2.1. Framework
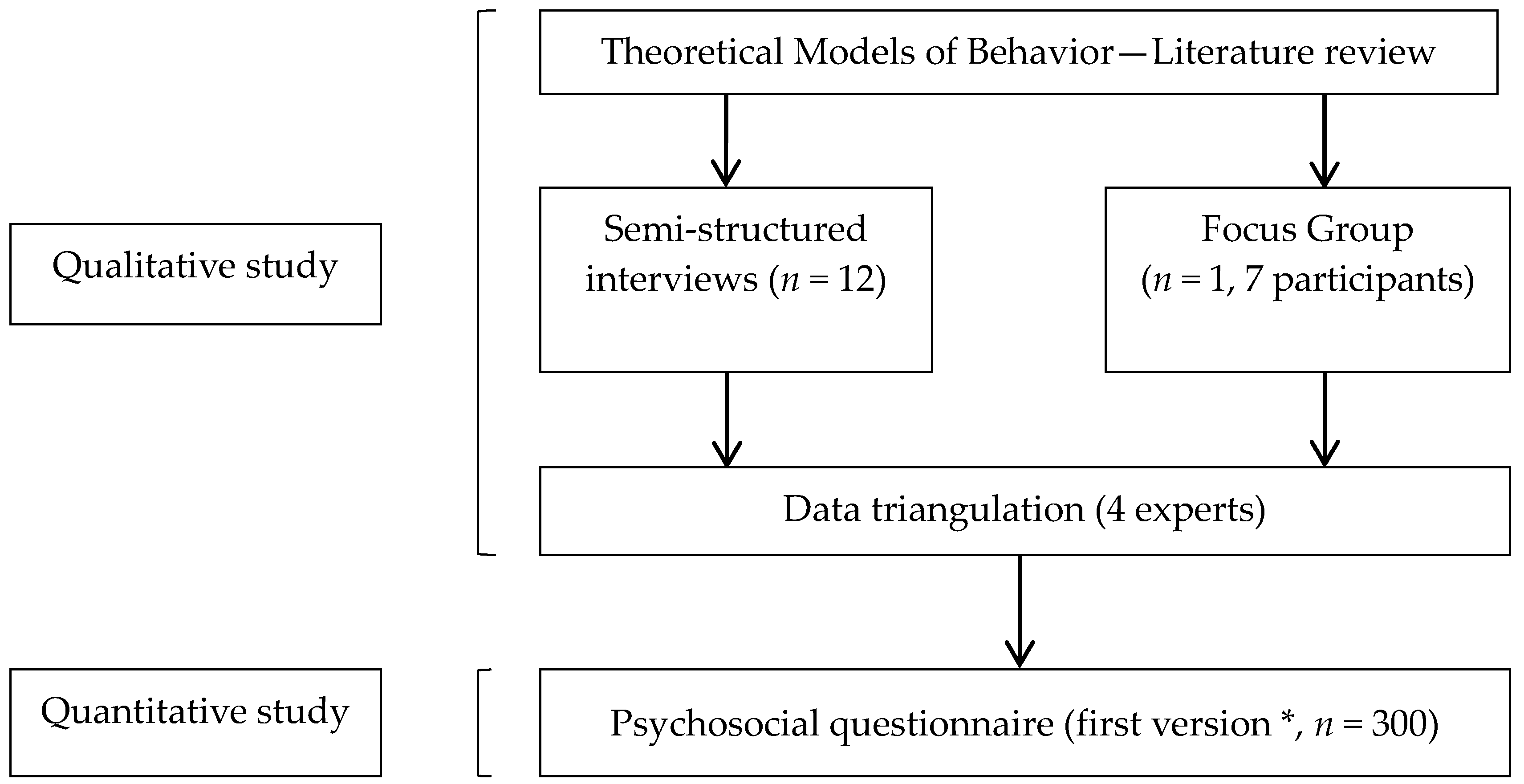
Our study was composed of three main steps: a qualitative study, with semi-structured interviews of pregnant women, a focus group of professionals, and a quantitative study administering a psychosocial questionnaire to pregnant or postpartum period women. A psychosocial questionnaire related to health behaviors, as our questionnaire, assesses the relations between individual psychological variables and variables related to the social context in order to better describe health behaviors in front of EDC risk exposure. These steps are detailed in
Figure 1.
