of education | <9 years | 224 (87.2) | 479 (62.3) | - | - | 1 | - |
| 9 years | 18 (7.0) | 120 (15.6) | - | - | 0.48 | (0.27, 0.85) | |
| 10+ years | 15 (5.8) | 170 (22.1) | - | - | 0.30 | (0.16, 0.56) | |
© 2011 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Ramroth, H.; Dietz, A.; Becher, H. Intensity and Inhalation of Smoking in the Aetiology of Laryngeal Cancer. Int. J. Environ. Res. Public Health 2011, 8, 976-984. https://doi.org/10.3390/ijerph8040976
Ramroth H, Dietz A, Becher H. Intensity and Inhalation of Smoking in the Aetiology of Laryngeal Cancer. International Journal of Environmental Research and Public Health. 2011; 8(4):976-984. https://doi.org/10.3390/ijerph8040976
Chicago/Turabian StyleRamroth, Heribert, Andreas Dietz, and Heiko Becher. 2011. "Intensity and Inhalation of Smoking in the Aetiology of Laryngeal Cancer" International Journal of Environmental Research and Public Health 8, no. 4: 976-984. https://doi.org/10.3390/ijerph8040976
APA StyleRamroth, H., Dietz, A., & Becher, H. (2011). Intensity and Inhalation of Smoking in the Aetiology of Laryngeal Cancer. International Journal of Environmental Research and Public Health, 8(4), 976-984. https://doi.org/10.3390/ijerph8040976