We chose a theoretical model of health behavior revolving around risk perception: the Health Belief Model (HBM). In this model, severity, susceptibility, benefits, barriers, and cues to action determine probability of health behavior change [
28]. These criteria were used to build the interview grids for the semi-structured interviews and for the focus group, which were used then to design the psychosocial questionnaire in two main parts: (i) a first part assessing risk perception, with severity and susceptibility to EDC risk exposure and (ii) a second part assessing benefits, barriers and cues to action to adopt a healthy behavior.
The first step of the study (semi-structured interviews) was performed in 2014 in the city of Poitiers (France) by a student midwife. This consists of the use of a topic guide that contains open-ended question and provides a great flexibility to explore experiences and attitudes. A semi-structured interview provides much information. The target population was composed of adult pregnant women, speaking French, who had previously had children or not, and were consulting for pregnancy monitoring at the University Hospital of Poitiers or in a private midwifery office in Poitiers. From medical records, a panel was formed taking age and type of housing into account in order to recruit a diversified range of pregnant women. The panel for semi-structured interviews was composed of 12 pregnant women. Socio-demographic data on pregnant women are detailed in
Appendix A,
Table A1. The semi-structured interviews were recorded once in an audio file. They were manually transcribed afterwards. The length of each interview was about one hour. All data were processed anonymously. Verbatim were not given to the women and idea saturation was sought out. The interviews took place in a confidential area. The partner or a friend of the pregnant woman was sometimes present.
The second step was the focus group of professionals. It took place in March 2015 on the premises of the Faculty of Medicine and Pharmacy of Poitiers. The target population was composed of professionals from different fields in perinatology, health promotion and environmental health education. The professionals, or future professionals, were a student midwife, a pediatric nurse from a French departmental structure responsible for mothers and their children’s protection, a student in prevention psychology, a project leader at the French health care mutual, a project leader at a French association involved in health education and promotion, an organizer of health education workshops and a Ph.D. student in environmental health. Their characteristics are detailed in
Appendix A,
Table A2. These seven professionals did not know each other before the focus group and had no marked hierarchical links in order to ease each person’s speech, which was completely free. Three main questions were posed to this group, as relaunches, during the focus group: (i) “How you would talk about perinatal exposure to endocrine disruptors?”; (ii) “What factors are likely to interfere with the perception of exposure at the time of the interview with a woman, pregnant or not?”; and (iii) “What factors are likely to influence a change in behavior of this exposure to endocrine disruptors?”. The focus group lasted 90 min. It was recorded in the presence of an organizer (M.A.-L.) and an observer (J.A.) who was asked to note the physical language of every participant. Idea saturation was searched, until no new information was brought forth, according to focus group methodology. While a private midwife was not able to join the focus group, her ideas were collected during a semi-structured individual interview.
In the qualitative study, analysis of the semi-structured interviews and focus group was processed by examination of the verbatim, in three phases: (i) extraction of all information, (ii) detection of the relevant data and (iii) organization in logic trees. The themes were not identified in advance. The analytical “triangulation” method was chosen. Data were selected and sorted out using the RQDA qualitative analysis software, a CAQDAS-type software (Computer-Assisted Qualitative Data Analysis Software) running on the [R] program (R development core team).
Then, using the information gained from the qualitative study, we constructed a questionnaire to assess women’s knowledge toward EDC, attitudes such as EDC risk perception and anxiety, and behaviors to reduce EDC exposure. It comprised 37 questions divided into 4 sections.
The third step consisted in the administration of this questionnaire to pregnant women or in postpartum period.
2.2. Population and Recruitment
A cross-sectional study was performed between 18 August 2015 and 8 April 2016 in French department of Vienne. Women were informed of the study by clinicians, leaflets in participant midwives’ offices (in and around the city of Poitiers) and in the 3 maternity units of the department, and on a social network.
Eligible subjects were pregnant women with a singleton pregnancy without complication, or women having given birth and being hospitalized with their healthy newborn in a maternity unit with a vaginal or uncomplicated cesarean delivery, French-speaking and aged 18 or older.
Before each interview, a simple explanation was given concerning the theme of the study. All women gave written informed consent. This study was approved by the local ethics committee (Comité de Protection des Personnes Ouest III, reference 2015-A00031-48, date of approval: 19 May 2015).
2.3. Data Collection
For the cross-sectional study, data were collected by a questionnaire in an interview with a researcher in the hospital room for women in postpartum period or in a medical office for pregnant women. The researchers were trained to limit information bias. This questionnaire contained visual analog scales which were scored from 0 at the left extremity to 100 at the right extremity.
Socio-demographic data (age, profession, education level, marital status and parity) and smoking status were collected in medical records.
2.3.1. Knowledge
We explored women’s knowledge about EDC, with questions about definition, ability to give some names, source of exposure, way of exposure and knowledge about how to avoid EDC. These items were assessed with closed-questions, except for the knowledge of molecules’ names. That allowed us to construct an EDC knowledge score with a maximum of 100 points. We used photo-language
® to increase the accessibility of the questions on exposure sources, knowledge of plastic packaging resin identification codes and those to avoid in daily life [
20,
29,
30]. There was also a question on perceived knowledge about EDC assessed with a visual analog scale. After this part, EDC definition such as “chemical mixtures in the environment that possess properties to alter function(s) of the endocrine system” was given to the women.
2.3.2. Attitude: Perception of EDC Risk
Perception of EDC risk for both maternal health and fetal health was then explored in the questionnaire. Questions like “EDC risk for my health is” or “EDC risk for my baby to have a low birth weight is”, or also “EDC risk for my baby to have fertility trouble in adulthood is” were assessed by the women on a visual analog scale and in a general way in three grades: null, low or high. Risk assessment “in a general way” relates to
perceived severity, whereas risk assessment for a given pregnant woman or a given child is considered as
perceived susceptibility. This part ended by assessing the concept of what a healthy baby is: women were asked to agree or disagree with several statements, for example “a healthy baby has normal weight at birth” [
31,
32]. Moreover, the hierarchy of risk during pregnancy between genetic and metabolic diseases, infectious diseases, toxic diseases, chemical-related diseases and pregnancy ailments was a subject on which the participants were interrogated.
2.3.3. Behaviors
We evaluated behaviors through cues to action. There were open questions on possible actions to limit EDC exposure like “how do you think you can act?” and questions to assess the efforts to reduce exposure with a visual analog scale.
2.3.4. Anxiety
Women evaluated their own situational anxiety before and after answering the questionnaire on a visual analog scale: the left extremity was for “Not anxious” and the right extremity for “Very anxious”. Anxiety in the preceding days and general anxiety were also assessed with the same tool. This approach of measuring both situational and general anxiety trait was inspired by the State-Trait Anxiety Inventory [
33,
34].
2.4. Statistical Analysis
In the cross-sectional study, continuous variables were expressed as mean, standard deviation (SD) and quartile. Categorical variables were expressed as frequency and percentage. The difference of situational anxiety between after and before administering the questionnaire was used to define the change of anxiety due to the administration of the questionnaire. A paired t-test was performed to assess change in anxiety when answering the questionnaire. The change in anxiety was then categorized as “increased anxiety” if the difference was strictly greater than zero point, or “stabilized or decreased anxiety” if this difference was equal to or less than zero point. Continuous variables such as perceived health, general anxiety and knowledge about EDC score were then categorized in quartile according to sample distribution. Bivariate analyses were performed to assess anxiety increasing with factors as age, socio-professional category, perceived health, general anxiety, pregnancy anxiety and knowledge about EDC. A multivariate logistic regression model was applied to assess predictors of increased anxiety. Variables that were associated with anxiety increasing at a p-value of <0.20 in bivariate analysis were included in the model except for age. All analysis was conducted in SAS 9.4 (SAS institute Inc., Cary, NC, USA) and Stata Statistical Software: Release 14 (College Station, TX, USA: StataCorp LP).